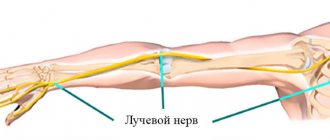
When the ulnar nerve is damaged, which is especially common in hockey players, pain is common, usually radiating to the little finger. Possible cyanosis, sweating disorders and a decrease in skin temperature in the area approximately coinciding with the area of sensory disorders.
The main goals of massage are:
providing analgesic effects;
accelerating the restoration of nerve conduction and sensitivity.
Massage technique
First, massage the cervicothoracic spine, then a preliminary massage of the entire limb. Apply stroking, kneading, rubbing using the “forceps” technique. Then the muscles innervated by the ulnar nerve are massaged using kneading, rubbing with the pads of the fingers and thumb. In addition, vibration is used.
Massage of the ulnar nerve itself, since it is accessible, is performed by stroking it along its entire length. The duration of the massage is from 10 to 15 minutes.
Causes of defeat
Neuropathy of the median nerve is considered to be damage to a section of the median nerve. The cause of the disease is often swelling of the soft tissues due to any mechanical damage or disease.
Damage to the median nerve is caused by the following factors:
- Injuries. Sprains, dislocations, fractures, bruises provoke dilation of blood vessels, fluid accumulates in the soft tissues. The nerve is compressed. The situation can be aggravated by bone damage and improper fusion.
- Arthritis. With this disease, the soft tissues of the body swell and pressure occurs on the nerve. Chronic disease often leads to disastrous results, hand deformation. This occurs due to the fact that the tissues begin to wear away, and the surfaces of the joints undergo fusion, exposing the bone.
- Fluid in soft tissues also accumulates due to other diseases, such as: nephrosclerosis, problems with the kidneys, problems with thyroid hormones, pregnancy, menopause, ischemia, as well as some other pathologies.
- Genetic predisposition. If parents or grandparents suffered from joint problems, then sometimes this is inherited.
- The risk group includes people suffering from diabetes. Due to impaired glucose metabolism and oxygen starvation of cells, nerve fibers are destroyed.
- . This disease belongs to diseases of the peripheral nervous system. Blood circulation is disrupted when the hands do not change their position while in a static state. This causes compression of the nerve. The syndrome often develops during prolonged use of the mouse and keyboard.
- Due to certain activities, compression-ischemic neuropathy of the median nerve occurs. It is associated with long-term macrotrauma to the nerve. This is facilitated, for example, by heavy physical labor with overload of the forearm and hand.
External causes of neuropathy of the median nerve of the arm also include:
- intoxication of the body;
- alcohol abuse;
- past infections (for example, HIV, diphtheria, herpes).
Classification
Neuropathy (neuropathy) is a disease characterized by damage to nerve fibers. When only one nerve becomes inflamed due to an illness, this is called mononeuropathy; two or more are called polyneuropathy.
Neuropathy is divided into 3 forms:
- (when nerve fibers and blood vessels are affected due to high blood sugar);
- toxic (infectious diseases, chemicals - all this affects the condition of nerve fibers);
- post-traumatic (this type of illness develops after damage to the myelin sheath of the nerve. Most often the sciatic, ulnar and radial nerves are injured);
Neuritis develops under similar conditions as median nerve neuropathy, but this disease is characterized by inflammation.
Based on the type and location of the pathology development zone, neuropathy has the following classification:
- damage to the lower extremities;
- sciatic nerve neuropathy;
- median nerve;
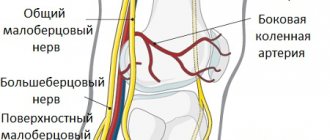
- peroneal nerve;
- facial nerve;
- tunnel neuropathy;
- sensorimotor neuropathy.
N medianus approaches the hand through the carpal tunnel. Here it innervates the muscles responsible for the opposition and abduction of the thumb, the lumbrical muscles, and the muscles that flex the finger. Its branches also supply nerve fibers to the wrist joint.
Median nerve neuropathy is associated with carpal tunnel syndrome, as the disease develops from constant compression in the wrist area.
From a surgical point of view, lesions of the median nerve are divided into open and closed. Open ones, in addition to the nerve, affect the tendons, blood vessels and muscles of the patient. Closed injuries include bruising, squeezing or spraining. Damage to the median nerve can develop along with plexopathy—damage to the cervical or brachial nerve plexuses.
Complex lesions (eg, trauma) often extend to the ulnar nerve. Cubital syndrome occurs (when the nerve of the cubital canal is compressed).
In what cases is it performed?
Neurolysis of the nerve is aimed at releasing it and restoring the impaired function of the limb. There is external and internal neurolysis:
- External is used when the scar has not penetrated deep into the nerve trunk.
- Internal is necessary when scar tissue grows between the fibers of the nerve that needs to be released.
There are many options depending on which nerve needs to be worked. Neurolysis of peripheral nerves is required after injuries, household or industrial injuries:
- Ulnar Nerve Area – Problems in this area are common and cause serious problems for the patient.
- The area of the median nerve under the knee greatly affects sensitivity.
- Radial nerve area - eliminating the problem of a hanging hand.
- Peroneal nerve area - to eliminate paralysis that prevents extension of the foot.
- Operations are also performed in the areas of the facial nerve, recurrent laryngeal nerve, etc.
Symptoms of the disease
Neuropathy of the median nerve of the hand (or neuritis) refers to diseases of the nervous system. When the disease begins to develop, the patient experiences difficulty clenching the first, second and third fingers of the hand into a fist. It is also difficult for him to simply move the second and third fingers. Other symptoms:
- Inability to oppose the thumb to the rest.
- Poor sensitivity in the palm and fingers.
- The appearance of the "monkey's paw". This is due to the fact that atrophy of the hand muscles occurs. As a result of this, the first finger of the hand is installed with the second in the same plane.
- The main symptom is acute pain, manifested in the area from the forearm to the fingers of the affected hand.
- Numbness of the hand, muscle weakness, tingling in the forearm.
Rehabilitation after neurolysis
Recovery after the intervention begins with the restoration of sensitivity and the cessation of painful sensations. This happens by relieving pressure on the nerve. All other functions are restored somewhat more slowly. The sooner the operation is performed, the easier the rehabilitation will be. After the operation, gradually:
- The functionality of the nerve improves or is completely restored.
- The pain disappears.
- The ability to feel is restored.
- Sweating returns to normal.
Diagnostics
To diagnose median nerve neuralgia, the doctor performs a series of procedures. As the disease develops, the patient cannot perform certain actions. For example, an attempt to scratch the surface of a table with the index finger (with the palm pressed against the table) fails. The patient is unable to clench his hand into a fist, or to place his thumb against the rest.
Another diagnostic method is to ask the patient to show the “mill”. To do this, with your arms crossed, you need to rotate the sore finger of your healthy hand around the thumb of the injured one. If the nerve is affected, the person will not be able to do this.
With median nerve neuropathy, the patient’s thumb cannot be moved to the side enough to form a right angle with the index finger. Also, the index finger of one hand cannot scratch the healthy hand if you put 2 palms together.
The doctor also diagnoses in the following ways:
- computed tomography of the hand;
- electroneuromyography;
- X-ray of the hand.
The examination will show which treatment is best. Diagnostic data will give the doctor the opportunity to study information about damage to the joint and bone canals of the nerve. The doctor will evaluate the reflexes, the condition of the muscles, and answer the question whether the disease is caused by the narrowness of the canal or the patient’s lifestyle. The doctor will determine whether it is possible to prescribe neurolysis to treat the disease - a surgical intervention during which the sensitivity of the nerves is restored.
Initial examination
To do this, he can prescribe the following types of diagnostics:
- computed and magnetic resonance imaging;
- X-ray of relevant organs and areas;
- testing for electrical excitability;
- certain tests for sensitivity and the ability of joints to perform certain motor functions.
When choosing a treatment method, the doctor takes into account the following factors:
- statute of limitations for injury;
- nature of damage;
- previous operations;
- degree of tissue scarring;
- level of nerve damage.
The specialist also evaluates the presence of concomitant pathologies.
Treatment
People with median nerve neuropathy rarely see a doctor at the first stage of the disease. Referral occurs when more alarming symptoms of neurological problems appear:
- spasms, convulsions;
- crawling sensation;
- problems with coordination;
- lack of sensitivity to temperatures.
For treatment of the median nerve of the arm to be successful, it is important to find the exact location of the lesion. It is equally important to establish the cause, which is done at the diagnostic stage.
For effective therapy, the doctor also needs:
- determine the degree of nerve damage;
- identify factors leading to this symptom;
- find a specific point of defeat.
Treatment happens:
- operative (using surgery);
- conservative (medicines). Often doctors turn to etiotropic therapy. This is treatment with antibiotics, antiviral agents, and vascular drugs.
The degree of damage is determined using a special examination - needle myography. If the nerve is compressed, treatment may include the following steps:
- Absorption therapy has a good effect in relieving nerve compression. It involves taking various medications and enzymes, agents that absorb and soften scar tissue. If the compression is not severe, manual therapy and special massage are often sufficient.
- Nerve restoration. Special medications prescribed by a doctor help “revitalize” the nerve.
- Muscle rehabilitation. The goal of therapy is to restore their muscle volume. Treatment procedures are prescribed by a rehabilitation doctor.
- Conservative treatment of the radial and ulnar nerves may include wearing special splints.
What other means are used?
- Demixidol in the carpal tunnel area.
- Acupuncture.
- Interstitial electrical stimulation.
- Therapeutic blockades in the carpal tunnel (diprospan plus lidocaine), intramuscular injections (movalis plus novocaine)
- Non-steroidal anti-inflammatory drugs, in addition to blockades (artrosilene).
During the diagnosis, a disease may also be identified - plexitis of the median nerve. It is caused by injury or infection.
Initially, medicinal, conservative methods of therapy are always used. If physiotherapeutic treatment is ineffective, surgery is performed in the clinic. The decision in favor of surgical intervention is made when the integrity of the nerve trunk is damaged and there is severe weakness in the fingers.
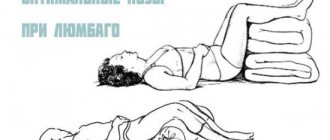
It is not recommended to treat the disease with folk remedies. During therapy, the patient should not overwork or subject himself to heavy physical activity. During the acute period of the disease, you need to lie down and rest more.
Exercise therapy and special exercises are usually prescribed in the postoperative period. Physiotherapy is carried out during conservative treatment or also after surgery.
For patients with the disease, sanatorium-resort treatment may be indicated. A contraindication to it is the acute period of the disease.
Types of procedure
The procedure is carried out using the following methods:
- external (external);
- internal (internal).
External neurolysis is usually performed: using a scalpel, the surgeon excises the connecting formations that compress the nerve. It is prescribed in cases where scarring has occurred in the tissues surrounding the nerve.
External neurolysis of the ulnar nerve
However, in some special cases, internal neurolysis is also prescribed: when the connecting formations are located between the bundles and pass through the nerve trunk.
This procedure is considered a very complex operation that must be carried out in a timely manner, since prolonged infringement of the nerve column can lead to paralysis of the limbs.
Prognosis and prevention
If there is no threat to health in the form of infections or injuries, sufficient attention should be paid to the prevention of neuropathy of the upper extremities, namely:
- Physical exercises for the arms. They include a simple warm-up for the hands.
- It is important to take breaks when working at a computer. When working with a computer mouse, you need to hold it in different hands alternately.
- Taking the vitamin is beneficial, as well as strengthening the overall health of a person. This reduces the risk of diseases of the neurology of the extremities.
It should be remembered that timely treatment begins to guarantee a good prognosis for future hand function. Restoring motor activity should begin as early as possible. Ignoring therapy or improper self-medication often causes disastrous consequences.
Neurolysis is a surgical procedure used to treat damage (including temperature) to nerve ganglia. The procedure carries certain risks: in rare cases, even greater nerve damage is possible.
The operation is performed only in a hospital setting, since it is technically difficult to perform. After the procedure, rehabilitation is prescribed to speed up and properly restore the nerve ganglion.
Where to do it?
Neurolysis requires extreme care, deep knowledge, high qualifications and experience. Neurolysis can be done at the clinic of the Central Clinical Hospital of the Russian Academy of Sciences in Moscow. Experienced specialists perform operations with a quality guarantee. To get a preliminary consultation and learn more about prices and terms of service, call the phone numbers listed on the website.
The disease neuropathy of the median nerve is often encountered in the practice of a neurologist. Proper movement of the arms and hands depends on the health of the radial, median, and ulnar nerves. The slightest damage to them leads to problems and discomfort. Disturbance in the functioning of nerves is accompanied by a disease called in neurology neuropathy of the upper extremities.
According to human anatomy, the median nerve (from the Latin nervus medianus) is the largest in the brachial plexus. It innervates almost the entire upper limb.
The median nerve responds:
- for flexing the muscles of the forearm;
- for motor activity of the thumb, middle and index finger;
- wrist sensitivity;
- abduction and adduction of the left and right hand.
General information
Median nerve neuropathy is quite common. The main contingent of patients are young and middle-aged people. The most common places of damage to the median nerve correspond to the areas of its greatest vulnerability - anatomical tunnels, in which compression (compression) of the nerve trunk is possible with the development of the so-called. tunnel syndrome. The most common tunnel syndrome is n. medianus is carpal tunnel syndrome - compression of the nerve as it passes to the hand. The average incidence in the population is 2-3%.
The second most common site of damage to the median nerve is its section in the upper part of the forearm, running between the muscle bundles of the pronator teres. This neuropathy is called “pronator teres syndrome.” In the lower third of the shoulder n. medianus may be compressed by an abnormal process of the humerus or Struther's ligament. Its lesion in this place is called Struzer's band syndrome, or supracondylar process syndrome of the shoulder. In the literature you can also find a synonymous name - Coulomb-Lord-Bedosier syndrome, which includes the names of the co-authors who first described this syndrome in 1963.
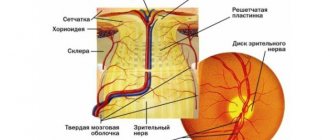
Anatomy of the median nerve
N. medianus is formed by the connection of the brachial plexus bundles, which, in turn, begin from the C5–Th1 spinal roots. After passing through the axillary zone, it runs next to the brachial artery along the medial edge of the humerus. In the lower third of the shoulder it goes deeper than the artery and passes under the Struther ligament; when it exits the forearm, it goes through the thickness of the pronator teres. Then it passes between the finger flexor muscles. In the shoulder, the median nerve does not give off branches; sensory branches extend from it to the elbow joint. On the forearm n. medianus innervates almost all the muscles of the anterior group.
From forearm to hand n. medianus passes through the carpal (carpal tunnel). On the hand, it innervates the opponensus and abductor pollicis muscles, partly the flexor pollicis muscle, and the lumbrical muscles. Sensory branches n. medianus innervate the wrist joint, the skin of the palmar surface of the radial half of the hand and the first 3.5 fingers.
Indications for the procedure
This surgical intervention is prescribed for any damage to the peripheral nerves in order to preserve its anatomical integrity.
Indications for this surgical intervention are as follows:
Now this operation has begun to be used for pseudoneuromas, brachial plexus injuries, partial nerve lesions, various injuries to the nerves of the digital branches, after unsuccessful nerve suture.
Neurolysis is carried out to restore the functions of peripheral nerves in the following cases:
- , causing “dangling hand” syndrome;
- , occurring with pronounced disturbances of sensory ability;
- , leading to impaired motor functionality;
- causing pain and inability to move normally;
- , characterized by paralysis of the extensors of the foot, fingers and muscles that ensure its outward rotation;
- , in which there is paralysis of the flexors of the foot, fingers and tibial muscles, which ensure its rotation inward.
Causes of median nerve neuropathy
Neuropathy of the median nerve can develop as a result of injury to the nerve: its bruise, partial rupture of fibers due to cut, torn, stab, gunshot wounds or damage by bone fragments during fractures of the shoulder and forearm, intra-articular fractures in the elbow or wrist joints. The cause of the lesion is n. medianus there may be dislocations or inflammatory changes (arthrosis, arthritis, bursitis) of these joints. Compression of the median nerve in any segment is possible with the development of tumors (lipomas, osteomas, hygromas, hemangiomas) or the formation of post-traumatic hematomas. Neuropathy can develop as a result of endocrine dysfunction (diabetes mellitus, acromegaly, hypothyroidism), with diseases leading to changes in ligaments, tendons and bone tissue (gout, rheumatism).
The development of tunnel syndrome is caused by compression of the trunk of the median nerve in the anatomical tunnel and disruption of its blood supply due to concomitant compression of the vessels supplying the nerve. In this regard, tunnel syndrome is also called compression-ischemic. Most often, neuropathy of the median nerve of this origin develops in connection with professional activities. For example, carpal tunnel syndrome affects painters, plasterers, carpenters, and packers; pronator teres syndrome is observed in guitarists, flutists, pianists, and in nursing women who hold a sleeping baby in their arm for a long time in a position where its head is on the mother’s forearm. The cause of tunnel syndrome can be a change in the anatomical structures that form the tunnel, which is noted with subluxations, tendon damage, deforming osteoarthritis, rheumatic disease of the periarticular tissues. In rare cases (less than 1% of the entire population), compression is caused by the presence of an abnormal process of the humerus.
Symptoms of median nerve neuropathy
Median nerve neuropathy is characterized by severe pain. The pain affects the medial surface of the forearm, hand and 1st-3rd fingers. It often has a burning causalgic character. As a rule, pain is accompanied by intense vegetative-trophic disorders, which is manifested by swelling, heat and redness or coldness and pallor of the wrist, the radial half of the palm and the 1st-3rd fingers.
The most noticeable symptoms of movement disorders are the inability to form a fist, oppose the thumb, or bend the 1st and 2nd fingers of the hand. Difficulty bending the 3rd finger. When the hand is flexed, it deviates to the ulnar side. A pathognomonic symptom is tenor muscle atrophy. The thumb is not opposed, but becomes on a par with the rest and the hand becomes similar to a monkey's paw.
Sensory disturbances are manifested by numbness and hypoesthesia in the area of innervation of the median nerve, i.e., the skin of the radial half of the palm, the palmar surface and the rear of the terminal phalanges of the 3.5 fingers. If the nerve is affected above the carpal tunnel, then the sensitivity of the palm is usually preserved, since its innervation is carried out by a branch extending from the median nerve before its entry into the canal.
Price fork
Neurolysis refers to a microsurgical type of surgery in which the nerve is freed from scar tissue.
The cost of the procedure is discussed during the patient’s consultation with the doctor and can vary significantly. This takes into account the severity of the pathological process, the presence of concomitant pathologies and complications, the type of planned operation and the length of stay in a medical institution.
In each city there are a number of clinics offering this procedure at different prices. In Moscow, for example, there are more than 30 medical institutions. The average cost of an operation in the capital is 50,000 rubles, so the cost of neurolysis of the radial nerve at the shoulder level ranges from 20,500 to 135,000 rubles, and intervention at the hand level will cost from 6,500 to 128,000 rubles.
In St. Petersburg, about 10 clinics offer their services, with an average cost of 25,000 rubles. The cost of surgery on the radial nerve ranges from 10,000 to 39,000 rubles, and neurolysis of the sciatic nerve will cost from 10,000 to 66,000 rubles.
In most cases, timely consultation with a doctor allows you to completely restore the conductive capacity of the nerve. Experienced doctors, modern equipment and innovative diagnostic methods will help you quickly and effectively get rid of peripheral nerve diseases.
When the C7-spinal nerve or the middle trunk of the brachial plexus is damaged, the function of the median nerve is partially affected, as a result there is a weakening of the flexion of the hand, its inward rotation in combination with damage to the radial nerve. Almost the same loss of function of the median nerve occurs with damage to the external bundle of the brachial plexus, into which the fibers of the upper peduncle of the nerve pass from the middle trunk, but in combination with damage to the musculocutaneous nerve.
With damage to the spinal nerves C8–Th1
, the lower trunk and internal bundle of the brachial plexus (Dejerine-Klumpke palsy) suffer in combination with damage to the ulnar nerve, those fibers of the median nerve that make up its lower leg (weakening of the finger flexors and thenar muscles).
The motor function of the median nerve mainly consists of inward rotation of the hand, palmar flexion of the hand due to contraction of the corresponding muscles, flexion of fingers, mainly I, II and III, extension of the middle and terminal phalanges of II and III fingers.
Sensitive fibers of the median nerve innervate the skin of the palmar surface of the I, II, III and radial half of the IV fingers, the corresponding part of the palm, as well as the skin of the rear of the terminal phalanges of these fingers.
When the median nerve is damaged (median nerve neuritis), inward rotation of the hand suffers, palmar flexion of the hand is weakened, flexion of the 1st, 2nd and 3rd fingers and extension of the middle phalanges of the 2nd and 3rd fingers are impaired.
Superficial sensitivity in case of median nerve neuritis is impaired on the hand in an area free from the innervation of the ulnar and radial nerves. Articular-muscular sensation with neuritis of the median nerve is always impaired in the terminal phalanx of the index, and often in the second finger.
Muscle atrophy with damage to the median nerve is most pronounced in the thenar region. The resulting flattening of the palm and bringing the thumb close and in one plane to the index finger create a peculiar position of the hand, which is called “monkey”. Pain when the median nerve is damaged, especially partial, is quite intense and often takes on a causal nature. In the latter case, the position of the hand may become bizarre.
Vasomotor-secretory-trophic disorders are also common and characteristic of lesions of the median nerve: the skin, especially the 1st, 2nd and 3rd fingers, becomes bluish or pale in color; nails become “dull”, brittle and streaked; skin atrophy, thinning of fingers (especially II and III), sweating disorders, hyperkeratosis, hypertrichosis, ulcerations, etc. are observed. These disorders, as well as pain, are more pronounced with partial rather than complete damage to the median nerve.
The median nerve, like the ulnar nerve, gives off its first branches only to the forearm, so the clinical picture when it is highly affected all the way from the axillary fossa to the upper parts of the forearm is the same. When the median nerve is damaged in the middle third of the forearm, the functions of internal rotation of the hand, palmar flexion of the hand and flexion of the middle phalanges are not affected.
The main tests to determine movement disorders that occur with damage to the median nerve (median nerve neuritis) are the following:
- When the hand is clenched into a fist, fingers I, II and partly III do not bend
- Bending the terminal phalanges of the thumb and index fingers is impossible, as is scratching the index finger on the table with the hand tightly adjacent to it.
- When testing the thumb, the patient cannot hold a strip of paper with a bent thumb and will hold it by adducting the straightened thumb with the adductor muscles from the stored
5169 0
Diagnosis of median nerve neuropathy
Classically, median nerve neuropathy can be diagnosed by a neurologist through a thorough neurological examination. To identify motor impairment, the patient is asked to perform a series of tests: clench all fingers into a fist (the 1st and 2nd fingers do not bend); scratch the surface of the table with the nail of your index finger; stretch a sheet of paper, grasping it only with the first two fingers of each hand; rotate your thumbs; connect the tips of the thumb and little finger.
In case of tunnel syndromes, Tinnel's symptom is determined - pain along the nerve when tapped at the site of compression. It can be used to diagnose the location of the lesion n. medianus. With pronator teres syndrome, Tinnel's symptom is determined by tapping in the area of the pronator snuff box (the upper third of the inner surface of the forearm), with carpal tunnel syndrome - by tapping on the radial edge of the inner surface of the wrist. With supracondylar process syndrome, pain occurs when the patient simultaneously extends and pronates the forearm while flexing the fingers.
To clarify the topic of the lesion and differentiate neuropathy n. medianus from brachial plexitis, vertebrogenic syndromes (radiculitis, disc herniation, spondyloarthrosis, osteochondrosis, cervical spondylosis), and polyneuropathy, electroneuromyography helps. In order to assess the condition of bone structures and joints, bone radiography, MRI, ultrasound or CT of the joints are performed. In supracondylar process syndrome, x-rays of the humerus reveal a “spur,” or bony process. Depending on the etiology of neuropathy, they take part in the diagnosis:
Especially when we are talking about complex pathologies that cannot be treated with conventional conservative methods - for example, compression of the nerve trunk due to postoperative complications. Then doctors resort to neurolysis of the sciatic nerve.
Determine the cause and eliminate it
If, during the consultation and initial examination, the doctor finds out that the patient previously suffered serious injuries to the lower part of the body, surgical operations were performed in the sacro-lumbar region or lower extremities, then most likely there is pinched nerve fiber:
- scar tissue;
- bone fragments;
- callus.
If we talk about scar tissue, it can appear as a result of:
- traumatic damage to tissue integrity;
- surgical interventions;
- deep burns, including chemical burns, etc.
If a person is admitted to the traumatology department with injuries to the lower part of the body and complains of acute pain that is clearly related to neurology, the doctor must check whether the nerve trunk is damaged and whether it is being compressed by bone fragments. Partial damage or stretching may also occur.
Neurolysis is a surgical operation, the meaning of which is to “free” the nerve trunk from the growths of connective tissue (scar tissue) or bone that are compressing it.
Neurolysis can be either a separate independent surgical operation or part of a treatment aimed at restoring the normal functioning of the body and the human musculoskeletal system.
This is very important, since pinching causes physical suffering to a person and makes changes in the functionality of the body. Due to severe pain and sensory impairment, the patient is unable to lead the same lifestyle as before the disease.
In addition, it significantly reduces a person’s performance, which affects his self-esteem and social status. The behavioral consequences of this disease are irritability and depression.
Neurolysis can be:
- external (external);
- internal (internal).
External neurolysis is prescribed in cases where scarring has occurred in the tissues surrounding the trunk of the sciatic nerve. Internal neurolysis is used when connective tissue growths penetrate the nerve trunk and are located between the bundles.
This is a very delicate and complex operation, but this is a treatment that needs to be carried out in a timely manner: with prolonged “suffocation” of the nerve trunk, complete paralysis of the limbs can occur. This is especially true in cases of bone impression.
Tumor and treatment methods
When they talk about neoplasms in nervous tissue, in most cases it is a neuroma - a benign tumor. The second name is schwannoma, named after the cells that make up the nerve sheath (Schwann cells).
Neuroma is a proliferation of the myelin sheath, a dense, rounded encapsulated formation. This disease can affect all nerves except the visual and olfactory ones.
In one out of five cases of detection of tumors in the sciatic nerve, a schwannoma is diagnosed.
The malignant form of neuroma is extremely rare. The main sign of a tumor transitioning from benign to cancer is the rapid growth of the tumor.
For comparison, with a benign nature, a neuroma can increase in size by a maximum of 2 mm per year. This is a clear sign of anaplasia (malignancy).
There is no drug treatment for this disease yet, although American doctors, during studies of the treatment of neuroma, found that taking acetylsalicylic acid slows tumor growth by almost half.
Neuroma symptoms:
- impaired sensitivity, up to complete absence;
- pins and needles feeling in the legs;
- decreased physical strength in the lower extremities;
- weakness.
Treatment methods:
- surgical;
- radiotherapy.
Contraindications to surgery to remove schwannoma are the patient’s advanced age (over 65 years), the presence of any pathologies, for example, cardiovascular, renal, etc.
The general serious condition of the patient also casts doubt on the advisability of surgical intervention.
The main indication for surgical removal of the tumor is large size (more than 5 cm).
Radiotherapy is used when the size of the neuroma is less than 5 cm. It is also indicated in cases where the tumor is located in a hard-to-reach place and when the patient has severe or chronic diseases.
Denial of responsibility
The information in the articles is for general information purposes only and should not be used for self-diagnosis of health problems or for therapeutic purposes. This article is not a substitute for medical advice from a doctor (neurologist, therapist). Please consult your doctor first to know the exact cause of your health problem.
I will be very grateful if you click on one of the buttons and share this material with your friends :)
5169 0
Partial nerve damage
In case of incomplete primary damage to the nerves and the incised nature of the wound, the ends of the damaged bundles almost do not diverge, since they are fixed in the correct position by the surviving trunk bundles and epineurium.
This allows the corresponding bundles to be identified and stitched without technical difficulties (Fig. 16.4.4). Rice. 16.4.4. Microsurgical suture for partial nerve damage (explanation in the text).
In case of old partial damage to the nerves, after their isolation from the tissues, the epineurium is peeled off in the areas of the nerve trunk adjacent to the lateral neuroma. Undamaged bundles are separated from damaged ones, the latter are refreshed, and the resulting defect is replaced with grafts (Fig. 16.4.5). A similar intervention can be carried out for primary injuries, if damaged fascicles require excision.
Rice. 16.4.5. Microsurgical plastic surgery of damaged nerve bundles with partial, old damage (explanation in the text).
It should be noted that for small marginal nerve defects, the ends of the damaged bundles can be brought together and sutured without tension. However, this creates the danger of a sharp bend and subsequent blocking of the remaining part of the nerve by scar tissue (Fig. 16.4.6, b).
Rice. 16.4.6. Scheme for preventing significant bending of the preserved part of the nerve when applying a suture to its damaged part (explanation in the text).
To prevent this from happening, the arc of curvature must be as flat as possible, which requires separation of the damaged and surviving parts of the nerve over a longer distance (Fig. 16.4.6, c).
To maximize the preservation of the intrastem vascular network in the preserved part of the nerve, it is advisable not to separate the part of the external epineurium adjacent to it. In general, the possibility of applying a lateral suture or the advisability of performing plastic surgery on the damaged part of the nerve is determined by the surgeon during the operation.
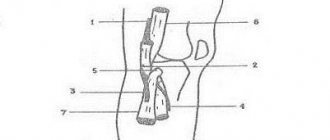
Carrying out the operation
The operation is carried out in several stages:
- Introduction of anesthesia.
- Opening the connective tissue with a scalpel along the entire length of the nerve.
- Detection of fiber bundles, excision of the scar between them.
- Access to the nerve is open, it is isolated from the surrounding tissues.
- The scarring area is determined by palpation. The scar is found and removed.
- Excision can be carried out only over the nerve, bypassing the sides, to avoid damage to blood vessels and other structures.
- Application of miniature sutures.
- Placement of the nerve into the resulting muscle space.
- After these manipulations, the tightness disappears, and previously lost sensitivity appears.