Ulnar nerve and its diseases: neuropathy, neuritis, tunnel syndrome and others
In the entire brachial weave, the ulnar nerve is given the most honorable place, since it, starting in the forearm, reaches the hand.
It is responsible for the mobility and sensitivity of the entire brachial plexus. But with neuralgic diseases, the functions of the ulnar nerve are impaired. Various lesions of the ulnar nerve (neuropathy, neuritis, tunnel and cubital syndromes) are quite common and can be associated with a number of different factors.
Ulnar nerve tunnel syndrome is a specific deviation that manifests itself in neuralgic diseases. The nerve is pinched in the area of the shoulder and forearm.
- pain syndrome;
- decreased sensitivity.
Treatment for carpal tunnel syndrome involves:
- restriction of physical activity;
- physiotherapy;
- taking vitamins and non-steroidal anti-inflammatory drugs.
If left untreated, damage to the ulnar nerve can lead to a decrease in sensitivity, and subsequently cause complete numbness of the hand.
- therapeutic exercises and other exercises aimed at developing the ulnar nerve;
- taking vitamins that help strengthen nerve endings.
The main causes of tunnel neuropathies are acute or chronic overstrain of the ligaments and muscles surrounding the nerve (professional, household, sports), trauma, prolonged stay in an uncomfortable position, prolonged work on the computer.
Hypothyroidism, diabetes mellitus, pregnancy, deforming osteoarthritis, rheumatoid arthritis, and nerve tumors contribute to nerve pinching. Women of menopausal age are more often affected.
Symptoms of tunnel neuropathies. A patient with carpal tunnel syndrome most often complains of painful numbness in the arms or legs, tingling, burning sensation, and crawling “goosebumps.” As a rule, numbness occurs at night, forcing you to get out of bed and shake and stretch the stiff limb.
The second symptom is pain of varying intensity at the site of pinching, spreading along the course of the nerve. A neurological examination reveals sensory disturbances. With a long course of the disease, weakness and muscle loss develop.
When you tap with a neurological hammer over the pinched nerve, pain and pins and needles spread along the nerve. Each nerve has its own diagnostic tests.
The most common tunnel neuropathies are:
- Anterior scalene syndrome;
- Inferior oblique capitis syndrome;
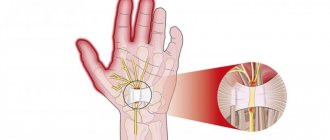
- Carpal tunnel syndrome;
- Ulnar nerve neuropathy at different levels;
- Radial nerve neuropathy;
- Roth's disease;
- Piriformis syndrome;
- Peroneal nerve neuropathy;
- Tarsal tunnel syndrome;
- Morton's neuralgia.
To confirm the diagnosis, you need to undergo ENMG (electroneuromyography) and ultrasound of the nerve. To exclude hypothyroidism, donate blood for TSH, to exclude diabetes mellitus, check blood glucose. MRI of the cervical spine is prescribed only if radiculopathy is suspected.
Treatment of carpal tunnel syndrome. People who have been treated for “osteochondrosis” in a clinic and even in a hospital for a long time and without success often turn to me for help. To eliminate pinched nerves, it is necessary to inject a drug with anti-inflammatory and anti-edematous effects directly into the tunnel.
In my medical practice, I often use therapeutic blockades with diprospan, lidocaine or novocaine, and movalis. Improvement with correct diagnosis and precise administration of the drug occurs after the first procedure. Usually 2-3 blockades are enough to eliminate pain and numbness in the arms or legs.
To restore nerve function, the following medications are indicated:
- Milgamma 2 ml intramuscularly No. 10;
- Thioctacid 600 mg intravenously drip No. 10 or orally 600 mg in the morning for 1 month;
- Neuromidin 20 mg 3 times a day for 1 month.
For tunnel syndromes, adequate and competent treatment gives quick and reliable results.
Anatomy
And again, you can’t do without anatomy.
The nerves originate from the brachial plexus, which is formed from the spinal nerves C5-Th1 (you need to know this to understand the symptoms and treatment of carpal tunnel syndrome). The brachial plexus is a very complex (see picture), but at the same time a very important formation.
There are others (musculocutaneous nerve, axillary), but they are less important to us.
In the picture we immediately see the most obvious weak point: the area of the elbow joint. Genetically, nature is designed in such a way that there are several “bottleneck” spots along the nerve. These are usually channels, “tunnels,” through which nerves pass. Therefore, pinched nerves in the canal are called tunnel syndrome. During inflammatory processes, compression of the nerve in the canal occurs with corresponding neurological symptoms.
As you can see, there are many tunnel syndromes. Many of them were described in the 19th and early 20th centuries, therefore they have romantic and poetic interesting names: “honeymoon paralysis”, “Saturday night paralysis syndrome”, etc. We will describe the most common tunnel syndromes.
For the ulnar nerve, this is entrapment in the cubital canal. This is what is called “cubital tunnel syndrome.”
The nerve passes near the internal epicondyle of the humerus, to which the tendons of several muscles are attached. These muscles are involved in the work of the hand. With excessive, prolonged movements of the hand, due to chronic trauma to the site of muscle attachment to the epicondyle, internal epicondylitis (inflammation) occurs, which also involves the ulnar nerve. The cubital canal becomes narrower, compressing the nerve.
Surgical treatment: decompression
How to treat ulnar nerve tunnel syndrome if conservative therapy does not give the desired effect? Unfortunately, sometimes it is simply impossible to do without surgery.
Quite often, so-called simple decompression is performed. The essence of the procedure is to cut the tendons and remove thickenings that pinch the nerve. This is a fairly simple operation, during which it is possible to preserve the blood supply to the nerve. And the restoration of the functions of the upper limb occurs quickly. The only disadvantages include the risk of re-exacerbation, although such cases are rarely recorded.
Anatomical and physiological certificate
It is impossible to understand what exactly caused the dysfunction of the ulnar nerve without the most basic knowledge of the anatomy of the human body, since only in this way can one obtain a complete picture of the course of the nerve fibers in the elbow.
The ulnar nerve is a long nerve located in the brachial plexus. It consists of biological fibers CVII-CVIII (7th and 8th cervical), which exit directly from the spinal cord.
On the arm itself, the nerve enters directly from the axillary fossa and moves to the intermuscular septum of the medial region in the middle of the shoulder and lies in the osteo-fibrous canal, which is formed inside the shoulder, tendon and wrist. This canal in the medical literature is called capital or Mouchet's canal.
It is in this place that the ulnar nerve is located almost on the very surface and as close as possible to the bones, and it is here that compression of the nerve fibers most often occurs.
As a rule, everyone who has injured their elbow at least once in their life, be it a fracture or a simple blow to a door handle, has felt quite unpleasant sensations that cause an immediate aggravation of the pain syndrome (also, the nerve can be pulsed in this place independently at any time and well feel it by touch).
After the fiber gradually leaves the limits of this channel, it ends up between the forearm muscles, but still part of its endings are in the muscle area. Moving to the border of the forearm, it is divided into several parts (external and dorsal), as well as into a small palmar branch, passing from the forearm to the palmar ligament and wrist. This part of the human body is responsible for the perception of the outside world - flexion and extension of the limb occurs.
Anatomical knowledge contributes to the fastest diagnosis of pathology.
Neuropathy is the most common disease of the ulnar nerve
Ulnar nerve neuropathy is a process of numbness and decreased sensitivity in the fingers and hand as a whole. The advanced stage of this disease leads to muscle atrophy, which can lead to complete numbness of the tips of the phalanges.
There are two types of ulnar neuropathy:
- Primary – the development of the inflammatory reaction does not depend on another pathological process occurring in the body. Most often, this condition is observed in people who rest their elbow for a long time on the working surface of a machine or table, the armrest of a chair, etc.
- Secondary (or symptomatic) is a complication of a disease that already exists in a person. The most common cause of the development of degenerative-dystrophic changes is compression (pinching) of the ulnar nerve, which is characteristic of certain diseases:
- osteomas – benign new formations of bone tissue;
- synovitis - inflammation of the synovial membrane;
- fractures and dislocations of the shoulder or forearm;
- bruised hand;
- tenosynovitis – inflammation of the inner joint membrane;
- deforming osteoarthrosis – a chronic disease of cartilage and joint tissues;
- bursitis of the elbow joint - inflammation of the joint capsule;
- post-traumatic arthrosis.
In some cases, neuropathy develops as a result of a severe acute infectious disease (typhoid or typhoid fever, tuberculosis, syphilis).
In general, damage to the ulnar nerve due to neuropathy is characterized by a violation of its basic functions, which leads to decreased mobility, pain, decreased sensitivity of a particular muscle group and general malaise. The cause of this condition may be damage that was caused to the fiber when a separate part of the elbow was compressed (this leads to pinching and damage to the nerve).
In addition, such damage can be either a separate or related disease.
Areas of numbness in ulnar nerve neuropathy
Symptoms of ulnar nerve neuropathy include the following:
- decreased sensitivity of the limb, which leads to the absence of pain;
- numbness of the limb, which deprives it of mobility.
With a broken elbow or other serious injuries, numbness and loss of sensation may occur simultaneously.
Establishing diagnosis
In order to establish damage to the ulnar nerve, a standard neurological examination is performed, during which the causes and nature of the disease are determined. The most informative method of damage diagnosis is electroneuromyography. It allows you to determine with maximum accuracy the location and extent of damage to the nerve fibers, as well as determine the level of damage to the nerve roots that form the elbow joint.
With modern patient care, diagnosing ulnar nerve damage is a quick and most accurate procedure.
Treatment of neuropathy consists of the following procedures:
- first of all, the patient is admitted to a hospital, since ulnar nerve neuropathy is a serious disease and without constant medical supervision the patient’s condition can only worsen;
- Painkillers are prescribed to reduce pain;
- An effective method of treating the disease is detoxification therapy, vitamins to maintain the body, non-steroidal anti-inflammatory drugs that reduce the inflammatory process.
Treatment
Inflammation of the ulnar nerve can be treated on an outpatient basis, since this disease does not require inpatient observation, with the exception of surgical intervention.
Treatment methods are as follows:
- conservative;
- surgical;
- folk
Conservative treatment involves the use of medications, which, in turn, include:
- anti-inflammatory drugs (glucocorticosteroids, diclofenac, ketorolac);
- painkillers (metamizole sodium, anesthetics);
- anticholinesterase drugs (ipidacrine, neostigmine);
- vasoactive drugs (nicotinic acid, pentoxifylline);
- metabolites (B vitamins, alpha lipolic acid).
The greatest effect is caused by injections of the above drugs, as the absorption of the active substance increases.
In addition, the doctor may prescribe a compress with dimexide and cold on the painful area.
At the acute stage, when the pain syndrome has just appeared, it is important to perform a motor blockade of the arm and elbow joint, especially at night.
The patient is recommended to have a fixing bandage, in most cases using a splint made from improvised materials (a needle or a strong stick).
In addition to drug treatment with tablets, physiotherapy is prescribed, which includes:
- UHF;
- phonophoresis;
- magnetotherapy.
An excellent way to eliminate the unpleasant consequences of inflammation (muscle atrophy) is massage and electrical myostimulation.
Surgical intervention (operation) is indicated in case of lack of effect from medications, the presence of a hematoma, tumor, and also in the case of the development of tunnel-type neuropathy.
Types of surgical intervention:
- nerve decompression;
- neurolysis;
- removal of adhesions;
- nerve transposition;
- tumor removal;
- scar removal;
- removal of hematoma.
Any operation, especially one performed on nerves, is performed under anesthesia. Pain relief can be performed using either general or local anesthesia.
Surgical option
Naturally, home remedies are used to treat ulnar nerve neuropathy, which in most cases are aimed at eliminating the pain symptom.
Before you start using traditional medicine, we strongly recommend that you consult your doctor for advice and obtain his permission to use a particular recipe.
Horse sorrel tincture:
Soak the roots of horse sorrel in vodka in a ratio of 1 to 1. Namely, half a jar of roots and half a liter of vodka are used for a liter jar. Infuse the root for at least 10 days and apply as a compress to the sore spot. The effect is enhanced if the compress is done at night.
Bay leaf ointment:
Mix 200 grams of vegetable oil and 4 tbsp. l. finely chopped bay leaf. Leave the ointment for a week. Rub the resulting product into the area that hurts until the pain stops.
Horseradish compress:
Horseradish is ground with raw potatoes in a ratio of 1 to 1 and 1 tbsp is added to the resulting mixture. l. honey The resulting mixture is wrapped in thick cloth and applied to the left or right hand, depending on the location of the pain syndrome, for an hour. Horseradish acts as an anesthetic, and potatoes compensate for its burning effect.
Hand rehabilitation exercises
Additionally, during the recovery stage, the patient is shown physical therapy exercises (PT), as well as classes on specialized equipment.
Symptoms
The origin of ulnar neuralgia can be different - somatic and infectious pathologies, trauma, prolonged compression.
The inflammatory process affects the fibers of the peripheral nerves and manifests itself:
- pain syndrome;
- numbness of the upper limb (impaired passage of nerve impulses to the brain);
- disruption of the functional activity of the arm muscles.
Treatment of neuralgia of the elbow joint is complex and consists of the use of medication and physiotherapeutic methods:
- using a plaster splint, the arm is fixed in a half-bent position and suspended in a special bandage - in this way, the cause that caused the neuralgia is most often eliminated;
- in case of an inflammatory reaction, antibacterial agents are prescribed, in case of an acute infectious disease - antiviral agents;
- to relieve swelling, it is necessary to take potassium-sparing diuretics;
- B vitamins are considered an effective means for improving cellular metabolism;
- Papaverine is strongly recommended to improve trophism and blood circulation in tissues;
- To maintain the physiological tension of nerve and muscle tissue, electrophoresis is prescribed. ampli-pulse and UHF;
- The patient can carry out massage sessions independently, starting with rubbing the fingertips, flexion and extension of the joints of the phalanges and hands.
They manifest themselves as burning pain in the hand area, paresthesia (decreased sensitivity), dysesthesia (perversion of sensitivity), or hyperesthesia (increased sensitivity) of the innervated fingers. The median nerve controls the first three fingers.
Diagnosis is also not particularly difficult. A carefully collected history and typical neurological picture help make the correct diagnosis.
In some cases, MRI of the wrist joint and electroneuromyography of the median nerve are used.
Characteristic symptoms
Depending on the severity of the nerve damage, different signs of neuritis may appear. Common symptoms are:
- Loss of sensitivity, tingling in the affected area, numbness, unresponsiveness to touch are the first signs of the disease. Or, conversely, acute pain may occur as a result of exposure to nerve impulses.
- Paralysis of the affected part of the body, immobilization or partial decrease in the motor function of the hand. There is a decrease in muscle strength; in the later stages, the muscles can completely atrophy, and tendon reflexes disappear. As a result, the palm may appear flat.
- Swelling near the lesion, bluish skin, increased hair loss, the appearance of pigmentation, increased sweating, fragility and separation of the nail plate.
- Decreased sensitivity in the palms and fingers. The joints on some fingers extend, while others bend, so the hand resembles a “clawed paw”.
If symptoms are detected, you should consult a doctor for a full diagnosis.
Diagnostics
When a patient consults a doctor with complaints about symptoms characteristic of ulnar nerve neuropathy, diagnostic measures are prescribed aimed at identifying the true factors that may affect not only the ulnar nerve, but also the radial nerve.
Testing a patient using the Froman method is quite effective for diagnosing neuropathy. In this case, patients are asked to perform several simple tasks:
- It is necessary to press the paper sheet firmly with your thumbs onto a flat surface. With a positive test for neuropathy, the patient constantly bends the thumb in the phalanx, and if necessary, it is almost impossible to straighten the finger.
- To confirm pinching of the ulnar nerve, the doctor applies several light blows to the cubital canal with the edge of the palm or fingers. When symptomatic signs intensify and become more pronounced, which is classified as Tinnel's sign, the presence of ulnar neuropathy is confirmed.
- Using light tingling and palpating of the hand, the degree of loss of sensitivity (paresthesia) is determined. The most common symptom of neuropathy is partial paresthesia.
Positive Tinnel's sign indicating ulnar nerve involvement
In all cases, patients are referred for instrumental diagnostics, which includes the following research methods:
- X-ray examination and MRI, necessary to determine various defects in the bone structure that cause the development of compression of nerve endings in the elbow or hand;
- Ultrasound is used to visualize changes in the structure of the nerve trunk (at the site of entry into the cubital or Guyon's canal);
- Electromyography (ENG) detects impulse conduction disturbances occurring below the compression area.
Electromyography allows the doctor to identify the location of the lesion in order to determine the activity of the ulnar nerve
In addition, the doctor can prescribe a number of laboratory tests (blood, urine, etc.) to more accurately determine the cause of the development of the pathological condition. After diagnostic measures, treatment procedures are prescribed, the purpose of which is to relieve negative symptoms as quickly as possible.
As a rule, it does not present any difficulties. A carefully collected history and typical neurological picture help make the correct diagnosis. In some cases, MRI of the elbow joint and electroneuromyography of the ulnar nerve are used.
Ulnar nerve neuropathy: features, symptoms and treatment
The ulnar nerve belongs to the peripheral system. Ulnar nerve neuropathy is a common disorder that occurs due to human habits and traumatic factors.
The ulnar nerve passes through the joint, which is considered the least protected area. Compression lesions in this area are almost as common as carpal tunnel syndrome, which is also sometimes called carpal tunnel syndrome.
Anatomy of nerve location
The ulnar nerve begins in the C7-C8 bundle, Th1, which is located in the medial part of the brachial plexus. The ulnar structure has no branches or small roots. It passes through the inside of the shoulder, gradually forming the back.
Important! In the area of the elbow joint, the nerve is located closest to the surface of the skin, and then passes into the cubital canal.
In the canal it is surrounded by ligaments and tendons, so protection against injury and compression in this area is increased. From the elbow to the wrist, the nerve runs along the inner edge of the forearm. At the head of the bone at the bottom of the wrist, an additional branch is formed on the back of the hand, then it goes deep into the palm and again divides into 2 branches.
When disturbed, the superficial branch leads to loss of sensitivity in the little finger and partially in the ring finger. The second branch takes over the functions of the sensory organ of the rest of the palmar ligament.
Classification of elbow neuropathy
There are several types of ulnar nerve neuropathy. The classification is based on an etiological basis, that is, on the causes of damage:
- post-traumatic neuropathy - appears due to rupture or severe stretching of the nerve;
- Compressive neuropathy - associated with nerve compression syndrome, this group includes Guyon's syndrome.
The latter group is more common and is associated with characteristics of professional activity and human diseases that affect the vulnerable area of the elbow.
Reasons for violation
The position of the ulnar nerve influences the causes of damage that lead to symptoms of neuropathy. Unlike the radial or median nerve, the ulnar nerve passes a few millimeters from the skin layer. Moreover, this area is constantly exposed to traumatic factors and pressure. The traumatic mechanism of neuropathy occurs under the following circumstances:
- dislocations, bruises of the arm and elbow area;
- fractures of various parts of the shoulder, wrist and forearm;
- wrist injuries, including sprains.
The second category of circumstances under which ulnar nerve neuropathy occurs is associated with compression-ischemic disorders due to diseases:
- deforming osteoarthritis, osteodystrophy;
- synovitis, bursitis, tendovaginitis;
- destruction of the myelin sheath of the nerve, characteristic of various sclerosis, encephalomyelitis and leukoencephalitis - the common name for such disorders is demyelinating;
- aneurysms located near joints;
- neoplasms leading to nerve compression;
- rheumatoid arthritis;
- enlarged lymph nodes.
Occupational habits and characteristics can cause neuropathy:
- the habit of leaning on your elbow when performing any task, or while talking on the phone;
- monotonous and monotonous work with tools with a fixed elbow position, including the use of a professional vibrating tool;
- prolonged stay under a drip – the patient’s arms are straightened, the nerve is in a state of compression;
- regularly riding a bicycle or motorcycle with tension in the elbow joints;
- resting on the elbows when working at a table, using tools, and also when driving a car.
In terms of frequency of occurrence, ulnar nerve neuropathy, caused by professional habits, occupies a leading place and can only compete with disorders such as arthrosis.
Symptoms of a neuropathic disorder
Peripheral nerve disease is caused by different causes, but the manifestations boil down to the same symptoms:
- muscle weakness appears and sensitivity in the area of the injured elbow decreases;
- the ulnar fossa begins to hurt, the discomfort spreads to the fingers and covers the area around the elbow;
- in patients with neuropathy, the little finger cannot move away from the other fingers even 10 degrees;
- as it develops, a symptom of “clawed paw” appears, when the fingers are twisted and it is difficult for a person to move the hand;
- numbness gradually develops and motor activity on the injured elbow decreases.
Guillain's syndrome is slightly different from classical neuropathy in that it has increased symptoms: the fingers hurt on the side of the palm, and paralysis of the little and ring fingers is possible. In some cases, paresis, swelling and numbness affect part of the middle finger.
The symptoms of the disease are sometimes confused with arthrosis, since they occur mainly in the morning, immediately after waking up. However, unlike arthrosis, the pain is stronger and does not go away after a short rest.
Methods for diagnosing pathology
Ulnar nerve neuropathy can be detected without complex and expensive examinations. First, the patient needs to contact a neurologist or therapist. Next, the doctor will conduct a diagnosis using the Froman method:
- You need to press the paper sheet against the table with your thumbs so that the rest of your palm is perpendicular to the surface. If there is neuropathy, the thumb will bend when pressure is applied, and it becomes impossible to straighten it.
- To confirm the pathology, you need to strike with the edge of your palm or your fingers in the place of the cubital canal. The pain will intensify in this case, as will the numbness or tingling sensation.
- By pinching and tingling, the doctor determines the degree of loss of sensitivity in the patient’s parts of the hand.
Of the instrumental examination methods, ultrasound is most often used to confirm the diagnosis. The device reflects changes in the structure of the trunk well.
Sometimes X-rays and MRIs are required to identify the causes of the disorder if they were not known in advance. If these methods fail to identify the factors of ulnar nerve neuropathy, electromyography is prescribed. Using this method, impulse conduction disturbances are determined.
It is not necessary to donate blood and urine for testing in all cases of diagnosing neuropathy. However, with their help it is possible to exclude infections and inflammatory processes, as well as some other diseases.
Treatment of the disease
It is necessary to begin treatment for ulnar nerve neuropathy after confirmation of the diagnosis. The doctor determines the therapy, taking into account the accompanying circumstances, symptoms and main causes of the disease.
In most cases, drug therapy is used, as well as traditional medicine.
In rare cases, for example, with severe injuries and mechanical clamping of the fiber, surgery is prescribed.
The objectives of therapy are reduced to solving one goal - restoring the conductivity of a nerve damaged by external factors. If it is ischemic, compression syndrome, then an integrated approach is required. In case of injuries and fractures, long-term fixation of the damaged structure is usually sufficient.
Drug treatment
Drug therapy for ulnar nerve neuropathy is mainly limited to eliminating pain. To do this, take drugs from the NSAID group: Nimesulide, Meloxicam, Ibuprofen, Diclofenac and products with similar active ingredients.
Diuretic drugs are also used if the patient has severe swelling. Be sure to use complex vitamins and injections with B vitamins - they have the best effect on the recovery process in diseases such as neuropathy.
Important! Neuromidin is a potent drug for restoring neuronal conductivity.
Antispasmodics are used if there is severe muscle hypertonicity and spasm that does not allow the limb to relax normally. In severe cases, they resort to lidocaine or novocaine blockade with the use of antibacterial substances or glucocorticosteroids.
Physiotherapeutic methods
This group includes therapeutic techniques that make ulnar nerve neuropathy go away faster. Physiotherapy relieves swelling, normalizes blood circulation, and helps with pain. Some methods help get rid of destructive and atrophic processes. Physiotherapy affects metabolism and increases the benefits of medications.
Important! Physiotherapeutic treatment can only be performed during the period of rehabilitation or remission; it is prohibited during the acute phases of the disease.
Acupuncture - acupressure - massage gives good results in restoring the pinched ulnar nerve. Additionally, doctors recommend taking courses of therapeutic exercises.
Acupuncture is also an acupuncture technique and is highly effective. Electrical discharges stimulate the nerve well and relieve spasms, so ulnar nerve neuropathy can be treated using electrophoresis and other methods using current.
Home treatment with traditional recipes
Any natural recipes can be taken only after consultation with the doctor. There are many effective folk remedies that have been used for many years for neuropathy:
- Orange peels . Decoction of 1 tsp. dried orange peels and 1 tsp. dry lemon balm perfectly relieves inflammation. Pour a glass of boiling water over the mixture and leave for 10 minutes. Then it is filtered, mixed with valerian tincture and taken a glass a day for a month, dividing the portion into 3-4 doses.
- Alcohol tinctures. They help relieve pain and are especially effective if ulnar nerve neuropathy is caused by compression. For tinctures you can use celandine, lilac and other medicinal herbs.
- Heat compresses. Heat can be used for treatment only if the neuropathy is not caused by an inflammatory process. Compresses are made from warm sand or cereal. You can use a heating pad filled with boiling water.
- White clay. Compresses of white clay mixed with water stimulate relaxation of the nerve and restore it.
You can do massage at home using unrefined natural oils: camphor, olive, turpentine.
In case of intense pain, doctors recommend immediately contacting a doctor rather than using traditional medicine. Often, when the pain is unbearable and other methods do not work, surgery is prescribed.
Surgery for neuropathy
Surgical intervention is required for advanced forms of the disease. To do this, they use the neurolysis method - it helps eliminate pinched nerves. The channel in which the fiber is located is also changed, or a new channel is formed. Additionally, dissection of the palmar ligament is required.
After the procedure, the patient undergoes rehabilitation: exercise therapy, massage and medication. The recovery period can last up to 6 months, since surgery in 90% of cases is prescribed for already neglected areas of the elbow.
Exercise therapy
Ulnar nerve neuropathy will not go away completely unless the patient engages in physical therapy. The complex can include special exercises for the arms and shoulder girdle:
- you need to work out the phalanges of all fingers, doing straightening and pressing exercises;
- you also need to warm up your elbow, making amplitude movements up and down;
- it is necessary to perform movements with the hand to restore all motor capabilities.
The doctor issues a referral to a physiotherapist or exercise therapy trainer, and the specialist selects the optimal set of exercises for the patient.
Inflammatory process in the elbow area
Ulnar nerve neuritis is an inflammation accompanied by constant pain in the elbow joint, numbness of the limb and weakness of the entire muscle.
Symptoms of ulnar nerve neuritis:
- burning sensation in the elbow area;
- swelling of the limb is pink-violet;
- weakness;
- change in body temperature;
- drooping of a limb when it is overexerted.
Treatment consists of the following set of procedures:
- First of all, the hand is fixed to prevent it from drooping. This is done using a compression bandage and, as a rule, the arm is completely immobilized.
- The next step of treatment is daily therapeutic exercises, taking anti-inflammatory and painkillers.
After some time, when hand mobility improves, the exercises will become more complex, gradually increasing the load.
Median nerve
- It is most often pinched in the carpal tunnel. It is called “carpal tunnel syndrome”, “carpal tunnel syndrome”. The channel is located, respectively, in the area of the wrist joint. Reasons:
- Chronic injury to the tendons in the area of the wrist joint in persons of certain professions (any profession associated with working at a computer, with a computer mouse: IT specialist, copywriter, designer, and many others)
Injuries: fractures of the radius and ulna in a typical location (the lower third of the forearm is considered a typical location).
- When the nerve passes through the muscle bundles of the pronator teres muscle: “pronator teres syndrome.”
Fractures of the radius and ulna in a typical location with displacement, as well as subsequent reduction and plaster application, are one of the most common causes of median nerve tunnel syndrome.
Ulnar nerve entrapment
Pinching of the ulnar nerve (cubital tunnel syndrome or ulnar nerve compression syndrome, ulnar syndrome) can lead to decreased sensitivity and complete loss of arm mobility.
Pinching is expressed by the following symptoms:
- numbness and decreased mobility of the limb;
- change in muscle mass in the arm;
- pain syndrome.
Treatment of cubital tunnel syndrome:
- adherence to a constant regimen (therapeutic exercises, reduction of physical activity, and so on);
- physiotherapy;
- taking painkillers.
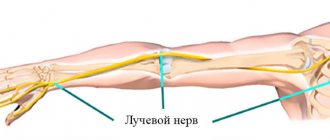
Radial nerve
Most often it is pinched in the spiral canal. The clinical picture is also typical: they manifest themselves as burning pain in the dorsum of the hand, paresthesia (decreased sensitivity), dysesthesia (perversion of sensitivity), or hyperesthesia (increased sensitivity) of the innervated area. The radial nerve is responsible for the back of the hand.
Diagnosis is not difficult. A carefully collected history, neurological examination and typical neurological picture help to make the correct diagnosis. In some cases, MRI of the elbow joint and upper third of the forearm, electroneuromyography of the radial nerve is used.
Diagnosis of cubital tunnel syndrome
When examining the elbow joint by a doctor, the patient may notice a significant increase in pain. A painful examination is necessary for a specialist to make an accurate diagnosis:
- If the nerve is compressed in the canal, there will be a positive Tinnel's sign, which is manifested by the sensation of a current shooting through the nerve into the little and ring fingers when the doctor taps with a neurological hammer - although this can happen when the nerve is without pathology, with a strong blow.
- The doctor will check to see if the nerve slips out of the canal when the patient bends the arm at the elbow.
- Tests sensitivity and strength in the hand and fingers.
If the doctor has doubts about the causes of cubital tunnel syndrome, the patient may be recommended to undergo additional examinations, such as MRI, ENMG, and radiography.
Radiography. Based on radiographs, it is possible to determine bone exostoses in the projection of the canal, which compress the nerve. But most of the causes of compression of the ulnar nerve cannot be seen on x-ray, since they are of soft tissue etiopathogenesis.
Electroneuromyography (ENMG). This study makes it possible to determine how well the impulses are transmitted along the nerve and to determine at what level and how much the nerve is compressed.
During nerve conduction testing, the nerve is stimulated proximally and the time required to conduct the impulse is measured and compared with normal values.
As a rule, it does not present any difficulties. A carefully collected history and typical neurological picture help make the correct diagnosis. In some cases, MRI of the elbow joint and electroneuromyography of the ulnar nerve are used.
Factors in the development of the disease
Existing factors that can lead to the development of neuropathy are conditionally divided into 2 groups:
- post-traumatic – in this case, inflammation of the nerve can be caused by rupture and tearing of ligaments, sprains caused by lateral dislocations, fractures and subluxations of the elbows;
- compression (Guyon's syndrome) - compression of nerve endings can be observed in various pathological processes, which are accompanied by swelling and changes in bone structures at the site of the nerve passage.
Compression of the cubital canal nerve is possible with long-term intravenous infusions, frequent flexion of the elbow joint and the habit of constantly leaning the arm on any surface (table, machine, open car window, etc.). Guyon's syndrome is possible when using a cane, driving bicycles and motorcycles, working with screwdrivers, hammers, drills, etc.
In addition to these factors, compression neuropathies quite often occur with rheumatoid arthritis, vascular aneurysm, tumor formations, deforming arthrosis and arthritis. The development of negative symptoms is possible with deformations of bone and connective tissue in the elbow after fractures, synovial cysts and thickening of the tendon sheath with the development of tenosynovitis, chondromalacia and chondromatosis.
Symptoms of neuropathy depend on the location of the lesion. With cubital tunnel syndrome there are:
- decreased sensitivity (paresthesia) in the ulnar edge of the hand, little finger and ring finger;
- pain in the area of the ulnar fossa, which gradually spreads to the forearm, little finger, ring finger and ulnar part of the hand;
- impaired motor activity, manifested by muscle weakness, difficulty flexing and abducting the hand, little finger and ring finger;
- muscle atrophy, characterized by a change in the appearance of the hand (“bird-like” or “clawed”).
Symptom of a “clawed” hand
The following symptoms are observed in Guyon's canal syndrome:
- paresthesia of the little finger and ring finger on the palm side and preservation of sensitivity on the back of the hand;
- the presence of pain symptoms and paresthesia in the little finger and ring finger from the palm, ulnar edge of the hand and wrist joint;
- just as with cubital syndrome, a “bird-like” or “clawed” hand is present.
Guyon syndrome is accompanied by weakness of the ring and little fingers when flexed. It is difficult to spread and close the fingers, and the thumb cannot be brought to the palm
What symptoms should you pay attention to?
They manifest themselves as burning pain in the hand area, paresthesia (decreased sensitivity), dysesthesia (perversion of sensitivity), or hyperesthesia (increased sensitivity) of the innervated fingers. The median nerve controls the first three fingers.
Diagnosis is also not particularly difficult. A carefully collected history and typical neurological picture help make the correct diagnosis.
In some cases, MRI of the wrist joint and electroneuromyography of the median nerve are used.
Cubital tunnel syndrome – also known as ulnar neuropathy, is caused by excess pressure on the ulnar nerve, which runs close to the surface of the skin at the elbow. You are more likely to develop cubital tunnel syndrome if you have the following factors:
- Repeated use of the elbow, especially on a hard surface.
- Keeping the elbow in a bent position for a long time, for example, while talking on a cell phone or sleeping with the arm bent at the elbow.
- Sometimes, cubital tunnel syndrome develops as a result of abnormal bone growth in the elbow or intense physical activity that increases pressure on the ulnar nerve. Baseball players, for example, have an increased risk of developing cubital tunnel syndrome because of the rotational motion required to hit the ball, which can lead to ulnar ligament damage and nerve injury.
Early symptoms of cubital tunnel syndrome include:
- Pain and numbness in the elbow.
- Tingling, especially in the ring and little fingers.
More severe symptoms of cubital tunnel syndrome include:
- Weakness in the ring and little fingers
- Decreased ability to flex fingers (thumb and little finger)
- Decreased hand strength
- Arm muscle atrophy
- Deformation of the hand
If any of these symptoms are present, your doctor may diagnose cubital tunnel syndrome based on a physical examination alone. In addition, it is possible to use special neurophysiological tests (such as EMG), which can determine the degree of conduction disturbance in a nerve fiber or muscle.
Radial tunnel syndrome is caused by increased pressure on the radial nerve, which runs in the bones and muscles of the forearm and elbow. Causes of radial tunnel syndrome include:
- Injury
- Benign tumors (lipomas)
- Bone tumors
- Inflammation of surrounding tissues
Symptoms of radial tunnel syndrome include:
- Sharp, burning or stabbing pain in the upper forearm or back of the hand, especially when trying to straighten the wrist and fingers.
- Unlike cubital tunnel syndrome and carpal tunnel syndrome, radial tunnel syndrome rarely causes numbness or tingling because the radial nerve primarily affects the muscles.
Just like with cubital tunnel syndrome, if any of these symptoms are present, your doctor may diagnose radial tunnel syndrome based on a physical examination alone. If necessary, electromyography may be prescribed to confirm the diagnosis, determine the level of damage and the degree of damage to the nerve fiber.
What are the symptoms of ulnar nerve tunnel syndrome? Symptoms and their severity directly depend on the degree of development of the disease. For example, in the initial stages, any disturbances in well-being may be completely absent. But as the space in the bone canal narrows, the symptoms become more pronounced. The clinical picture looks like this:
- periodically there is pain in the elbow, which intensifies after physical activity;
- some patients complain of numbness in the palms or fingers;
- when a joint or ligament is sprained, the pain increases (tapping on the affected area is also accompanied by discomfort);
- as the disease progresses, stiffness appears when moving in the affected joint;
- Gradually, the muscles in the area of the affected nerve begin to weaken and gradually atrophy.
It is worth noting that with such a pathology, pain can spread to the forearm, shoulder, shoulder blade and even the back, which often complicates the diagnostic process.
It is not necessary to have all the signs.
- Stiffness, loss of sensation, or significant dull or sharp pain in the ulnar part of the hand, 4th and 5th fingers.
- Pain and weakness when attempting to grasp an object with a brush.
- Discomfort in the elbow area.
Such symptoms indicate ischemia (lack of blood supply) of the nervous tissue. These symptoms are most pronounced in the morning, after the hand has been resting overnight. After some time, when the patient performs a certain amount of movements, the pain and numbness slightly recedes.
Classification
Neuropathy arising in the ulnar nerve is accompanied by decreased sensitivity and numbness of the hand and fingers. At an advanced stage, muscle atrophy may develop, which can cause complete numbness of the fingertips.
There are currently 2 types of ulnar neuropathy:
- primary - with this type of development, the inflammatory reaction occurs regardless of additional pathological processes developing in the patient’s body. The disease most often occurs in people who lean on their elbow for a long time when sitting, driving, or working;
- secondary (symptomatic) - occurs as a result of complications of diseases that are present in the human body. Most often, degenerative-dystrophic changes occur due to pinching (compression) of the ulnar nerve, which is present in some diseases.
You may also read: Treatment of cubital tunnel syndrome
These include:
- fractures, dislocations of the forearm and shoulder;
- hand bruises;
- synovitis (inflammation of the synovial membranes) and tendovaginitis (inflammation of the inner lining of the joint);
- osteomas (benign bone tumors);
- deforming osteoarthritis (a chronic process in articular and cartilage tissue);
- inflammation of the joint capsule (bursitis) and post-traumatic arthrosis.
It is extremely rare that acute infectious processes (tuberculosis, typhoid and typhus, syphilis, etc.) can cause the development of neuropathy.