A pinched nerve in the cervical spine is a pathological phenomenon that occurs due to compression of the nerve roots of the spinal cord. Incarceration can be caused by pressure from neighboring vertebrae, intervertebral discs, muscles, as well as pathological formations of various etiologies.
A pinched cervical nerve is called cervical radiculopathy. If the occipital nerve is pinched, then we are talking about occipital neuralgia. This condition is accompanied by quite pronounced pain - even greater intensity than when nerves are pinched in other parts. In addition, this pathology develops much more often, which is due to the peculiarities of human anatomy.
The problem of a pinched nerve in the cervical spine is not as harmless as it might immediately seem. In case of prolonged absence of proper treatment, the blood supply is seriously impaired, which can cause a number of complications: disturbances in the functioning of the brain, ischemic stroke, pathological changes in the facial muscles, etc. In the material we will understand the causes of the disease, the symptoms and treatment of this disease, its prevention .
Structure of the cervical spine
There are several terms that define this condition in different sources, and it is called cervical myelopathy or radiculopathy of the cervical spine. Moreover, if the latter pathology directly implies clamping of the nerve roots in the cervical region, then the first is spinal cord dysfunction, which manifests itself in the neck area.
With such diseases, the transmission of impulses in the problem area is disrupted.
The upper (cervical) spine consists of two segments that differ in structure:
- Atlant. Consists of two arches (lateral masses). The atlas fixes the skull to the spinal column.
- Axial. In front of this segment there is a growth that penetrates deep into the atlas and acts as the axis of rotation of the skull.
In the cervical spine, blood vessels and nerve fibers pass through the corresponding openings, connecting the spinal cord and brain. The cervical nerve plexus provides innervation to local muscles and skin and consists of the following elements:
- Motor branches. Provide innervation to the muscles of the neck and sublingual area.
- Sensitive branches. They run to the occipital zone and innervate this area along with the subclavian region. This branch includes the lesser and greater occipital, supraclavicular and transverse cervical nerves.
- Mixed branches. They include the phrenic nerve (it is the largest nerve of the cervical plexus), which innervates the region of the same name and passes through the lungs and pericardium. Some of these fibers affect the liver capsule.
The latter circumstance explains the reason for the occurrence of painful sensations in the area of the right hypochondrium when pressing on the area where the affected cervical nerve is located.
Depending on the location of the compression, there are two types of pinching:
- occipital neuralgia;
- radiculopathy.
Occipital neuralgia is diagnosed when the sensory branch is compressed (more precisely, when the small and large occipital nerves are pinched). Basically, the symptoms of such a lesion are localized on one side. In addition to the back of the head, painful sensations appear in the cervical region.
Radiculopathy is diagnosed when other nerve fibers are pinched. This condition causes spasm of muscle tissue, which negatively affects neck movements.
Any pinched nerve fibers require appropriate and timely treatment.
Without treatment, neuralgia transforms into neuropathy, which is characterized by almost constant headaches and neck pain. Also, due to compression of local tissues, the volume of blood flowing to the brain decreases. In the future, such lesions cause dysfunction of various internal organs.
Medicines
Regardless of the selection of a specific treatment method, pain relief is considered the number one problem. For this purpose the following is prescribed:
- Non-steroidal anti-inflammatory drugs: Nurofen, Naproxen. They can be purchased without a prescription. The substances remove suppuration and exhibit an analgesic effect.
- Strong analgesics - their purpose is rational only when absolutely necessary. Such medications can only be used under continuous medical supervision, as they have every chance of causing drug addiction.
- Muscle relaxants. To treat pinched nerves, the main muscle relaxants are used: Baclofen, Tizanidine, Cyclobenzaprine, Methocarbamol. As a rule, they are not used for a long period, since such substances have a bad effect on other body systems. The peculiarity of the action is the contraction of muscles and relaxation of muscle fibers, as a result of which compressed nerve roots are released and pain is alleviated.
- Medicines to maintain blood vessels, improve blood circulation and metabolic actions. The resumption of normal blood flow and metabolism in the affected area helps to eliminate degenerative phenomena and, as a result, activate the restoration of damaged nerve fibers.
- Corticosteroids. Their use is a rather radical measure. Substances in this category have every chance of causing significant side effects, for this reason hormonal resources are used only when other medications are ineffective.
Causes of pinching
Cervical plexus neuropathy develops under the influence of a whole complex of factors. The risk group for such a disorder includes persons with the following deviations:
- osteochondrosis;
- vertebral protrusion;
- osteoporosis;
- intervertebral hernia;
- tumors of various etiologies localized in the back;
- connective tissue hypertrophy;
- destruction of the intervertebral disc.
Cervical injuries (fractures, dislocations) can lead to neuropathy. However, the described list of factors is incomplete. Inflammation of the nerve in the cervical spine can be caused by various pathologies occurring in other parts of the body:
- tumor processes;
- infectious diseases;
- dysfunction of the endocrine system.
Among the possible causes of neuralgia are spasms of the neck muscles, which are often disturbing when:
- sedentary lifestyle;
- physical overload;
- weak muscular system.
Psychosomatics has a certain influence on the likelihood of a pinched nerve in the cervical spine. That is, the risks of developing neuralgia in the neck due to nervous strain cannot be ruled out.
As a person grows older, due to the natural processes of aging, the chances of developing such pathologies increase. This is due to a decrease in the concentration of mineral elements in the body, which leads to the gradual destruction of bone tissue and displacement of the vertebrae. However, regular physical activity significantly reduces the risk of developing the disease, even in older people.
In addition to the described reasons, neuralgia is caused by difficult childbirth, during which the child’s neck is bent at an unnatural angle.
What is a pinched nerve in the neck?
A pinched nerve occurs when a nerve root protruding from the spinal cord is compressed or pinched. Nerve root entrapment can occur for many reasons. In young people, the disease can appear as a result of injury and, as a result, the appearance of a herniated disc. In adults, radiculopathy, as a rule, appears suddenly as a result of osteochondrosis or a decrease in the height of the intervertebral discs in the cervical region of the ridge.
The cervical spine consists of seven cervical vertebrae (bones that create the cervical center of the spine). Any pair of vertebrae is separated from each other by an intervertebral disc. It functions as a hydraulic friction shock absorber. The spinal cord passes through a canal founded by the cervical vertebrae. Spinal nerve roots extend from the spinal cord and branch out to specific areas of the arm. The spinal nerves send movement signals to the muscles and also ensure the transmission of perceptual information. The spinal cord is like the trunk of a log, and the spinal nerves are like branches. If infringement or improper influence occurs close to the trunk, then everything located along the branch will be affected.
Symptoms
With cervical neuritis, the symptoms are varied, which is due to the structural features of the nerve plexus in this area. Also, the features of the clinical picture are determined by the localization of the pathological process.
The most characteristic symptom of a pinched nerve in the cervical spine is pain, which radiates to:
- parietal and temporal areas of the head;
- shoulder;
- hand;
- under the shoulder blade.
Symptoms of neuralgia of the cervical spine manifest themselves in the form of burning, paroxysmal, shooting pains and drug treatment is required to reduce or eliminate their intensity.
In addition to pain, the following symptoms are distinguished:
- numbness and tingling in the hands, fingers, neck and back of the head;
- frequent dizziness that occurs after a person gets up;
- increased fatigue;
- weakening of cognitive abilities (impaired concentration, memory impairment);
- sudden surges in pressure;
- frequent tinnitus;
- “flies” before the eyes;
- stiffness of neck movement due to overstrain of local muscles.
If the nerve is significantly pinched, signs of the disease may appear as:
- speech disorders;
- inability to swallow food;
- numbness of the tongue;
- swelling of the mucous membranes of the mouth;
- paresis and paralysis of the upper limbs.
Depending on the location of the pathological process, the following symptoms of radiculopathy are noted:
- 1-2 vertebrae. Pain in the head (back of the head, temple) and neck, memory impairment, increased irritability, constant fatigue, insomnia.
- 2-3 vertebrae. Pain in similar areas, decreased quality of vision and hearing, partial numbness of the mucous membrane of the larynx and mouth. Occasional fainting may occur due to insufficient blood supply.
- 3-4 vertebrae. Shooting pains that extend into the jaw in case of damage to the trigeminal nerve. With severe pinching, paresis of the hyoid muscles is observed, which impairs speech.
- 4-5 vertebrae. The pain radiating to the collarbone and forearm is aching in nature. With this localization, neck mobility decreases and sometimes problems with hearing and breathing occur.
- 5-6 vertebrae. The pain is localized in the back of the head and shoulders.
- 6-7 vertebrae. Painful sensations spread from the neck to the fingers. Tingling is noted in these areas, and numbness is localized in the area of the collarbone and shoulder blades. The muscles in these areas become hard. When palpating the affected area, the pain syndrome intensifies.
If the compression is located in the area where the cervical spine passes into the thoracic spine, a violation of fine motor skills of the hands is possible.
The remaining symptoms with this localization do not differ from those given above.
Cervical radiculopathy manifests itself in the form of pain and tingling in these areas. Symptoms with such a lesion in most patients are localized on one side. The intensity of painful sensations increases during movement.
With occipital neuralgia, the symptoms are localized in the zone of the same name. The pain in this case is sharp, similar to hammer blows. Each attack lasts no more than two minutes. Less commonly, occipital neuralgia manifests itself as a decrease in sensitivity in the specified area.
When the vagus nerve is pinched in the cervical spine, symptoms characteristic of pathologies of internal organs are added to the general clinical picture. Such disorders require a comprehensive diagnosis of the whole organism.
How to treat cervical neuralgia?
Due to the fact that compression of the fibers is caused by a whole complex of factors, a doctor must determine methods of treating a pinched cervical nerve. In this case, the procedure depends on the nature of the lesion and the intensity of the manifestation of painful sensations.
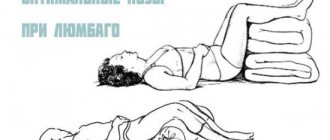
If cervical syndrome occurs unexpectedly, the patient needs to take a pain reliever (anti-inflammatory non-steroidal drugs are usually recommended) and lie down on a hard surface. The doctor develops further treatment tactics.
Before examining it, it is not recommended to massage or otherwise apply pressure to the problem area. This is explained by the fact that a number of pathologies that provoke neuralgia, with such manipulations, provoke a deterioration in the patient’s condition.
Drug treatment
Before treating cervical osteochondrosis, pinched nerves and neuralgia, you should limit the mobility of the problem area. For this, a special corset is installed.
As part of drug treatment for neuralgia, both local and systemic drugs are used. Injections for a pinched nerve in the cervical region are indicated if intense pain is bothering you, and ointments are indicated if the course of neuralgia is not accompanied by intense symptoms and the disease is not caused by tumors.
Within this approach, Ketorol is mainly used, which quickly relieves pain. To achieve a similar effect, you can use propolis-based ointments.
If the nerves of the neck are severely pinched, the following painkillers are recommended:
- "Ketoprofen";
- "Diclofenac";
- "Naproxen."
These drugs are potent, so the dosage of medications should be calculated by a doctor.
If the disease causes unbearable pain, injections of anti-inflammatory drugs are used. Also, depending on the development characteristics and causes of neuralgia, the following tablets are prescribed for pinching in:
- diuretics;
- means that restore metabolism;
- muscle relaxants;
- analgesics;
- chondroprotectors;
- corticosteroids;
- antioxidants.
Drug therapy for neuralgia due to osteochondrosis is supplemented with ointments and warm compresses.
Drugs for pinched nerves in the cervical spine must be selected taking into account the causes of the disease. In some cases, the treatment regimen includes venotonics, antiplatelet agents, steroids and vasodilators.
Gymnastics
It is quite difficult to immediately determine what to do if your neck is pinched. Appropriate medications help relieve pain. But the effect of the drugs is temporary. A set of exercises helps to restore the patient’s condition for a long time.
Exercise therapy, like drug therapy, is developed taking into account the characteristics of the causative factor. In particular, it is prohibited to perform a set of exercises in case of pinched nerves in the cervical spine during an exacerbation of osteochondrosis and in some other pathologies.
Basically, classes for such disorders involve tilting the head back and forth and to the sides. These exercises help increase blood circulation in the problem area, thereby relieving pain and eliminating muscle spasms.
A similar effect can be achieved through massage for a pinched neck. To do this, it is enough to press for several minutes on special points located at the site of pain. Self-massage is allowed after consultation with a doctor, since this approach is used exclusively for swelling and muscle spasms.
Treatment at home
For cervical neuralgia, treatment with folk remedies is not recommended. Such therapy is dangerous because it does not eliminate the causes of the pathology. And if symptoms of a pinched nerve in the cervical spine occur, treatment at home may cause the patient’s condition to worsen.
Traditional medicine can be used as an addition to traditional drug therapy. In this case, treatment of a pinched nerve at home is carried out with the direct participation of a doctor. The doctor must give permission to use traditional medicine.
To improve the patient’s condition when the cervical nerve is pinched, the following help:
- Horseradish leaves. The plant is first treated with boiling water, after which it is applied to the problem area overnight. The leaves must be covered with warm material.
- Mountain wax. It must first be melted and placed at the bottom of the vessel. The resulting piece of wax is also applied overnight to the area where the pain is located.
- Extract from marsh cinquefoil. Rub the product onto your neck and then cover it with warm material.
- Fresh cottage cheese with a little vinegar. Used as a compress.
Neuralgia of the neck cannot be treated at home. The described remedies for the symptoms of the disease help to relieve or reduce the intensity of the pain syndrome.
Diagnostics
The first diagnostic step is to visit a neurologist. During the consultation, the doctor will ask in detail about the time of onset, nature, localization of pain, and conduct a neurological examination. In order to clarify the diagnosis, they may be sent for auxiliary studies. For example, magnetic resonance imaging (MRI) or electromyography (EMG). MRI images clearly show soft matter, including the spinal cord and nerve endings. This study can help determine what causes nerve impingement, including protrusion and herniated discs. EMG measures the activity of nerves and muscles. This study may help determine how well the spinal nerves provide signals to the muscles.
Prevention
It is impossible to completely exclude the possibility of a pinched nerve in the cervical vertebrae. This is explained by the fact that this type of neuralgia develops for many reasons. The following recommendations help reduce the risk of damage to nerve endings in the cervical spine:
- maintain normal weight;
- to live an active lifestyle;
- avoid physical overload;
- organize your workplace correctly.
To avoid pinching a child’s cervical nerve, it is necessary to constantly monitor his correct posture.
Older people are advised to regularly exercise to prevent muscle spasms in the neck. In addition, it is important to promptly treat inflammatory diseases in the body, and if frequent headaches occur, consult a doctor.
What complications can there be?
If the cervical nerve is pinched, a person begins to experience frequent and often prolonged headaches, which reduce productivity and deteriorate cognitive function. Over time, this syndrome affects the mental state.
When a nerve is pinched in the neck, the volume of blood flowing to the brain decreases, which leads to frequent dizziness, which usually occurs when suddenly changing positions. In the future, due to insufficient blood supply, ischemic stroke and inflammation of the trigeminal nerve may occur. The latter leads to facial paresis and the development of central nervous system pathologies.