This is a short article. But I think that those who are interested should know what kind of brain tumors there are and how they differ from each other. Therefore, I present to you the most complete classification of brain tumors. Knowledge of the classification is very important for diagnosis and determining treatment tactics. The classification of tumors is based on the location and histological type of the tumor.
Types of brain tumors
Among malignant neoplasms, glioblastomas and medulloblastomas are distinguished. Glioblastoma is one of the most common types. Typically, it affects people between 40 and 60 years of age. The tumor does not have definite boundaries with tissues, so it can develop secondary changes. Among them are the formation of cysts, necrosis and hemorrhages. Metastases are found only in the brain, but the lesion develops quickly. This can lead to death of the patient within 3 months. Medulloblastoma is a malignant brain tumor because it is formed from immature medulloblast cells. The main reason for the formation of this pathology is dysgenetic processes. In other words, the embryonic rudiments are displaced during the prenatal period. At the same time, immature embryonic cells remain in the brain tissue. Therefore, medulloblastoma is often diagnosed in children. The lesion is mainly localized in the cerebellar vermis.
Along with the above, high-grade neoplasias are distinguished. They are characterized by low sensitivity to radiation, chemotherapy and even surgical removal. In this regard, the prognosis when this disease is detected is always poor.
Forms
As we have already said, the symptoms of cavernous angioma largely depend on the location of the vascular formation and its size. Manifestations of the disease occur when a bundle of blood vessels begins to put pressure on surrounding tissues and nerve endings in certain areas of the brain.
- Cavernous angioma of the frontal lobe, in addition to standard symptoms, may be accompanied by disorders of self-regulation of mental activity. The fact is that the frontal areas of the brain are responsible for motivation, setting and realizing goals, controlling one’s actions and evaluating results. Patients' memory deteriorates, handwriting changes, and uncontrolled unnecessary movements of the limbs appear. Cavernous angioma of the left frontal lobe gives a symptom such as a violation of speech regulation: a person’s vocabulary becomes poor, he forgets words, and speaks extremely reluctantly; There is apathy and there is no initiative.
- Cavernous angioma of the right frontal lobe, on the contrary, is characterized by excessive speech activity. The patient may periodically enter a state of passion, he becomes emotional and sometimes even inadequate. The patient's mood is largely positive - often he is not aware of the onset of his illness.
Cavernous angioma of the right temporal lobe can manifest itself with the following symptoms:
- the patient ceases to determine the identity of sounds and cannot find out the origin of a particular noise. The same goes for voices: a previously familiar voice may seem foreign.
Cavernous angioma of the parietal lobe is often characterized by so-called intellectual disorders. The patient loses the ability to solve simple mathematical problems, forgets the basic rules of division, multiplication, subtraction and addition. Logic and the ability to think technically are lost.
Cavernous angioma of the cerebellum sometimes occurs with pronounced symptoms - uncertainty in gait and even sitting, inadequate positions of the head and body (strange bends, postures). Violation of speech function, nystagmus, convulsions, contractures are noticeable.
- Thrombotic cavernous angioma is usually caused by an infectious disease that spreads mainly from the sinuses and nasal cavity. Symptoms include increased body temperature, weakness, hyperhidrosis, and fever. All this occurs simultaneously with the standard signs of angioma, depending on the location of the vascular formation.
There is another type of angiomas that often raises questions among patients - this is a cavernous angioma with an abundance of hemosiderophages. What is it about?
Hemosiderophages are specific macrophage cells that contain hemosiderin, an iron-containing pigment. The presence of these cells means that the resorption process is occurring in the pathological focus: siderophages appear 3-4 days from the beginning of the process and are destroyed approximately on the 17-18 day. Resorption is the resorption of the decaying erythrocyte mass, in which macrophages take an active part. Based on the degree of maturity of hemosiderophages, one can determine how long ago the inflammatory lesion appeared in the angioma.
What is the medical name for brain cancer?
This area of science characterizes this disease as a malignant formation that occurs in various membranes and formations of the brain. Among all registered tumors, this cancer accounts for about 1.5%.
To date, the exact causes of brain cancer have not been identified. However, some factors have been identified that can become a mechanism for triggering this oncology.
Among them are the following:
- Genetic diseases;
- Treatment using radiation therapy;
- The influence of viruses;
- Negative influence of mobile phones;
- Presence of tumors in other parts of the body;
- Harmful working conditions;
- Head injury;
- Smoking.
Gliomas
The group of gliomas is represented by various pathologies; they are the most common space-occupying formations of the corpus callosum of the brain. They are diagnosed in 80% of cases. Gliomas are classified according to their level of malignancy, and therefore the prognosis and clinical picture may vary. The most common type of glioma is glioblastoma. Also distinguished:
- Oligodendrogliomas. This pathology is very rare; in this case, a neoplasm is formed from protective elements that also support the process of hemostasis in the brain. The peculiarity of such space-occupying formations of the brain stem is that most often they form in middle-aged patients. Such neoplasms are moderately malignant.
- Astrocytomas. This neoplasm is diagnosed in 3/5 cases of brain cancer. Astrocytomas are formed from cells that separate neurons from vessels. These cells (astrocytes) are involved in the nutrition and natural development of nervous tissue. Astrocytomas are differentiated based on the degree of malignancy.
- Ependymomas. They are formations formed by the cells of the inner layer of the cerebral ventricles. These cells take part in the process of cerebrospinal fluid production, and therefore the symptoms of ependymoma are associated with a violation of this particular function. Ependymomas are classified into malignant and high-grade.
- Mixed gliomas. This type of tumor is formed from several types of tissue that are normally present in the brain.
A mass formation in the parietal lobe of the brain may appear suddenly. Neurological symptoms when the tumor is localized in this area manifests itself in disturbances in the sensitivity of the torso on the side opposite to the lesion. Disorientation in parts of one's own body and opto-aphasic disorders are noted.
Ocular pathology occurs only with large tumor volumes and manifests itself in less than half of patients. A characteristic feature is the occurrence of partial inferior quadrant homonymous hemianopia as a result of damage to the upper part of the Graziole bundle, the nerve fibers of which pass in this lobe. Subsequently, when the process spreads to the occipital lobe, complete homonymous hemianopsia develops.
Symptoms
Many tumors develop asymptomatically, so they are detected only as a result of an autopsy. There are focal and cerebral signs of cancer development. They have similar symptoms, which can appear as a result of pressure from a malignant tumor on the brain.
Among the main symptoms of this cancer are the following:
- Permanent headache that gets worse when sneezing, bending or coughing;
- Dizziness;
- Vomiting and nausea;
- Constant weakness;
- Increased intracranial pressure;
- Visual and hearing impairment;
- Speech impairment;
- Indifference;
- Difficulty moving;
- Confusion;
- Hallucinations.
The headache is bursting in nature and can appear in the morning or at night. May disappear if the person assumes an upright position. Pain syndrome cannot be eliminated with painkillers. Brain tumor size
Symptoms such as nausea and vomiting are completely unrelated to food intake. They constantly accompany headaches. The vomiting reaction is not associated with food poisoning. Due to an acute headache, a person may become lethargic and drowsy. The patient is completely lost in space and does not understand where he is and who surrounds him. If the tumor is located in the motor cortex, paresis or complete immobility may develop. Paralysis occurs only on one half of the body.
If it is localized in the temples, then a person may experience auditory hallucinations. If the formation is located in the back of the head, then the hallucinations are visual in nature. The patient loses the ability to understand written text. There is a significant difference in the reaction of the pupils to light. Asymmetry of individual parts of the face and its parts is possible. The patient feels a lack of coordination, as there is staggering in a standing position and when walking. The person may become aggressive and lose control of their emotions. The pain sensitivity of certain parts of the body is completely or partially impaired. When formed in the pituitary gland, hormonal disorders occur.
Differential diagnosis
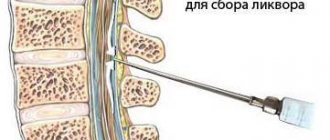
Differential diagnosis, as a rule, is carried out with other tumors or with an aneurysm - if a rupture is suspected, the patient is prescribed a cerebrospinal fluid examination in the hospital. The analysis will detect traces of bleeding or hemorrhage in it. This procedure can only be performed in a hospital setting.
Additionally, examinations and consultations with other specialists, such as a vascular surgeon, neurosurgeon, neurologist, geneticist, etc., may be prescribed.
Stages of tumor development
The following stages of disease development are distinguished.
- The neoplasm is located on the surface, so its components maintain their vital functions and do not spread. It is almost impossible to detect the disease at this stage.
- Progression of mutation. The neoplasm penetrates neighboring structures and affects the lymphatic vessels. Dizziness and headache appear. Visual disturbances and vomiting may occur. Metastases pass to the liver, lungs and cause their damage. Epileptic seizures may occur.
Classification
Depending on the type of cells, there are 3 types of tumors:
- giant cell glioblastoma, when the neoplasm includes large cells containing two or more nuclei;
- glioblastoma multiforme, the tissue of which includes overgrown blood vessels, foci of necrosis, etc.;
- gliosarcoma, consisting of glia (auxiliary cells of nervous tissue) and connective tissue cells.
The difference in the location of the tumor allows us to distinguish the following types:
- cerebral (the tumor is located in the temporal, frontal or other areas of the brain);
- stem, when the tumor is located in the brain stem (the tumor is inoperable, since surgical intervention leads to disruption of the musculoskeletal system).
According to histological classification, there are 3 types of glioblastoma:
- isomorphic cellular, when the tumor consists of cells of the same type;
- multiform, in which the neoplasm consists of cells of different types;
- polymorphocellular (glioblastoma cells of different sizes and shapes).
Another basis for classification is the number of malignant cells of the neoplasm. In accordance with this, there are 4 stages of glioblastoma.
- The first stage is transitional. Diagnosis is impossible due to the complete absence of manifestations. Only a portion of benign cells develop into cancerous ones.
- The second stage is slow cell growth.
- The third stage is the development of a malignant tumor. Rapid growth of atypical cells occurs.
- The fourth stage is the manifestation of a vivid clinical picture. Stage 4 glioblastoma is most often diagnosed. The patient's life expectancy after diagnosis is several months.
Types of glioblastoma
There are 4 main types of glioblastoma depending on the cells predominant in the tumor tissue. Each type has a specific pathology and degree of malignancy.
- Multiform pathology
This type of glioblastoma is distinguished by the species diversity of cancer cells. The basis for the development of neoplasms is glia, which is the connective tissue of a network of neurons. The trigger for degeneration is the impact of unfavorable factors.
Active growth of atypical cells contributes to the spread of cancer to other parts of the nervous system (for example, with the subsequent development of glioblastoma of the spinal cord). Treatment of multiform pathology has certain difficulties. They are due to the fact that each type of cancer cell is susceptible to different methods of therapy and has different rates of growth and development. Multifocal glioblastoma is considered the most dangerous.
- Giant cell form
During the study of the material, large pathological cells are revealed. They include multiple cores. The disease is considered less dangerous.
- Gliosarcoma
The neoplasm is characterized by bidermality. The tumor is a mixture of glial cells and connective tissue cells. Gliosarcoma is difficult to treat.
- Polymorphic cell form
Atypical cells are large and vary in shape. The examination reveals a small amount of cytoplasm. The kernels have different structures and sizes. Polymorphic cell glioblastoma is more common than other types.
Diagnostics
A neurologist may order an examination if cancer is suspected. First, the doctor evaluates reflexes and vestibular functions. Only after this does he refer the patient to related specialists. They conduct electroencephalography, which allows you to determine the focus and degree of activity of the formation. The doctor will also make a diagnosis and identify the exact location. To do this, MRI, computed tomography and magnetic resonance angiography are performed. The latter method provides effective examination of the vessels that feed the tumor. To do this, a contrast agent is injected into the bloodstream. In order to draw up a treatment plan and prognosis for the future, a biopsy is used.
It is performed after constructing a three-dimensional model of the formation itself. Other methods are also used that make it possible to accurately determine the stage of development of the disease. To do this, instrumental diagnostics of the organs in which the tumor is located is carried out. The main treatment for brain cancer is surgery. Its implementation is possible only if there are boundaries between neoplasms. If the formation has spread to the meninges, then the operation cannot be performed. However, if it puts pressure on important areas of the brain, emergency surgery is performed. In this case, not all tumors are removed, but only parts. Removal occurs using a scalpel, laser or ultrasound. In order to reduce the number of infected cells, radiation therapy is performed. It is also prescribed for incomplete tumor removal or in the presence of metastases.
It is prescribed after 3 weeks from the date of surgery. Radiation therapy can be combined with chemotherapy. Its task is to stop the activity of tumor cells. If it is impossible to remove using the above methods, then the person’s condition is improved with the help of radiotherapy. If a secondary appearance of the disease occurs, then remote irradiation of the head is performed. At the same time, the patient's hair falls out. But after a few weeks, they grow back. Targeted therapy uses drugs that block the growth of blood vessels. If the tumor is localized deep in important areas of the brain, then cryosurgery is prescribed.
Diagnosis of cavernous angioma
Treatment of cavernoma should always begin with a full diagnosis, the scheme of which doctors determine individually for each patient. General diagnostic techniques may include the following types of studies:
- Detailed blood tests (for the presence of an inflammatory process, anemia), as well as cerebrospinal fluid tests (for the presence of hemorrhages in the cerebrospinal fluid).
Instrumental diagnostics:
- angiography method - x-ray examination of blood vessels using contrast fluid. The resulting image will help detect the degree of narrowing or destruction of brain vessels, identifying changes in the vascular wall and identifying weak points. This diagnostic procedure is prescribed to determine circulatory disorders in the brain. It allows you to clearly determine the location, volume and shape of the angioma, as well as detect the damaged vessel. Diagnostics are carried out in a specially equipped room. First, the doctor administers local anesthesia, after which he inserts an elastic catheter into the vessel and moves it to the affected area. The contrast agent introduced into the circulatory system disperses through the vascular network, after which the doctor takes several photographs, which subsequently establish the diagnosis;
- The computed tomography method is a very popular painless procedure that does not cause discomfort, and at the same time is quite informative. It is usually performed either with or without the use of a contrast agent. As a result, the doctor receives detailed layer-by-layer X-ray images in the form of two-dimensional images, which allows a detailed examination of the pathology. The procedure is carried out only in special rooms with the appropriate equipment - a tomograph;
- The magnetic resonance imaging technique is somewhat reminiscent of computed tomography, but instead of X-rays, it uses radio waves and magnetic radiation. The images are detailed and three-dimensional. The procedure is non-invasive, provides comprehensive information about the disease, but is relatively expensive;
- The electroencephalography method allows you to study the biological potentials of the brain, as well as determine where the angioma is located and what its size is. If a tumor is present, the doctor detects a change in the signal sent to the brain structures.
Types of brain tumors in adults
Generally, the prevalence of cancer is described using different stages. However, brain tumors do not respond to this system because they spread throughout the brain and spinal cord. They practically do not spread to other parts of the body. To accurately determine treatment options, types of brain tumors in adults are classified by cell type.
Pituitary microadenoma and pregnancy
Brainstem gliomas are a disease that occurs in the part of the brain that connects to the spinal cord. Such tumors tend to grow rapidly, so their cells differ from normal ones. Gliomas can be diagnosed without a biopsy. Pineal astrocytic formations form in or near the pineal gland. The body is a small organ that produces melatonin.
This substance helps to control processes that are associated with the change of day and night. Piloid astrocytoma is an infected area that forms in astrocytes. They grow quite slowly and do not spread to other tissues. Pathologies of this type respond well to treatment. Diffuse astrocytoma tends to grow slowly, however, it can spread to other tissues.
Anaplatic astrocytoma is a malignant tumor that grows rapidly and affects nearby tissue. Gliboblastomas are malignant astrocytomas. They have a tendency to intensive growth and spread. Oligodendroglial occur in areas of the brain that nourish and support nerve cells. The names of all varieties come from the location and type of cells that make up the neoplasm.
There are the following types of brain tumors:
- Primary, which develop from nervous tissue;
- Secondary, which are metastases.
The first type is of particular importance, since it relates to diseases of the central nervous system. Neoplasms can be benign or malignant. Benign tumors do not differ from ordinary cells, so they do not penetrate other tissues. However, they can compress tissue and disrupt brain activity. Malignant tumors develop quickly and grow into nearby areas.
Treatment of cavernous angioma
Surgical treatment is the most effective treatment option for cavernoma. There is no universal medicine that could eliminate the pathology.
Prescribing treatment is often complicated by the fact that cavernous angioma does not cause discomfort to many patients, and persistent disability is observed mainly only with repeated hemorrhages from deep-lying angiomas or from neoplasms of the brain stem - areas that are difficult to access for surgical intervention.
However, even a benign course of the disease does not guarantee the absence of complications in the future, and timely surgery can completely eliminate the danger of negative consequences.
- with superficial cavernous angiomas, which manifest themselves as hemorrhages or seizures;
- for neoplasms that are located in active brain zones and manifest as hemorrhages, persistent neurological disorders, and epileptic attacks;
- with dangerous sizes of angioma.
In any case, the doctor must inform the patient about all possible risks and options for the course of the disease.
Surgical treatment of cavernous angioma can be carried out in several ways:
- Surgical intervention is a classic method of removing tumors, which will reduce the pressure of the vascular bundle on the surrounding brain tissue, which will eliminate unpleasant symptoms and the danger of rupture of pathological vessels. It has some contraindications: old age and multiple vascular formations.
- Radiosurgical surgery is the removal of a tumor using special devices (Cyber Gamma Knife). The essence of the method is that the angioma is exposed to a beam of radiation aimed at a certain angle. This procedure is considered safe, but is not as effective as surgery. This technique is used mainly in cases where surgery is impossible or difficult due to the inaccessibility of the angioma.
Traditional treatment of cavernous angioma
Herbal treatment for cavernous angioma is used only to relieve the symptoms of the disease. It is foolish to hope that taking herbal remedies will help completely get rid of the problem - we repeat once again that the only radical treatment for angioma is surgery. However, before starting such treatment, it is still recommended to consult a specialist.
- To prevent vascular wall ruptures, it is recommended to increase its elasticity. This can be achieved by drinking 2 tbsp daily on an empty stomach. l. any vegetable oil (one spoon in the morning, the second at night). Both olive or linseed oil and unrefined sunflower oil are used.
- To increase the elasticity of blood vessels, another common method is used: take a mixture of equal parts of natural honey, vegetable oil, flaxseed and lemon juice on an empty stomach every morning.
- To improve blood circulation, the following recipe may be useful: every day in the morning on an empty stomach, take one tablespoon of freshly squeezed potato juice. It is also recommended to drink an infusion of rose hips.
- To cleanse blood vessels and improve blood circulation, take garlic infusion. It is prepared as follows: grate a head of garlic and one lemon (with peel) on a fine grater, mix, pour in 0.5 liters of boiled chilled water and leave for 3-4 days. Drink 2 tbsp. l. daily. Can be stored in the refrigerator.
- Dill seeds help eliminate symptoms such as headaches. It is necessary to pour 1 tbsp of boiling water into a glass. l. seeds Take 1 tbsp. l. 4 rubles/day.
- To get rid of dizziness and noise in the head, it is useful to drink mint or lemon balm tea several times during the day.
- To strengthen blood vessels, it is recommended to eat a couple of green olives once a day in the morning before breakfast.
A tumor is usually understood as all brain tumors, that is, benign and malignant. This disease is included in the international classification of diseases, each of which is assigned a code, brain tumor code according to ICD 10: C71 denotes a malignant tumor, and D33 denotes a benign neoplasm of the brain and other parts of the central nervous system.
Since this disease is classified as oncology, the causes of brain cancer, as well as other diseases in this category, are still unknown. But there is a theory that experts in this field adhere to. It is based on multifactoriality - brain cancer can develop under the influence of several factors simultaneously, hence the name of the theory. The most common factors include:
Benign brain tumors
- Meningioma. Among primary brain tumors, it is diagnosed in approximately 20%. This disease originates from the pia mater of the brain. Meningioma looks like a smooth and dense nodule that is connected to the pia mater. The size of this formation can range from a few millimeters to 16 centimeters. The prognosis for development will depend entirely on its location and size. After surgery, such formations do not recur.
- Schwannoma. Formed from the sheath of peripheral nerves. It consists of white nodes that are enclosed in a kind of capsule. May cause hearing loss and trigeminal neuralgia.
- Pituitary adenoma. Despite the fact that the formation grows quite slowly, it causes very severe symptoms.
- Astrocytoma. The tumor tends to grow slowly and can reach very large sizes. Often in its structure you can find various cysts. May develop into a malignant formation.
- Oligodendroglioma. It is a neoplasm of gray-pink color. Cystic formations develop inside. It occurs mainly in mature males.
- Ependymoma. Foci of necrosis and cystic formations may be located inside this neoplasm.
The classification of brain tissue neoplasia into malignant and benign is quite arbitrary. Because all types of brain cancer can cause serious damage, leading to the death of the patient.
A brain tumor is an intracranial neoplasm that includes tumor lesions of the central nervous system and endocrine structures of the brain.
The question of what brain cancer is called worries many people. This term refers to cancer, which is based on intensive cell division. In children, the disease occurs as a result of a disorder in the structure of genes that are responsible for the proper formation of the nervous system. Scientists have concluded that cells that are actively dividing are susceptible to change. Since such processes occur more often in children than in adults, tumors can occur even in newborns.
Classification of tumors. (WHO 1993)
1.tumors of neuroepithelial tissue (astrocytoma, glioblastoma, oligodendroglioma, epindymoma, etc.),
2.tumors of the cranial nerves (neurolemmoma, or neuroma of the vestibulocochlear nerve, etc.),
3. tumors of the brain (meningioma, etc.),
4. lymphomas and tumors of hematopoietic tissue, tumors of germ cells (teratoma, etc.),
5.
cysts and tumor-like processes (craniopharyngioma, etc.),
6.tumor areas of the sella turcica (pituitary adenoma, etc.),
7.growth of tumors from nearby tissues, metastatic tumors, unclassified tumors.
In relation to the substance of the brain, tumors can be intracerebral (glioblastoma, etc.) and extracerebral (meningioma, etc.), depending on the location of the tentorial tentorium of the cerebellum - supratentorial (tumors of the cerebral hemispheres, etc.) and subtentorial (tumors of the cerebellum and brain stem).
Brain Tumor Clinic
1.Headache
2.Vomiting
3.Visual impairment – often occurs with pituitary adenomas
.
4. Impaired function of the cranial nerves - impaired sense of smell, impaired movements of the eyeballs, pain and/or numbness in the face, paresis of the facial muscles, decreased hearing, impaired balance, impaired swallowing, taste, etc. 5. Focal symptoms
Diagnosis of brain tumors
1. neurological examination , including a detailed ophthalmological examination of acuity, visual fields and fundus. 2. CT (computed tomography), MRI (magnetic resonance imaging), angiography, etc., as well as radioisotope methods 3. Electroencephalography (EEG) 4. Radiography
6. Ultrasonography is used in children with open fontanelles.
7.Lumbar puncture.
Treatment
Treatment
. Therapeutic tactics depend on the exact histological diagnosis, the following options are possible: . observation. surgical resection. resection in combination with radiation and/or chemotherapy. biopsy (usually stereotactic) in combination with radiation and/or chemotherapy. biopsy and observation. radiation and/or chemotherapy without tissue verification based on CT/MRI results and studies of tumor markers.
Forecast
depends mainly on the histological structure of the tumor. Without exception, all patients operated on for brain tumors require regular MRI/CT control studies due to the risk of relapse or continued tumor growth (even in cases of radically removed benign tumors).
ICD-10. C71 Malignant neoplasm of the brain. D33 Benign neoplasm of the brain and other parts of the central nervous system
D18.0 Hemangioma of any location
G93 Other brain lesions
Diagnostic methods
The variety and nonspecificity of people’s complaints when they develop piloid astrocytoma of the brain require a specialist to prescribe various diagnostic procedures. First of all, consultations are carried out with doctors - a neurologist, an ophthalmologist, as well as an otolaryngologist and an endocrinologist.
Laboratory diagnostics consists of performing studies such as:
- blood tests - general and biochemical, for tumor markers and hormone parameters;
- assessment of the state of the cerebrospinal fluid;
- identification of neuroinfections suffered by a person.
Instrumental examination methods are also used:
- MRI – allows you to identify the size of the tumor and its localization, involvement of neighboring structures in the pathological process, the presence of metastases;
- EEG – assessment of the functioning of different parts of the brain, predisposition to epilepsy;
- angiography - identifying disruptions in the blood supply to brain structures;
- ultrasound examination of internal organs - their damage by metastases;
- biopsy - taking, if possible, biomaterial from a cancerous lesion and histological examination of cells for atypia.
After carefully compiling information from diagnostic procedures, the oncologist gives his conclusion and then selects an adequate scheme for eliminating the disease.
Symptoms (signs)
Clinical picture.
The most common symptoms of brain tumors are progressive neurological deficit (68%), headaches (50%), and seizures (26%). The clinical picture mainly depends on the location of the tumor and, to a lesser extent, on its histological characteristics. Supratentorial hemispheric tumors.. Signs of increased ICP due to mass effect and edema (headaches, congestive optic discs, impaired consciousness).. Epileptiform seizures.. Focal neurological deficit (depending on location).. Personality changes (most typical for frontal lobe tumors). Supratentorial tumors of mid-localization.. Hydrocephalic syndrome (headache, nausea/vomiting, disturbances of consciousness, Parinaud's syndrome, congestive optic discs)... Diencephalic disorders (obesity/emaciation, thermoregulation disorders, diabetes insipidus)... Visual and endocrine disorders in tumors. chiasmal-sellar region. Subtentorial tumors.. Hydrocephalic syndrome (headache, nausea/vomiting, disturbances of consciousness, congestive optic discs).. Cerebellar disorders.. Diplopia, severe nystagmus, dizziness.. Isolated vomiting as a sign of an effect on the medulla oblongata. Tumors of the base of the skull. Often remain asymptomatic for a long time and only in the later stages cause neuropathy of the cranial nerves, conduction disorders (hemiparesis, hemihypesthesia) and hydrocephalus.