What it is
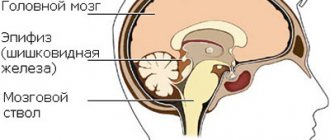
The mammalian brain is enveloped in three layers. Hard, cobwebby and soft. The middle structure is a connective tissue layer. Between the second and third layers is the subarachnoid space filled with cerebrospinal fluid. In addition, there is a system of vascular caverns that feed the organ. Due to infection, inflammation appears, which leads to clouding and the formation of dense areas of the arachnoid layer.
This is how adhesions appear between arteries and veins. As a result, fluid movement slows down significantly. Cystic formations appear on hardened areas. As a result, the pressure inside the brain cavity increases greatly.
Thus, arachnoiditis is a disease associated with inflammation of the meninges. The venous sinuses, which serve to accumulate blood and drain cerebrospinal fluid, begin to decrease in size, and cerebrospinal fluid fills the cavity of the cranium.
The disease occurs due to many reasons: an allergic reaction, an autoimmune process, a viral or bacterial infection, a post-traumatic effect. Inherent in young people and children.
Timely treatment will ensure a further healthy existence. Lack of therapy causes inflammation to transfer to the cerebral cortex and, as a result, encephalitis.
Forms and types of disease
Clinical diagnosis distinguishes several types depending on topography. There are several classifications.
According to the cause, the disease is divided into:
- True (arising from autoimmune diseases).
- Secondary (appears as a concomitant pathology).
According to topographical characteristics:
- Cerebral – damages the brain.
- Spinal – the spinal cord is affected.
Based on the location of the source of inflammation inside the skull, they are divided into:
- Convexital (convex areas of the cerebral hemispheres).
- Basilar or basal (an alternative name is opto-chiasmatic).
- The area at the back of the head.
Symptoms of pathology
Signs by which a doctor may suspect a disease are a set of symptoms of a cerebral disorder. However, there are also symptoms characteristic of arachnoiditis:
- Headache in some cases accompanied by nausea and even vomiting. It mainly bothers the patient in the morning. The pain is local. After any effort (sudden movement, straining, etc.), its manifestations intensify.
- Dizziness.
Read more about the causes of dizziness. We'll tell you what can make you feel dizzy.
- General weakness of the body.
- Sleep disorders.
- Memory impairment.
- Increased irritability.
Dr. Myasnikov Alexander Leonidovich in the program “About the Most Important Thing” will talk about the most alarming clinical causes of sharp and severe headaches:
As a rule, during the disease the entire surface of the arachnoid membrane becomes inflamed. In the case of limited arachnoiditis, disturbances occur in a separate area. Depending on where the source of the disease is located, the following symptoms are possible:
- The convexital type of arachnoiditis is manifested by irritation of the brain. In this case, the patient may experience seizures similar to epileptic ones.
- If the swelling is more developed in the occipital region, hearing and vision impairment occurs. The patient notes loss of the visual field, and during an examination of the fundus, the doctor may note optic neuritis.
- The patient reacts sharply to changes in weather. At the same time, he experiences excessive sweating or chills. In some cases, a person complains of a constant feeling of thirst. Sometimes there is an increase in body weight.
- When the cerebellar angle is damaged, pain occurs in the occipital part of the head, dizziness and tinnitus. There is an imbalance.
The figure shows the largest cisterns of the subarachnoid space. Depending on the location of the inflammation, the patient experiences different clinical manifestations of the disease.
- Cystic arachnoiditis can have various manifestations, which are associated with the nature of the adhesions. If it does not lead to an increase in ICP, the disease may not be detected for several years. During this time, balance gradually deteriorates and synchronization is lost.
- When the anterior lobes of the brain are damaged, memory decreases, the patient’s psychological state is disrupted, convulsions and various mental abnormalities appear.
- It is very difficult to identify adhesive cerebral arachnoiditis, since it is not characterized by localization of manifestations, and the symptoms are similar to those of many diseases.
- If arachnoiditis affects the occipital cisterns, then signs of damage to the facial nerve appear. The patient's body temperature rises.
Read about the main causes of Bell's palsy (inflammation of the facial nerve) in a detailed article.
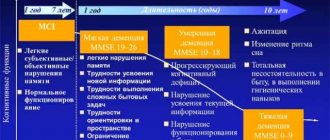
It is worth noting that cerebral arachnoiditis does not develop spontaneously. From the moment of an infectious disease to the appearance of the first symptoms, at least several months or even 1 year can pass. In case of injury, the disease can make itself felt only 2 years after brain damage. Phases of exacerbation of the disease are always followed by periods of remission.
The onset of the pathology is subacute. The patient complains of irritability, headache or dizziness, constant weakness and fatigue. Over time, as the inflammatory process progresses, focal or cerebral signs of the disease appear.
Neurologist Mikhail Moiseevich Shperling talks about the symptoms of increased intracranial pressure:
This disease is characterized by the formation of adhesions and fusion of the membranes of the brain, as a result of which the outflow of cerebrospinal fluid is necessarily disrupted. When cerebrospinal fluid accumulates in the subarachnoid space or cysts, this leads to expansion of the brain cavities. Thus, intracranial pressure increases, which is considered one of the main symptoms of the disease.
Causes and risk factors
Pathology can occur due to various factors. Most often it manifests itself against the background of autoimmune diseases that affect the cellular composition of the arachnoid layer and blood vessels.
Most often it appears due to the following health problems: acute infectious pathologies, rheumatic diseases, purulent tonsillitis, sinusitis, otitis media, meningitis or encephalitis.
Risk factors include:
- cranial trauma;
- chronic excess of toxins in the body;
- occupational diseases;
- chronic pathologies of the respiratory tract;
- hard work in difficult environmental conditions.
Thus, there are plenty of opportunities to contract the disease. It is important to recognize and begin therapy in time.
Possible consequences
One of the consequences of arachnoiditis can be adhesions and cysts of the brain. This complication often requires conservative treatment. The patient undergoes surgery to remove the cyst or adhesions.
Despite the seriousness of such a diagnosis as arachnoiditis, in general the disease can be resolved successfully. The most important thing is a timely response to neurological symptoms and other deteriorations in well-being.
With successful therapy, the patient leads a completely normal life. But, if qualified assistance is not provided, a transition to a chronic form of the disease will occur, which leaves an imprint on life activity and leads to disability.
Symptoms and signs of arachnoiditis
The disease is characterized by focal and cerebral symptoms. Species of different topography differ in symptoms. These are the most common manifestations of the opticochiasmatic flow.
General cerebral
The development of these manifestations is influenced by an increase in pressure inside the membranes of the GM. Typically, patients have the following complaints:
- The appearance of a headache after waking up. Problems with eye movement, vomiting.
- Sometimes dizziness occurs.
- Tinnitus.
- Problems with exposure to excessive environmental factors.
- Sensitivity to weather changes.
Diagnosis of brain arachnoiditis
In most cases, obvious signs of cerebral arachnoiditis, which can be called dizziness, frequent headaches with regular nausea and vomiting, do not cause suspicion in the patient. At the initial stage, they appear several times during the month and only when the disease becomes chronic do they occur quite often and last a long time, so they force a person to seek medical help.
The difficulty is that the symptoms of developing arachnoiditis are characteristic of a large number of ailments, so treatment is often delayed. To make an accurate diagnosis, the doctor will need to conduct a number of examinations:
- Ophthalmological examination. The most common type of disease is opticochiasmatic arachnoiditis. Approximately half of patients have signs of posterior fossa involvement.
- Magnetic resonance imaging. This research method makes it possible to determine the presence of inflammation in the brain in 99% of cases. The examination reveals the presence of cysts and inflammation in the arachnoid membrane of the brain. It also allows you to exclude other pathologies that have the same manifestations (abscess, tumor, etc.).
Accumulation of cerebrospinal fluid in the convexital space. Cerebral arachnoiditis on MRI in T2 mode
- A clinical blood test makes it possible to determine the inflammatory process in the body and the presence of infection in it. It is also possible to identify an immunodeficiency state, that is, to detect the main causes of the development of the disease.
- Radiography makes it possible to diagnose intracranial hypertension.
- Consultation with an otolaryngologist is indicated for people with manifestations of hearing loss.
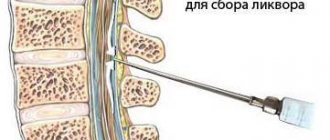
- Lumbar puncture allows you to determine the level of intracranial pressure. In the case of development of brain arachnoiditis, an increased amount of protein and neurotransmitters can be detected in the cerebrospinal fluid.
Only after a comprehensive examination and accurate diagnosis will the doctor be able to prescribe the correct treatment.
Treatment of arachnoiditis
Inflammation of the meninges is treated comprehensively. It is necessary to first establish the cause of the disease to clarify the use of appropriate remedies. In addition, medications are used that enhance the immune system and ensure the absorption of fluid.
Traditional
Treatment of brain arachnoiditis is carried out with antibacterial agents: for purulent tonsillitis, sinusitis or otitis. For allergies - drugs that reduce sensitivity and remove the consequences. Absorbable drugs and diuretics are used to reduce hypertension. Medicines are used against seizures, as well as substances that improve metabolism.
Folk
It is impossible to cure cerebral arachnoiditis using traditional methods of therapy. Tinctures and decoctions can be used as an additional remedy for conservative treatment. However, it is practically impossible to recover using only traditional methods.
Prevention
In order to prevent it, it is necessary to promptly treat foci of infectious processes in the body (caries, sinusitis), treat acute inflammatory diseases, and monitor the condition of brain structures after injuries.
Treatment methods
After the diagnosis is established, the patient is hospitalized in the neurosurgical department and undergoes a course of treatment. The first priority is to eliminate the source of the main infection if the disease develops as a complication. For this purpose, antibiotics and antihistamines are prescribed.
Since the disease leads to disruption of the outflow of cerebrospinal fluid from the brain, this complication should be eliminated. To do this, the patient is given diuretics, as well as vascular and absorbable drugs to reduce the amount of cerebrospinal fluid: furosemide, piracetam. In some forms, seizures are serious symptoms, so the patient is prescribed anticonvulsants: convulex, phenobarbital.
Prognosis for arachnoiditis
Unfortunately, it is quite rare that complications disappear without a trace for the body. When detected in time, arachnoiditis practically does not pose a threat to life, only hydrocephalus is included in the sad statistics.
After recovery from arachnoiditis, ability to work can be fully restored. If this is not possible, then a group 3 disability is assigned.
A rare consequence of the disease is the appearance of epilepsy after severe cerebral arachnoiditis. The only way to counteract this is to undergo a course of treatment with anticonvulsants throughout your life. In this case, disability of group 2 is assigned.
The worst prognosis is for those whose hearing or vision has decreased due to the disease, or the facial nerve has been damaged. Their restoration is almost impossible, so such patients are assigned disability group 1.
Methods for diagnosing the disease
To make a correct diagnosis, the following measures are necessary:
- thorough questioning of the patient to identify the fact of previous infectious diseases, injuries, operations using spinal anesthesia;
- neurological examination to identify disorders of sensitivity, motor function, visual impairment, hearing, and vestibular apparatus;
- X-ray examination of the skull bones is carried out to identify changes characteristic of traumatic brain injury, as well as expansion of the cerebrospinal fluid cavities of the brain (ventricles);
- Ultrasound examination of the brain allows one to establish the fact of increased intracranial pressure;
Increased intracranial pressure is a symptom of arachnoiditis - computer (magnetic resonance) imaging is performed to assess the degree of cystic lesions of the arachnoid membrane, the substance of the brain, determine the size of the cavities (ventricles), and also to exclude a tumor;
Computed tomography is the most important method for diagnosing arachnoiditis. The arrows indicate a pathological brain formation (cyst) - electroencephalography (EEG) – registration and interpretation of electrical signals from the brain, carried out to identify signs of epilepsy;
- an examination by an ophthalmologist is necessary to assess visual acuity, visual fields, and the fundus picture;
- an examination by an ENT doctor is carried out to determine hearing acuity, the function of the vestibular apparatus, to exclude an infectious process in the outer, middle, inner ear, and paranasal cavities;
- examination by a psychiatrist is necessary to identify disturbances in thought processes, symptoms of personality changes;
Differential diagnosis is carried out with the following diseases:
- tumor of the central nervous system;
- multiple sclerosis;
- optic neuritis;
- neurosarcoidosis;
- idiopathic epilepsy;
- neurosis and neurasthenia;
Pathogenesis of the disease
The arachnoid meninges are formed from connective tissue. Like a thin web, it fits tightly to the pia mater of the brain, so they are often considered as one whole. Between these membranes there is a subarachnoid space filled with cerebrospinal fluid and blood vessels that nourish the entire structure.
Therefore, inflammation is not local. Infection in the arachnoid membrane can come from the hard or soft membrane. When infected, the arachnoid membrane thickens and becomes cloudy. Adhesions occur between it and the blood vessels, which interferes with the normal circulation of the cerebrospinal fluid. Over time, cysts form here. This pathological process leads to increased intracranial pressure and the formation of hydrocephalus.
The autoimmune variant of arachnoiditis suggests the possibility of producing antibodies that have an inhibitory effect on the arachnoid membrane. Such inflammation can occur locally, only in this membrane of the brain. It is called true arachnoiditis.
Clinical picture
The patient suffers from frequent headaches, which are accompanied by:
- painful sensations in the limbs;
- epileptic seizures;
- visual impairment;
- dizziness;
- tinnitus (tinnitus)
The patient's gait is unstable, "staggering". Sleep is disturbed and insomnia develops. Efficiency drops.
CSF crises appear. These conditions are characterized by increased blood pressure. Patients complain of increased headaches. There is no appetite, and in 15-20% of cases, vomiting occurs after eating. Headaches worsen when coughing, laughing, sneezing.
With moderate arachnoiditis, CSF crises appear 1-2 times a month. As the disease progresses, crises occur 1-3 times a week.
In 80% of cases, arachnoiditis develops gradually. The patient complains of signs characteristic of neurasthenia or asthenia.
The following nonspecific symptoms of arachnoiditis are characteristic:
- frequent mood changes;
- fatigue;
- drowsiness;
- lethargy;
- decreased concentration.
In 30-40% of cases, convulsive seizures appear, transforming into status epilepticus (characterized by the fact that seizures often recur within 3-7 days).
Treatment
Cerebral arachnoiditis takes a long time to treat. The therapeutic regimen involves repeated treatment courses every four to five months.
The best results are achieved by therapy started in the stage of acute inflammation. This clinical variant of the disease can be cured before the formation of irreversible pathological changes. This means that there is a high probability of complete recovery without long-term consequences.
Therapy for this disease is carried out in the following main areas:
- antibacterial therapy aimed at eliminating the primary infectious focus;
- anti-inflammatory therapy;
- absorbents;
- hyposensitizing effects;
- dehydration therapy is relevant in connection with intracranial hypertension and is used to avoid complications that may be caused by increased intracranial pressure;
- anticonvulsant therapy is carried out when a convulsive syndrome occurs;
- symptomatic therapy is carried out as needed.
Surgical treatment of cerebral arachnoiditis has the following indications:
- insufficient effectiveness or ineffectiveness of conservative therapy;
- progression of intracranial hypertension despite drug treatment;
- increasing severity of focal symptoms;
- optico-chiasmatic form of arachnoiditis with progressive deterioration of vision.
This situation often occurs, for example, with cystic adhesive arachnoiditis, when there is a pronounced difficulty in the circulation of cerebrospinal fluid.
The use of medications does not always help eliminate a disease such as cerebral arachnoiditis. Treatment in some cases is surgical. Indications for surgical intervention are:
- lack of improvement after drug therapy;
- increase in intracranial hypertension;
- increase in focal symptoms;
- the presence of opticochiasmatic arachnoiditis, which is characterized by a steady deterioration of vision.
For example, a neurosurgical operation can be performed when an adhesive process develops with the formation of adhesions or a cystic process in a disease such as cerebral arachnoiditis of the brain. Treatment of this kind will allow you to get rid of obstacles that interfere with the normal circulation of cerebrospinal fluid.
Treatment for arachnoiditis is usually carried out in a hospital. It depends on the etiology and degree of disease activity. Drug treatment is carried out over a long period of time, in courses, taking into account the etiological factor and includes:
- Antibacterial or antiviral drugs;
- Antihistamines (pipolfen, diphenhydramine, suprastin, claritin, etc.);
- Anticonvulsant therapy (carbamazepine, finlepsin);
- Anti-inflammatory drugs - glucocorticoids (especially for allergic and autoimmune inflammation);
- Absorbable treatment aimed against adhesions in the interthecal space (lidaza, rumalon, pyrogenal);
- Diuretics for hypertension syndrome (mannitol, diacarb, furosemide);
- Neuroprotective treatment (mildronate, cerebrolysin, nootropil, B vitamins).
Since the disease lasts a long time, is accompanied by manifestations of asthenia and emotional disorders, a number of patients need to be prescribed antidepressants, sedatives, and tranquilizers.
In all cases of arachnoiditis, other foci of bacterial or viral infection are searched for and treated, since they can be a source of repeated inflammation of the meninges. In addition to antibiotics and antiviral drugs, general strengthening measures, taking multivitamin complexes, good nutrition and an adequate drinking regimen are indicated.
Diagnosis of the disease begins with an examination. The doctor asks questions, and the patient answers them: how often does the headache occur and what location does it have, do attacks of nausea and vomiting occur, and how often does this happen, are there epileptic seizures, how much vision is reduced. Such a survey makes it possible to establish the localization of the disease and the degree of development of the disease.
Diagnosis of arachnoiditis:
- Visual acuity examination, fundus examination. Establishing how narrowed the field of view is. Which eye sees better, what is the dynamics of vision deterioration.
- Craniography is an X-ray of the brain without contrast. Diagnostics allows you to see an inflammatory effusion if it is present - it manifests itself as a loose area in the skull in which cerebrospinal fluid accumulates.
- Magnetic resonance imaging. The most striking study that will allow you to see the degree of swelling of the arachnoid membrane, as well as establish the locations of cysts and adhesions. This is extremely important for further treatment and possible surgery.
- An electroencephalogram of the brain allows us to determine the degree of development and severity of the epileptic component.
- Angiography, scintigraphy, X-ray with contrast, cerebrospinal fluid puncture.
All types of research are aimed at determining the exact location of arachnoiditis. It is important to establish how the disease progresses, what the dynamics of development are, whether drug treatment is possible, and what the prognosis is for the patient. Only guided by the results of the study, the doctor is able to make an accurate diagnosis.
Treatment is carried out only in a hospital setting
Main methods of treatment:
- Drug therapy with antibiotics: ampicillin series, Oxacillin, Amoxiclav. Antibiotics are prescribed for a course of treatment, which is repeated several times. Also prescribed are drugs to reduce intracranial pressure and diuretics, drugs aimed at reducing swelling of the arachnoid membrane.
- Medicines are injected directly into the carotid artery - intracarotid infusion.
- Surgical intervention is indicated for arachnoiditis of the postcranial fossa or for severe visual impairment. They also operate if the disease has affected the convex surface of the brain or with local manifestations of spinal arachnoiditis.
- If confused arachnoiditis occurs, when adhesions and cystic-adhesive formations appear, it is recommended to treat with neurosurgical intervention in the brain cavity. Pneumoencephalography is performed when compressed air is introduced into the cavity of the subarachnoid membrane to break the adhesions, restoring the circulation of cerebrospinal fluid.
- Radon baths, mud, physiotherapy, massages, herbal medicine.
If the disease is in the initial stage, then it is subjected to drug treatment. If there is a serious threat of vision loss or other serious complications, surgical intervention is used. Traditional medicine for the treatment of arachnoiditis comes down to maximally reducing swelling, eliminating inflammation, and stimulating the immune system.
Treatment of arachnoiditis with folk remedies:
- A teaspoon of dried and crushed elecampane root is poured with 0.5 liters of hot water and left for 20 minutes. The decoction is taken 50 g per dose 3-4 times a day before meals.
- A tablespoon of dried arnica flowers is poured with boiling water and left for up to one and a half hours. The infusion is taken one tablespoon 3 times a day. Helps relieve swelling of the brain.
- Coltsfoot is a universal anti-inflammatory plant. The dried leaves are crushed. For 3–5 tablespoons of dry plant there is up to 1 liter of boiling water. Leave in a warm place for 30 minutes. The infusion is taken a quarter glass on an empty stomach 4 times a day.
- Essential aromatic oils have a good effect on the nervous system. They perform acupressure on the head to reduce pain. Lavender, incense, thyme, sage, bergamot, sandalwood.
Essential oils and herbal medicine are recommended to be used continuously along with the main treatment. There will be no harm from this. And the patient will feel more calm and confident.
The principles of treatment for inflammation of the arachnoid membrane of the brain depend on its type. The patient is admitted to the hospital to avoid unforeseen complications. Medication is aimed at eliminating symptoms, reducing intracranial pressure, and eliminating the consequences caused by brain injuries.
In most cases, the doctor prescribes treatment, the prognosis of which promises a speedy recovery. Timely intervention by specialists makes arachnoiditis not such a terrible disease.
- To combat inflammation, a group of glucocorticosteroid and absorbable drugs, such as Prednisolone and Pyrogenal, are used.
- Adhesive and cystic-adhesive arachnoiditis lead to epileptic seizures, so the use of carbamazepine is also recommended.
- Allergic reactions are fought with Clemastine or Hifenadine.
If purulent foci of infection are observed in the subarachnoid layer, specialists carry out a number of health measures. Surgery is acceptable in case of emergency.
Important! The use of traditional medicine methods for inflammation of the arachnoid layer is strictly prohibited, as it can only worsen the situation.
The method of treatment, medicinal or surgical, depends on the severity of the clinical course and localization of the pathological process. Surgery is performed in the following cases:
- Optical-chiasmal type of arachnoiditis.
- Arachnoiditis of the posterior cranial fossa.
- For hydrocephalus, a shunt is performed to create pathways for the outflow of cerebrospinal fluid.
With the help of surgery, it is possible to restore the passage of the cerebrospinal fluid pathways; cysts can be removed and adhesions can be separated. If visual acuity is significantly reduced, electrodes are implanted to stimulate the optic nerves.
Drug therapy:
- Antibacterial therapy directed against a specific infection. Antibiotics of the penicillin group, cephalosporins, etc. are prescribed. They are administered intramuscularly, intravenously, and also into the posterior cervical lymph nodes (endolymphatic route of administration). Chronic foci of infection are sanitized with antibiotics.
- Anti-inflammatory therapy. It consists of prescribing corticosteroids: prednisone, dexamethasone, etc. They are effective in cases of infectious and allergic nature of brain damage.
- Dehydration therapy is carried out to reduce the level of intracranial pressure. Diuretics are prescribed: Diacarb, Mannitol, Furosemide, etc.
- Antiepileptic drugs are prescribed for convulsive syndromes: Finlepsin, Carbamazepine, etc.
- Neuroprotectors and drugs to improve metabolic processes: Actovegin, Piracetam, Mildronate, Iodine preparations, Lidaza, etc.
- Psychiatric drugs: antidepressants, tranquilizers.
- Vasodilator drugs are prescribed to improve cerebral circulation: Cavinton, Vinpocetine, Cerebrolysin, etc.
- Antihistamine therapy: Diazolin, Tavegil, etc.
- Lumbar puncture is performed to reduce intracranial pressure.
- Vitamin therapy is prescribed to increase the internal strength of the body.
- Antioxidant therapy is allowed.
Causes of the disease
Arachnoid inflammation is associated primarily with the following primary injuries:
- infections of acute or chronic type (sinusitis, pneumonia, meningitis, tonsillitis, etc.);
- constant poisoning (alcohol, lead, chemicals, etc.);
- post-traumatic disorders (that is, the consequences of traumatic brain injuries and bruises of the spinal column);
- pathologies of the functioning of the endocrine system.
However, the exact cause of this disease cannot always be determined.
Diagnostics
The diagnosis of “arachnoiditis” is made only based on:
- anamnestic data;
- information about the mental and neurological condition of the patient;
- results of various examination methods: EEG; MRI and computed tomography of the brain; lumbar puncture; ophthalmological; otolaryngological, etc.
Only after reviewing and evaluating all of the above data can an accurate diagnosis be made.
Types of arachnoiditis
By etiology:
- true;
- traumatic;
- post-flu;
- toxic;
- rheumatic;
- tonsilogenic.
According to the course of the disease:
- spicy;
- subacute;
- chronic.
According to the location of the pathological process:
- convexital arachnoiditis (with damage to the frontal, parietal, temporal or central gyri);
- basal arachnoiditis (base of the brain);
- arachnoiditis of the cerebellopontine angle;
- arachnoiditis of the posterior cranial fossa.
Below we will consider these types of arachnoiditis in more detail, since the localization of cysts and adhesions significantly affects the clinical manifestations of the disease.