What is an epidural hematoma?
An epidural hematoma of the brain is a hemorrhage between the dura mater and the bones of the skull itself.
Frequency:
- In 5% of these cases it is bilateral (sometimes only after surgical decompression on one side).
- 1-5% of all victims with traumatic brain injury
- Acute, usually traumatic hemorrhage between the inner plate of the skull bones and the dura mater. Usually a consequence of damage to the artery (in 85% of all cases - the middle meningeal artery)
- Venous hemorrhage occurs in 15% of all cases (diploic veins, venous sinuses of the dura mater of the brain, especially with subtentorial hematomas)
- In 20% of cases it can occur in combination with other types of hematoma (subdural, subarachnoid, intracerebral)
- Localization: usually temporo-parietal region.
Clinical symptoms of intracerebral hematomas
The slow onset of the subdural form is explained by rupture of the pontine veins. Venous bleeding does not progress as quickly as arterial bleeding. The danger to life is higher due to compression of brain structures. Neurological disorders are caused by damage to active centers. Focal manifestations are accompanied by impaired vision, hearing, and innervation of the muscles of the limbs.
An epidural hematoma has a “light gap” at the beginning of its development. Symptoms develop quickly. The first manifestations can be seen a few minutes after a brain injury or taking medications. The danger is posed by sharp braking with counter-impact, which contributes to double-sided hemorrhage.
The clinical picture is variable. Depends on the location and size of the outbreak. Focal neurological disorders occur several hours after TBI.
Acute SDH is characterized by a violation of consciousness of the cortical type with a decrease in self-criticism and frontal symptoms. Patients experience headache and psychomotor agitation. Signs of meningeal pathology are intoxication, nausea, vomiting. Extensive hemorrhage causes epileptic attacks of muscle contractions. Generalized attacks of multiple symptoms can only be eliminated by surgical decompression.
Time frame for hematoma resorption
The time for spontaneous disappearance of acute hematomas varies. It is difficult to determine the timing, since the nosology must be immediately eliminated using medications. Surgical intervention is aimed at eliminating hypertension and clearing the area of hemorrhage from blood clots.
Small subacute types resolve on their own after a few months with proper treatment. The prescription of anticoagulant drugs allows the pathological focus to be eliminated, but therapy must be carried out carefully so as not to provoke re-bleeding.
Chronic subdural hematoma
It is more difficult to eliminate chronic subdural hematomas (CSH). The nodes have a tendency to bleed. Prescribing anticoagulant (anti-clotting) therapy increases the likelihood of exacerbation. The right tactics can eliminate HSH within a few months.
If the formation is formed for more than three weeks, a fibrous capsule appears. The dense wall does not dissolve. The period of resorption of formations is more than half a year.
Literary sources do not describe the exact time of appearance of the capsule, so it is difficult to accurately indicate the time of complete cure of chronic FH.
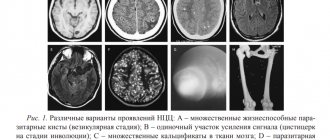
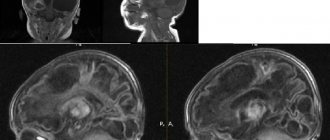
Tomograms of epidural hematomas
Which method of diagnosing epidural hematoma to choose: MRI, CT, X-ray, angiography
Selection method:
- MSCT
What will a head x-ray show for an epidural hematoma?
- It allows you to detect only a fracture of the skull bones, but not intracranial hemorrhage.
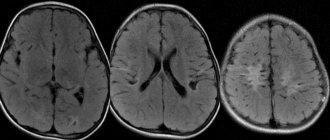
What will CT scans of the brain show in the presence of an epidural hematoma?
- Lenticular shape
- Hyperdense
- Fresh, unclotted blood may also be hypodense
- The hematoma does not cross the suture lines, since the dura mater is tightly fused with the bones of the calvarium along the boundaries between them
- Pronounced volumetric impact: displacement of midline structures
- Blurred boundaries between gray and white matter
- Impaired cerebrospinal fluid circulation (occlusion of the interventricular foramen of Monroe)
- Narrowing of the surrounding cistern (possible herniation of the medial parts of the temporal lobe into the notch of the tentorium of the cerebellum)
- The volume of the hematoma can quickly increase
- There is usually a fracture of the calvarial bones with displacement
- After removal of ventricular tamponade, recurrent postoperative contralateral bleeding (epidural or intracerebral) may occur.
Is MRI of the brain informative for epidural hematoma?
- Not shown, since organizing and conducting the study takes a lot of time.
Diagnostics
The initial treatment for TBI is a complete neurological examination. If there is a suspicion of severe injury, the patient undergoes x-rays, computed tomography and magnetic resonance therapy.
Computed tomography is an effective diagnostic method. The formations in the epidural space have a biconvex shape. Their typical localization area is the temporal bone (os temporale), namely the scaly part (pars squamosa). They represent an area of tissue with reduced density. The structure of hematomas is heterogeneous. The boundaries of education are unclear.
With large tumor sizes, there are no difficulties in making an accurate diagnosis. However, if the blood collection is small, or there is damage to the brain parenchyma, a more careful differential diagnosis is required. Magnetic resonance imaging makes it possible to conduct accurate studies, excluding subdural hematoma.
Possible complications and consequences of epidural hematoma
The consequences of an epidural hematoma are:
- Chronic fatigue syndrome
- Depression
- Speech Impairment
- Neuroses, psychoses
- Decreased memory and mental activity
- Numbness, paralysis of limbs
- Convulsions
Epidural hematoma. CT, axial slice. Convex hyperdense formation adjacent to the calvarium. Sutures serve as a natural barrier to epidural hematomas, since in these areas the dura mater of the brain is tightly attached to the calvarium (a). Epidural hematomas usually occur at the fracture site (b).
Symptoms of EPG
The classic picture of epidural hemorrhage is characterized by the appearance of a “light interval” - a period when the patient’s serious condition is compensated by the body. This period of time is characterized by the following symptoms:
- Loss of consciousness for a short time, followed by recovery of the state either completely or to a state of stupor;
- Dizziness with moderate headache;
- Weakness;
- Amnesia, often retrograde, in which a person does not remember the events preceding the injury;
- Nystagmus - twitching of the eyeballs;
- Sensitivity disorder.
This condition is usually classified as mild or moderate TBI and lasts from 30 minutes to several hours. The end of the “bright period” is accompanied by a significant deterioration in the person’s condition. Symptoms increase, consciousness becomes clouded, until stupor or coma develops. The difference between these two conditions is obvious.
An increase in blood pressure occurs, paresis of the facial nerve may occur, as well as weakness of the muscles of the upper extremities, moreover, on the opposite side of the hematoma. On the side where the epidural hematoma is located, the pupil is dilated and there is no reaction to light. Such a difference between the “bright gap” and the deterioration of the condition allows one to suspect a complication such as EPG. But sometimes the “bright gap” occurs in an erased form. And it is immediately accompanied by coma. A light period nevertheless occurs and the coma gives way to stupor, and then the condition worsens again. Paresis and paralysis, oculomotor dysfunction and vestibular disorders are possible.
Much less common is EPG without a “light gap” at all. This is typical for severe traumatic brain injuries. A person falls into a coma and never comes out of it. In addition to the classic picture of an epidural hematoma, it is characterized by focal symptoms - that is, signs of damage characteristic of injury to a certain area of the brain.
If the epidural hematoma is located in the frontal lobe, then mental disorders with speech impairment predominate; if its localization affects the occipital region, then the field of vision is lost - partially or completely. Hemorrhage in the parasagittal region leads to a pronounced manifestation of pyramidal disorders, which are combined with foot paresis.
Diagnosis and treatment of EPG
Not only the clinical picture speaks of an epidural hematoma. The diagnosis must be supported by instrumental examination data. For this use:
- X-ray of the skull, in which it becomes possible to accurately determine the presence of a fracture in the area of intersection of the vascular network of the brain. Usually the hematoma is located precisely at the fracture site;
- Echoencephalography (ECHO-EG), which allows you to record the displacement of the echo signal axis. Echo-EG for diagnosing hematomas is used much less frequently due to the advent of CT and MRI. However, in their absence, it is used as a valuable diagnostic method;
- Cerebral angiography, which allows to detect changes in the vascular pattern. The hematoma looks like an avascular area that has the shape of a convex lens;
- Computed tomography (CT) is a modern accurate diagnostic method that allows you to obtain accurate information about the formations inside the cranial cavity - their volume and location;
- Magnetic resonance imaging (MRI), which is considered the most accurate and sensitive method of diagnostic manipulation, which allows you to examine each of the structures of the human brain layer by layer. However, it is not always possible to perform an MRI due to the fact that during the procedure you need to remain completely still; many victims are not able to do this. In addition, not every hospital is equipped with an MRI machine.
Treatment of an epidural hematoma should not be delayed. Both conservative drug therapy and surgical intervention are carried out. Drug therapy is prescribed only in the case of:
- Small hematoma, volume up to 30-50 ml;
- Minimal symptoms of brain damage, without an increase in general cerebral and focal signs;
- Asymptomatic hematomas, when the small size is confirmed on CT or MRI, and there are no signs of displacement of brain structures.
Treatment is accompanied by dynamic observation, that is, diagnostics, which includes monitoring the condition of the hematoma and its size. In order to proceed with surgical intervention in case of negative progression. Most often, treatment is performed surgically. Special holes are made in the skull, above the hematoma, which reduces the increased intracranial pressure.
If the pressure rises rapidly, then aspiration, that is, blood suction, immediately begins through the holes. And after this, trepanation is performed, during which the EPG is completely removed and the damaged vessels are ligated. Indications for surgical treatment are:
- Increasing clinical symptoms of hematoma with focal, cerebral, dislocation signs;
- Signs of massive EPG on CT or MRI, as well as symptoms of displacement of brain structures, deformation or compression;
- Open penetrating head injury or other concomitant cranial injuries such as a depressed fracture, which require surgical intervention regardless of the volume of the hematoma.
Of course, surgical intervention is carried out using decongestants, hemostatic drugs, as well as using symptomatic therapy. During the recovery period, absorbable agents are used, as well as a number of neurometabolic agents. In addition to medications, therapy is complemented by massage and physical therapy. About a quarter of epidural hematomas are fatal. The prognosis will depend on the size of the hematoma, the condition of the patient, her age, as well as the timeliness of treatment measures.
However, among all types of hematomas, epidural has a fairly good prognosis. For example, in comparison with subdural. It is important to differentiate these two types of intracranial hemorrhages. The accumulation of blood in a subdural hematoma occurs between the dura mater and the arachnoid. In this case, venous bleeding is observed, whereas with EPG it is arterial. The subdural hematoma is located mainly extensively, and the epidural one is limited. The “light gap” with subdural hematomas can last for weeks, and with EPG, a maximum of 1-2 days.
The introduction of CT and MRI devices into medical practice contributed to earlier detection and treatment of EPG. According to statistics, thanks to these diagnostic studies, mortality has decreased by 10-15%. The age factor plays a significant role in predicting the outcome of EPG. The lowest percentage of mortality is children and young people, up to 10%, and the highest is the elderly – from 50 to 90%. The compensatory capabilities of their body are weaker, and the signs of hematoma are often hidden. And the overlap of many other diseases typical of older people makes diagnosis difficult.
Treatment prescribed at the appropriate time has a favorable prognosis with the elimination of neurological disorders. The later treatment is started, the worse the prognosis. Thus, EPG in the stage of decompensation, treatment of which began late, has a chance of death of up to 40%. And surviving patients often cannot get rid of neurological defects. This means that timely diagnosis and treatment is the key to quality of life, and life as such.
Author of the article: neurologist Lidiya Rashidovna Magdoteva
Diagnosis of the disorder
When making a diagnosis, it is necessary to differentiate epidural hematoma from subdural hematoma. For this purpose, the computed tomography method is used. In this case, the EG has the appearance of a biconvex lens, and the SG has a concave crescent shape.
Diagnostics also allows us to identify the severity of the process, which is determined by the time interval from the moment of injury, after which the first signs of the disorder appeared.
Symptomatically, ES is diagnosed by the presence of the following signs:
- the presence of a light gap;
- increase in pupil size;
- partial paralysis;
- arrhythmia and high blood pressure;
- pain localized in a specific place;
- the presence of edema of the membrane.
Treatment
The diagnosis of epidural hematoma is an indication for emergency surgery. A craniotomy is performed to remove liquid blood and blood clots using an aspirator. Then the source of bleeding is found and careful hemostasis is carried out. After placing a bone flap in place, the wound is sutured.
Conservative treatment methods involve managing the patient in the postoperative period and preserving the vital functions of his body. You can refrain from surgery if the volume of the hematoma is insignificant and there is no phenomenon of decompression and dislocation of the brain.
10.1. Epidemiology
According to the literature, the frequency of eggadural hematomas (EDH) among observations of initially hospitalized victims with TBI varies widely from 0.54% to 9%. The dispersion of indicators is due to the characteristics of neurotraumatology clinics: the percentage of ED^ is lower where all acute TBI is treated,
and* increases sharply with a concentration of victims with only severe TBI.
On average, the proportion of EDH in the structure of TBI
does not exceed 1.5-2%. Isolated EDHs account for up to 1/4 of all cases of brain-compressing intracranial hemorrhages.
Widespread use of CT and MRI
led
to
a significant increase in the intravital detection of EDH, primarily due to the asymptomatic and low-symptomatic forms of their clinical course, which is more often observed in mild TBI.
The age spectrum of EDH is dominated by young people 16-25 years old. FA Guitierrez et al state that about 60% of all patients with EDH occur in people under 20 years of age. S. Kwiatkowski emphasizes that EDH mainly occurs in patients under 40 years of age. At the same time ,
In infants and children under 2 years of age, epidural hematomas are rare, which is due to a denser fusion of the dura mater with the inner plate of the skull bones than in adults. For the same reason, the elderly and old people have specific
The weight of the EDH also decreases compared to young and middle age.
Reflecting the general structure of TBI
by gender, EDH occurs 4 times more often in men than
in
women. In children, this ratio changes: up to the age of two years, the frequency of occurrence of EDH is the same in boys and girls; later, EDH in boys is approximately three times higher than EDH in girls. In old age and old age, EDH develops twice as often in men as in women.