Anatomical features
There are noticeable differences in the anatomy of the pudendal nerve in men and women due to the structural features of the small pelvis.
For the former, the concept of genital organs includes more structures than for the latter and it is more branched. In addition, in women these nerve fibers are located more compactly. However, in both men and women, the pudendal nerve is a paired structure that arises from the spinal plexus. In people of both sexes, this nerve is divided into two large branches (femoral and inguinal), which are responsible for innervation:
- bladder sphincters;
- perineal tissue;
- levator ani muscle;
- sphincters of the rectum.
The inguinal branch in men and women performs different functions:
- In men, it is responsible for sensitivity and vegetative processes in the cavernous bodies of the penis and scrotum.
- In women, it performs the same functions in relation to the labia majora and minora, and the clitoris.
This structure, as well as the presence of vegetative fibers, ensures the automatic operation of various muscle groups responsible for urination and defecation, without the participation of consciousness.
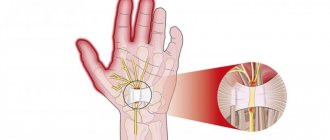
The pudendal nerve is short in length. But this is a very important nerve of the last sacral plexus (if you move from the brain). It is located in the pelvic cavity and along the way it bypasses the ischium. It then divides into three branches:
- Rectal.
- Perineal.
- Dorsal nerve of the clitoris or penis.
Clinical picture
Sacrococcygeal plexus The
pudendal nerve is a paired nerve, the branches of which are located on the right and left sides of the human body.
- Nerve roots – S2-S4
- Sensory branches - innervate the external genitalia of men and women, as well as the skin around the anus, anal canal and perineum.
- Motor branches - innervate a number of pelvic floor muscles, the external urethral sphincter and the external anal sphincter.
- Autonomic - carry sympathetic nerve fibers to the skin of the dermatomal area S2-S4.
Entrapment of the pudendal nerve at different levels (sciatic spine, sacrospinous and sacrotuberous ligaments, Alcock's canal) is the cause of disabling, chronic and intractable pelvic pain. This pain is highly varied and complex because it is often associated with a variety of functional symptoms that are confusing.
The clinical characteristic of PN is pain in the pelvic area, which increases during the day while sitting and decreases if the patient gets up or lies down. Symptoms also include sexual dysfunction and difficulty urinating and/or defecating. To confirm the diagnosis, it is recommended to use the Nantes criteria. The pain is similar to that experienced by patients with compressive neuropathy.
In most cases, patients describe neuropathic pain as burning, tingling, or numbing, worsening when sitting.
At an early stage, the pain may only appear while sitting, but over time it becomes more or less constant and only gets worse from sitting. Many patients with PN are unable to sit down at all. It is curious that sitting on the toilet is much less painful for them, which is most likely due to the fact that in this case the pressure is not on the pelvic floor muscles, but on the ischial tuberosities. Basically, pain with PN only gets worse as the day goes on.
The pudendal nerve tract begins significantly above the innervated zones, which is why doctors often call it the femoral-genital nerve. It passes through the muscles of the lower back and over the ureter, and then extends to the groin area. At this point it is divided into 2 branches:
- Femoral;
- Inguinal (genital).
The femoral-genital nerve, passing into the inguinal branch, has 2 options for continuation depending on the gender of the person:
- Male. It exits through the canal along with the spermatic cord and follows into the scrotum;
- Female. In the case of the weaker sex, the pudendal nerve leaves the canal along with the round ligament of the uterus and smoothly passes into the skin of the labia majora.
The inguinal nerve in women and men innervates the following tissues:
- Muscle tissue of the anus;
- The outer skin of the anus and genitals;
- Anal sphincter;
- Musculature of the perineum;
- Female clitoris;
- Male cavernous bodies of the penis;
- Bladder sphincter.
It performs the last two functions thanks to the vegetative fibers in its composition. It is the autonomous (vegetative) part of the nervous system that is responsible for many systems that are not controlled by human consciousness, for example, constriction of the pupils, heart rhythm, etc.
Damage to this nerve is caused by pinching of the piriformis muscle, ligaments, etc. Sometimes the cause of such compression lies in the injury received, as a result of which the pelvic bones were crushed or ligaments were torn. This type of neuralgia is usually accompanied by a feeling of tension and inflammation.
Pudendal nerve and entrapment, genitofemoral nerve neuropathy
There are many nerve pathways in the human body, each of which innervates a specific area. Among them we can distinguish the pudendal nerve, which in medicine is called the genital nerve.
It is responsible for the innervation of the pelvic floor muscles, and when this bundle is pinched, people experience chronic pain in the pelvic area. This phenomenon usually occurs due to compressive neuropathy. It represents compression (pinched nerve).
In men, this problem occurs 2-3 times more often than in women due to anatomical features.
Causes of inflammation
Traction-compression neuropathy of the left or right nerve tract occurs in the Alcock canal. Therefore, pinching of the pudendal nerve that occurs in this area is called Alcock syndrome.
Among other types of neuropathy characteristic of this nerve pathway, one can distinguish the femoral-genital form. It manifests itself mainly due to groin injury or the development of an inguinal hernia. Ilioinguinal nerve neuropathy also falls into this group.
It occurs due to the appearance of scars on muscle tissue, which are a consequence of surgery.
Pinching of the pudendal nerve occurs mainly due to the following factors:
- Trauma sustained during childbirth;
- Spasm of the muscle tissue of the anus;
- Pelvic fracture;
- Development of malignant oncological diseases;
- High tone of the piriformis muscle;
- Complications of herpes;
- Spasm of the obturator internus muscle;
- Compression of the pudenda due to riding a horse or bicycle.
Symptoms
Compressive neuropathy of the pudendal nerve is characterized by many symptoms, but their severity is rather mild. For this reason, it is extremely difficult to diagnose pathology. Among the main manifestations of the disease are the following:
- Aching pain in the pelvic area;
- Genital dysfunction;
- Constant feeling of discomfort in the anal area;
- Involuntary urination;
- False sensation of a foreign object in the groin area;
- Feeling of burning and slight tingling in the groin area;
- Excessively high sensitivity of the skin in the groin area.
In women, severe itching and burning in the genital area can be added to the main symptoms of neuropathy. In a sitting position, these symptoms intensify significantly.
In more rare cases, the following symptoms are observed:
- Abnormal bowel movements (constipation);
- Numbness of the genitals;
- Pain during sexual intercourse and when urinating.
What functions does it perform?
- Innervates the muscle that elevates the anus and sphincter.
- Innervates the sphincter of the urinary canal.
- Innervates the female clitoris and the cavernous bodies in men.
- Makes the skin of the anus and external genitalia sensitive.
From the above list it is clear that the pudendal nerve plays a very important role both in the intimate life of a person and during bowel movements and urination. This nerve includes a large number of autonomic fibers that ensure the correct functioning of the sphincters without the use of conscious tension. After all, people never think, do not try to control and do not consciously squeeze their muscles so as not to urinate or defecate completely accidentally at the wrong moment. These functions are performed by the autonomic fibers that enter the pudendal nerve.
What to do when the pudendal nerve is pinched or inflamed? Symptoms and treatment of the disease
The pudendal nerve, also called the pudendal nerve, is quite often the cause of chronic pain in the pelvic area that occurs in adults. This is caused in most cases by a pinched nerve, called compression neuropathy. The pudendal nerve is pinched more often in women. This happens three times less often in men.
Anatomical features
The pudendal nerve is short in length. But this is a very important nerve of the last sacral plexus (if you move from the brain). It is located in the pelvic cavity and along the way it bypasses the ischium. It then divides into three branches:
- Rectal.
- Perineal.
- Dorsal nerve of the clitoris or penis.
What functions does it perform?
- Innervates the muscle that elevates the anus and sphincter.
- Innervates the sphincter of the urinary canal.
- Innervates the female clitoris and the cavernous bodies in men.
- Makes the skin of the anus and external genitalia sensitive.
From the above list it is clear that the pudendal nerve plays a very important role both in the intimate life of a person and during bowel movements and urination.
This nerve includes a large number of autonomic fibers that ensure the correct functioning of the sphincters without the use of conscious tension.
After all, people never think, do not try to control and do not consciously squeeze their muscles so as not to urinate or defecate completely accidentally at the wrong moment. These functions are performed by the autonomic fibers that enter the pudendal nerve.
Trouble may occur due to the piriformis muscle located in the pelvic cavity or due to compression between a pair of ligaments.
In addition, the pudendal nerve can be damaged after unforeseen situations, which include a car accident or a fall from a height. In such situations, a fracture of the pelvic bones may occur. Very often, the cause of chronic pain is damage to the nerve during childbirth or its involvement in the growth of a malignant tumor.
It is worth mentioning that certain types of human activities can also lead to pinching of the pudendal nerve over time. This includes riding a bicycle or horse.
Pudendal nerve: symptoms of neuropathy
As with any other pinching, symptoms include pain, sensory disturbances, muscle weakness and disorders of the autonomic system.
When the pudendal nerve is pinched, the symptoms in women and men are similar:
- Painful sensations appear in the perineum.
- The pain has a burning tint.
- There is discomfort in the genitals and anus.
- Urinary and fecal incontinence, which may be incomplete, that is, manifest itself in the form of drip incontinence or spotting.
- Skin sensitivity decreases in these areas, and a sensation of “goosebumps” appears.
- There may be an unpleasant presence of something foreign in the anus and urethra.
- Sexual disorders such as lack of orgasm and impotence may occur.
When the pudendal nerve is pinched, symptoms in women whose treatment should not be delayed are observed in the lower part of the vagina. This causes great discomfort.
Severe pain may be felt during sexual intercourse and walking - these are the symptoms in men if the pudendal nerve is pinched.
Treatment is required immediately, as the pain becomes burning, and touching the skin becomes painfully unpleasant.
The sensations can be described as the presence of a cold or hot foreign object or electric shock. In general, a pinched pudendal nerve entails a large number of unpleasant symptoms.
Diagnosis of pinching
With the above painful and unpleasant sensations, a person is simply not able to endure it for long, because it is not the same pain as in a leg or arm. Most often, those suffering from neuropathy turn to either a neurologist or a proctologist if they experience disorders associated with the anal sphincter, or problems with fecal and urinary incontinence.
In rare cases, patients may go to a sex therapist. But a good specialist, using simple questions, should be able to identify organic disorders and then refer the patient to the appropriate doctor. Pinched pudendal nerve is diagnosed with the following tests and complaints:
- All those complaints that were listed earlier.
- Patients may note that when something cold is applied to the perineum, temporary relief occurs and the burning pain begins to subside. This symptom indicates that the nerve damage is neuropathic in nature.
- When using a trial therapeutic and diagnostic nerve block with novocaine, the severity of symptoms decreases or completely eliminates all suffering for the duration of the painkiller, which lasts from 12 hours to 3 days.
- The nature of the pain indicates that pinching has occurred (unpleasant sensations when touched and all kinds of itching, burning and a feeling of “pins and needles”).
- When performing ultrasound and Dopplerography of the pelvis and perineum, in almost all cases when the pudendal nerve is pinched, a slowdown in the speed of blood flow in the nearby pudendal artery is observed. Since it runs along the same channel as the nerve, narrowing of the artery indicates that it, too, has been compressed.
- A very important criterion for diagnosis is that pain increases in a person in a sitting position and decreases when the patient lies on his back. Pinching of the pudendal nerve is also characterized by damage on only one side. This is where the disorders are felt.
In addition to these diagnostic criteria, when palpating the perineum, you can find characteristic areas that are pain points reflecting muscle spasms.
It is important that the pathology of the pudendal nerve is closely related to the development of myofascial syndrome, which is much less treatable due to the deep location of the muscles.
In addition, pinched pudendal nerves greatly increase depression and anxiety, and people become more susceptible to negative events.
Treatment of pudendal nerve neuropathy
As in other situations, treatment of this disease must be comprehensive.
What are the basic principles of treating neuropathy?
- Influencing the characteristic pain pattern of pinching with the help of gabapentin, which is part of the medicine.
- Regular nerve blocks using hormones and anesthetics.
- The use of centrally acting muscle relaxants, which allow the muscles to relax, resulting in a decrease in the tone of the piriformis muscle.
- The use of physiotherapeutic effects, which include electrophoresis and phonophoresis.
- Taking B vitamins, which are part of the blockade, as well as in tablet form.
Other procedures
Often, treatment of a pinched pudendal nerve requires the support of a good psychologist who performs correctional therapy and prescribes antidepressants.
You may need to prescribe vaginal or rectal suppositories that contain diazepam.
The patient may be prescribed special physical exercises, the meaning of which is to slowly compress and relax the muscles located in the perineum.
In situations where conservative treatment methods do not have a positive effect, decompressive surgeries are performed. They are performed in special centers for the treatment of chronic pelvic pain.
Long-term treatment
It must be remembered that treatment of neuropathy of the pudendal nerve is a very long process, during which all recommendations of the attending physician should be followed. The recovery period takes at least six months.
Treatment of the disease should be carried out only in a hospital setting, as this will allow doctors to take control of the healing process, as well as successfully select a set of means that will be used for proper treatment. After all, a person may be allergic to some medications, which will only worsen the situation.
Results
Thus, it was discussed what the pudendal nerve is, symptoms and treatment for its pinching, and diagnosis.
In order to avoid this disease, it is recommended to be careful and avoid injury, as well as to lead an active lifestyle, exercise and have an active sex life.
Well, if trouble does happen, then you must strictly follow the doctors’ recommendations.
Source: https://FB.ru/article/282966/chto-delat-kogda-zaschemlen-ili-vospalen-sramnoy-nerv-simptomyi-i-lechenie-neduga
Pathophysiology
Pathological conditions associated with pudendal nerve damage
The exact mechanism of nerve dysfunction and damage depends on the etiology. The damage may be one or two sided.
Causes of PN can include compression, stretching, direct nerve injury, and radiation. Pudendal neuralgia is a functional pinching in which pain occurs during compression or stretching of the nerve. Symptoms worsen over time due to repeated microtrauma, ultimately leading to persistent pain and dysfunctional complaints. The pudendal nerve becomes pinched during prolonged sitting or cycling.
Pudendal neuropathy can be caused by stretching of the nerve due to straining during labor or constipation. Other etiological factors include fitness classes, working out in the gym, weighted squats, leg presses, karate, kickboxing and roller skating. Sports popular among young people are considered a risk factor, which may be associated with bone remodeling of the ischial spine.
Symptoms of trochlear nerve damage
- Diplopia (double vision) is a phenomenon that occurs when looking at an object with both eyes. When the trochlear nerve is affected, it occurs in all directions of gaze except the upward direction;
- Sometimes, with paresis of the trochlear nerve, there is a tilt of the head to the shoulder (to compensate for double vision) in the direction opposite to the affected one.
- Convergent strabismus (strabismus is a position of the eyes characterized by non-crossing of the visual axes of both eyes on a fixed object; the eyes look in different directions, the line of their gaze is not parallel; with convergent strabismus, the squinting eye deviates towards the nose)
Other procedures
Often, treatment of a pinched pudendal nerve requires the support of a good psychologist who performs correctional therapy and prescribes antidepressants. You may need to prescribe vaginal or rectal suppositories that contain diazepam. The patient may be prescribed special physical exercises, the meaning of which is to slowly compress and relax the muscles located in the perineum.
In situations where conservative treatment methods do not have a positive effect, decompressive surgeries are performed. They are performed in special centers for the treatment of chronic pelvic pain.
In situations where conservative treatment methods do not have a positive effect, decompressive surgeries are performed. They are performed in special centers for the treatment of chronic pelvic pain.
Long-term treatment
It must be remembered that treatment of neuropathy of the pudendal nerve is a very long process, during which all recommendations of the attending physician should be followed. The recovery period takes at least six months.
Treatment of the disease should be carried out only in a hospital setting, as this will allow doctors to take control of the healing process, as well as successfully select a set of means that will be used for proper treatment. After all, a person may be allergic to some medications, which will only worsen the situation.