Structure of the optic nerve
To understand the causes of diseases and treatment methods, it is necessary to know the structure of the optic nerve. Its average length in adults varies from 40 to 55 mm, the main part of the nerve is located inside the orbit - the bone formation in which the eye itself is located. The nerve is surrounded on all sides by parabulbar tissue - adipose tissue.
It has 4 parts:
- Intraocular.
- Orbital.
- Canalicular.
- Cranial.
Optic disc
The optic nerve begins in the fundus of the eye, in the form of the optic nerve disc (OND), which is formed by processes of retinal cells, and it ends in the chiasm, a kind of “crossroads” located above the pituitary gland inside the skull. Since the optic disc is formed by a collection of nerve cells, it protrudes slightly above the surface of the retina, which is why it is sometimes called the “papilla”.
The area of the optic disc is only 2-3 mm2, and the diameter is about 2 mm. The disc is not located strictly in the center of the retina, but is slightly displaced to the nasal side, and therefore a physiological scotoma is formed on the retina - a blind spot. The optic disc is practically not protected. The nerve sheaths appear only when it passes through the sclera, that is, at the exit from the eyeball to the orbit. The blood supply to the optic disc is carried out by small processes of the ciliary arteries and is only segmental in nature. That is why, when blood circulation is impaired in this area, a sharp and often irreversible loss of vision occurs.
Optic nerve sheaths
As already mentioned, the optic nerve head itself does not have its own membranes. The optic nerve sheaths appear only in the intraorbital part, at the site where it exits the eye into the orbit.
They are represented by the following tissue formations:
- Pia mater.
- Arachnoid (arachnoid, or choroid) membrane.
- Dura mater.
All membranes envelop the optic nerve layer by layer until it exits the orbit into the skull. Subsequently, the nerve itself, as well as the chiasm, are covered only by a soft membrane, and already inside the skull they are located in a special tank formed by the subarachnoid (choroidal) membrane.
Blood supply to the optic nerve
The intraocular and orbital part of the nerve have many vessels, but due to their small size (mainly capillaries), the blood supply remains good only under conditions of normal hemodynamics throughout the body.
The optic disc has a small number of small vessels - these are the posterior short ciliary arteries, which only segmentally supply this important part of the optic nerve with blood. The central retinal artery supplies blood to the deeper structures of the optic disc, but again, due to the low pressure gradient in it and its small caliber, blood stagnation, occlusion and various infectious diseases often occur.
The intraorbital part already has a better blood supply, which comes mainly from the vessels of the pia mater, as well as from the central artery of the optic nerve.
The cranial part of the optic nerve and the chiasm are also richly supplied with blood due to the vessels of the soft and subarachnoid membranes, into which blood enters from the branches of the internal carotid artery.
Symptoms
Damage to the optic nerve is a pathology characterized by inflammation of the nerve sheaths or fibers. Its symptoms may be: pain when moving the eyeballs, blurred vision, changes in color perception, photopsia, the eye may swell.
Patients may complain of a decrease in the peripheral field of vision, vomiting, nausea, darkening of the eyes, and fever. Each form of optic nerve damage has its own symptoms.
Symptoms characteristic of optic nerve atrophy of any etiology:
- decrease in distance visual acuity, and patients note that vision has decreased sharply, more often in the morning, can be reduced to hundredths of a unit, but sometimes remains high;
- loss of the visual field, which depends on the location of the pathological process; Central scotomas (“spots”) and concentric narrowing of the visual field may be observed;
- impaired color perception;
- complaints characteristic of the underlying disease.
There are primary and secondary atrophy of the optic nerves, partial and complete, complete and progressive, unilateral and bilateral.
The main symptom of optic nerve atrophy is a decrease in visual acuity that cannot be corrected. Depending on the type of atrophy, this symptom manifests itself differently.
Thus, as atrophy progresses, vision gradually decreases, which can lead to complete atrophy of the optic nerve and, accordingly, to complete loss of vision. This process can take place from several days to several months.
With partial atrophy, the process stops at some stage and vision stops deteriorating. Thus, progressive atrophy of the optic nerves is distinguished and complete.
Visual impairment due to atrophy can be very diverse. This can be a change in visual fields (usually narrowing, when “lateral vision” disappears), up to the development of “tunnel vision”, when a person looks as if through a tube, i.e. sees objects that are only directly in front of him, and scotomas often appear, i.e. dark spots in any part of the visual field; It could also be a color vision disorder.
Since the optic nerve carries visual images, the most common signs of its inflammation are the following:
- sudden deterioration of vision in one or both eyes;
- the appearance of black and white vision. Color vision, being more perfect, suffers first;
- Pain appears when moving the eyes. An optional symptom that may be absent if there are no signs of classic inflammation and swelling of the retrobulbar tissue;
As noted above, the defining symptom here is a sharp decrease in human visual acuity. It can manifest itself in different ways, depending on the type of atrophy. If the form is partial, the deterioration of vision simply stops at some stage, after which it stops falling. Accordingly, the progressive form is characterized by the fact that a person begins to see worse and worse and, in the end, completely loses vision.
Vision with ocular atrophy is impaired in a variety of ways. For example, the field of vision changes (as a rule, they begin to narrow), and peripheral vision completely deteriorates. A person experiences symptoms of “tunnel” vision, when all objects are visible as if through a narrow tube.
READ MORE: Serous meningitis symptoms, treatment
The pathogenetic course and symptoms of optic neuropathy directly depend on the etiological factors that caused this or that disorder, and are characterized by some differences in the impairment of visual functionality.
Thus, anterior ischemic optic neuropathy is characterized by:
- gradual painless loss of vision, usually worsening during morning awakening;
- loss of the lower fields of vision in the early stages of the disease, then the process includes the loss of the upper areas.
Posterior optic neuropathy is caused by spontaneous and sudden complete loss of vision at a certain point in the development of the pathological process.
Characteristic symptoms of optic neuritis are:
- sudden decrease in visual acuity;
- loss of color characteristics;
- pain in the eye sockets;
- photopsia;
- phenomena of visual hallucinations.
Optic neuritis is a treatable disease, with good remission and prognosis rates. However, in complicated cases, it is capable of leaving irreversible marks in the visual neurostructure, which can provoke neuropathic progress.
The toxic etiology of neuropathies usually causes acute loss of vision, but with a favorable prognosis if you immediately consult a doctor. Irreversible processes of destructive changes in the neurons of the optic nerve begin 15-18 hours after taking methanol, during which time it is necessary to use an antidote, as a rule, ethyl alcohol.
Other types of neuropathic conditions of the optic nerve have identical symptoms of gradual loss of visual acuity and color qualities. It is worth noting that the perception of red shades always decreases first, followed by all other colors.
Regardless of the level of damage (above or below the chiasm), there are two reliable signs of optic nerve atrophy - loss of visual fields (“anopsia”) and decreased visual acuity (amblyopia). How pronounced they will be in a particular patient depends on the severity of the process and the activity of the cause that caused the disease. Let's take a closer look at these symptoms.
Loss of visual fields (anopsia)
What does the term "field of view" mean? Essentially, this is just an area that a person sees. To imagine it, you can close half of your eye on either side. In this case, you see only half of the picture, since the analyzer cannot perceive the second part. We can say that you have “lost” one (right or left) zone. This is exactly what anopsia is - the disappearance of the field of vision.
Neurologists divide it into:
- temporal (half of the image located closer to the temple) and nasal (the other half from the side of the nose);
- right and left, depending on which side the zone falls on.
With partial atrophy of the optic nerve, there may be no symptoms, since the remaining neurons transmit information from the eye to the brain. However, if a lesion occurs through the entire thickness of the trunk, this sign will certainly appear in the patient.
Functions of the optic nerve
There are not very many of them, but they all play a significant role in human life.
List of main functions of the optic nerve:
- transmission of information from the retina to the cerebral cortex through various intermediate structures;
- quick response to various external stimuli (light, noise, explosion, approaching car, etc.) and as a result - operational reflex defense in the form of closing the eyes, jumping, withdrawing hands, etc.;
- reverse transmission of impulses from the cortical and subcortical structures of the brain to the retina.
Treatment
Treatment of optic nerve atrophy with medication and physiotherapy:
- Drug treatment is effective only in case of compensation of the underlying disease and with visual acuity of at least 0.01. If the cause of atrophy is not eliminated, a decrease in visual function will also be observed during neuroprotective therapy.
- Physiotherapy is carried out if there are no contraindications to this type of treatment. Main contraindications: stage 3 hypertension, severe atherosclerosis, fever, neoplasms (tumors), acute purulent-inflammatory processes, condition after a heart attack or stroke for 1-3 months.
Stages of treatment:
- Treatment of the underlying disease, if identified, is carried out by an appropriate specialist, often in a hospital setting. The prognosis of the course of optic nerve atrophy depends on timely detection of the disease.
- Giving up bad habits allows you to stop the progression of the disease and preserve the patient’s visual functions.
- Direct acting neuroprotective agents protect the axons (fibers) of the optic nerve. The choice of a specific drug is carried out taking into account the leading role of one or another pathological factor (hemodynamic impairment or regional ischemia).
- Indirectly acting neuroprotective agents affect risk factors that contribute to optic nerve cell death. The choice of drug is carried out individually.
- Magnetotherapy.
- Electro-laser stimulation of the optic nerve.
- Acupuncture.
The last three points are physiotherapeutic procedures. They are prescribed to improve blood circulation, stimulate reduced metabolic processes, increase tissue permeability, improve the functional state of the optic nerve, which ultimately corrects the state of visual functions. All treatment is carried out in a hospital setting.
Direct acting neuroprotective agents:
- methylethylpyridinol (Emoxipine) 1% solution for injection;
- pentahydroxyethylnaphthoquinone (Histochrome) 0.02% solution for injection.
Neuroprotective agents of indirect action:
- Theophylline tablets 100 mg;
- Vinpocetine (Cavinton) tablets 5 mg, solution for injection;
- Pentoxifylline (Trental) injection solution 2%, tablets 0.1 g;
- Picamilon tablets 20 mg and 50 mg.
Treatment of optic atrophy is a very difficult task for doctors. You need to know that destroyed nerve fibers cannot be restored.
One can hope for some effect from treatment only by restoring the functioning of nerve fibers that are in the process of destruction, which still retain their vital functions. If this moment is missed, then vision in the affected eye can be lost forever.
When treating atrophy, it is necessary to keep in mind that this is often not an independent disease, but a consequence of other pathological processes affecting various parts of the visual pathway. Therefore, treatment of optic nerve atrophy must be combined with elimination of the cause that caused it.
If the cause is eliminated in a timely manner and if atrophy has not yet developed, normalization of the fundus picture and restoration of visual functions occurs within 2-3 weeks to 1-2 months.
Treatment is aimed at eliminating edema and inflammation in the optic nerve, improving its blood circulation and trophism (nutrition), restoring the conductivity of not completely destroyed nerve fibers.
But it should be noted that the treatment of optic nerve atrophy is long-term, its effect is weak, and sometimes completely absent, especially in advanced cases. Therefore it should be started as early as possible.
READ MORE: Laryngotracheitis in a child: symptoms and treatment of the disease
As mentioned above, the main thing is the treatment of the underlying disease, against the background of which complex treatment of optic nerve atrophy is carried out. For this, various forms of drugs are prescribed: eye drops, injections, both general and local; tablets, electrophoresis. Treatment is aimed at
Treatment tactics for toxic damage to the optic nerve depend on the stage and characteristics of the disease. At stage I, patients are indicated for detoxification therapy.
Intensive dehydration and administration of anti-inflammatory drugs are recommended at stage II. At stage III, it is advisable to administer antispasmodics.
With the development of stage IV, in addition to vasodilators, the complex of treatment measures should include immunomodulators, multivitamin complexes and physiotherapeutic methods of treatment (magnetic therapy, physioelectric therapy in combination with electrolaser therapy).
The most difficult task for the attending physician is to correctly prescribe treatment. This is explained by the fact that it is no longer possible to restore dead nerve fibers, although a certain effect in this area can be achieved. We are talking about fibers that are in the active stage of destruction.
All treatment methods can be divided into three types:
- Conservative. The doctor prescribes a whole series of drugs with different spectrum of effects. For example, papaverine and no-spa improve blood circulation in the affected nerve, nootropil improves the functions of the nervous system, and hormonal drugs stop the process of inflammation.
- Therapeutic. Patients are prescribed a fairly wide range of procedures, including magnetic stimulation, acupuncture, laser or electric current stimulation. As a rule, patients undergo such treatment every few months in separate courses.
- Surgical. It involves the elimination of pathological formations compressing the patient’s nerve, implantation of biogenic materials and subsequent ligation of the temporal artery. This improves the overall blood circulation of the nerve and its further vascularization.
The main direction of therapeutic regimens for the treatment of optic neuropathy is to inhibit the pathological processes developing in the parenchyma of the optic trunk, and, if possible, completely eliminate them, as well as to restore lost visual qualities.
As already mentioned, optical neuropathy is a secondary pathology initiated by other diseases. Based on this, first of all, primary diseases are treated under regular monitoring of the condition of the optic nerve and attempts to restore its organic characteristics.
Several methods are available for this purpose.
- Magnetic stimulation of optic nerve neurons using an alternating electromagnetic field.
- Electrical stimulation of the nerve trunk by conducting currents of a special frequency and strength through the parenchyma of the optic nerve. This method is invasive and requires a highly qualified specialist.
The essence of both methods is to stimulate the metabolic processes of optic nerve fibers, which partially contributes to their regeneration due to the body’s own forces.
One of the most effective treatments for optic neuropathy is therapy through autologous stem cell transplantation.
The general background of each therapeutic regimen is traditional conservative support.
- Vasodilators.
- Tonics.
- B vitamins.
- In some cases, especially toxic neuropathy, blood transfusions are used.
Surgical treatment is the main method of treatment for compression of the optic nerve, its trauma or infiltration.
There is a widespread belief in society that “nerve cells do not recover.” This is not entirely correct. Neurocytes can grow, increase the number of connections with other tissues and take on the functions of dead “comrades”. However, they do not have one property that is very important for complete regeneration - the ability to reproduce.
Can optic nerve atrophy be cured? Definitely not. If the trunk is partially damaged, medications can improve visual acuity and fields. In rare cases, even virtually restore the patient's ability to see to normal levels. If the pathological process completely disrupts the transmission of impulses from the eye to the brain, only surgery can help.
The visual pathway, or the pattern of movement of the visual impulse
The anatomical structure of the visual pathway is complex.
It consists of two sequential sections:
- Peripheral part . It is represented by rods and cones of the retina (1 neuron), then by bipolar cells of the retina (2 neuron), and only then by long cell processes (3 neuron). Together, these structures form the optic nerve, chiasm, and optic tract.
- Central part of the visual pathway . The optic tracts end their path in the external geniculate body (which is the subcortical center of vision), the posterior part of the optic thalamus and the anterior quadrigeminal. Further, the processes of the ganglia form the optic radiation in the brain. A cluster of short axons of these cells, called Wernicke's area, from which long fibers arise that form the sensory visual center - Brodmann's cortical area 17. This area of the cerebral cortex is the “director” of vision in the body.
Normal ophthalmic appearance of the optic disc
When examining the fundus of the eye using ophthalmoscopy, the doctor sees the following on the retina:
- The optic disk is usually light pink in color, but with age, with glaucoma or atherosclerosis, the disc becomes pale.
- There are normally no inclusions on the optic disc. With age, small yellowish-gray disc drusen (deposits of cholesterol salts) sometimes appear.
- The contours of the optic disc are clear. Blurred disc contours may indicate increased intracranial pressure and other pathologies.
- The optic disc normally does not have pronounced protrusions or depressions; it is almost flat. Excavations are observed with high myopia, in the later stages of glaucoma and other diseases. Disc edema is observed during congestion both in the brain and in the retrobulbar tissue.
- The retina in young and healthy people is bright red, without various inclusions, and is closely adjacent to the choroid over its entire area.
- Normally, there are no bright white or yellow stripes along the vessels, as well as hemorrhages.
Diseases and pathological changes of the optic nerve
All diseases of the optic nerve are usually divided by reason:
- Vascular - anterior and posterior ischemic neuroopticopathy.
- Traumatic . There can be any localization, but most often the nerve is damaged in the canalicular and cranial parts. In case of fractures of the skull bones, mainly the facial part, a fracture of the process of the sphenoid bone, in which the nerve passes, often occurs. With extensive hemorrhages in the brain (road accidents, hemorrhagic strokes, etc.), compression of the chiasm area may occur. Any damage to the optic nerve can result in blindness.
- Inflammatory diseases of the optic nerve - bulbar and retrobulbar neuritis, optochiasmatic arachnoiditis, and papillitis. Symptoms of inflammation of the optic nerve are in many ways similar to other lesions of the optic tract - vision deteriorates quickly and painlessly, and fog appears in the eyes. Treatment of retrobulbar neuritis very often results in complete restoration of vision.
- Non-inflammatory diseases of the optic nerve . Frequent pathological phenomena in the practice of an ophthalmologist are represented by edema of various etiologies and optic nerve atrophy.
- Oncological diseases . The most common tumor of the optic nerve is benign gliomas in children, which appear before the age of 10-12 years. Malignant tumors are rare and usually have a metastatic nature.
- Congenital anomalies - an increase in the size of the optic disc, hypoplasia of the optic nerve in children, coloboma and others.
Research methods for diseases of the optic nerve
For all neuro-ophthalmological diseases, diagnostic examinations include both general ophthalmological methods and special ones.
Common methods include:
- visometry - the classic definition of visual acuity with and without correction;
- perimetry is the most revealing examination method, allowing the doctor to determine the location of the lesion;
- ophthalmoscopy - with damage to the initial parts of the nerve, especially with ischemic opticopathy, pallor, disc excavation or swelling, its blanching or, conversely, injection are detected.
Special diagnostic methods include:
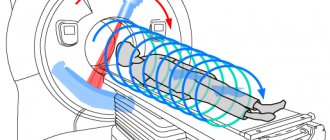
- Magnetic resonance imaging of the brain (to a lesser extent, computed tomography and targeted radiography). It is an optimal study for traumatic, inflammatory, non-inflammatory (multiple sclerosis) and oncological causes of the disease (optic nerve glioma).
- Fluorescein angiography of retinal vessels is the “gold standard” in many countries, which makes it possible to see in which area the cessation of blood circulation occurred, if anterior ischemic neuropathy of the optic nerve has occurred, to establish the localization of the blood clot, and to determine further prognosis for the restoration of vision.
- HRT (Heidelberg retinal tomography) is an examination that shows changes in the optic disc in great detail, which is very informative for glaucoma, diabetes, and optic nerve dystrophies.
- Ultrasound of the orbit is also widely used for damage to the intraocular and orbital nerves; it is very informative if a child is diagnosed with optic nerve glioma.
Causes
The causes of optic nerve atrophy may be different, but they all lead to either the development of edema or destruction of nerve fibers.
So, the main factors provoking the disease:
- eye diseases of varying severity (glaucoma, retinal occlusion, retinitis, optic neuritis, benign and malignant tumors);
- diseases of the central nervous system (tumor processes in the pituitary gland or posterior cranial fossa, brain abscess, meningitis, arachnoiditis, multiple sclerosis, hydrocephalus);
- trauma (traumatic brain injury, mechanical damage to the skull near the eye);
- bacterial infections (syphilis, tuberculosis);
- viral infections (flu, measles, rubella, herpes and common ARVI);
- parasitic infections (toxoplasmosis, toxocariasis);
- other reasons (alcohol poisoning, medications, drugs or tobacco, sudden blood loss, diabetes, anemia).
The optic nerve can atrophy as a result of a common acute respiratory infection, which causes complications in the eyes; naturally, such cases are rare, and yet they have occurred in practice.
In addition, this disease can simply be inherited by newborns from their parents.
Various reasons can provoke atrophy of varying severity, but if you don’t start treating the ailment that provoked the disease and the disease itself in a timely manner, things can end very badly for the patient - complete blindness.