Demyelinating optic neuropathy of the optic nerve is a pathology of the optic nerves, accompanied by their atrophic and degenerative lesions. As the disease progresses, specific clinical symptoms develop that are not characteristic of other diseases. Previously, in ophthalmological practice, this condition was referred to as “optic nerve atrophy,” but now doctors practically do not use this term.
Optic neuropathy is not considered a primary independent disease, but is a consequence of the development of other diseases, intoxications or traumatic injuries. Based on this, patients with this diagnosis often become patients of medical specialists of various specialties: ophthalmologists, endocrinologists, neurologists and often oncologists, maxillofacial surgeons. A comprehensive examination is an important factor in the success of the therapy.
Causes
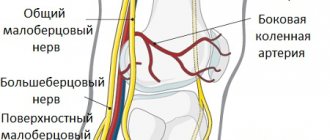
Anterior ischemic neuropathy occurs as a result of ischemia of the retinal, choroidal (prelaminar) and (laminar) layers of the optic disc against the background of circulatory disorders in the posterior short ciliary arteries. Posterior ischemic neuropathy is associated with impaired blood flow in the carotid and vertebral arteries.
Additionally, acute circulatory disorders of the optic nerve are provoked by arterial spasms, atherosclerotic lesions, and thromboembolism. In addition, the occurrence of the disease is associated with various systemic pathologies, which are the causes of hemodynamic disorders, disorders in the vascular system, and microcirculatory problems.
Quite often, ischemic neuropathy is detected in systemic atherosclerosis, arterial hypertension, temporal arteritis, periarteritis nodosa, obliterating arteritis and atherosclerosis, diabetes mellitus, disorders of the cervical spine, and thrombosis of the great vessels. Sometimes this disease can develop after massive acute gastrointestinal bleeding, trauma, surgery, anemia, arterial hypotension, blood diseases, after anesthesia, after hemodialysis.
Possible symptoms
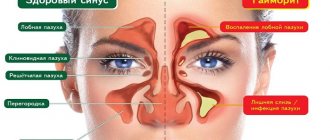
Signs depend on the location and scale of the process. In the first stages, partial or limited damage appears, then the disease develops into a total form. If the process develops in the intrabulbar region, anterior ischemic neuropathy is observed. This is an acute disorder of blood circulation, localized in the head. The main symptom is swelling of the organ, with the following symptoms occurring:
- rapid decrease in visual acuity;
- square loss from the field of view;
- dull headache;
- dilated retinal vessels;
- traces of pinpoint hemorrhage.
A person becomes completely blind in the total form of the pathology.
The acute form of the disease lasts for a month, then the swelling disappears. This means atrophy of nerve fibers begins. If swelling develops in the intraorbital region, posterior ischemic neuropathy is diagnosed. In this case, the damaged nerve is located immediately behind the eyeball. The symptoms are almost identical to the anterior type, but some changes in the fundus are observed. The danger is the total form, when all parts are damaged and optical neuropathy develops. This process leads to irreversible blindness. Ischemic neuroopticopathy is rare, but practically untreatable.
Ischemia is characterized by rapid development; sometimes the patient remembers the exact time when his vision began to decrease. But the first stages are completely asymptomatic.
Clinical features of ischemic neuropathy
In most cases, the lesion is unilateral, but one third of patients may exhibit bilateral changes. Sometimes the second eye is affected after some time (after several days or several years), more often within 2-5 years. Also quite often, anterior and posterior neuropathies are combined together with occlusion of the central artery.
Optical ischemic neuropathy usually develops acutely and can occur after sleep, exercise, or taking a hot shower or bath. Against this background, vision drops sharply, sometimes to the point of blindness. This condition develops over a period of several minutes to several hours. In this case, the patient, as a rule, clearly notes the time of onset of vision deterioration. Sometimes this condition is preceded by warning symptoms: pain behind the eye, periodically occurring in front of the eyes, intense headache.
This condition is usually accompanied by a disorder (in the form of loss in the lower part of the visual field, loss of the nasal and temporal halves of the visual field, concentric narrowing of the visual fields).
During the first 4-5 weeks, a period of acute ischemia develops. Then, over time, swelling of the optic disc decreases, hemorrhages resolve, and optic nerve atrophy forms. As a rule, visual field defects remain, but may become much smaller.
Symptoms
The course of ischemic optic neuropathy is often unilateral. Only in 30% of cases the disease affects both eyes. Moreover, bilateral eye damage is usually observed in those patients who did not undergo timely treatment for anterior ischemic neuropathy (neuropticopathy).
Most patients are diagnosed with both forms of the disease simultaneously.
Along with this pathology, lesions of the retinal vessels are noted.
Symptoms of optic nerve ischemia appear suddenly. Initially noted:
- a sharp decrease in visual acuity;
- impaired light perception;
- complete blindness (in case of total defeat).
These phenomena are temporary, and after a few minutes or hours, visual functions are restored on their own. In some cases, before the appearance of these signs, warning symptoms are noted:
- blurred vision;
- pain behind the eyeball;
- intense headaches.
Regardless of the form of the pathology, with ischemic neuropathy of the optic nerve, the quality of peripheral vision decreases, manifested in the form of:
- scotomas (blind spots in the field of vision);
- concentric narrowing of vision;
- loss of the lower, temporal or nasal region of the visual field (the patient does not see objects from the side of the temples, jaw or near the nose).
Clinical phenomena characteristic of the acute stage of the disease develop for about 4-5 weeks. At the end of this period, the swelling of the optic nerve subsides, and internal hemorrhages in the eyeball area resolve without intervention.
At this stage, optic nerve atrophy of varying severity develops and visual acuity (especially peripheral) is not restored. Often, after the acute period ends, the disease progresses.
Diagnosis of ischemic optic neuropathy
All patients with such a diagnosis should be consulted with related specialists: cardiac rheumatologist, endocrinologist, neurologist, hematologist.
In this condition, consultation with an ophthalmologist is carried out in full: an examination, a number of functional tests, ultrasound, X-ray, and electrophysiological studies are carried out.
- The visual acuity test reveals its decrease from minimal to the level of light perception. Visual field defects are also detected, characterizing damage to various parts of the optic nerve.
- Ophthalmoscopy reveals pallor, an increase in size due to ischemic edema of the optic disc, and its protrusion into. Retinal edema around the disc is also detected, and a “star figure” is detected in the macula. In the area of compression by edema, the veins are narrow, but on the periphery, on the contrary, they are dilated. Sometimes focal hemorrhages and exudation are detected.
- Angiography of retinal vessels reveals retinal angiosclerosis, age-related fibrosis, uneven caliber of arteries and veins, occlusion of cilioretinal arteries.
- In case of posterior ischemic optic neuropathy in the acute period, ophthalmoscopy does not reveal any features of the optic disc. However, when performing Dopplerography of the ophthalmic, supratrochlear, carotid, and vertebral arteries, blood flow disturbances in these vessels are often detected.
- Electrophysiological tests reveal a decrease in the functional parameters of the optic nerve.
- In the blood coagulation system, the predominance of coagulation processes is determined. The lipid profile shows hypercholesterolemia and increased low and very low density lipoproteins.
Ischemic optic neuropathy must be differentiated from retrobulbar neuritis, orbital and central nervous system tumors.
Eye clinics
Optic neuritis
Eye diseases6 June 2016
Eye diseases
Central retinal artery occlusion
Eye diseases6 June 2016
Eye examination
Visual field examination
Eye examinationNovember 29, 2017All on the topicNo comments yetLeave a comment All about vision on VKontakteAll about vision on Facebook
All about vision
Popular materials
10/31/2017 02:02:22textarea>
Patient's school. Glaucoma
Schools31 October 2017
New version of articles
World Sight Day. Reason to think
New version of articles October 16, 2018
Eye diseases
Cataract - cost of surgery
Eye diseasesDecember 22, 2014
Laser vision correction
Prices for laser vision correction.
Laser vision correctionDecember 8, 2014
Eye diseases
Cataract phacoemulsification surgery
Eye diseasesDecember 17, 2014
Vision in adults
Treatment of ischemic optic neuropathy
Assistance should be provided in the first hours from the onset of the disease to prevent the death of nerve cells. As an emergency aid, intravenous aminophylline, sublingual nitroglycerin, and inhalation of ammonia vapor are recommended. Subsequently, it is recommended to undergo a course of inpatient treatment.
Therapy for this disease is aimed at eliminating edema and restoring adequate trophism of the optic nerve, creating collateral blood supply pathways. An important point is the treatment of the underlying disease, restoration of adequate indicators of the blood coagulation system and lipid profile indicators, as well as normalization of blood pressure numbers.
It is recommended to prescribe diuretics (diacarb, lasix), vascular drugs and brain metabolites (cavinton, trental), thrombolytics (phenylin, heparin), glucocorticoids, vitamins B, C, E. Subsequently, magnetic therapy, electrical stimulation, and laser stimulation have proven themselves well.
Prognosis and prevention of ischemic optic neuropathy
Unfortunately, quite often, despite the therapy, the prognosis for ischemic neuropathy remains unfavorable: decreased vision and peripheral vision defects that have developed as a result of optic nerve atrophy persist. If both eyes are affected, low vision or complete blindness may occur.
To prevent the formation of the disease, adequate and timely treatment of vascular and systemic pathologies is necessary.
Patients with a history of ischemic optic neuropathy are subject to medical examination by an ophthalmologist.
The main sign of optic nerve atrophy is a decrease in visual acuity that cannot be corrected with glasses and lenses. With progressive atrophy, a decrease in visual function develops over a period of several days to several months and can result in complete blindness. In the case of incomplete atrophy of the optic nerve, pathological changes reach a certain point and do not develop further, and therefore vision is partially lost.
With atrophy of the optic nerve, disturbances in visual function can manifest themselves as concentric narrowing of the visual fields (disappearance of lateral vision), the development of “tunnel” vision, disturbance of color perception (mainly green-red, less often - blue-yellow part of the spectrum), the appearance of dark spots (scotoma) in areas fields of view. Typically, an afferent pupillary defect is detected on the affected side - a decrease in the pupillary reaction to light while maintaining a congenial pupillary reaction. Such changes can occur in one or both eyes.
Objective signs of optic nerve atrophy are revealed during an ophthalmological examination.
In children, optic nerve atrophy can be either congenital or develop later. In the first case, the child is already born with impaired vision. You may notice an impaired reaction of the pupils to light; also draws attention to the fact that the child does not see objects brought to him from any particular direction, no matter how close they are to his eye(s). Most often, a congenital disease is detected during a routine examination by an ophthalmologist, performed before the age of one year.
Optic nerve atrophy, which occurs in children 1–2 years old, can also go unnoticed without undergoing a routine examination by an ophthalmologist: children of this age do not yet understand what happened and cannot complain.
In some cases, attention is drawn to the fact that the child begins to rub his eyes and turn sideways towards the object.
Symptoms in older children are the same as in adults.
With timely treatment, if this is not a genetic disease in which nerve fibers are irreversibly replaced by connective tissue, the prognosis is more favorable than in adults.
Atrophy of the optic nerves in tabes and progressive paralysis has the character of simple atrophy. There is a gradual decrease in visual functions, a progressive narrowing of the visual field, especially in colors. Central scotoma occurs rarely. In cases of atherosclerotic atrophy, which appears as a result of ischemia of the optic nerve head tissue, a progressive decrease in visual acuity, concentric narrowing of the visual field, and central and paracentral scotomas are noted. Ophthalmoscopically, primary optic disc atrophy and retinal arteriosclerosis are determined.
For optic nerve atrophy caused by sclerosis of the internal carotid artery, nasal or binasal hemianopia is typical. Hypertension can lead to secondary optic nerve atrophy caused by hypertensive neuroretinopathy. Changes in the visual field are varied, central scotomas are rarely observed.
Atrophy of the optic nerves after profuse bleeding (usually gastrointestinal and uterine) usually develops after some time. After ischemic edema of the optic disc, secondary, pronounced atrophy of the optic nerve occurs with significant narrowing of the retinal arteries. Changes in the visual field are varied; narrowing of the boundaries and loss of the lower halves of the visual field are often observed.
Atrophy of the optic nerve from compression caused by a pathological process (usually a tumor, abscess, granuloma, cyst, chiasmatic arachnoiditis) in the orbit or cranial cavity usually occurs as simple atrophy. Changes in the visual field are different and depend on the location of the lesion. At the beginning of the development of optic nerve atrophy from compression, a significant discrepancy is often observed between the intensity of changes in the fundus and the state of visual functions.
With mildly expressed blanching of the optic nerve head, a significant decrease in visual acuity and sharp changes in the visual field are noted. Compression of the optic nerve leads to the development of unilateral atrophy; compression of the chiasm or optic tracts always causes bilateral damage.
Familial hereditary optic atrophy (Leber's disease) is observed in men aged 16−22 years in several generations; transmitted through the female line. It begins with retrobulbar neuritis and a sharp decrease in visual acuity, which after a few months turns into primary atrophy of the optic nerve head. With partial atrophy, functional and ophthalmoscopic changes are less pronounced than with complete atrophy. The latter is distinguished by a sharp pallor, sometimes a grayish color of the optic disc, amaurosis.
Vascular pathology of the optic nerve is one of the pressing problems in ophthalmology, due to the complexity of arteriovenous circulation in various parts of the optic nerve. Recently, the incidence of vascular diseases of the optic nerve, leading to low vision and blindness, has increased, including in young people. The causes of vascular pathology are varied. The most common diseases that cause circulatory disorders in the optic nerve are atherosclerosis and hypertension. Circulatory disorders in the vessels of the optic nerve develop with occlusive lesions of the carotid arteries, against the background of diabetes mellitus and other endocrine pathologies. Vascular pathology of the optic nerve is possible in case of systemic diseases, vasculitis, cerebrovascular accidents, and glaucoma. Depending on the etiology of the disease, the clinical course of ischemic neuropathies has its own characteristics, which makes it possible to select adequate treatment. The terminology of vascular diseases of the optic nerve is very diverse, however, most authors consider the most acceptable term to be ischemic optic neuropathy, which, according to the location of the lesion, is divided into anterior (damage to the optic nerve head) and posterior (damage to the postlaminar part of the optic nerve).
Anterior ischemic optic neuropathy (AION) can be a bilateral process characterized by acute loss of visual function. In the pathogenesis of PION, the main role is played by circulatory disorders in the system of the posterior short ciliary arteries.
Target
— identification of features of the clinical course of PION depending on the etiology of the disease.
Material and methods
. We observed 34 patients aged from 45 to 77 years (20 men, 14 women). To assess visual functions, the following techniques were used: visometry, computer perimetry, tonometry, biomicroscopy, ophthalmoscopy, electron tonography, ultrasound biomicroscopy, laser scanning retinal tomography (HRT), laser Dopplerography. The patients were examined by a therapist, a neurologist, an endocrinologist, and, if indicated, by a cardiologist and an angiosurgeon. Diagnoses were established: arterial hypertension - in 13 patients, glaucoma - in 10, diabetes mellitus - in 8, atherosclerosis - in 3 patients. Diagnoses of hypertension, atherosclerosis, and diabetes mellitus were established by a therapist and an endocrinologist.
Results and discussion
. PION in arterial hypertension was characterized by a sudden decrease in visual acuity, the appearance of a central scotoma, loss of the lower half of the visual field or sector 8-24 hours after the hypertensive crisis. Visual acuity decreased on average to 0.02-0.04. During biomicroscopy, all patients showed a decrease in the pupillary reaction on the affected side. In the fundus of the eye, in 89.0% of cases the Solyus-Hun symptom of the 2nd-3rd degree was visualized, in 43.0% the presence of streak-shaped hemorrhages, in 85.6% - swelling and prominence of the optic nerve head, in 38.5% - cotton-like exudates. With significant blood pressure levels, 77.9% of patients had ischemic edema of the peripapillary retinal zone involving the macular region and ischemic exudate on the optic nerve head. Computed retinotomography (HRT) revealed unclear boundaries of the optic disc, its prominence by 1-2 mm, banded hemorrhages, pale optic disc and an average increase in area of 1.8 times, narrowing of the arteries and slight dilatation of the veins of the fundus.
For PION due to glaucoma, vision loss was characteristic for 5-7 hours. All patients had an open-angle form with stages 1-3 of the disease, the level of intraocular pressure on average was 22 mm. rt. Art. against the background of antihypertensive therapy. Visual acuity in the affected eye averaged 0.02. In the other eye, 8 (80%) patients had glaucomatous atrophy of the optic disc, visual acuity averaged 0.2. Biomicroscopy revealed dystrophic changes in the iris, baldness of the pigmented pupillary border, initial signs of cataracts, and a decrease in the pupil's reaction to light on the affected side. During perimetry, 80% of patients had loss of the nasal and lower half of the visual field, and 20% had arcuate scotomas with concentric narrowing. In the fundus there is blurred boundaries, prominence of the optic disc in 90% of patients, swelling of the peripapillary layer of nerve fibers in 80%, cotton wool-like exudates in 45%, hemorrhages on the optic disc in 90% of patients. The color of the optic disc was pale, glaucomatous excavation, atrophic changes in the deep layers of the retina, significant narrowing of the arteries and veins. On HRT - prominence of the optic nerve head by 0.5-1.0 mm, an increase in its size by 1.1 times, unclear boundaries, an increase and deepening of the excavation area by an average of 0.78 mm. In the other eye, a decrease in the visual field on the nasal side was recorded, the presence of various scotomas, and low vision with glaucomatous changes in the optic nerve head was noted.
In 8 patients, PION occurred against the background of diabetes mellitus. An ophthalmoscopic picture of diabetic angioretinopathy of varying severity was revealed in both eyes. A gradual decrease in visual acuity was noted against the background of an increase in blood sugar levels within 16-24 hours to 0.08, a concentric narrowing of the visual field with loss of the lower sector. In the lens there are opacities of varying severity, destruction of the vitreous body. In the fundus there was pallor and prominence of the optic disc, blurred boundaries, peripapillary edema of the retina in 87.5%, cotton wool-like and hard exudates in 75%, hemorrhages in 87.5% of patients, narrowing of the arteries and significant dilatation of the veins of the fundus . Computed retinotomography (HRT) revealed prominence of the optic disc into the vitreous body by an average of 0.9-1.0 mm, an increase in optic disc size by 1.2 times, unclear boundaries, and stagnant veins. In the fellow eye, visual acuity is 0.4-0.5.
Anterior optic neuropathy in atherosclerosis developed in elderly and old patients due to sclerosis and was organic in nature. There was a decrease in vision within 410 hours to 0.02. In the field of view there is prolapse of the lower half with paracentral scotomas. Dystrophic changes in the stroma of the iris and pigment border, decreased pupil reaction to light on the affected side. In the fundus there is a pale coloration of the optic disc, unclear boundaries, slight prominence, single streak-shaped hemorrhages in 52.7% of patients, peripapillary retinal edema in 71.5%, pronounced narrowing of the arteries and slight narrowing of the veins. HRT shows blurred boundaries and prominence of the optic nerve head by 0.5 mm, an increase in size by 1.1 times.
conclusions
.
Anterior ischemic optic neuropathy occurs in elderly patients with general vascular diseases, severe atherosclerosis, hypertension, and has its own course characteristics depending on the etiology of the disease. The most severe form of the course is anterior ischemic optic neuropathy against the background of glaucoma and atherosclerosis. With diabetes mellitus and arterial hypertension, with adequate treatment, the prognosis is more favorable. 09/01/2014 |
Viewed by: 6,269 people. Ischemic neuropathy of the optic (optic) nerve is a pathology of this area of the eye, occurring due to local circulatory disorders (in the intraorbital and intrabulbar region).
The disease is accompanied by a rapid decline in visual acuity, narrowing of visual fields, and the appearance of blind spots. Methods for diagnosing ischemic optic neuropathy - ophthalmoscopy, visometry, ultrasound, CT and MRI, angiography and others.
Treatment is medicinal, including vitamins, decongestants, antispasmodics, thrombolytics. Treatment is often complemented by physiotherapeutic procedures and laser stimulation of the optic nerve.
The disease is more often observed in the age group of 40-60 years, mostly affecting men. Optic neuropathy is considered a serious pathology, since it can significantly reduce visual acuity, and in some cases threaten its complete loss.
The disease is not considered independent: it is always part of a systemic pathological process (both in the organs of vision and in other parts of the body).
In this regard, ischemic neuropathy is considered not only by ophthalmologists, but also by neurologists, cardiologists, endocrinologists, hematologists, etc.
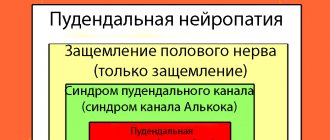
Types of ischemic optic neuropathy
The disease can occur in two different ways. The first of them is called locally limited ischemic neuropathy, the second is complete, or total ischemic neuropathy. According to the area covered by pathological processes, the disease can be anterior or posterior.
With the development of anterior neuropathy, damage to the optic nerve is observed against the background of acute circulatory disorders in the intrabulbar area.
The posterior form of neuropathy is diagnosed much less frequently. It is caused by ischemia-type damage in the intraorbital region.
How is it classified?
Based on the location of the pathological process, anterior and posterior forms of ischemic neuropathy are distinguished. Depending on the degree of damage to the optic nerve, the disease is divided into local (limited) and total.
The development of anterior ischemic neuroopticopathy is associated with impaired blood flow in the intrabulbar region. Such problems are caused by various forms of vascular lesions: thrombosis, embolism, spasm. With posterior ischemic optic neuropathy, the pathological process is localized in the retrobulbar region (behind the eyeball). The anterior form develops less frequently.
Etiology and pathogenesis
Anterior ischemic neuropathy is associated with abnormal changes in blood flow in the ciliary arteries. Due to insufficient oxygen supply to tissues, a state of ischemia (oxygen starvation) of the retinal, prelaminar, and scleral layers of the optic nerve head develops.
Posterior ischemic neuropathy occurs as a result of impaired blood supply to the posterior parts of the optic nerve, often due to stenosis of the carotid and vertebral arteries.
In general, the development of acute circulatory disorders in most cases is provoked by vascular spasms or organic damage to these vessels (for example, thrombosis, sclerosis).
The above conditions, which entail the appearance of signs of ischemic optic neuropathy, may have different prerequisites.
The disease starts against the background of the underlying pathology, mainly vascular disorders - hypertension, vascular atherosclerosis, temporal giant cell arteritis, periarthritis nodosa, obliterating arteritis, thrombosis of arteries and veins. Among the pathologies of metabolic processes, ischemic neuropathy is often accompanied by diabetes mellitus.
The disease can also develop in combination with discopathy of the cervical segment of the spine. Occasionally, pathology can accompany severe blood loss, for example, when a stomach or intestinal ulcer is perforated, injury to internal organs, or after surgery.
Sometimes ischemic neuropathy occurs with serious blood diseases, anemia, during hemodialysis, after administration of anesthesia, and with arterial hypotension.
Clinical picture
In most cases, the symptoms of ischemic neuropathy are unilateral. Less commonly (up to 1/3 of cases), the pathology spreads to the second organ of vision.
Since the course of the disease can be very long, the second eye is affected later - several weeks and even years after the onset of pathological phenomena in the first. Most often, in the absence of treatment, after 3-5 years, both organs of vision become involved in the process.
With the initial occurrence of anterior ischemic neuropathy, posterior ischemic neuropathy may subsequently develop, and signs of occlusion of the central retinal artery may also appear.
Usually the disease starts quickly and suddenly. After waking up in the morning, taking a bath, doing any physical work or playing sports, visual acuity decreases, and in some patients - to the point of blindness or identification of the light source.
In order for a person to feel a deterioration in visual acuity, it sometimes takes from a minute to a couple of hours. In some cases, damage to the optic nerve is preceded by a severe headache, the appearance of a veil before the eyes, pain in the orbit on the back side, and the occurrence of unusual phenomena in the field of vision.
Ischemic optic neuropathy always leads to deterioration of a person's peripheral vision. Often, vision pathologies come down to the formation of blind spots (scotomas), the disappearance of the image in the lower part of the view or in the nasal and temporal areas.
The acute condition lasts up to a month (sometimes longer). Further, the swelling of the optic nerve head decreases, hemorrhages gradually resolve, and the nervous tissue atrophies with varying degrees of severity. In many patients, vision is partially restored.
Preventive measures and forecasts
Unfortunately, treatment of ischemic neuroopticopathy rarely results in significant success. Since the eye is difficult to restore, and atrophy of nerve fibers is sometimes an irreversible process, there is a high probability of losing most of the visual functions, and blind spots often return. If the disease affects both eyes, there is a risk of complete loss of vision.
Optic neuropathy is a very serious enemy, and to prevent the possible development of this disease, doctors recommend treating any vascular diseases, systemic pathologies and metabolic problems without delay. If neuropathy affects one eye, you need to be regularly monitored by a specialist in order to prevent it from spreading its destructive effect to the second organ by any means.
Don’t forget to take care of your eyes, get regular examinations from your doctor, and try not to get carried away with traditional medicine unless it’s indicated by a specialist. In medical practice, the best method of treatment is always characterized by its immediate application, so it should never be delayed.
Taking care of your eyes also consists of regularly performing a set of special eye exercises, especially if you work hard for a long time. Do not work in poor lighting and promptly respond to any defects or visual impairments. Take care of your eyes and stay healthy!
Diagnostics
If any of the above symptoms occur, you must urgently call an ambulance or quickly seek help from an ophthalmologist. The examination program necessarily includes consultations with other specialists - a cardiologist, neurologist, rheumatologist, hematologist, etc. (until the cause of ischemic neuropathy is identified).
Ophthalmological studies include functional testing of the eyes, biomicroscopy, instrumental examinations using ultrasound, x-rays, and various electrophysiological methods. The specialist checks the patient's visual acuity.
With ischemic neuropathy, varying degrees of decrease in this indicator are found - from slight loss of vision to complete blindness. Abnormalities in visual function are also detected depending on the affected nerve area.
During ophthalmoscopy, swelling, pallor, an increase in the size of the optic nerve head, as well as its advancement towards the vitreous body are detected.
In the area of the disc, the retina swells greatly, and a star-shaped figure appears in its central section. The vessels in the area of compression narrow, and at the edges, on the contrary, they become more filled with blood and pathologically expand. In some cases, hemorrhages and exudate are present.
As a result of retinal angiography, retinal angiosclerosis, occlusion of cilioretinal vessels, and pathological changes in the caliber of veins and arteries are visualized.
Usually, disturbances in the structure of the optic nerve head are not detected in posterior ischemic neuropathy. When performing an ultrasound of the arteries with Doppler sonography, a violation of normal blood flow is recorded.
Electrophysiological examinations include an electroretinogram, calculation of the maximum flicker fusion frequency, etc. Usually there is a decrease in the functional properties of the nerve. A coagulogram reveals hypercoagulation, and a blood test for cholesterol and lipoproteins reveals an increased amount.
Ischemic neuropathy should be differentiated from retrobulbar neuritis, tumors of the nervous system and orbit of the eye.
Treatment
Treatment should be started as early as possible, optimally in the first hours after the onset of symptoms. This need is due to the fact that long-term disruption of normal blood supply leads to the loss of nerve cells.
Emergency measures include intravenous injections of aminophylline, taking tableted nitroglycerin, and short-term inhalation of ammonia fumes. After emergency treatment, the patient is admitted to the hospital.
In the future, the goal of therapy is to reduce swelling, improve the trophism of nervous tissue, and also provide an alternative route of blood circulation. In addition, the underlying disease is treated and normalization of blood clotting, fat metabolism, and blood pressure is ensured.
Vasodilators for ischemic neuropathy include Cavinton, Cerebrolysin, Trental, decongestants - diuretics Lasix, Diacarb, blood thinners - thrombolytics heparin, phenylin.
Additionally, glucocorticosteroids, vitamin complexes, and physiotherapy (electrical stimulation, laser nerve stimulation, magnetic therapy, microcurrents) are prescribed.