| Common peroneal nerve | |
| Nerves of the lower limb. Back view | |
| Latin name | Nervus fibularis [peroneus] communis |
| Innervation | muscles of the anterior group of muscles of the lower leg and dorsum of the foot, skin of the dorsum of the foot and the anterior surface of the lower leg |
| Begins | sciatic nerve |
| Catalogs |
|
Common peroneal nerve
(lat. Nervus fibularis [peroneus] communis) - nerve of the sacral plexus.
It is formed after the division of the sciatic nerve in the area of the popliteal fossa into two parts. Formed by fibers of the LIV, LV, SI, SII
nerves.
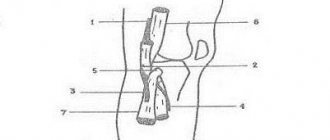
From the proximal apex of the popliteal fossa it goes to its lateral side and is located under the medial edge of the biceps femoris muscle, between it and the lateral head of the gastrocnemius muscle, spirals around the head of the fibula, being covered here only by fascia and skin. In this area, non-permanent articular branches extend from the nerve trunk to the lateral parts of the knee joint capsule. Distally, it penetrates into the thickness of the initial part of the peroneus longus muscle, where it divides into its two terminal branches - the superficial and deep peroneal nerves[1].
human anatomy
In order to understand how this neuropathy manifests itself, let’s remember human anatomy. The largest nerve plexus in the human body is the sacral plexus. Connecting with each other, the nerves of this plexus form the thick sciatic nerve, which is the longest and thickest nerve in the human body. In addition to the sciatic nerve, short branches also extend from the plexus, which innervate the pelvic muscles, gluteal muscles, as well as the perineum and genitals (pudendal nerve).
Nerves of the tibia
As for the sciatic nerve, it is, as it were, a direct continuation of the sacral plexus itself, and contains all its constituent roots and nerve fibers. It exits the pelvis through the greater sciatic foramen and is covered on top by the gluteus maximus muscle.
Then this nerve descends almost vertically down, hiding under the muscles - the hip flexors, along its back surface.
Having reached the fossa poplitea, or popliteal fossa, it branches into two main branches: the tibial nerve, which lies more centrally, and the thin branch, which lies more outward. This is what is called the common peroneal nerve.
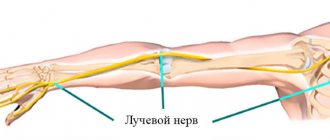
The common peroneal nerve, continuing to descend down the lower leg, is itself divided into two branches: superficial and deep. Even before division, it gives off small cutaneous branches that innervate the lateral (outer) part of the leg and give it sensitivity. In addition, these branches, uniting with others, on the foot provide sensitivity to its outer edge along with the little toe.
Anatomy of the leg
The superficial part of the peroneal nerve is both a muscular (motor) and cutaneous (sensory) nerve. It, again, dividing in half, innervates the pennate muscles of the leg, and the cutaneous branches go to the big toe, as well as to the edges of the 2nd and 3rd toes facing each other. A separate branch of the external peroneal nerve innervates the dorsum of the foot in the area of 2-5 toes.
The deep branch of the peroneal nerve goes along with the tibial artery, and provides movement of the tibialis anterior muscle, the common long extensor of the digitorum, the extensor pollicis, and also gives branches to the ankle joint. After “wandering” along the lower leg, this nerve, together with the vessel, enters the dorsum of the foot, providing innervation to the short extensor muscles of the fingers, and the skin of the 1st and 2nd fingers.
Such a whimsical course of the long peroneal nerve ensures its vulnerability along the way. How does damage to this nerve manifest itself?
Forecast and prevention of occurrence
The prognosis of the pathology depends on how soon the patient sought help from a specialist and how correct the treatment was. Irreversible changes significantly worsen the prognosis and lead to disability.
To prevent the occurrence of neuritis, it is recommended:
- maintain optimal body weight,
- protect your feet from injury,
- periodically give your legs a break during prolonged vertical or uncomfortable body positions,
- wear comfortable shoes with orthopedic insoles,
- do not wear high-heeled shoes all the time,
- people involved in sports need to be regularly screened for compression-ischemic neuropathy (tunnel syndrome).
It is strictly not recommended to delay treatment of the pathology at the first symptoms , as this can aggravate the situation and lead to irreversible consequences. Ignoring the symptoms of pathology leads to incapacity and permanent disability.
Symptoms of neuropathy
As has already become clear, since its main function is extension of the foot, it is this that is disrupted, as well as raising the inner edge of the foot. It is difficult to straighten the toes, abduct the foot, and simultaneously try to lift it outward.
The foot hangs, the toes are bent at the metatarsophalangeal joints (equine foot). Due to the inability to straighten it, stepping occurs, or “cock gait,” in which the foot must be raised high at the expense of the knee and placed from a vertical position.
Equine foot affected by peroneal nerve neuropathy
When the peroneal nerve is damaged, sensitivity on the outer surface of the leg is impaired (numbness, tingling, crawling sensation). As a rule, the patient does not notice pain when polyneuropathy develops.
A very characteristic sign of damage to the peroneal nerve is the inability to stand up, much less walk on your heels, since this requires straightening your toes. With a long course of the pathological process, it is possible to notice emaciation and hypotrophy of the extensors of the toes, which are located on the back of the foot. This is manifested by pronounced tendon contours. The dorsum of the foot on the affected leg appears “ridged.”
In addition, sensitivity disturbances in the interdigital space, between the 1st and 2nd fingers, are characteristic. Reflexes (Achilles) with damage to the peroneal nerve are usually intact.
Diagnostics
Early seeking medical help for neuropathy is the key to success in the fight against pathology. During the examination, the specialist determines the extent of sensory and motor disorders. In order to confirm a preliminary diagnosis, it is necessary to perform the following studies:
- electromyography - conduction of an impulse along a nerve fiber,
- Ultrasound – examination of soft tissues and choroid plexuses,
- magnetic resonance or computed tomography - study of images in which all structures of the lower extremities are depicted in different planes to clarify the localization of the pathological focus and its size,
- for injuries - radiography,
- various blood tests - general, biochemical, hormonal parameters and tumor markers.
The specialist will carry out differential diagnosis with infectious lesions and injuries, cancer formations and toxic effects on the human body. A thorough analysis of diagnostic information and identification of the causes of the pathology facilitates the selection of a treatment regimen.
Causes of damage to the peroneal nerve
It is worth dwelling on the causes of damage to the peroneal nerve:
- neuritis or neuropathy. In this case, sometimes pain may occur in the upper third of the leg, but the main symptoms will be loss of movement and sensitivity;
- compression-ischemic neuropathy. The nerve is pinched on the back of the thigh under the biceps tendon. It is the deep branch of the peroneal nerve, which “manages” the foot, that is affected;
- It is also possible that the superficial branch of the peroneal nerve is affected; this occurs in the area of the upper head of the fibula. This causes pain in the lower leg when walking. Such manifestations are caused by frequent squatting, prolonged stay in the “leg-to-leg” position, etc.
Damage to the peroneal nerve due to a fracture of the fibula
- in addition, spondylogenic tunnel syndrome may occur. The intervertebral disc in the lumbar spine is to blame for this, which caused ischemia in the basin of the Deproge-Gotteron artery, which supplies blood to the spinal cord. The result is radiculo-epiconus - cone syndrome.
In addition to these “local” causes, symmetrical nerve damage may occur, and one of the reasons is chronic alcoholism. Another reason is diabetes. This causes a toxic effect on the nerves. In the first case - ethanol, and in the second - glucose. In this case, a “socks” and “gloves” type lesion occurs, with impaired sensitivity and movement disorders, which is symmetrical in nature.
In diagnosing damage to the peroneal nerve, electroneuromyography is of great importance, by which one can judge the processes that caused disturbances in the functioning of the nerve.
Of course, a neurologist must examine, and even more so, prescribe treatment; sometimes he works together with an endocrinologist or a narcologist. But even for a simple person who does not have any medical education, it is easy to remember that if it is impossible to stand on your heels, then the peroneal nerve is affected, and if on your toes, then the tibial nerve, since they innervate muscles that are antagonists, that is, performing opposite functions.
Therefore, if you doubt whether the damage to the peroneal nerve is progressing or not, just walk on your heels. If this becomes increasingly difficult to do, you should consult a doctor.
It is important to understand that often the progression of peroneal nerve neuropathy with discogenic lesions occurs gradually, and what is especially dangerous is that it can occur with little or no pain. People tend to tolerate these violations in the hope that everything will go away on its own.” But, as a rule, nothing goes away on its own, and a person turns to doctors when the leg begins to interfere with walking, and a disturbance in gait becomes noticeable to others.
If a year or two passes from the beginning of pronounced changes, then the chances that the nerve will recover are very small. Therefore, you should consult a doctor if there are minimal signs of a gait disorder or sensory disturbance in the lower leg area.
Principles of treatment
After identifying the causes that caused the neuritis, appropriate therapy is prescribed:
- if bacterial in nature - antibiotics and sulfonamides,
- for a viral infection - interferon and gamma globulin,
- for ischemic - vasodilator drugs,
- in case of trauma – immobilization of the limb, anti-inflammatory, diuretic, vitamin and painkillers.
If necessary, surgical intervention is performed. Physiotherapy, massage and special gymnastic exercises are also prescribed . Of all the physiotherapeutic techniques, electrophoresis, electromyostimulation, and magnetic therapy give the best results.
Massage therapy is carried out using smooth movements with minimal pressure from the periphery to the center. The “squeezing” technique is also used, the plantar and dorsal surfaces are compressed, as well as all tissues from the fingers to the knee. Stretching procedures are carried out until a feeling of tolerance is felt - each toe and the base of the ankle.
Massage can relieve pain and improve the condition, but it can also aggravate the situation, so it should be performed by an experienced specialist as prescribed by a doctor.
Therapeutic gymnastics includes the following exercises:
- anaerobic,
- to maintain balance,
- for flexibility,
- power.
Gymnastics in water is very useful.
Neuritis or inflammation of the tibial nerve (symptoms)
In the acute phase, tibial nerve neuritis can give rise to several clinical syndromes. The most important symptom of inflammation of the tibial nerve is pain that is burning and acute in nature. It appears suddenly and does not go away after changing the position of the leg. External clinical symptoms of tibial nerve neuritis can manifest themselves in the form of hyperemia and slight swelling of the subcutaneous fatty tissue. Although this is not a mandatory clinical sign.
With chronic inflammation of the tibial nerve, the flexion of the foot with its lowering is impaired. Subsequently, a disturbance in the flexion of the toes occurs. Any attempts to stand on your toes end in complete failure. If you observe the patient’s gait, you will see that when placing the foot, the emphasis is on the heel, without the typical rolling from the base of the foot.
If timely treatment is not carried out, then atrophy of the muscular system of the foot and lower leg begins. The foot takes on a characteristic appearance, more reminiscent of a clawed paw. Tendon reflexes in the ankle area fade away.
During the examination, the neurologist notes a significant decrease in pain sensitivity in the back of the lower leg and along the plantar surface of the foot. The first three toes are numb. The activity of the pulse wave on the inner bend of the foot decreases. Vascular insufficiency gradually develops, leading to the development of long-term non-healing trophic ulcers of the leg and foot.