| Oculomotor nerve palsy | |
| Diagram of the optic nerves | |
| ICD-10 | 49.049.0 |
| ICD-9 | 378.52378.52 |
| DiseasesDB | 2861 |
| eMedicine | oph/183 |
| MeSH | D015840 |
Oculomotor nerve palsy
is an eye condition resulting from damage to the oculomotor nerve or its branch. As its name suggests, the oculomotor nerve controls the bulk of the muscles that control eye movements. Thus, damage to this nerve causes the affected person's eyes to be unable to move. In addition, the nerve also controls the muscle of the upper eyelid and the muscles responsible for constricting the pupil (pupillary sphincter). Restrictions in eye movements are usually so severe that the affected person is unable to maintain normal eye alignment when looking straight ahead, resulting in squinting and resulting double vision (diplopia).
Oculomotor nerve palsy is also known as “oculomotor neuropathy.”[1]
General information
The nervous system is represented by various nerve plexuses, peripheral nerves, spinal cord and brain.
Neuropathy is a non-inflammatory lesion of the nervous system. Peripheral nerves have a very thin structure and are not resistant to damaging factors. According to the level of damage they distinguish:
- Mononeuropathy. Characterized by damage to one single nerve. Mononeuropathy is considered a fairly common option. Most often, mononeuropathy of the upper limb is diagnosed (mononeuritis of the radial or ulnar nerve).
- Multiple neuropathy affecting several nerve endings.
- Polyneuropathy , which is characterized by the involvement of several nerves localized in one area.
Eye positioning
Complete oculomotor nerve palsy
results in a characteristic
downward and outward
. The eye will move outward and downward; outward because the lateral rectus muscle (innervated by the sixth cranial nerve) will receive muscle tone relative to the paralyzed medial rectus muscle. The eye will move downward because the superior oblique muscle (innervated by the fourth cranial nerve or trochlear nerve) is not antagonistic to the paralyzed superior rectus muscle, inferior rectus muscle, and inferior oblique muscle. The affected person will also have ptosis, or drooping eyelids, and mydriasis (dilated pupils).
It should be borne in mind, however, that the extensive structure of the oculomotor nerve means that damage suffered at different points along its path, or damage caused in different ways (compression from loss of blood supply, for example), will result in effects on different muscle groups, or different individual muscles, thus producing different patterns of presentation.
Compressive injury to the oculomotor nerve can cause compression of the parasympathetic fibers before the motor fibers become impaired, since the parasympathetic fibers travel along the outer surface of the nerve. Thus, it can lead to eyelid ptosis and mydriasis (dilation of the pupil) as a result of the compression of the parasympathetic fibers to a "down and out" position.
Pathogenesis
Neuropathy is usually determined by the nature of the nerve damage and its location. Most often, the pathology forms after a traumatic injury, after suffering from general diseases and during intoxication.
There are 3 main forms of neuropathy:
- Post-traumatic neuropathy. Violation of the integrity of the nerve myelin sheath occurs as a result of acute injury or severe blow. With tissue swelling, improper scar formation and bone fractures, compression of the nerve fibers occurs. Post-traumatic neuropathy is characteristic of the ulnar, sciatic and radial nerves.
- Diabetic neuropathy. Damage to nerve endings is also recorded with high levels of sugar and blood lipids in the blood.
- Toxic neuropathy. As a result of infectious diseases such as herpes , HIV , diphtheria , etc., toxic damage to the nerve plexus occurs. Poisoning with chemical compounds and overdose of certain medications can lead to disruption of the integrity of the nerve trunk.
Neuropathy can develop against the background of a disease of the hepatic system, kidney pathology, osteochondrosis , arthritis , the presence of neoplasms and insufficient levels of thyroid hormones .
Description
Femoral nerve neuropathy.
Damage to the n femoralis of various etiologies, leading to disruption of the conduction of nerve impulses through it. Clinical manifestations depend on the topic of the lesion and can be pain and sensory disturbances on the anteromedial surface of the thigh and lower leg, difficulty walking due to impaired extensor movements in the knee, etc. In the diagnosis of n femoralis neuropathy, they rely on ultrasound data of the nerve and EMG. Therapeutic tactics include the elimination of nerve compression, metabolic, vascular, anti-inflammatory, analgesic and decongestant therapy, physical therapy and electrical myostimulation.
Classification
They are classified according to localization:
- Neuropathy of the lower extremities. The most common diabetic neuropathy of the lower extremities is caused by diabetes mellitus . In this form, the peripheral nervous system innervating the lower extremities is affected.
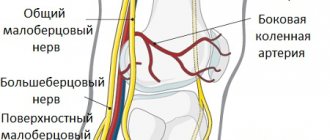
- Peroneal nerve neuropathy. Characteristically, one peroneal nerve is affected, which is manifested by muscle weakness and impaired sensitivity in the innervated area. ICD-10 code: G57 – mononeuropathies of the lower extremities.
- Distal axonal neuropathy after cutting. Post-traumatic or axonal neuropathy develops as a result of damage to nerve endings that arise from certain structures of the spinal cord and are responsible for transmitting nerve impulses to the limbs. If nerve transmission is difficult or completely interrupted, the patient complains of tingling or complete loss of mobility. Distal axonal neuropathy manifests itself differently depending on the nature, type and location of the pathological process.
- Ischemic neuropathy develops when nerve endings are compressed in the area of the musculoskeletal joints and in the spinal column. A violation of not only innervation, but also blood circulation is recorded, which leads to the formation of ischemia. With a chronic course of the process and a long-term disorder, paresthesia and hypotrophic processes develop, which in severe cases can lead to paralysis and necrosis . Ischemic neuropathy has a wide range of symptoms and is not difficult to diagnose.
- The best known form is optic neuropathy. Anterior ischemic optic neuropathy . Characterized by damage to the anterior segment of the optic nerve, which leads to very rapid and persistent impairment of visual function, up to complete or partial atrophy of the optic nerve. Anterior optic neuropathy is also known as vascular pseudopanillia . Posterior ischemic optic neuropathy. It is characterized by damage to the retrobulbar posterior part of the optic nerve due to ischemic effects. The posterior form is also fraught with loss of visual perception.
- Ulnar nerve neuropathy. The peripheral nervous system can be affected by several causes. Damage to the ulnar nerve is most often encountered in traumatology. As a result of compression of the nerve trunk, which is located in the area of the elbow joint, the entire upper limb is affected.
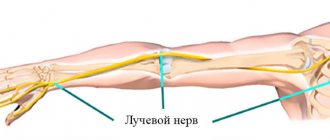
- Radial nerve neuropathy. Clinically, it manifests itself as a characteristic symptom of a “dangling hand,” which is caused by the inability to straighten the hand and fingers. Damage to the radial nerve can be associated with trauma, metabolic processes, ischemia, and compression.
- Median nerve neuropathy. The nervus medianus can be affected in any area, which will inevitably lead to swelling and severe pain in the hand area and impaired sensitivity. The process of flexion of all fingers and opposition of the thumb is disrupted.
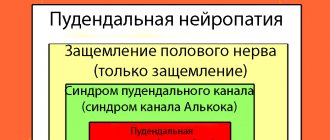
- Pudendal nerve neuropathy. It develops as a result of damage to the pudendal nerve, which is located in the pelvic area. Takes an active part in the act of urination and bowel movement, sending nerve impulses along the nerve trunks that pass through the genitals. Pathology is characterized by severe pain.
- Neuropathy of the tibial nerve. The clinical picture depends on the level of nerve damage. The tibial nerve is responsible for the innervation of the muscles of the foot and lower leg and the sensitivity of the skin in this area. The most common cause of tibial nerve neuropathy is traumatic injury to the nerve trunk.
- Femoral nerve neuropathy. The clinical picture of damage to the femoral nerve depends on the level of damage to the large nerve trunk.
- Neuropathy of the oculomotor nerve. Diagnosis of pathology requires a thorough examination and is complex. The clinical picture is represented by symptoms that occur in many diseases. When the oculomotor nerve is damaged, ptosis, divergent strabismus, etc. are observed.
What is ulnar nerve neuropathy
Neuropathy (neuropathy) is damage to one or another nerve, accompanied by loss of sensory and/or motor function (disease code according to the International Classification of Diseases, 10th revision - ICD 10 G56.2).
This article will talk about ulnar nerve neuropathy. Among all diseases of the nerves of the upper limb, ulnar neuropathy ranks second. This is due to some structural features of the hand. This article will discuss this in more detail, as well as diagnostic and treatment methods.
Compression
This type of neuropathy occurs during prolonged, uncomfortable, stationary work, due to compression by stiff ligaments and muscles . In order to better understand the mechanism, you need to understand the anatomy of the ulnar nerve.
It starts from the spinal cord, at the level of the 7th cervical and 1st thoracic vertebrae. Next, the nerve goes through the shoulder to the back of the arm, reaches the elbow joint, then down to the forearm.
On it, the ulnar nerve passes to the anterior surface of the arm and enters the narrow canal of the ulnar nerve (cubital). It further breaks down into separate nerves going to the palm and fingers.
As we can see, there are 3 possibilities for compression (squeezing) of the ulnar nerve.
- Behind the elbow joint, at the level of the epicondyle of the ulna. The nerve passes almost under the skin, so it is often damaged. For example, everyone knows the sharp pain when hitting an elbow on a hard surface.
- Between the flexor carpi ulnaris muscle and the bone: in the so-called cubital canal.
- In the canal of the ulnar nerve of the wrist (Guillaume's canal) Also sometimes the nerve can be damaged during the transition from the superficial part of the palm to the deep part. This type of compression is observed during sports activities.
Compression in the areas indicated above can occur for a variety of reasons. But usually this is long-term uncomfortable work in a non-physiological position. According to research, the nerve on the “leading” hand is twice as likely to be affected (that is, if a person is right-handed, then on the right and vice versa).
In the cubital canal (tunnel), neuropathy occurs due to prolonged holding of the elbows in one position on a desk, machine, workbench, for the driver when leaning on some part of the car cabin, etc.
Compressions in the wrist area (Guillaume's channel) occur when working at a computer, when a person is forced to sit at an uncomfortable keyboard, or move a computer mouse that is too high or, conversely, low for a long time. This pathology is widely known as “Tunnel syndrome”. Also due to working with tools for a long time, walking with crutches and a cane.
Tumors, arthrosis and arthritic changes in joints, and hematomas (bruises) after blows can compress the nerve all along the arm. You can press it while you sleep (this usually happens after taking a large dose of alcohol)
Post-traumatic
Neuropathy can be caused by trauma. These are most often dislocations of the elbow and wrist joints, as well as fractures, gunshot and household wounds, sprains and ruptures of ligaments, and blows.
After other diseases This type of disease occurs as a complication of any common diseases. For example, after acute infectious diseases: typhus and typhoid fever, syphilis, bites of certain insects (ticks), etc. Also for polyneuropathy due to diabetes mellitus, intoxication.
Help : it is recommended to take breaks during work and do a simple warm-up of your arms and back. This prevention will protect you from carpal tunnel syndrome and many other diseases.
Symptoms
With damage at the level of the cubital canal, first of all, patients pay attention to:
- Feeling of numbness in the fingertips, especially the little finger and ring finger, gradually spreading to all fingers and hand
- Weakness of the hands during work, reaching the point that it is difficult for the patient to pick up and hold any object
- Pain in the elbow area
These symptoms tend to progress slowly but surely. First one of them appears, then several and finally all.
If there is a lesion at the level of Guillaume's canal:
- Paresthesia (burning sensation, pins and needles) on the forearm and hand
- Insomnia or a person wakes up at night
- Increased or, conversely, decreased sensitivity to temperature on the hand
- Decreased elevation of the little finger (hypotenar)
- Problems with the movement of the fingers, especially the thumb
If the functions of the nerve are completely impaired, the patient experiences the so-called a symptom of a “clawed paw” - the fingers of the hand hang down, their movement is impossible. There is a gradual atrophy of the muscles innervated by the ulnar nerve. This makes a person disabled.
Important : do not let your brush get to this point. If you experience any discomfort in your hands, especially if you have the above-described provoking factors due to work or some habits, you should immediately consult a doctor.
Diagnostics
The type of diagnosis depends on the doctor’s experience, the nature of the disease, and the capabilities of the hospital or clinic. Sometimes an anamnesis of the disease is sufficient: interviewing the patient about his life history, the time and cause of the onset of symptoms, as well as a general examination. Sometimes you have to resort to more complex methods.
- The simplest is a diagnostic test . The patient is asked to place his hand on the table, palm down, and try to move his little finger. If the ulnar nerve is damaged, this cannot be done. They also suggest clenching your hand into a fist. Squeezing the little finger and ring finger will not work, or it will not work completely. Another test is to spread and move your fingers in the position of the hand extended forward. This is difficult to do with neuropathy.
- Reflex test.
- Rheogram of the forearm - measurement of vascular tone. With neuropathy it will be reduced.
- Electromyography is an analysis of the tone of innervated muscles.
- Palm prints using ninhydrin : measuring the degree of sweatiness of the hands.
- CT, MRI, X-ray examination of the wrist , hands, spine: to search for various injuries, degenerative-dystrophic diseases.
- Thermal imaging study.
- Ultrasound examination.
Ulnar nerve neuropathy treatment
Treatment should be comprehensive, that is, use all available methods . It is necessary to perform exercises for the hands, and here the patient must be motivated to recover. First of all, provoking factors are identified and removed. These may be inconvenient tools for work, some habits.
If neuropathy is caused by a common medical condition, treat it aggressively. A special orthosis, elastic bandages and other orthopedic devices are put on the wrist.
Important : maintain a work-rest schedule, spend more time in the fresh air, eat vegetables and fruits, and foods containing calcium.
Drug therapy
In mild cases, non-steroidal anti-inflammatory drugs (aspirin, diclofenac) are prescribed. If the cause of compression may be edema, then diuretics (Lasix, etc.).
Novocaine, analgin, and glucocorticosteroids are injected into the affected area (elbow or wrist). The dosage depends on the patient’s age, severity of the disease, and concomitant diseases.
It is advisable to rub pain-relieving ointments and gels onto the area of nerve damage.
Vitamins
Help restore immunity. Strengthen metabolism in the nerve, eliminate ischemia, expand capillaries. Used: Vitamins B1, B6, as well as complex preparations: Milgamma. They are prescribed intramuscularly, or you can inject directly into the area of compression or injury to the ulnar nerve.
It will be useful to take multivitamin complexes internally.
Physiotherapy as an additional method can help in treatment. Are used:
- Magnetotherapy
- Massage
- Electrophoresis of various drugs, such as novocaine
- Reflexology
- Ultrasound irradiation
- Sanatorium-resort treatment in specialized institutions
Surgical intervention
If there is no effect in conservative treatment, you have to resort to surgery. 1) Dissection of the canals in which compression of the nerve occurs. You can also, for greater efficiency, pull out and move the nerve to another place (transposition). 2) Neurolysis and nerve suture. Used for hand injuries.
3) Removal of the epicondyle of the ulna (with cubital compression)
The operations are performed with minimal incision and blood loss. Some hospitals use endoscopes. It should be noted that sometimes after surgery the condition may worsen.
Physiotherapy
Simple exercises can effectively relieve ulnar neuropathy.
1. Clench your hand into a fist, unclench your fingers one by one.2. Rotate the hand clockwise and counterclockwise at the wrist joint.3. Exercise with a manual expander.4. If your fingers are difficult to straighten, try to collect small objects (coins, keys, children's cars, etc.), then throw them and collect them again.5.
Modeling from plasticine, dough, finger painting with paint, etc. will be beneficial.6. In water, clench your hand in a fist and sharply straighten it upward7. Try to grasp a piece of paper with your thumb and forefinger8. Roll a special ball with spikes - the so-called. Su Jok therapy9. Self-massage the affected arm once a day
10.
After exercise, take a bath with pine needles and sea salt.
All exercises, unless otherwise stated, should be performed 15 times, several times a day.
Find out more in this video
Causes
It is extremely rare that neuropathy develops as a separate independent disease. Most often, nerve endings are affected against the background of a chronic pathology, which acts as a traumatic factor. The development of neuropathy is preceded by the following diseases and conditions:
- hypovitaminosis;
- metabolic disorder ;
- decreased reactivity;
- intoxication , poisoning;
- nerve fiber injury;
- neoplasms (malignant and benign);
- severe hypothermia;
- hereditary pathology;
- diagnosed endocrine diseases.
Neuralgia of the brachial nerve (plexus): symptoms of plexitis, diagnosis, treatment of the shoulder joint
Neuralgia of the shoulder joint is a pathology associated with acute pain resulting from pinching of the brachial nerve.
This disease is not an inflammatory process; pain occurs as a result of swelling or inflammation of a part of the body resulting from defects in innervation.
The pinched nerve cannot fully perform its basic functions, as a result, tissue sensitivity suffers and pain occurs.
Many people confuse neuritis with neuralgia, but these concepts imply different conditions. With neuritis, the brachial nerve itself is inflamed, and with neuralgia, the tissues that it innervates are inflamed. However, neuralgia in some cases can be aggravated by complications, and then neuritis itself develops.
What is brachial neuralgia
Neuralgia of the shoulder joint is periodic attacks of pain of varying nature and strength. Pain syndrome with neuralgia is associated with an inflammatory process in the area that is adjacent to a given part of the body - in our case, the shoulder.
As a result of changes in nearby tissues, compression of the nerve occurs. As a rule, the nerve is pinched by inflamed ligaments, intervertebral discs, swollen muscle tissue, and tumors.
Much is determined by the reasons that caused neuralgia, as well as whether the patient has any concomitant diseases.
It is important to know that in the absence of proper treatment, tissue inflammation can spread directly to the nerve, causing plexitis (neuritis) in the nerve tissues.
Symptoms
Unlike diseases that can be practically asymptomatic in the first stage, it is impossible not to pay attention to this disease. A sign of brachial neuralgia is severe pain in the shoulder joint.
It can last from several minutes to several hours, causing suffering to a person. The pain can be of a different nature: aching, dull or sharp, acute.
The localization of pain can also be different - both directly in the shoulder joint or next to it, and in the arm from the elbow to the sore shoulder.
Patients may experience accompanying symptoms: decreased joint mobility, stiffness, inability to make free movements of the hand, sharp pain when trying to touch, or, conversely, decreased sensitivity. This may be accompanied by increased sweating, redness or paleness of the skin around the joint, trembling or twitching of the muscles.
In advanced, untreated cases, the intervals between attacks of pain are reduced, the pain itself becomes longer and stronger, to the point that the arm hurts constantly.
In such cases, there is a risk of signs of numbness, necrosis, paralysis of the shoulder and limb.
They are expressed in a slight tingling (so-called “pins and needles”) in the limb at a time when there is no pain, insensitivity to irritants, weakness and numbness.
Causes
Neuralgia can appear due to severe hypothermia of the joint, too much physical stress on the muscles adjacent to the shoulders.
The shoulder often suffers from the side on which the main working arm is located - for example, a right-handed person lifted a weight with his right hand and suffered a pinched nerve in the right shoulder joint.
According to statistics, the right shoulder joint is affected more often than the left.
Poor nutrition, severe or frequent colds, systematic use of alcohol and drugs - all these factors, weakening the body, can accelerate the development of neuralgia, aggravating its severity. An aggravating factor can be the stress experienced, provoking psychosomatic reactions.
Neuralgia can develop as a result of infection, injury in the collarbone area - sprain, dislocation, severe bruise, fracture.
Osteochondrosis of the cervical or thoracic spine, impaired metabolism, diseases of the digestive tract, diabetes mellitus, heart and vascular diseases, the presence of tumors, and hernias can have a direct impact on the development of this disease.
In addition to physical compression of the nerve, the cause is insufficient supply of nerve tissue with oxygen and nutrients.
What it is? ICD-10 code
Anatomically, the nervous system is the most important component of the human body ; it is responsible for the coherence and consistency of the work of other organs and vital systems.
There are some pathologies that are directly related to damage to the nerve trunks - these are various neuralgia (occipital, trigeminal, external femoral nerve).
Brachial neuralgia - spasms of the shoulder muscles , pinching and damage (in clinical cases) to the peripheral nerve processes or roots of the brachial plexus.
The plexus of nerves emerges from the cervical spine and is located at the level of the joint (at the junction of the clavicle, the process of the scapula and the head of the humerus). This plexus then branches throughout the arm.
The essence of the interaction between the nervous and muscular systems is simple - the branches of the brachial plexus send electrical signals to the muscle, which contracts under the influence of this signal. Any movement is a muscle contraction.
With neuralgia, the inflammatory process only compresses, but does not damage the nerve fibers.
According to the international classification of diseases (1999) - ICD-10 - the disease is assigned the code: G54.0, denoting diseases of the nervous system, class No. 6. This pathology can also be classified as class M, No. 13 (diseases of the musculoskeletal system), depending on the root cause of its origin. If the diagnosis is “blurred”, specialists use coding M79.2 (subsection of unspecified neuralgia).
Source: https://neuro-orto.ru/bolezni/perifericheskaya-nervnaya-sistema/nevryt/nevrit-plechevogo-nerva.html
Symptoms of neuropathy
When nerve endings are damaged, muscle fibers become thinner and their reflex function is impaired. In parallel, there is a decrease in contractility and partial loss of sensitivity to stimuli that cause pain.
The clinical picture of neuropathy can be very different, and the pathological process can be localized anywhere, causing neuropathy of the peroneal nerve, trigeminal nerve, facial nerve, ulnar and radial nerve. Damage to sensory, motor or autonomic nerve function negatively affects the patient's quality of life. Several forms of neuropathy occur in patients with diabetes
- Peripheral neuropathy. Characterized by damage to the peripheral nerves that are responsible for the innervation of the upper and lower extremities. Symptoms of neuropathy of the upper extremities manifest themselves in the form of impaired sensitivity in the fingers and toes, a tingling sensation, and a feeling of numbness in the upper extremities. The symptoms of neuropathy of the lower extremities are identical: tingling and sensory disturbances in the lower extremities are noted.
- Proximal form. It is characterized by impaired sensitivity mainly in the lower extremities (buttocks, thigh, lower leg).
- Autonomous form. There is a functional disorder of the genitourinary system and digestive tract organs.
Symptoms of alcoholic neuropathy
Most often, alcoholic neuropathy is accompanied not only by sensory disorders, but also by motor ones. In some cases, patients complain of muscle pain of various locations. The pain syndrome may be accompanied by a sensation of “crawling” in the form of paresthesia, tingling, a feeling of numbness and impaired motor activity.
At the initial stage, patients complain of muscle weakness and paresthesia. In every second patient, the disease first affects the lower extremities, and then the upper ones. There are also simultaneous lesions of the upper and lower belts.
Characteristic symptoms of alcoholic neuropathy:
- a sharp decrease, and in the future a complete absence of tendon reflexes;
- diffuse decrease in muscle tone.
Alcoholic neuropathy is characterized by disruption of the facial muscles, and in more advanced cases, urinary retention is noted. In the advanced stage, alcoholic polyneuropathy is characterized by:
- muscle weakness in the limbs: unilateral or symmetrical;
- paresis and paralysis;
- violation of surface sensitivity;
- sharp inhibition of tendon reflexes followed by their complete extinction.
Symptoms
The clinical symptom complex of femoral neuropathy depends on the topic of the process. When pathology occurs at the iliopsoas level, a full range of symptoms develops, including sensory, motor and autonomic-trophic disorders throughout the area innervated by the femoral nerve. In rare cases, with a high division of the nerve, only sensory or only motor disturbances can be observed, sometimes a mosaic picture of motor and sensory disturbances. Complete neuropathy of the femoral nerve is accompanied by only partial disruption of the iliopsoas muscles, due to the existence of their alternative innervation. Therefore, flexion and supination of the hip are practically not impaired. Paresis of the quadriceps muscle, which is responsible for straightening the leg at the knee joint, is more pronounced. Due to difficulty in extension, patients try not to bend their leg at the knee. Running and walking are difficult, especially when it is necessary to climb stairs. The gait changes. The leg is fixed in a hyperextension position. There is a lack of knee reflex. Sensory disorders include disorders of tactile and pain perception on the anterior inner surface of the thigh and lower leg, and the medial edge of the foot. In the same zone, trophic and vegetative changes are observed, and irritating pain is possible. When lying on the stomach, symptoms of tension are detected - pain along the front surface of the thigh when trying to raise a straight leg as much as possible (Wassermann's symptom) or bend the leg at the knee joint (Mickiewicz symptom). Neuropathy of the femoral nerve when it is affected in the area of the inguinal ligament is in general similar to the clinical picture described above. With a high origin of the saphenous nerve, predominantly movement disorders can be observed. Along with the symptoms of tension, pain is detected when pressing in the middle of the inguinal ligament. Compression of the femoral nerve trunk in Gunter's canal is characterized by painful and tactile hypoesthesia of the skin of the medial edge of the knee joint, the anterior inner surface of the leg and the inner edge of the foot. In the same area, paresthesia and pain are observed, which increase in intensity when the lower leg is extended. The latter forces the patient to walk and stand with the leg slightly bent at the knee. The knee reflex is not impaired. Pain is detected at the point of exit of the saphenous nerve from the adductor canal, Tinel's symptom is the appearance of paresthesia along the nerve when it is tapped with a neurological hammer.
Tests and diagnostics
Neuropathy is considered a rather difficult disease to diagnose, which is why it is so important to correctly and thoroughly collect anamnesis. The difficulty lies in the long-term absence of certain symptoms. The doctor will have to find out: whether medications were taken, whether viral diseases were suffered, or whether there was contact with certain chemicals.
The onset of the disease can occur against the background of alcohol abuse. The diagnosis is pieced together based on many factors. Neuropathy can occur in different ways: progressing over several days or years, and even lightning fast.
Using palpation, the doctor examines the nerve trunks, identifying pain and thickening along their course. A Tinnel test is required . This method is based on tapping the nerve ending and identifying tingling in the zone of sensitive innervation.
A laboratory blood test is performed to determine ESR, and sugar levels are measured. Additionally, an X-ray examination of the chest . Electrophoresis of whey proteins is also performed .
Diagnostics
Making a diagnosis of femoral neuropathy requires a careful and thorough examination of the lesion by a neurologist. X-rays of the spine are not very informative, since often neuropathy of the femoral nerve occurs in patients who already have changes in the spinal column (spondyloarthrosis, osteochondrosis) and the radiographic pathology of the spine does not in any way exclude the presence of neuropathy. In such cases, neuropathy is supported by the neural, rather than segmental, nature of the disorders identified during a neurological examination. EMG helps resolve controversial diagnostic situations. With neuropathy, it reveals a slowdown in the conduction of impulses along the femoral nerve, a decrease in the amplitude of the M-response, signs of denervation in the muscles innervated by the femoral nerve and the absence of such signs in the paravertebral muscles of the L2-L4 segments. A relatively new but promising method for studying peripheral nerve trunks is ultrasound, which can be used to assess the integrity of the nerve, identify its tumor changes, swelling, scar-adhesive deformation and degenerative processes. Ultrasound diagnostics of the femoral nerve (ultrasound of the nerve) with dynamic tests allows you to determine the degree of its mobility in the adductor canal. Damage to the femoral nerve needs to be differentiated from vertebrogenic radiculopathies L2-L4, lumbosacral plexopathy (especially occurring against the background of diabetes mellitus), knee injury or gonarthrosis. To exclude pathology of the retroperitoneal space, it is necessary to conduct an ultrasound, CT or MRI.
Treatment
Therapy for non-inflammatory damage to nerve endings is individual in nature and requires not only an integrated approach, but also regular prevention.
Treatment methods are selected depending on the form, degree and causes that contributed to the damage to neuromuscular conduction. All therapy is aimed at fully restoring nerve conduction. In case of toxic damage to the nervous system, detoxification measures are carried out (elimination of influencing factors, administration of an antidote ).
Treatment of diabetic neuropathy
In diabetic cases, measures to maintain normal blood sugar levels are recommended. At the same time, it is recommended to get rid of bad habits. Metabolic disorders in diabetes mellitus contribute to an increase in the level of free radicals circulating in the bloodstream, with impaired antioxidant activity of one’s own organs and systems. All this leads to disruption of the integrity of the inner lining of the vessel and nerve fiber.
For diabetic neuropathy, the use of medications based on alpha-lipoic acid is indicated:
- Thiogamma;
- Berlition;
- Espa-Lipon.
The traditional neurological set involves the introduction vitamins for the complete restoration of neuromuscular conduction. It is not recommended to resort to treatment with folk remedies.
Neuritis of the radial nerve of the right and left hand: ICD-10 code, causes, symptoms and treatment of inflammation
The radial nerve is a structure of mixed fibers. It starts from the cervical plexus and goes towards the hand.
Responsible for the innervation of the arm, flexion movements of the hand and skin sensitivity.
If it is damaged and left untreated, a person is deprived of the ability to act with this limb, to make subtle movements with the hand and fingers. This leads to disability.
The article discusses what radial neuritis is, how it manifests itself, and how it is treated.
What is it and the ICD-10 code
Radial neuritis is an inflammatory pathology that affects the nerve fiber itself and its sheath. Its ICD-10 code is (G56.3) .
Nerve damage is often caused by pinching. This is accompanied by pain, loss of motor function of the arm in the forearm, shoulder and hand with decreased skin sensitivity.
The arm stops bending at the wrist and elbow joints . Its frequent development is facilitated by the anatomical features of the location of this nervous structure.
These include:
- spiral course of the nerve trunk;
- close to the surface of the skin.
Thanks to this, it is easily and quickly affected by any adverse effects.
Causes of inflammation
There are several causes of damage to the radial nerve for the right and left arms.
These include:
- complications after an infectious disease, bacterial or viral;
- traumatic effect on the nerve fiber - this can be prolonged compression and disruption of blood supply due to an uncomfortable sleeping position, using a crutch or a tourniquet to stop bleeding;
- direct injury to the nerve due to injury or bruise, injection into the outer surface of the shoulder;
- compression of the nerve by a keloid scar formed after injury in the space between the muscles;
- toxic effects on nerve fibers from household and industrial toxic substances, carbon oxides, salts of heavy metals (lead, mercury).
These reasons lead to disruption of the conduction of impulses along the nerve fiber of the radial nerve.
Symptoms and manifestations of damage
When the radial nerve is damaged, the patient loses fine motor skills of the hands, and movements in the hand are impaired. He cannot perform both complex and elementary actions with it. There is a loss of sensitivity or a decrease in it in characteristic areas.
Pain along the nerve trunk is extremely rare in patients. This only happens with infectious and traumatic lesions. The right upper limb is more affected.
Manifestations of neuritis of the radial nerve of the right and left hand depend on the location of the inflammation.
Depending on this, the following symptoms occur at different levels:
- With high nerve damage in the armpit area, paralysis of the extensor muscles of the fingers, hand and forearm is observed.
- For lesions in the middle third of the nerve trunk (at the level of the middle third of the shoulder), extension of the forearm and hand is typically affected. Movement in the shoulder is preserved.
- Damage to the nerve in the lower third of the shoulder is manifested by impaired flexion of the fingers and hand. All other movements in the arm (flexion of the weep and forearm) are preserved.
- If the nerve is damaged at the level of the lower part of the forearm, the ability to extend the fingers disappears or decreases. All other functions are retained. Patients develop a “dangling hand” typical of this nerve lesion. The thumb is pressed against the index finger. The patient is unable to shake hands and the fingers are fully extended.
Possible patient complaints
Patients present a variety of complaints of weakness in the arm, fingers and hand, and decreased range of motion. Their pain radiates or even shoots into the third, second and first fingers of the hand.
They complain of numbness in the affected hand, goose bumps in the fingers of the hand, except for the fourth and fifth, the outer side of the shoulder and the inner side of the forearm.
There is a violation of deep and superficial sensitivity in the area of the fingers (I-III) and forearm on the inside. The brush swells and acquires a bluish-purple color.
The patient notes a violation of the flexion of the wrist joint, the fingers do not straighten . Occasionally, numbness along the nerve trunk is possible.
Diagnostic methods
A neurologist treats radial nerve neuritis . First, he asks the patient about complaints and medical history.
Finds out under what circumstances and when the signs appeared. Then the doctor proceeds directly to examining the patient. Based on this, he makes a preliminary diagnosis.
A neurological examination reveals:
- During examination of the patient's hand, a characteristic drooping hand is revealed when the arm is extended forward.
- Difficulties in bending joints are revealed. The patient does not straighten his hand, forearm, and his arm does not straighten at the elbow joint.
- When examined with a neurological hammer, the doctor detects a decrease in the carporadial and extensor reflexes.
- There is a violation of skin sensitivity in the area of the 1st, 2nd, and 3rd fingers.
- A series of tests are performed to determine the level of radial nerve damage. He cannot move his thumb to the side. The patient is unable to simultaneously touch the back of the hands with all fingers. He cannot place his palms on the table and cross his middle and second fingers. A patient with damage to the nerve trunk is unable to spread his fingers to the sides.
Tests and neurological examination data may suggest damage to the radial nerve. It can be confirmed by performing a series of instrumental studies.
Electroneuromyography plays a leading role in making a diagnosis. It allows you to determine a violation of the conduction of a nerve impulse along a nerve fiber and a defect in the innervation of certain muscle groups. There is a decrease in the amplitude of the muscle response to electric current stimulation.
They also conduct electroneurography , which reveals a slowdown in conduction along the nerve trunk.
https://www.youtube.com/watch?v=7eVOFiHypyM
In addition to these studies, additional testing is carried out. They are carried out to identify the cause of damage to the radial nerve.
These include:
- consultations with a traumatologist, orthopedist and endocrinologist;
- blood biochemistry;
- determine blood sugar levels;
- general blood analysis;
- radiography of the bones of the shoulder, forearm, hand;
- CT scan of the elbow and wrist joints.
What diseases should be distinguished from?
Differential diagnosis for neuritis of the radial nerve is carried out with neuropathy . It is characterized by all the same symptoms, but there is no pain syndrome.
Neuritis should also be distinguished from post-traumatic compression of the radial nerve . To do this, a hydrocortisone-novocaine blockade is carried out in the area of its membranes.
When the nerve fiber is compressed, relief of symptoms is observed, which is absent with neuritis.
Features of treatment
Treatment of the radial nerve is carried out only by a neurologist or a rehabilitation specialist. Self-medication is unacceptable. The limb must be immobilized during treatment.
Therapy has two goals. The first is treatment of the underlying disease or injury that led to the nerve damage. The second is the removal of symptoms: pain, swelling, sensory disturbances and decreased muscle strength. Its tactics are determined by the cause of the disease and the level of damage.
The following drugs are used:
- Non-steroidal anti-inflammatory drugs (Ibuprofen, Nimesulide) reduce hand swelling and nerve inflammation.
- Angioprotectors are used to improve regional blood circulation and blood supply to the nerve trunk. Used: Actovegin, Pentoxifylline, Trental.
- Anticholinesterase drugs (Prozerin) enhance the conduction of impulses along the nerve.
- B vitamins improve metabolism in nerve fiber.
For treatment, drugs high in vitamins B1, B6 and B12 are used. Vitamin complexes are used: Neuromultivit, Neurodiclovit and others. - To treat severe pain and swelling, I use glucocorticoids; they have anti-edema and anti-inflammatory properties.
- Antioxidants (Vitamin E, Vitamin C) reduce the severity of damage in the nerve fiber.
In the recovery period for neuritis , physiotherapy, electrical myostimulation, acupuncture, massage, and exercise therapy are prescribed .
Physical therapy plays an important role in the treatment of neuritis of this localization. A set of exercises is developed by a rehabilitation specialist for each patient.
The following exercises are used:
- The patient is seated at the table. He bends at the elbow joint and rests against the surface of the table. In this position, he raises his index finger up and lowers his thumb down. The exercise is performed ten times.
- In the same position, raise your thumb up and your index finger down. The exercise is performed ten times.
- Extend the fingers of the healthy hand ten times. Then grab the fingers of the affected hand into a fist with your healthy hand and squeeze ten times.
In rare cases, if there is no effect from conservative treatment, surgery is performed . With them, the nerve is released from compression.
Consequences and complications
In the absence of systemic and complex treatment, persistent paresis and paralysis of the upper limb and sensory disturbances develop . Disruption of innervation leads to muscle atrophy and joint contractures.
Prognosis and prevention
Radial neuritis responds well to treatment in young people . In the elderly, neuritis, in the presence of concomitant diseases, is difficult to treat. Complications develop quickly.
To prevent diseases, it is necessary to promptly treat the pathologies that cause them. Radiation neuritis is caused by a complex of causes.
With minimal manifestations of illness, numbness, or weakness in a limb, you should consult a doctor and follow all his prescriptions and recommendations .
Otherwise, paralysis and paresis occur, and disability develops. This significantly reduces the patient’s ability to work and quality of life.
on this topic
The video will tell you about the symptoms and treatment of radial neuritis:
Source: https://nerv.guru/zabolevaniya/nevrit/tipy-i-vidy/konechnostej/luchevogo-nerva.html
Medicines
Treatment of lower extremity neuropathy includes the following medications:
- Neuroprotectors or metabolic accelerators in nerve cells. Drugs for treatment: Mildronate ; Piracetam .
- Anticholinesterase medications , the action of which is aimed at optimizing the sensory functioning of nerve endings. The drugs improve neuromuscular conduction of the lower extremities. These include: Prozerin ; Ipidacrine .
- Antioxidants. Prevent negative consequences from the influence of free radicals on the functioning of the nervous system. A high concentration of free radicals has a destructive effect on the tissues of the peripheral nervous system. Preparations: Cytoflavin ; Mexidol .
- Alpha lipoic acid. The drugs help restore neurocytes and speed up metabolism. High effectiveness is observed in diabetic neuropathy.
- Other medications. The use of B vitamins has a good effect; in particular, B1 , B6 , B12 . Vitamin complexes help restore neuromuscular conduction. There are tablet and injection forms: Milgamma ; Neuromultivitis ; Combilipen .
Self-treatment at home is not recommended.
Treatment of neuropathic pain in adults
Neuropathic pain - what is it?
Neuropathic pain occurs when the transmission of impulse signals along the nerves is disrupted. In adults, neuropathic pain syndrome is described as stabbing, burning, shooting and is often associated with electric shock.
Therapy begins with the simplest painkillers ( Ibuprofen, Ketonal ). If they are ineffective and the pain syndrome is severe, antidepressants and antiepileptic drugs (for example, Tebantin ) are prescribed.
Tricyclic antidepressants
Drugs in this group are often used to relieve neuropathic pain. It is believed that the mechanism of their action is based on preventing the transmission of nerve impulses. The most commonly prescribed medication is Amitriptyline . The effect may occur within a few days, but in some cases, pain therapy is extended for 2-3 weeks. The maximum effect of therapy is recorded at 4-6 weeks of intensive treatment. A side effect of therapy is drowsiness , which is why treatment begins with the smallest doses, gradually increasing the dosage for better tolerability. Drinking plenty of fluids is recommended.
Anticonvulsants, antiepileptic drugs
If it is impossible to use antidepressants, anti-epileptic drugs ( Pregabalin, Gabapentin ) are prescribed. In addition to the treatment of epilepsy, medications are excellent for relieving neuropathic pain syndrome. Treatment begins with the smallest doses, identical to antidepressant therapy.
POLYNEUROPATHIES AND OTHER LESIONS OF THE PERIPHERAL NERVOUS SYSTEM (G60-G64)
Excludes: neuralgia NOS ( M79.2 ) neuritis NOS ( M79.2 ) peripheral neuritis during pregnancy ( O26.8 ) radiculitis NOS ( M54.1 )
G60 Hereditary and idiopathic neuropathy
G60.0 Hereditary motor and sensory neuropathy Disease: • Charcot-Marie-Toots • Dejerine-Sotta Hereditary motor and sensory neuropathy, types I-IY. Hypertrophic neuropathy in children Peroneal muscular atrophy (axonal type) (heper trophic type). Roussy-Levi syndrome G60.1 Refsum's disease G60.2 Neuropathy in combination with hereditary ataxia G60.3 Idiopathic progressive neuropathy G60.8 Other hereditary and idiopathic neuropathies. Morvan's disease. Nelaton's syndrome Sensory neuropathy: • dominant inheritance • recessive inheritance G60.9 Hereditary and idiopathic neuropathy, unspecified
G61 Inflammatory polyneuropathy
G61.0 Guillain-Barre syndrome. Acute (post-)infectious polyneuritis G61.1 Serum neuropathy. If it is necessary to identify the cause, use an additional code of external causes (class XX). G61.8 Other inflammatory polyneuropathies G61.9 Inflammatory polyneuropathy, unspecified
G62 Other polyneuropathies
G62.0 Drug-induced polyneuropathy If necessary, identify the drug, use an additional code for external causes (class XX). G62.1 Alcoholic polyneuropathy G62.2 Polyneuropathy caused by other toxic substances If it is necessary to identify a toxic substance, use an additional code for external causes (class XX). G62.8 Other specified polyneuropathies. Radiation polyneuropathy If necessary, identify the cause, use an additional code for external causes (class XX). G62.9 Polyneuropathy, unspecified. Neuropathy NOS
G63* Polyneuropathy in diseases classified elsewhere
G63.0 * Polyneuropathy in infectious and parasitic diseases classified in other headings Polyneuropathy in: • diphtheria ( A36.8 +) • infectious mononucleosis ( B27 . -+) • leprosy ( A30 . -+) • Lyme disease ( A69.2 +) • mumps ( B26.8 +) • herpes zoster ( B02.2 +) • late syphilis ( A52.1 +) • congenital syphilis ( A50.4 +) • tuberculosis ( A17.8 +) G63.1 * Polyneuropathy in neoplasms ( C00 - D48 +) G63.2 * Diabetic polyneuropathy ( E10 - E14 + with a common fourth sign .4) G63.3 * Polyneuropathy in other endocrine diseases and metabolic disorders ( E00 - E07 +, E15 - E16 +, E20 - E34 +, E70 - E89 +) G63.4 * Polyneuropathy with malnutrition ( E40 - E64 +) G63.5 * Polyneuropathy with systemic connective tissue lesions ( M30 - M35 +) G63.6 * Polyneuropathy with other bone diseases -muscle lesions ( M00 - M25 +, M40 - M96 +) G63.8 * Polyneuropathy in other diseases classified in other headings. Uremic neuropathy ( N18.8 +)
G64 Other disorders of the peripheral nervous system
Peripheral nervous system disorder NOS
Procedures and operations
In addition to drug therapy, neuropathy of the peroneal nerve also includes physiotherapeutic procedures:
- Magnetotherapy. It is based on the effect of a magnetic field on the human body, which helps relieve pain, restore nerve cells, and reduce the severity of the inflammatory reaction.
- Amplipulse. It is based on the effect of modulated current on the affected area, due to which nerve cells are restored and swelling is reduced. Has an anti-inflammatory effect.
- Electrophoresis with drugs . It is based on the influence of an electric field, due to which medications enter the site of inflammation.
- Ultrasound therapy. When exposed to ultrasound, blood circulation is stimulated and the severity of pain is reduced. Has a tonic and anti-inflammatory effect.
- Electrical stimulation. Restoration of neuromuscular conduction occurs under the influence of electric current.
Radial nerve neuropathy is treated in the same way. A course massage is also recommended to restore the radial nerve.
Additional facts
Neuropathy of the peroneal nerve, or peroneal neuropathy, occupies a special position among peripheral mononeuropathies, which also include: neuropathy of the tibial nerve, neuropathy of the femoral nerve, neuropathy of the sciatic nerve, etc. Since the peroneal nerve consists of thick nerve fibers that have a larger layer of myelin sheath, it more susceptible to damage due to metabolic disorders and anoxia.
This point is probably responsible for the fairly wide prevalence of peroneal neuropathy. According to some data, neuropathy of the peroneal nerve is observed in 60% of patients in traumatology departments who have undergone surgery and are treated with splints or plaster casts. Only in 30% of cases, neuropathy in such patients is associated with primary nerve damage.
It should also be noted that often specialists in the field of neurology have to deal with patients who have a certain history of peroneal neuropathy, including the postoperative period or time of immobilization. This complicates treatment, increases its duration and worsens the result, since the earlier therapy is started, the more effective it is.
The superficial peroneal nerve runs along the anterolateral surface of the leg, where it gives off a motor branch to the peroneal muscles, which are responsible for pronation of the foot with its simultaneous plantar flexion. In the area of the medial 1/3 of the leg, the superficial branch of the n peroneus passes under the skin and is divided into 2 dorsal cutaneous nerves - the intermediate and medial.
The first innervates the skin of the lower 1/3 of the leg, the dorsum of the foot and the III-IV, IV-V interdigital spaces. The second is responsible for the sensitivity of the medial edge of the foot, the back of the first toe and the II-III interdigital space. Anatomically determined areas of greatest vulnerability of the peroneal nerve are: the place where it passes in the area of the head of the fibula and the place where the nerve exits the foot.
Prevention
Preventive measures include timely treatment of infectious and systemic diseases, normalization of general metabolism. It is important to understand that pathology can become chronic, which is why timely and competent treatment is so important.
In case of a mild course of the disease and a chronic form of neuropathy, sanatorium-resort treatment is indicated, where the following is carried out:
- aromatherapy;
- laser and light treatment;
- magnetic therapy;
- massage, exercise therapy;
- acupuncture;
- psychotherapy.
Consequences and complications
There are many complications from peripheral neuropathy and they depend primarily on the causative factor that led to damage to the nerve trunk. Main complications:
- Diabetic foot. It is considered one of the most terrible complications of diabetes.
- Gangrene . The cause of the putrefactive process is the complete lack of blood flow in the affected area. The pathology requires emergency surgical treatment: excision of necrotic areas, amputation of a limb.
- Autonomic cardiovascular neuropathy. It is characterized by disturbances in various autonomic nervous functions, including sweating, bladder control, heart rate, and blood pressure .
Additional facts
Neuropathy of the peroneal nerve, or peroneal neuropathy, occupies a special position among peripheral mononeuropathies, which also include: neuropathy of the tibial nerve, neuropathy of the femoral nerve, neuropathy of the sciatic nerve, etc. Since the peroneal nerve consists of thick nerve fibers that have a larger layer of myelin sheath, it more susceptible to damage due to metabolic disorders and anoxia. This point is probably responsible for the fairly wide prevalence of peroneal neuropathy. According to some data, neuropathy of the peroneal nerve is observed in 60% of patients in traumatology departments who have undergone surgery and are treated with splints or plaster casts. Only in 30% of cases, neuropathy in such patients is associated with primary nerve damage. It should also be noted that often specialists in the field of neurology have to deal with patients who have a certain history of peroneal neuropathy, including the postoperative period or time of immobilization. This complicates treatment, increases its duration and worsens the result, since the earlier therapy is started, the more effective it is. The superficial peroneal nerve runs along the anterolateral surface of the leg, where it gives off a motor branch to the peroneal muscles, which are responsible for pronation of the foot with its simultaneous plantar flexion. In the area of the medial 1/3 of the leg, the superficial branch of the n peroneus passes under the skin and is divided into 2 dorsal cutaneous nerves - the intermediate and medial. The first innervates the skin of the lower 1/3 of the leg, the dorsum of the foot and the III-IV, IV-V interdigital spaces. The second is responsible for the sensitivity of the medial edge of the foot, the back of the first toe and the II-III interdigital space. Anatomically determined areas of greatest vulnerability of the peroneal nerve are: the place where it passes in the area of the head of the fibula and the place where the nerve exits the foot.