Neuralgia is a lesion of peripheral nerves, accompanied by intense pain in the area of innervation of a particular nerve. If symptoms appear, you should seek medical help immediately. The prognosis for early treatment is favorable. Neuralgia refers to severe shooting pain that occurs due to a damaged or irritated nerve. Neuralgia can affect any part of the body, causing mild to severe pain. Certain medications and surgical procedures can effectively treat neuralgia.
Severe neuralgia can affect a person's ability to perform everyday tasks and can affect their quality of life.
Neuralgia has many possible causes, including:
- infections such as shingles, Lyme disease, or HIV
- pressure on bone nerves, blood vessels or tumors
- other medical conditions such as kidney disease or diabetes
- aging
Causes of neuralgia
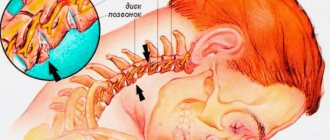
During prolonged physical activity, microtraumas of the nerve trunk occur. These disorders can occur due to damage by toxins of various etiologies, which are either infectious in nature or occur as a result of alcohol intoxication, taking medications or interaction with heavy metals. Causes, symptoms and treatment depend on the type of disease: knee joint, lower extremities, facial nerve, solar plexus, pelvic, intervertebral, vagus nerve, etc. Causes of neuralgia:
- osteochondrosis;
- hypothermia;
- diseases associated with the musculoskeletal system and hip joint (congenital anomalies of joints and bones, spinal injuries);
- tumors;
- diabetes;
- peripheral vascular diseases that disrupt the blood supply to nervous tissue;
- atherosclerosis.
Other reasons
As for the reasons that provoke short-term transient pain in the sternum with neuralgia, most people encounter similar factors in their lives:
- hypertonicity of muscle tissue;
- spasms in unprepared muscles during sudden loads or stretches;
- long stay of the body in an uncomfortable position (at work or during rest);
- crooked posture;
- stress or overwork;
- hormonal imbalance.
Diabetic neuropathy
The most common chronic complication of diabetes mellitus.
Due to metabolic disorders and changes in the vessels supplying the nerves, demyelination, atrophy and degeneration of axons, atrophy of neurons in the anterior horns and intervertebral ganglia occur; signs of nerve regeneration and changes in the vessels supplying the nerves also appear.
Classification: segmental symmetric neuropathy (distal sensory and sensorimotor neuropathy, diabetic long fiber neuropathy, chronic inflammatory demyelinating polyradiculoneuropathy) and asymmetric neuropathy (mononeuropathy, multiple mononeuropathy, radiculopathy, lumbar plexopathy, chronic demyelinating polyradiculopathy) generalized symmetric polyneuropathy ( chronic sensorimotor, autonomic or acute sensory), focal or multifocal neuropathies.
Forms of neuropathy:
1.
Chronic sensorimotor polyneuropathy (so-called painful, the most common): paresthesia and dysesthesia of the hands and feet; painful muscle spasms and attacks of acute pain; loss of superficial and deep sensitivity; muscle weakness; weakened or absent tendon reflexes; trophic changes; autonomic disorders; symptoms appear chronically, have no connection with physical activity, and usually worsen at night. Diagnostic tests: tactile sensitivity test (on the sole) with a monofilament with a pressure force of 10 g (for example, Semmes-Weinstein caliber 5.07, which is applied to specific points on the foot for ≈1.5 seconds with a force that causes it to flex); vibration sense testing (recommended every 6–12 months) with a tuning fork (128 Hz applied to the lateral and medial malleolus, upper part of the fibula, base of the big toe and fifth toe); study of pain sensations (on the sole) with a sterile needle, and study of temperature sensitivity - with a pointer with 2 tips: metal and plastic. If indicated, nerve conduction studies are performed and electromyographic studies are performed. 1) cardiovascular system - mainly manifested by orthostatic hypotension and syncope. Diagnostic studies: so-called. Ewing tests, i.e., a set of tests to detect the absence of heart rate variability during deep breathing, the upright position and the Valsalva maneuver, as well as orthostatic hypotension during the transition to an upright position or the absence of an increase in pressure during compression of the dynamometer.
2) gastrointestinal tract - manifested by motility disorders. Diagnostic studies: including X-ray examination of the stomach, ultrasound of the stomach, manometry of the gastrointestinal tract, electrogastrography, isotope studies (assessment of residual food content in the stomach).
3) the genitourinary system is one of the most common causes of erectile dysfunction (in ≈50% of men with diabetes); in women it can cause vaginal dryness and decreased libido; causes urinary retention in the bladder (assessed by ultrasound after urination).
4) others - for example, the organ of vision (including abnormal reaction of the pupils to light), impaired sweating, taste and salivation.
First of all, compensation of carbohydrate metabolism; exclusion of hypoglycemia; it is possible to prescribe an ACEI.
2. Symptomatic treatment of painful polyneuropathy up
1) treatment of neuropathic pain → section. 22.1; including antiepileptic drugs - pregabalin 150–600 mg/day, gabapentin 900–1800 mg/day, carbamazepine up to 800 mg/day; tricyclic antidepressants - for example, amitriptyline 25–150 mg/day; selective serotonin reuptake inhibitors - for example, paroxetine 20–40 mg/day; paracetamol ≤1500 mg/day or NSAIDs; opioids - for example, tramadol 50–400 mg/day, codeine 0.5–1 mg/kg bw per day in 4 divided doses; local anesthetics - capsaicin, lidocaine; up
2) lipoic acid 600 mg/day, during the first 2–4 weeks. i.v., later p.o. In a number of European countries, alpha-lipoic acid is recognized as an ineffective, but possible drug for the treatment of neuropathy.
3. Treatment of symptomatic autonomic neuropathy 1) fainting → section. 23.2.1;
2) gastric atony - diet modification (frequent intake of small portions of food, in severe forms - a liquid or semi-liquid diet), prokinetics (eg, cisapride), erythromycin, drugs inhibiting gastric secretion → section. 4.7; for severe gastric paresis - surgical treatment, stimulation of the bioelectrical activity of the stomach;
3) intestinal dysfunction—diet modification (eg, gluten-free, lactose restriction), cholestyramine, clonidine, octreotide, antidiarrheals (loperamide), pancreatic enzymes, antibiotics;
4) bladder atony - avoidance of urinary retention, parasympathomimetics (eg, bethanechol), bladder catheterization (temporary or permanent);
5) erectile dysfunction - phosphodiesterase type 5 inhibitors (sildenafil, tadalafil, vardenafil). Avoid co-administration with nitrates in patients with coronary heart disease.
6) sweating disorders - botulinum toxin, vasodilators, moisturizing creams.
Source: //empendium.com/ru/chapter/B33.II.13.4.3.
What are the types of neuralgia?
There are two main classifications of this condition:
- depending on the reason.
- depending on which nerve is affected.
Depending on the cause, primary and secondary neuralgia are distinguished.
Primary is an independent disease. It is also called idiopathic and essential. There are no concomitant diseases that could lead to nerve damage.
Secondary - occurs as a symptom of another disease. Its other name is symptomatic. Separately, there is postherpetic neuralgia, which is a complication of herpes zoster.
Depending on which nerve is affected, neuralgia is distinguished:
- trigeminal nerve;
- glossopharyngeal nerve;
- pterygopalatine node; intercostal;
- costoclavicular;
- external cutaneous nerve of the thigh;
- occipital
General information
With the so-called primary, or essential
, neuralgia clinical examination does not reveal any other diseases;
with secondary, or symptomatic
, neuralgia, inflammatory, tumor and other processes are detected that have a negative effect on the nerve.
Neuralgia can occur in any part of the body: from the head to the feet. In most cases, neuralgia appears as a result of various injuries, infections or severe forms of colds. Hypothermia is another good reason for the appearance of neuralgia. In the case of a prolonged course, neuralgia passes into the neuritic stage, that is, pronounced structural changes in the nerve and loss of sensitivity appear.
Symptoms of neuralgia
The main symptom of the disease is severe pain that develops suddenly, like a lumbago. It penetrates the affected area, accompanied by a strong burning sensation. The localization of pain depends on the affected nerve:
- with trigeminal neuralgia, the patient is bothered by severe itching of the nose and face, which is replaced by an attack of pain covering the face;
- when the intercostal nerve is damaged, pain passes between the ribs, encircles the torso and intensifies when sneezing, coughing and even during breathing;
- if the external cutaneous nerve of the thigh is affected, severe pain will develop in the outer surface of the thigh, the affected area itches and burns;
- Inflammation or pinching of the glossopharyngeal nerve is characterized by attacks of pain in the pharynx with innervation to the ear and lower jaw.
Diagnostics
If the symptoms listed above appear, you must contact a medical facility as soon as possible to conduct a comprehensive diagnosis and prescribe the correct treatment plan. The doctor can assume the presence of such an illness during an initial examination and assessment of the patient’s complaints. To confirm the preliminary diagnosis, the patient is referred for additional examinations.
Diagnostic methods:
- X-ray;
- CT;
- NMR;
- blood analysis;
- Analysis of urine;
- blood biochemistry.
Treatment of neuralgia
It is necessary, first of all, to treat the underlying disease, as well as carry out symptomatic treatment.
Physical rest, bed rest for sciatica.
Painkillers and anti-inflammatory:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): diclofenac sodium, nimesulide, naproxen, ibuprofen, etc.
- Complex – analgin + amidopyrine;
- Antispasmodics: Baclofen, Mydocalm, Sirdalud.
For severe pain, the following medications may be prescribed:
- Anticonvulsants: Tegretol, Finlepsin (Carbamazepine), Difenin (Phenytoin), Oxacarbazepine (Trileptal).
- Antidepressants for very severe pain: Amitriptyline, Duloxetine.
Anti-inflammatory ointments can be used topically: Diclofenac sodium (Voltaren), Ketonal, Ibuprofen, Sustamed (with bear fat), ointments with snake venom, etc.
Blockade with solutions of local anesthetics (Novocaine, Lidocaine, etc.) and steroid hormones (as anti-inflammatory).
- Vitamins B1 and B12 in the form of injections, vitamin C, E.
What can you do?
During an attack of neuralgia, you can take a painkiller and rub ointments with anti-inflammatory and painkillers into the affected area. After this, the pain may subside or disappear completely. But the problem remains unresolved - new attacks will arise in the future. Therefore, it is necessary to consult a doctor. A neurologist treats neuralgia.
We found no evidence of level 1 quality. Based on level 2 evidence of at least a 50% reduction in pain intensity, gabapentin is significantly better than placebo for postherpetic neuralgia and painful diabetic neuropathy. There is insufficient information to draw reliable conclusions about other disease states. We found no obvious difference between standard gabapentin formulations and newly introduced drugs or between different doses of gabapentin.
The occurrence of adverse events was significantly increased with gabapentin. Serious side effects occurred in 3% of participants taking gabapentin and were no more common than placebo. Data were insufficient for direct comparison with other active treatments. There was only level 3 evidence for other disease states.
ethnoscience
Traditional medicine can be used in combination with basic medications. There are several time-tested food products that help improve the course of pathological processes.
You can try rubbing in a 10% mummy solution. To do this, the powder must be dissolved in water. The ointment is rubbed in once a day for 5 minutes. The duration of the course of therapy is 3 weeks. You need to do everything again after a pause of 10 days.
Radish juice is used as a skin treatment or compress.
Related posts:
- Left side hurts Pain is a complex process, the occurrence of which is not fully understood. She…
- Hemorrhagic stroke Hemorrhagic stroke (hypertensive intracerebral hemorrhage) is a polyetiological nosological form,…
- Prolactin: what is this hormone? The human body produces many vital hormones every day. Their balance...
- Ingrown nail Onychocryptosis is the ingrowth of part of the nail plate into the tissue of the nail fold...