Ganglionitis of the pterygopalatine ganglion.
Sluder syndrome is characterized by sharp pain in the periorbital region, in the eyeball, in the root of the nose, in the upper and lower jaws, and sometimes in the teeth.
The pain radiates to the tongue, soft palate, temple, back of the head, ear, neck, shoulder blade, and shoulder. The pain lasts from several minutes to several hours. Necessarily pronounced vegetative symptoms - hyperemia and swelling of the skin of half the face, lacrimation, rhinorrhea. There is hyperemia and swelling of the mucous membrane of the posterior nasal cavity. The painful attack stops after application of anesthesia to the posterior part of the nasal cavity, which serves as a differential diagnostic criterion, which indicates the presence of ganglionitis of the pterygopalatine ganglion in the patient.
Complications
Anterior exudative uveitis in nasociliary nerve syndrome is complicated by serous retinal detachment and papilledema. Disruption of the innervation of the anterior segment of the eye leads to xerophthalmia. Patients are at risk of developing bacterial and infectious complications (conjunctivitis, keratitis, iritis). If the innervation of the mucous membrane of the nasal cavity deteriorates over a large area, there is a high probability of a decrease in the sense of smell (anosmia). A common complication is atrophic rhinitis, rhinosinusitis. The pathology is accompanied by the development of dysmia, which is not associated with dysembryogenetic stigmas.
General information
The auricular autonomic ganglion is a collection of interneurons of the sympathetic and parasympathetic nerve pathways. The node receives sympathetic preganglionic fibers through the plexus of the middle meningeal artery, and parasympathetic fibers from a branch of the glossopharyngeal nerve. Postganglionic fibers of the auricular ganglion are part of the auriculotemporal nerve, which is a branch of the trigeminal nerve. They go to the ear gland and vessels of the temporal region, providing their autonomic innervation.
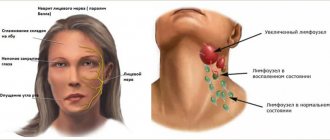
Neuralgia of the ear ganglion is included in the group of vegetative ganglionitis of the head, which also includes neuralgia of the submandibular and sublingual ganglion, ganglionitis of the ciliary ganglion, ganglionitis of the pterygopalatine ganglion and the upper cervical sympathetic ganglion, cervical truncitis. Specialists in the field of neurology have collected statistical data indicating that neuralgia of the ear ganglion is most common in middle-aged and young women.
Neuralgia of the ear ganglion
Causes
Etiopathogenetically, neuralgia of the ear node is an irritative disease that develops reflexively in the presence of pathological autonomic impulses coming from chronic infectious foci or chronic processes in somatic organs. The most important pathology is one that is localized in the same region as the ear node and is infectious and inflammatory in nature. These include diseases of the parotid gland (mumps, sialadenitis, stones), chronic purulent otitis, chronic tonsillitis, sinusitis (frontal sinusitis, sinusitis, ethmoiditis), dental diseases (chronic periodontitis, stomatitis, gingivitis, periodontitis).
Less common is neuralgia of the ear node, caused by the presence of a distant source of infection (pyelonephritis, urethritis, cystitis), a general infectious process (tuberculosis, syphilis, chronic sepsis), metabolic disorders due to endocrine pathology (hyperthyroidism, diabetes mellitus) or somatic disease (cirrhosis of the liver). , cholecystitis, chronic renal failure, chronic gastritis, gastroduodenitis, adnexitis).
Neuralgia of the nasociliary nerve (Charlen's syndrome).
Characterized by attacks of acute pain in the eyeball area. Pain often occurs at night and is accompanied by severe autonomic symptoms (rhinorrhea, lacrimation, photophobia, hyperemia of the conjunctiva of the eye). The attack of pain lasts about half an hour, and sometimes several hours. On palpation there is pain in the eyeball. The appearance of herpetic rashes on the skin of the forehead and nose is typical. Patients may develop conjunctivitis and keratitis.
There are excruciating pains in the area of the eyeball and eyebrows, radiating to the corresponding half of the nose. The pain occurs at night, and vegetative symptoms are pronounced. Pain on palpation of half the nose and the inner corner of the orbit. Herpetic eruptions on the skin of the nose and forehead. Phenomena of keratoconjunctivitis.
Classification
Charlin's syndrome is an acquired pathology. Congenital cases have not been described, but in some cases it is possible to trace a genetic predisposition to the development of the disease. From a clinical point of view, the disease is classified into the following forms:
- Typical neuralgic
. It develops when the main nerve trunk is damaged and manifests itself with classic symptoms of neuralgia. In most patients, trigger points can be identified. - Erased hyperpathic
. Occurs when small terminal branches are affected. This option is characterized by atypical neuropathic sensations, among which hyperpathia and dysesthesia dominate. The trigger point cannot be detected, but zones of hypoesthesia appear.
Sources
- https://medistoriya.ru/nevrologiya/nevralgiya-nosoresnichnogo-nerva.html
- https://www.krasotaimedicina.ru/diseases/zabolevanija_neurology/Charlin
- https://1neurologia.ru/nevralgiya/sindrom-charlina/
- https://stom4you.ru/nevralgiya-nosoresnichnogo-nerva-sindrom-charlina.html
- https://neuro-logia.ru/zabolevaniya/nevralgiya/nosoresnichnogo-nerva.html
[collapse]
Symptoms of neuralgia of the ear node
Neuralgia of the ear ganglion is manifested by attacks of vegetalgia that occur in front of the opening of the external auditory canal, in the parotid region and in the ear on the affected side. Intense burning or throbbing pain radiates to the lower jaw, behind the ear, to the back of the head, neck and shoulder girdle of the corresponding side. The reflex mechanism of pain irradiation leads to its spread to the upper chest and arm. Painful paroxysms can be provoked by ingestion of hot food or drinks, hypothermia of the face, psycho-emotional stress, and excessive physical activity. The duration of an attack of vegetalgia, as a rule, is several minutes, but can be an hour or more.
The dependence of the functioning of the autonomic nervous system on external factors (lighting, barometric pressure, temperature changes, air humidity, etc.) determines the characteristic rhythm of vegetalgia - its occurrence mainly in the evening and at night, exacerbation in the autumn and spring.
In some cases of neuralgia, a paroxysm of pain is accompanied by ear congestion or a sensation of clicking in it. The latter is caused by periodic reflex spasms of the muscles of the auditory tube. Often during an attack, patients note a noticeable increase in salivation, while in the interictal period hypersalivation is not observed. Hearing function is not affected.
Diagnosis of the disease
The diagnosis of trigeminal neuralgia is established by a neurologist. A preliminary diagnosis is established on the basis of the patient’s characteristic complaints and typical medical history.
During the examination, the neurologist pays attention to the presence of specific complaints and symptoms.
The presence of typical complaints in a patient with trigeminal neuralgia is decisive in diagnosis.
The patient complains of the following:
- paroxysmal, severe pain in one half of the face, it alternates with light intervals;
- the appearance of pain is preceded by itching, redness of the facial skin or goosebumps;
- exposure to the trigger zone provokes an attack;
- the pain is burning, occurs suddenly, is comparable to the passage of an electric current and never changes its character.
In the anamnesis, the patient indicates a head injury or herpetic rashes on half of the face, where pain is bothersome.
Neurologists, along with a general neurological examination, examine in detail the functions of the cranial nerves.
When examining a person, he pays special attention to the following signs:
- the exit points of the trigeminal nerve of its three branches are examined (on the forehead, near the nose and on the chin);
- a search is underway for trigger zones that trigger an attack of pain;
- decreased superficial sensitivity on the skin of half the face.
The patient is prescribed standard general clinical laboratory tests (complete blood count, urinalysis, blood biochemistry) and no changes are detected.
There are no specific laboratory tests for trigeminal neuralgia. These methods are used for differential diagnosis with viral lesions of the nervous system.
In the diagnosis of trigeminal neuralgia, instrumental examination methods are widely used.
Differential diagnosis is carried out with several diseases manifested by pain in the face.
It is advisable to do this with the following pathologies:
- Neuritis of the facial nerve - it is characterized by constant aching pain without light intervals. It gets worse at night. There are no convulsive contractions at the height of a painful attack.
- Inflammation of the ganglion of the pterygopalatine ganglion - characterized by sharp, intense pain in the periorbital region, eyes, nose, and root of the tongue. It is accompanied by redness of the skin, lacrimation and swelling of the nasal mucosa.
- Inflammation of the semilunar ganglion - it is characterized by loss of sensitivity on the affected side and rashes on the skin.
- Inflammation of the ciliary ganglion is characterized by pain in the eye area, which radiates to the eyebrow on the same side and half of the nose.
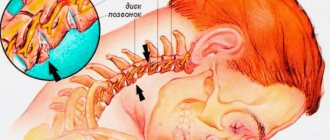
- Osteochondrosis of the cervical spine - it is typical that shooting pains intensify when turning the head.
- Toothache – with pulpitis, the pain intensifies at night. A tooth affected by caries is identified.
- Arthritis of the jaw joint - it is typical that the pain intensifies with chewing movements and opening the mouth.
- Sinusitis - with it the pain is aching in nature. An X-ray of the skull reveals the level of fluid in the affected sinus.
- Otitis media - it is characterized by constant pain that gets worse at night. The patient's body temperature rises.
Trigeminal neuralgia is manifested by characteristic pain. For an experienced neurologist, making this diagnosis is not difficult due to the characteristic clinical picture. Conducting a comprehensive examination of the patient is important to establish a diagnosis and prescribe adequate treatment.
Patients often turn to a dentist or otolaryngologist for help, and are then referred to a neurologist for consultation. The latter makes a diagnosis based on typical complaints, the presence of sharp pain on palpation of the sclerotomal points of the auriculotemporal, mental and mandibular nerves, Richet's point - the place where the ear ganglion anastomoses with the mandibular nerve. The detection of hyperalgesia in the parotid region also speaks in favor of neuralgia. In a difficult diagnostic situation, they resort to diagnostic novocaine or lidocaine blockade of the ear ganglion.
In the diagnostic process, determining the etiology of neuralgia plays an important role. For this purpose, a dental examination and ultrasound of the parotid salivary gland, an otolaryngological examination (audiometry, otoscopy, rhinoscopy, pharyngoscopy, radiography of the paranasal sinuses) are performed. If necessary, consultations with specialized specialists (urologist, gastroenterologist, gynecologist, endocrinologist, etc.) and additional studies of somatic organs (gastroscopy, ultrasound of the abdominal cavity, ultrasound of the kidneys, study of thyroid hormone levels, etc.) are prescribed.
Differential diagnosis includes otitis media, eustachitis, trigeminal neuralgia, mumps, tumors, cysts and stones of the parotid gland.
Causes, signs and treatment of Frey's syndrome
Frey's syndrome is a type of facial pain that is rare. What signs can be attributed specifically to this pathology, and why do those suffering from this disease hate chewing gum? By learning about the most effective methods of treating Frey's syndrome, you can get rid of the unpleasant condition faster.
Why does Frey's syndrome appear?
SindromFrey is a diagnosis that in 90% of cases is given to patients due to an unforeseen complication of surgical intervention on the parotid salivary glands or others located within 1-3 cm of tissue. Often, after operations performed in the cervical spine, symptoms of Frey's syndrome appear.
Since, as a result of the surgeon's actions, the nerve endings may be cut in some way, their further development is disrupted, and the nerve fibers may grow excessively, causing discomfort to the patient, or join other glands, changing their own function, thereby also causing inconvenience.
In addition to incorrect actions of the surgeon, risk factors for the development of parotid neuralgia include:
- injuries and tumors of the neck and head;
- inflammatory processes;
- neuralgia of nearby areas.
There are frequent cases of the disease manifesting itself in people who are fond of piercing and scarring.
Neuralgia of the parotid and temporal region is a disease of adults; in rare cases, it is observed in newborns. The causes of the anomaly in children are birth injuries that lead to nerve compression. In persons under 30 years of age, the pathology, if it is not congenital, is not recorded in any source.
How not to miss the development of auriculotemporal syndrome?
Many patients notice signs of Frey's Syndrome several months after surgery. Symptoms are initially temporary and begin more often during meals, that is, during the process of chewing food. Signs of pathology disappear, accordingly, only when the chewing process is completed.
A person suffering from this disease can be recognized by the following signs:
- increased sweating in the ear area;
- redness and hyperthermia of the affected area;
- pain spreading to the lower face and ear;
- numbness of some areas of the skin;
- feeling of stuffiness in the ear.
In addition to the process of chewing, massage or involuntary pressure in the area under the jaw can lead to these unpleasant sensations.
Attacks occur more frequently, and if you do not respond to them, the symptoms will become more pronounced.
With obvious progress of neuralgia, Frey's syndrome will make its existence known even after minor stress or minor hypothermia. Therefore, it is better not to postpone a visit to the dentist.
How is the diagnosis done?
In order to accurately determine Frey's syndrome, it is necessary to exclude a number of other diseases, sometimes similar in several symptoms.
To do this, after an examination, which includes several otolaryngological methods, and collection of data from the patient, specific tests are performed. If at the time of an attack a 2% solution of novocaine is injected subcutaneously, the symptoms will disappear.
Or a solution of starch and iodine is applied to the affected area; when the process is stimulated, the area turns shades of blue.
As part of the diagnosis, radiography and ultrasound are required.
Glossopharyngeal nerve.
Paroxysmal pain that begins at the root of the tongue or in the tonsil area. They radiate to the palate, pharynx, ear, eye, lower jaw and even neck. Pain occurs when talking, swallowing, eating food (especially very cold or hot). The attacks last 1-3 minutes. The intervals between attacks vary. During an attack, a dry throat appears, and after an attack of pain, increased salivation occurs.
When carrying out differential diagnosis of this disease, one must remember that pain always begins at the root of the tongue or in the tonsil area, and mechanical irritation of these areas always provokes an attack. When the root of the tongue, tonsil and posterior wall of the pharynx are lubricated with an anesthetic (dicaine, pyromecaine), the attacks stop.
It is characterized by attacks of cutting pain in the area of the external auditory canal with irradiation to the face and mastoid area. The pain occurs acutely and subsides gradually. The occurrence of an attack of pain is provoked by palpation of the external auditory canal.
Will folk remedies help with “Charlina” syndrome?
The pain that occurs as a result of neuralgia of the nasociliary ganglion is quite noticeable and often debilitating. Medicines prescribed by medicine, although they have analgesic properties, can be addictive. Moreover, the pain goes away only for a certain period of time. There are times when some medications recommended by a neurologist do not help. Then patients turn to traditional healers. They, in turn, share their knowledge in the field of treating neuroses.
Aesculapians among the people often recommend the following recipes in the fight against neuralgia of the nasociliary nerve:
- Lilac buds should be boiled until thick, then mixed with pork fat (fresh). After thorough mixing, you will get an ointment that is applied to the affected area.
- Squeeze the juice of black radish and rub it on the sore spot.
- The leaves and roots of ordinary horseradish have proven themselves to be quite good. They must be rubbed through a grater and applied to the affected area.
- It is useful to drink decoctions and infusions of various herbs (mint, yarrow, chamomile, birch buds and some others)
We must remember that traditional methods can be effective in combination with the treatment prescribed by the doctor. Self-medication for neuralgia of the nasociliary ganglion is excluded.
Treatment of neuralgia of the ear node
Emergency care aimed at relieving paroxysms of vegetalgia includes the use of anti-inflammatory and analgesic drugs: metamizole sodium, acetylsalicylic acid, aminophenazone, therapeutic novocaine blockades. They are combined with ganglion blockers (benzohexonium, pachycarpine), antispasmodics (drotaverine, ganglefen), sedatives (motherwort, valerian, bromine preparations) and hypnotics (phenobarbital, barbamyl, zopiclone). An additional analgesic effect is provided by electrophoresis with novocaine or ultraphonophoresis with hydrocortisone on the area of the ear node.
Metabolic and vascular therapy is indicated: vitamins gr. B, pentoxifylline, nicotinic acid. To reduce swelling, antiallergic drugs (promethazine, chloropyramine, loratadine, desloratadine) are used. If signs of irritation of parasympathetic fibers predominate in the neuralgia clinic, anticholinergic drugs are prescribed: platiphylline, diphenyltropin, etc.
Intolerance to pharmacotherapeutic treatments is an indication for reflexology using acupuncture, magnetic puncture, and laser puncture methods. During the period of convalescence, DDT, amplipulse therapy, and electrophoresis with hyaluronidase are recommended.
Of fundamental importance in treatment is the elimination of the root cause of the disease: sanitation of the oral cavity, treatment of otolaryngological diseases and oral pathology, correction of endocrine disorders, therapy of chronic diseases of somatic organs. According to indications, surgical interventions are performed: removal of tumors and stones of the parotid gland, dissection of adhesions, sanitizing surgery on the middle ear, ethmoidotomy, maxillary sinusotomy, frontotomy, etc.
Treatment of the disease
Treatment of nasociliary nerve neurosis consists of eliminating the disease that affects it.
In case of inflammatory processes in the ENT organs, patients are prescribed a course of treatment with antibiotics and a set of drugs that affect the elimination of inflammation and restoration of the mucous membrane, or surgical intervention (for pathologies of the nasal septum).
For vascular diseases, patients are prescribed drugs with antihypertensive and nootropic effects. Treatment is also carried out using vasoactive drugs.
To relieve pain and other symptomatic and clinical manifestations of neuralgia, local anesthetic drugs are used in medical practice in combination with non-narcotic painkillers and vasodilators. Their use is determined by which part of the nasociliary nerve has undergone pathological effects:
- For neuralgia of the long ciliary nerve, dicaine (0.25% eye solution) mixed with adrenaline (4 drops per 10 ml of solution) is used.
- For neuralgia of the subtrochlear region of the nasociliary nerve, cocaine hydrochloride (2% solution) mixed with 0.1% adrenaline (4 drops per 5 ml of the drug) is used. A solution of lidocaine is also used in the form of a spray, which is injected into the nasal passages on the corresponding side or both at once (for bilateral neuralgia) up to 4 times a day.
- If any part of the nerve is damaged, use a powder mixture of papaverine, glucose, antispasmodic, diphenhydramine and aminazine 2 times a day.
As an additional therapy for patients diagnosed with Charlin's syndrome, a course of intramuscular vitamin B12 is indicated, as well as intravenous administration of sulfonamide drugs.
Unpleasant chest pain is often a sign of heart disease. But a similar symptom is also characteristic of neuralgia. A competent specialist should be able to distinguish the signs of neuralgia in the heart area from heart pain. Read the article about how to treat this disease.
We will consider the causes and symptoms of trigeminal neuralgia in this topic.
Ganglionitis of the sublingual ganglion.
It is characterized by sharp attacks of pain, which are localized in the area of the anterior two-thirds of the tongue. Pain occurs spontaneously or when eating, as well as when talking. Hyperesthesia of the corresponding half of the tongue often occurs, and often leads to loss of pain and taste sensitivity in this area.
An attack of acute pain in the submandibular region and tongue lasting from several minutes to an hour. Painful paroxysms are infrequent (1-2, less than 3 times a day). The pain radiates to different parts of the lower part of the face and, especially, to the tip of the tongue, as well as the sublingual area. They are provoked by eating spicy and rich food. There is no swelling of the soft tissues of the sublingual area.
Prevention
In principle, there are no specific measures aimed at preventing nasociliary neuralgia. It is enough to monitor your health, timely treat your ENT organs, and monitor the cleanliness and hygiene of your eyes. If any unpleasant symptoms begin to bother you, you should immediately consult a specialist.
Only a careful attitude towards your own health and regular visits to specialists can prevent the development of various diseases, including this one. Bringing it to an advanced stage will lead to complications and complicate the recovery process itself. It is also important to follow safety regulations at work. Foci of infection located in the facial area must be eliminated.