Types and classification
Depending on the time of development of inflammation, two types of neuralgia are distinguished:
- congenital;
- acquired.
Depending on the area of pain, a certain type of nerve damage is diagnosed:
- unilateral neuralgia;
- bilateral neuralgia.
The odontogenic variety is a dangerous pathology with persistent pain. The nature of the disease is persistent, with significant pain. The cause of damage to nerve endings is problems with periodontal and periodontal tissues, advanced stages of caries, chronic inflammation of the nasopharynx.
Note! Even when the underlying disease is cured, excruciating pain in the facial area continues for a long period.
Toothache with neuralgia: characteristic features
Toothache is not always a symptom of dental disease. It can occur in a person with completely healthy teeth and gums. In this case, you will have to visit a neurologist, since trigeminal neuralgia may be “masked” as toothache.
This condition is difficult to treat, however, it must be carried out without fail. Excruciating attacks of pain due to neuralgia can spread to the entire row of teeth and be repeated with high frequency.
How to distinguish toothache due to dental disease from pain caused by neuralgia, what treatment methods are used today and how effective they are, you will learn from the article.
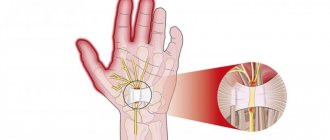
The trigeminal nerve is one of 12 pairs of cranial nerves. Anatomically, it is a continuation of the spinal cord. Its functions are to provide many reflexes, such as blinking, eyebrow movements, and sneezing. The trigeminal nerve, along with other nerves, is responsible for ensuring breathing. It consists of 3 branches:
- the first branch passes at eye level;
- the second - in the area of the nose above the upper jaw;
- the third - in the area of the lower jaw.
The location of the branches of the nerve determined their names: the first is called the orbital, the second is called the maxillary or zygomatic, and the third is called the mandibular. A symptom of nerve inflammation is pain, and its localization depends on which branch is affected.
So, with neuralgia of the second and third branches, a person experiences toothache. When the second branch becomes inflamed, the pain spreads to the nose, facial muscles and all upper teeth.
When the third branch is affected, a person feels pain in the neck, chin, cheeks, and the teeth of the lower row hurt.
Branches of the trigeminal nerve.
Depending on what caused the development of the pathology, neuralgia can be true or secondary. True (its second name is primary) is a self-limiting disease.
It occurs due to a pinched nerve or a change in blood supply. This can happen due to displacement of arteries and veins, the presence of adhesions and tumors.
Any injuries in the facial area can become a provoking factor for the development of neuralgia.
We advise you to read what advantages and disadvantages porcelain dental crowns have, and how much their installation costs.
Secondary neuralgia can be a complication of other diseases. Dental diseases that can lead to the development of inflammation of the trigeminal nerve include gingivitis, pulpitis, periodontitis, and periostitis. In addition, neuralgia can develop after tooth extraction.
A common cause of the development of secondary neuralgia is diseases of the ENT organs, for example, tonsillitis, inflammation of the sinuses. Pathology can develop when the body is severely hypothermic. Thus, people who do not wear hats in winter have a higher risk of developing neuralgia. The causes of secondary neuralgia also include metabolic disorders in the body, gout, and brucellosis.
Symptoms of neuralgia
Most often, the second and third branches of the facial nerve are affected, less often the orbital nerve. The main symptoms of neuralgia are pain in the teeth, radiating deep into the bones. The pain caused by inflammation of the nerve is strong, cutting, shooting.
https://www.youtube.com/watch?v=ORg3v-CmleI
It is paroxysmal in nature, and patients often compare it to an electric shock. The duration of the painful attack is several seconds, after which relief occurs.
In the future, attacks can be repeated several times, and the intervals between them can be short. This will create the impression that the attack lasts a long time.
Neuralgia pain is paroxysmal in nature.
Most patients with neuralgia go to the dentist because they are sure that the cause of the pain lies in the tooth. However, most often the patient is unable to determine which tooth hurts, since toothache with neuralgia spreads to the entire jaw.
Note: due to the connection between neurons, pain from the face can radiate to distant parts of the body, for example, “radiate” to the chest or arm.
Toothache due to neuralgia can be distinguished from pain associated with dental disease by the following signs of inflammation of the trigeminal nerve:
- with neuralgia, the pain is paroxysmal;
- without treatment, the frequency and duration of attacks, as well as the intensity of pain, does not change;
- outside of an attack, the oral mucosa and facial skin do not change externally, there is no swelling or redness.
Toothache with neuralgia covers the entire jaw.
The following symptoms have nothing to do with neuralgia:
- pain that is felt all the time in one tooth and spreads to the entire jaw: it indicates residual pulpitis, you need to see a dentist for x-rays and re-treatment of the canals;
- pain in one tooth, the appearance of which is accompanied by swelling of the gums: it indicates the development of inflammation; treatment of pulpitis or periodontitis may be required;
- aching pain in the area of a recently treated tooth, intensifying when you press on it: it may indicate a violation of the canal filling technology and removal of the filling material outside the tooth.
If you suspect that toothache is a symptom of neuralgia, you should immediately contact a neurologist to prescribe treatment. It is worth knowing that the treatment will be complex and complex. However, complete recovery cannot be guaranteed.
Damage to both the main (rare) and smaller branches of the trigeminal nerve can occur, of which the alveolar nerves are most often affected. Patients complain of constant pain, which periodically intensifies. Often complaints of a feeling of numbness in the teeth, gums, and facial skin.
When the lingual branch of the trigeminal nerve is involved in the process, these sensations occur in the anterior 2/3 of the corresponding half of the tongue; patients often bite their tongue. Simultaneously with the lingual branch, the buccal branch may be affected. The anterior palatine nerve rarely suffers (pain, burning sensation in half of the palate). Severe sensitivity disturbances in the area of the affected nerve (decrease in all types or loss) can only be detected at a certain stage of the disease.
The electrodiagnostic method determines the decrease in electrical excitability of teeth innervated by the affected nerve. When the alveolar nerves are involved in the process, the last sign is especially important. In patients with prolonged neuropathy, trophic disorders occur in the corresponding zone of innervation: desquamation of the epithelium of the mucous membrane, looseness and bleeding of the gums, etc.
When the 3rd branch of the trigeminal nerve is involved, if the process affects before the departure of the muscle branches, paresis of the masticatory muscles occurs, the lower jaw deviates in the direction of the lesion when opening the mouth. Atrophy of the masticatory muscles (especially the temporal and masticatory muscles) may occur. A common phenomenon of irritation is spasm of the masticatory muscles (trismus).
Types of nerve lesions in the tooth
The first thing to do (if the cause of the lesion is not known) is to undergo a full diagnosis and find out why this problem occurred. This will allow the doctor to choose the right treatment tactics.
It is very important to consult a doctor as soon as possible if you experience the first symptoms of complications after tooth extraction or implant installation. If treatment is started promptly, complete restoration of muscle functionality can be achieved. It is also important that if numbness persists for 3 months and no measures have been taken, it will most likely not be possible to restore the affected nerve, since persistent degenerative changes develop in it.
In the chronic course of the disease, discomfort may periodically arise and then subside again. In this case, the carious cavity can reach large sizes. Often the disease is asymptomatic, and the patient does not have any pain, so radiography is required to make an accurate diagnosis.
Symptoms
It is not difficult to recognize the disease: a pronounced form of pain significantly worsens the quality of life. The patient only thinks about how to prevent a new attack.
With trigeminal neuralgia, one or, more often, several signs of a pathological process appear:
- unbearable pain affects one or both sides of the face;
- attacks of acute, shooting pain last 1–2 or several seconds;
- the patient feels a strong lumbago, similar to an electric shock, in the left or right half of the face;
- painful attacks appear within one to two days or torment a person with a certain frequency for up to several months;
- stabbing/shooting pain occurs spontaneously or under the influence of certain irritants: brushing teeth, inhaling a stream of cold air, during an active conversation with expressive facial expressions;
- severe discomfort and pain affect areas controlled by the trigeminal nerve: gums, teeth, jaws, cheeks. Less commonly, lumbago is felt in the eyes and forehead area.
A serious illness has a characteristic symptom - short-term and paroxysmal pain. If you notice that a toothache appears for a few seconds, then disappears, or appears again under the influence of certain irritants, make an appointment with a dentist and neurologist as soon as possible.
Pain, neuralgia: dental diseases depending on gender
Some diseases are associated with age, race, or even gender. In medicine, childhood infections are distinguished separately: chickenpox, scarlet fever, etc. The so-called periodic disease can be registered in the original inhabitants of the Mediterranean basin, also called the Armenian disease. Some diseases are gender-linked. In dentistry, one can also trace a gender predilection for certain diseases: while men most often come with toothache and injuries to the maxillofacial area, women come with complaints of inflammation of the gums, neuralgia of the trigeminal nerve or its branches.
MedAboutMe found out which oral diseases are more likely to threaten men and which women?
Complaints of toothache due to caries complications
Toothache can appear in several cases: with complications of caries - pulpitis, periodontitis, or with deep caries, but under the influence of irritants. The appearance of pain is always a reason to contact a specialist and undergo treatment.
If we consider the percentage of patients, then most often it is men who come with caries complications. As a rule, women are more responsible about their health, observe oral hygiene more carefully and visit the dentist several times more often for preventive examinations.
These simple manipulations make it possible to treat caries before it turns into complications, therefore, before severe pain appears. The overwhelming majority of men ignore preventive visits and go to the appointment only when absolutely necessary, when the symptoms that appear leave no choice and the person develops severe toothache. Perhaps this is precisely what can explain the higher percentage of patients among men with secondary edentia - lack of teeth.
Complaints of toothache due to hypersensitivity
Increased sensitivity of teeth is manifested by sharp acute pain when exposed to temperature, less often - chemical irritants. Sharp pain from a cold is familiar to many, but most often it is women who suffer from this illness.
Why does hyperesthesia occur? Often the cause is hidden in areas of thin enamel, its absence or underdevelopment, in other words - non-carious lesions of the teeth. Scientific research has proven that hormonal and metabolic disorders play a leading role in their formation. A reduced concentration of estrogen is one of the causes of erosion, wedge-shaped defect, increased abrasion of enamel, with the subsequent formation of hypersensitivity symptoms.
Women with such diagnoses are at risk for the formation of osteoporosis, and hyperesthesia will be a signal of existing and increasing dysfunction - osteopenia (decreased bone mass).
Men also experience all the unpleasant symptoms, but most of them are associated with other causes - degenerative changes in the alveolar process of the jaw or progressive inflammation of the gums.
Complaints about gum inflammation
Gum inflammation is one of the most common complaints among patients, regardless of age. If we track the statistics of complaints among men and women, then it is necessary to make a reservation. Among women, complaints of gingivitis predominate; among patients diagnosed with periodontitis, the majority are men.
Gingivitis is an inflammation of the gums in which the integrity of the periodontal junction is not compromised. For a better understanding, we are talking about “superficial” inflammation, the symptoms of which can be: swelling, redness of the gums, bleeding when brushing teeth or eating rough food, bad breath. Inflammation of the gums can accompany many somatic pathologies or be a “symptom” of physiological conditions, for example, gingivitis during pregnancy.
Due to hormonal imbalances during pregnancy or menopause, a special type of gum inflammation is formed, which is characterized by: bleeding when brushing teeth, swelling, and growth of mucous membrane, which in complex forms of the gums can cover up to a third of the tooth crown. Treatment of this type of inflammation is exclusively symptomatic.
Periodontitis is an inflammation of the gums, in which the ligamentous apparatus of the tooth is destroyed and the bone plate is lost. Periodontitis is a complicated form of gingivitis. If measures are not taken promptly and gingivitis is not treated, it develops into complications, the ligaments of the tooth are gradually destroyed, gums recede, tooth mobility may develop, and in severe cases, tooth loss. It is precisely because of the reluctance to seek help from specialists in a timely manner, the presence of bad habits, and chronic diseases that men more often suffer from this disease.
Periodontal disease is a systemic destructive disease characterized by degenerative changes in the bone tissue of the alveolar process of the jaw, significant receding gums, exposure of tooth roots, but no inflammation. The main cause of periodontal disease lies in the disruption of trophism (nutrition) of periodontal tissues that surround the tooth and hold it in place, due to sclerosis of blood vessels. Due to a lack of nutrients, bone tissue atrophy and gum recession (loss) begin. Diseases of the heart, blood vessels, and nervous system can be called a provoking factor in the development of periodontal disease.
Trigeminal neuralgia
Neuralgia is a syndrome characterized by sudden, short-term, intense pain in the area of innervation of a certain nerve. For dentists, it is the trigeminal nerve that is of interest. Due to the fact that its branches have a large area of innervation - almost the entire face - it is not possible to determine the exact localization of pain. The pain from neuralgia is so severe that it forces you to quit everything you do.
According to statistics, middle-aged women suffer more often from neuralgia. And it is not yet possible to say for what reason. Moreover, there is no exact data yet on why neuralgia appears at all. There are several theories:
- According to one version, neuralgia appears due to compression of the trigeminal nerve or its branches by a blood or lymphatic vessel, an aneurysm. Such irritation causes sharp paroxysmal and severe pain. In some cases, it is extremely difficult for doctors to calculate the location of this compression, which complicates the treatment process.
- Another theory states that the destruction of the myelin sheath of the nerve due to the aging process of the body (most often middle-aged and elderly people suffer), as well as various diseases contribute to the destruction of this sheath. These include, for example, infections, demyelinating pathologies, and autoimmune diseases.
- Tumor processes.
- Neuralgia of unknown etiology.
Men also suffer from neuralgia, but much less frequently, and in their case the pain is more often associated with tumor processes, including the oral cavity. Indeed, according to static data, oncological processes are registered several times more often in men.
Even with a predisposition, the development of most dental pathologies can be prevented. It is enough to visit a specialist in a timely manner for preventive examinations, cavity sanitation, perform all hygienic procedures and adhere to the principles of proper nutrition.
Causes of trigeminal neuralgia: symptoms and treatment, useful advice from experts
Trigeminal neuralgia is a serious disease with painful symptoms. Pain in the jaw or cheek area is often so severe that a person’s life turns into a constant struggle with dangerous symptoms.
Inflammation of the trigeminal nerve is difficult to treat and forces you to give up many usual activities. Attacks paralyze the will, forcing one to seek salvation in any, even unconventional methods, potent drugs that can alleviate suffering.
The patient experiences unbearable pain when the trigeminal nerve is compressed by a vascular loop, veins/arteries of the posterior cranial fossa. Some patients with trigeminal neuralgia have excessive pressure in the bone canals at the base of the skull, where part of the nerve is located.
Main reasons:
- congenital pathologies;
- inflammatory diseases of a chronic nature in nearby areas. Most often - sinusitis, deep caries, sinusitis.
Causes of neuralgia
In medicine, there is no exact reason why certain parts of the trigeminal nerve become inflamed, causing pain in the head. But doctors identify several possible pathology factors:
- stress;
- chronic infections and inflammatory processes;
- hypothermia of the head;
- a sharp decrease in immunity;
- excessive emotional and physical stress;
- caries;
- poor nutrition.
The situation is aggravated by chronic diseases, including cancer, multiple sclerosis and metabolic failure. Stem strokes, anomalies in the development of blood channels, atherosclerosis and aneurysms affect the health of the nerve. Often, neuralgia of the head is caused by injuries to the skull and face.
Inflammation of the occipital nerve, the symptoms and treatment of which are described in this article, has its own triggers.
Elena 2 years ago
Development of the disease
Trigeminal neuralgia has a characteristic clinical picture:
- The main category of patients is over 50 years old. Sometimes dangerous symptoms develop in people aged 30–35 years, less often - after 25 years;
- Many patients in the neurological and dental departments have a history of the following problems: hypothermia of the face, sinusitis, sinusitis, dental diseases;
- neuralgia does not occur without a reason. Tooth decay due to caries, untreated pulpitis, advanced forms of nasopharyngeal diseases can lead to inflammation of the trigeminal nerve with all the ensuing consequences;
- the first signs of neuralgia appear in the area of a dilapidated unit of the dentition or in the gum area. Often, the dentist removes a healthy tooth, mistakenly believing that it is this problematic unit that provokes painful attacks;
- gradually the pain spreads to new areas. Painful attacks occur with any action in the facial area: talking, sneezing, coughing, facial movements;
- hygiene procedures turn into torture, a person is afraid to wash his face, open his mouth too much, or shave. The patient prepares only liquid meals for himself, often expressing himself in writing in order to minimize the work of facial muscles;
- During attacks, pain literally paralyzes the face. The person is afraid to move, sometimes pressing on his temple or cheek, trying to relieve the pain with an antagonistic gesture;
- often stunning pain is accompanied by lacrimation, mucous secretion from the nasal passages, and redness of the facial skin;
- a painful tic is accompanied by a spasm of the facial muscles. The area of the cheek or eye “freezes,” or the problem spreads over a large area.
Diagnosis and differential diagnosis
Since the key diagnostic sign is headache, often unilateral, the main differential diagnosis is migraine, with which occipital neuralgia is sometimes confused. Indeed, in some cases the symptoms are similar: for example, photophobia and pain in half of the head.
But, with careful questioning, you can find the key to understanding. For example:
- With migraines, the pain is often throbbing, the patient feels the passage of blood flow, and the orbit “aches.” With neuralgia, the pain is fast, lightning fast, coming and going suddenly;
- With migraines, a condition called aura often develops first. This may be dizziness, an attack of “fly spots” flashing before the eyes and other signs. With neuralgia there is no aura;
- As a rule, bright light does not provoke a migraine attack, but only becomes unbearable during pain, this is also accompanied by intolerance to loud noise;
- Migraine can be accompanied by nausea, and at the height of the headache, single (or less often, repeated vomiting) occurs, while occipital neuralgia (like any other) is not accompanied by nausea, much less vomiting.
- Migraine has a characteristic symptom - patients try to squeeze their temples tighter, or clasp their head with their hands, tie it, this brings relief during an attack. With neuralgia, on the contrary, every touch can cause pain;
- The cause of a migraine attack can be long-term use of hormonal contraceptives, foods containing tyramine - cheese, as well as nuts, chocolate and red wine, as well as abuse of headache medications (with the development of the so-called abuse headache).
Of course, trial treatment also gives an answer to the question of what is the cause of the headache: if it is neuralgia, then it will be persistent and cannot be treated with triptans, with ergotamine drugs (ergot alkaloids) and with vasoconstrictor drugs.
Migraines can go away simply by normalizing your diet, work and rest, and giving up medications and unhealthy foods. Only refusal of medications must be agreed with your doctor, since refusal to take some medications can lead to serious complications.
Routine diagnosis of occipital neuralgia, as a rule, gives little results. Its main task is to confirm the functional nature of pain and search for destructive processes in the cervical spine, as well as space-occupying formations. The following methods are used for this:
- Competent and attentive questioning, and a detailed neurological examination. This is also a set of methods, and one of the best. Unfortunately, fewer and fewer specialists are able to do this, replacing clinical thinking with instrumental methods;
- CT scan. The advantage of this method is its speed, but the assessment of the condition of soft tissue and cartilaginous formations is not good enough. Radiation exposure during computed x-ray tomography is insignificant.
- Magnetic resonance imaging. The most informative way to diagnose the condition of cartilage tissue, muscles, the central nervous system and organs of the neck. In order to obtain an informative tomogram, the magnetic field strength of the tomograph must be at least 1.5 - 2 Tesla. This should be enough to confidently distinguish formations whose size is about 1 mm.
Contraindications to MRI are claustrophobia (fear of closed spaces), since the examination time is about 30 – 40 minutes. In addition, this procedure cannot be performed on patients with metal implants in the body that consist of magnetic materials (ferroalloys). Patients with pacemakers (heart pacemaker) are also prohibited from undergoing MRI for health reasons, due to the risk of developing fatal arrhythmias.
One of the “exotic” contraindications to MRI is the presence of tattoos on the body containing metallic dyes. Under the influence of a magnetic field, these paints begin to move and, when heated, cause burning pain.
- The standard screening method, low cost, and safe when proper precautions are taken, is the classical radiological method. In this case, radiography is performed in direct and lateral projections, with functional tests.
Teeth hurt with sinusitis: why and what to do?
With sinusitis, teeth hurt when fluid collects in the maxillary sinuses and pus forms. The pathological process is accompanied by an increase in temperature, the appearance of a disgusting odor, and an excruciating headache occurs that radiates to the ear or jaw, reaching the temple or forehead.
Sinusitis occurs after rhinitis, colds, flu, scarlet fever. They are preceded by untreated infections and decreased immunity. The sinuses become inflamed when viruses and bacteria travel into the airways.
Sinusitis sometimes develops due to damage to the nasal septum, which happens after an injury. Not everyone knows whether damaged teeth can contribute to the development of inflammation in the sinuses. Caries provokes the emergence of a pathology from which both adults and children suffer.
The accumulated fluid puts pressure on the upper jaw, which is the reason why teeth hurt with sinusitis. The unpleasant feeling is more pronounced when a person chews food.
With prolonged inflammation of the mucous membrane, bone tissue is affected, the abnormal process affects the jaw, which is located above the cavity.
Therefore, toothache with sinusitis is often present, it is dull when the trigeminal nerve is damaged, and it is acute and painful in the odontogenic form of pathology, which occurs when the upper molars are destroyed by caries.
An abnormal process occurring in the area of the paranasal sinuses is often detected during a visit to the dentist. People turn to him when their teeth hurt due to sinusitis.
Pathology in the maxillary cavity is usually not accompanied by obvious symptoms. A person may not have a headache or a stuffy nose when pus enters the mouth through a fistula. Provoke the development of odontogenic sinusitis:
- abscesses;
- granulomas on the roots of the units;
- molar periostitis;
- cyst growth.
The maxillary cavity becomes inflamed when particles of the material used for filling are directed into the sinus. Sinusitis occurs when a painful tooth is removed, when a fistula appears in the hole. It accumulates pus, which ends up in the paranasal sinus.
With sinusitis, which develops when molars are damaged, the following symptoms are observed:
- Headache.
- There is a disgusting smell.
- Fever and chills are present.
- Tormented by body aches.
- The temperature is rising.
- Food enters the sinus.
Due to severe nasal congestion, the sense of smell disappears. If the source of inflammation is in the sinus or near the root, the teeth continue to hurt during remission. An unpleasant phenomenon is observed with ascending sinusitis, when the oral cavity is first affected, and the mucous membrane of the paranasal sinuses immediately becomes inflamed with a descending type of pathology. If, after applying a filling during the treatment of caries, the material was not removed:
- purulent discharge is formed;
- pain occurs when chewing food;
- loss of appetite.
In addition to chronic sinusitis, the presence of a foreign body can trigger the formation of a cyst. In rare cases, the bones of the skull become inflamed. Particles of the filling are removed through a puncture made in the gum using an endoscope.
Diagnostics
If tooth pain is tormented by sinusitis, in addition to an otolaryngologist, you will need the help of a dentist who will know what to do after an instrumental examination. Treatment is prescribed based on the following data:
- x-ray of the oral cavity;
- magnetic resonance and computed tomography;
- diaphanoscopy;
- sinus punctures.
The presence of sinusitis is determined without problems. It is much more difficult to identify that its cause was damage to the upper molars.
In case of inflammation of the paranasal sinuses, treatment is aimed at eliminating symptoms, sanitizing teeth and preventing pathology. Therapy for sinusitis is carried out using antibiotics in the form of injections and tablets. Nestoroids Diclofenac, Ibuprofen, Naklofen, Aspirin are prescribed to relieve inflammation.
With odontogenic sinusitis, it is often necessary to remove the affected tooth and close the fistula. After this, conservative treatment begins, which includes:
- sinus rinsing;
- use of anti-inflammatory drugs;
- physiotherapeutic procedures.
At home, a herbal decoction or medicinal solution is poured into a teapot or syringe. A tip is inserted into one nostril and liquid is applied under pressure so that it flows out of the other.
In a clinic or hospital, having identified why teeth hurt, the patient is given a remedy that dilates blood vessels. The doctor then uses a special suction to create negative pressure in the nasal cavity and speed up the circulation of the saline solution, which is injected into the other nostril.
A Yanik sinus catheter is used to rinse the maxillary sinus in babies and expectant mothers. Before the procedure, an injection of Novocaine or Lidocaine is given. The posterior balloon is inserted into the nasopharynx, the anterior balloon into the nasal cavity. After inflating it with a syringe, the air is sucked out, causing the pus to come out.
You can eliminate toothache due to sinusitis with vasodilating drops, taking mucolytics, which thin the mucus. Analgesics and physiotherapeutic procedures in the form of darsonvalization and electrophoresis alleviate a person’s condition with sinusitis caused by damage to the trigeminal nerve.
It is not always possible to get rid of inflammation in the paranasal sinuses by washing, using antibiotics, or warming procedures. In case of purulent sinusitis, surgical intervention is used:
- in the absence of a positive result for 5 days;
- at high temperature;
- severe headache;
- with swelling of the connecting canal.
The procedure is carried out after anesthesia. The wall of the sinus is pierced with a thick needle. An antiseptic is injected with a syringe and the pus is removed.
To prevent inflammation from starting, bacteria are not activated, antibiotics are infused.
After a sinus puncture, the person’s condition improves and the pain goes away. Treatment is continued with physiotherapeutic procedures and rinsing the nasal cavity with antiseptics.
Odontogenic sinusitis is dangerous because it can lead to sinus damage. Residues of food will begin to enter the maxillary cavity, bacteria will quickly multiply, which will provoke complications in the form of:
- meningitis;
- blood poisoning;
- inflammation of the orbit;
- abscess formation.
The main methods of preventing odontogenic sinusitis include constant oral care and rinsing with special solutions. If you identify a diseased tooth, you should not delay your visit to the dental clinic. People who have strong immunity suffer less from sinusitis.
(55.00 out of 5)
With sinusitis, the cheek, temple, and forehead may hurt. One of the symptoms may be toothache. It can manifest itself in different ways: it occurs during chewing, the doctor can identify it by palpation.
Sometimes there is discomfort, a feeling as if the teeth of the upper jaw have lengthened.
In some cases, the pain is neuralgic in nature (the so-called shooting pain, which radiates to the upper jaw, ear, temple).
Inflammation of the maxillary sinus is accompanied by various ailments. There may be a headache, a rise in body temperature, and a stuffy nose. But these signs are characteristic of all sinusitis. But with sinusitis, the teeth of the upper jaw often hurt. There are many reasons for this phenomenon:
- The accumulated exudate presses on the walls of the sinus. Since it is located above the upper jaw, discomfort and pain occur in the area of the upper teeth. The pain intensifies when chewing, tapping on the molars (the doctor thus identifies why the patient has a headache and a stuffy nose).
- The inflammatory process affected the trigeminal nerve. Therefore, neurological type pain (shooting) occurs, which can radiate to the teeth and ear.
- Due to a long-term, chronic illness, not only the mucous membrane became inflamed, but pathological processes began in the bone tissue (osteomyelitis). Since the maxillary sinus in adults is located directly above the upper jaw, it is also affected.
- Sinusitis is caused by diseases of the upper molars.
Teeth pain with sinusitis can occur in different ways. If the pain is dull and intensifies with chewing, then most likely it is associated with toxic damage to the trigeminal nerve. Sharp and strong - indicates that the patient has an acute form of odontogenic disease.
Inflammation of the maxillary sinus, resulting from disease of the upper molars, is very common in adults. It is usually detected by dentists, since sinusitis causes teeth pain.
The most common causes of odontogenic inflammation:
- Foreign bodies. Filling material, fallen tooth roots, parts of broken dental instruments, and turundas can get into the sinus from the oral cavity.
- Granulomas at the root of the tooth or abscess. These pathological processes contribute to the penetration of pus and the occurrence of the disease.
- Periostitis of a molar tooth. In the area of the molars, the bone wall is very thin, a hole (fistula) appears there very quickly and through it air and even food particles can enter the sinus.
Identifying the odontogenic form of the disease is not easy. Often it is practically asymptomatic. The patient does not have a headache or a stuffy nose, since the pus flows through the fistula into the oral cavity.
Accordingly, there is no pressing and bursting feeling in the sinus area, because the appearance of this sign of the disease is facilitated by the accumulation of exudate in the cavity. Often, inflammation of the maxillary sinus is detected after the removal of a diseased tooth.
In this case, a fistula remains in the hole leading into the sinus. Because of this, pus accumulates in it and inflammation occurs.
The pressure of the choleastomy promotes the resorption of the bone walls, therefore, following the maxillary sinus, the ethmoid labyrinth is affected and tissue necrosis occurs.
This process occurs latently (there are no typical symptoms), and the disease can only be detected because the patient is bothered by toothache, which is not so easy to relieve.
Most often, with inflammation caused by molar disease, patients complain of:
- for mild pain in the forehead;
- discharge of pus in the alveolar process;
- when blowing your nose, air enters the oral cavity;
- small pieces of food enter the sinus;
- There is a putrid odor coming from the mouth.
How to relieve pain before visiting a doctor?
Toothache is difficult to endure, it becomes intrusive and does not allow a person to lead a normal lifestyle. Pain can be relieved with the help of analgesics. Analgin, Paracetomol, Baralgin, etc. can be used as painkillers. However, their effect will be weak. The best way to treat toothache is with drugs containing ketorolac trometamol or ibuprofen (Nurofen, Ketorol, etc.) as the active substance.
It is necessary to monitor the condition of the oral cavity. If symptoms of inflammation of the dental nerve appear, you need to brush your teeth and rinse your mouth thoroughly with water or mouthwash, since food particles stuck in the interdental spaces can cause similar unpleasant sensations. If your teeth hurt, rinsing with herbal decoctions (sage, chamomile, etc.) or a soda solution will help. Rinsing should be done every 2-3 hours.
Normally, a person's sensory supply is always observed in the area of the front of the face. It is carried out thanks to fibers passing through this area related to the trigeminal nerve. It is responsible for how we react to problems in the oral cavity. And if neuralgia of the teeth appears, then it hurts us very much.
Diagram of the innervation pathways of the trigeminal nerve in the jaw area
Let's understand the differences:
- Untreated caries can cause a condition such as neuralgia, toothache in this case will be vague. It can be of different localization and radiates more outside the face than inside the structures that hold the mineral formation.
- Toothache with neuralgia is provoked by everything that happens to you, from cold food to wind in the face.
- Neuralgia of the teeth has a similar nature of response to irritation, but of a more acute piercing nature. Letting you go for a while, the pain appears again.
- Colds, sinusitis.
- Tooth decay causing bacteria to penetrate to the root apex. The result is the onset of inflammation.
Soft tissues increase in volume and put pressure on the passing branches of the sensory system. Prolonged irritation leads to the fact that for such a symptom as dental neuralgia, treatment must begin in an acute manner. Because it is very difficult to tolerate irritation in this special nerve with complex response pathways.
Rules and methods of treatment
It is not easy to alleviate suffering and rid the patient of dangerous symptoms. Some patients suffer from trigeminal neuralgia for many years. Therapy does not always bear fruit; treatment is long-term and sometimes ineffective. Even after filling all the carious cavities and eliminating nasopharyngeal problems, pain does not leave the facial area for a long time.
Dentalogy {amp}gt; Treatment{amp}gt; Oral diseases {amp}gt; Trigeminal neuralgia: causes, symptoms and methods of treating the disease
Trigeminal neuralgia is characterized by severe pain in the jaw or lower face.
Sometimes the pain that this disease causes is compared to an electric shock.
Such symptoms occur when the trigeminal nerve is irritated, the fibers of which are connected to the nerve endings of the cheeks, forehead and jaw.
This disease is typical for adults, more often for women who have already crossed the 40-year mark.
Trigeminal nerve irritation occurs when arteries come into contact with veins at the base of the skull. At the same time, the nerve is compressed, which provokes painful attacks.
The causes of trigeminal neuralgia may be as follows:
- Disturbance in the location of cerebral vessels.
- Infectious diseases. Herpes viruses, and especially herpes zoster, very often lead to the development of neuralgia. But other viral infections can also lead to these disorders.
- Deterioration of blood circulation in the vessels of the brain.
- Hypothermia of the face.
- Severe stress, which contributes to decreased immunity.
- Multiple sclerosis.
- Brain tumors.
Do your gums hurt due to wisdom teeth erupting? Find out how to cope with pain in this article.
How to strengthen loose teeth? Useful recommendations, dental gymnastics.
Sharp intense pain is the main symptom of trigeminal neuralgia. The pain usually occurs on one side of the face, it can be almost unbearable, shooting, comparable only to an electric discharge.
Attacks can last from a few seconds to 2-3 minutes. Sometimes attacks are accompanied by increased salivation and uncontrollable lacrimation. Throughout the course of the disease, the pain does not change its location.
An attack always occurs under certain conditions, more often when some area of the face is irritated. Patients noticed the following factors causing another attack of neuralgia:
- washing, brushing teeth, shaving;
- touching the face;
- blow to the nose;
- applying makeup;
- a breath of wind;
- yawn;
- talk;
- smile;
- chewing food.
When a person is calm, such as during sleep, attacks never occur. Other symptoms of neuralgia may include:
- Facial spasms or distortion. During an acute attack, the patient may experience contraction of the facial muscles. Facial expressions are distorted, muscles twitch. If the attacks are very severe, the person begins to behave in a certain way during them - he moves less, remains silent, trying to minimize the pain.
- Headache.
- A mild increase in body temperature that causes chills, weakness, and muscle or joint pain.
- Constant irritability and fatigue, which are associated with frequent painful attacks.
- In rare cases, a rash on the face.
Since patients with neuralgia often experience pain when chewing food, they try to chew only on one side of the mouth. This leads to the appearance of muscle thickening on the other side. Over time, this threatens dystrophy of the masticatory muscles, as well as a decrease in the sensitivity of the side of the face that is susceptible to the disease.
The trigeminal nerve has several branches, each of which can cause different symptoms of neuralgia.
- The first branch – pain occurs in the eye area, it can radiate to the temple, forehead or bridge of the nose.
- The second branch – pain is localized in the area of the upper lip or teeth. Pain can move to the temporal region and back. Sometimes such neuralgia is confused with toothache.
- Third branch - pain occurs near the chin, spreading to the ear or lower jaw.
Neuralgia pain can be typical or atypical. In the first case, pain occurs in attacks that are provoked by certain conditions. Between attacks the person feels normal.
In the second case, the person experiences pain constantly, and it can occur in different parts of the face. This type of neuralgia is much more difficult to cure than the first.
Trigeminal neuralgia is characterized by a certain cyclicity. Some people experience attacks almost every hour, while others may have them as often as a few times a week.
Neuralgia can be confused with a disease such as temporal tendonitis, so it is imperative to consult a doctor at the slightest suspicion of this disease.
It is extremely difficult to cure this disease and even radical treatment methods do not always give a positive result.
But proper therapy can relieve pain and significantly alleviate human suffering.
The following treatment is usually prescribed:
- Antiviral drugs - herpevir, acyclovir, lavomax. They are used if the cause of neuralgia is an infectious disease.
- Anti-inflammatory drugs that do not contain steroids - indomethacin, Celebrex, Revmoxib, Dicloberl, Celebrex.
- Painkillers – dexalgin, ketanov, ketalgin. If the pain is very severe, they may prescribe narcotic drugs - morphine, promedol, tramadol or nalbuphine.
- Antispasmodics – sirdalud, mydocalm, etc.
- Glucocorticoids – dexamethasone, methylprednisolone, hydrocortisone. These drugs reduce swelling of the nerve and also relieve inflammation.
- Neuroprotectors and vitamins - neurobion, milgama, proserin, neurorubin and others.
- Local remedies - lidocaine or anesthetic ointment.
Physiotherapeutic procedures also have a beneficial effect. For this disease, electrophoresis, magnetic therapy, ionogalvanization, ultraphonophoresis, transcutaneous electrical stimulation, paraffin-ozokerite, diadynamic therapy, UHF, etc. are often prescribed.
Drug therapy does not always help cope with the disease. Sometimes doctors have to resort to surgery. There are the following types of operations:
- Percutaneous surgery. Used in the early stages of the disease. Under local anesthesia, the trigeminal nerve is destroyed by exposing it to chemicals or radio waves.
- Nerve decompression. This operation is aimed at correcting the location of the arteries that compress the trigeminal nerve.
- Radiofrequency destruction of the nerve root. In this operation, only a certain part of the nerve is destroyed.
The type of operation is prescribed depending on the individual characteristics of the patient’s disease.
Do your gums hurt and bleed? Find out how to get rid of this unpleasant phenomenon at home.
Why do teeth crumble? Causes of tooth decay in adults and children.
Some folk recipes can reduce pain from neuralgia, relieve inflammation and swelling. The most popular means are:
- Mint tincture. Take 200 g of mint and 100 g of St. John's wort and valerian. These herbs are mixed, a liter of water is poured on top and put on fire. After the water has boiled, the herbs are boiled for 15 minutes, then the broth is filtered and infused in a dark place for about 5 hours. You need to take this tincture one spoonful three times a day. A similar tincture can be prepared from burdock and chamomile.
- Aloe juice. The juice of an adult plant, which should be taken a teaspoon 3 times a day, preferably before meals, effectively helps against neuralgia.
- Black radish juice. By mixing it with a small amount of lavender oil, you need to rub it into sore spots, thereby reducing the number of attacks and reducing pain.
- Birch juice. By taking it orally or lubricating it on the side of the face affected by neuralgia, you can reduce the symptoms of the disease. You need to drink 4-5 glasses of this juice per day.
- Geranium compresses. Take fresh leaves of this plant, place it on a cloth or napkin, and then fasten it to the diseased area. Periodically you need to replace geranium leaves with fresh ones.
- Marshmallow root. Several roots of this plant are crushed and brewed with boiling water. The decoction should sit for about a day, after which a cloth is soaked in it and applied to the affected areas for 1 hour.
It is recommended to use any of the above methods only with the approval of your doctor.
Preventing trigeminal neuralgia is much easier than curing it.
It is necessary to treat all kinds of infectious diseases in a timely manner, monitor the condition of the teeth, avoid hypothermia of the body, and especially the face, as well as eat properly and avoid injury to the nose or jaw, which often causes the disease.
Main methods of treatment
Treatment of occipital neuralgia consists of etiological and symptomatic therapy. Etiological treatment is aimed at eliminating the very cause of the disease.
If the cause of the pain is accurately determined, appropriate therapy is prescribed. For example, if the cause of pain is the herpes virus, drugs with Acyclovir are used.
The table below describes the principles of symptomatic treatment. They are the same, regardless of the cause and etiology of the disease.
| principles of treatment for occipital neuralgia | ||||
| Drug group name | Drug name | Operating principles | Features of application | Contraindications |
| Non-steroidal drugs against inflammation | Diclofenac; Ibuprofen; Indomethacin; Analgin; Ketorolac; Paracetamol. | They are able to reduce the inflammatory process. They also have an antipyretic and analgesic effect. | These drugs can be taken strictly after a heavy meal, as they can contribute to the development of gastritis and peptic ulcers. These drugs can be used as a general therapy, or applied topically in the form of ointments, creams and gels. | gastritis; peptic ulcer; pregnancy; lactation; acute and chronic renal failure. |
| Diuretics | Lasix; Furosemide; Torsemide. | Reduce swelling at the site of the inflamed nerve. Thereby relieving the pain a little. | These drugs can be used in the treatment of neuritis only after consultation with a doctor. If taken uncontrolled, it can cause acute disturbances in water and electrolyte balance. | acute renal failure in the stage of oligoanuria; liver failure; dehydration; decreased blood pressure. |
| B vitamins | These vitamins are commercially available in their pure form, or in special vitamin complexes, for example, Neurovitan, Magnesium B6 | Vitamins of this group have a protective effect on the central and peripheral nervous system and promote nerve restoration. | You can take them after a doctor's prescription. If they are taken orally, they should only be taken after meals. | pregnancy; lactation; allergy; erythremia; glomerulonephritis; oncological diseases. |