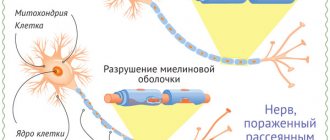
The figure (below) shows the process of transmission of nerve excitation along intact and damaged nerve fibers.
Most often, multiple sclerosis begins between the ages of 20 and 40. After the first attack of symptoms, partial or complete remission (weakening or disappearance of disease symptoms) may occur. Further attacks eventually lead to progressive disability.
Although the exact cause of MS is still unknown, doctors believe it is an autoimmune disease in which the immune system attacks the myelin sheath of its own nerve cells. Genetics plays a certain role in this disease—the risk of developing MS is higher among relatives of a sick person compared to the general population. In addition, the farther a geographic region is from the equator, the higher the incidence of MS. The incidence is also higher in those countries where they eat more meat and animal fats and less unsaturated fats and fish.
There is no effective conventional treatment for multiple sclerosis yet, but several new drugs, including two forms of interferon (AVONEX and Betaseron) and another drug, glatiromer acetate (Copaxone), may reduce the rate of relapses (exacerbations) in people with certain forms of the disease and slow the rate its progression. Other drugs reduce the severity of exacerbations or are aimed at treating specific symptoms. For example, muscle spasticity.
LINOLEIC ACID
Linoleic acid (omega 6) is found in high concentrations in sunflower and safflower oils and in lower concentrations in most other vegetable oils. Three groups of scientists performed double-blind studies to determine the effectiveness of linoleic acid (in the form of sunflower oil) in MS. Participants in the experiments received from 17 to 20 grams of linoleic acid per day, which is equivalent to approximately 30 ml of sunflower oil. The results of these 3 studies were mixed.
Two of these studies (using 75 people in one study and 116 people in the other) found that those who took linoleic acid had shorter and less severe flare-ups compared to those who took a placebo in the form of olive oil. However, 2-year studies have shown that taking linoleic acid does not significantly affect the frequency of exacerbations and the overall level of disability.
A third study of 76 people lasting 2.5 years found that linoleic acid had no effect on either the frequency of exacerbations or the degree of disability compared with the group taking olive oil.
Another researcher suggests that the studies conducted were not long enough for linoleic acid to show a significant positive effect on the myelin sheath.
Another research scientist, after carefully studying the results of the experiments, concluded that linoleic acid may be effective in people with less severe symptoms of the disease. But this statement needs proof.
OTHER ESSENTIAL FATTY ACIDS
Blood tests of people with MS have found lower levels of omega 3 fatty acids in body fluids and tissues compared to levels in healthy people. This suggests (but has not been proven) that supplementing with omega 3 may help. Unfortunately, in a 2-year, double-blind study of 292 patients with multiple sclerosis, there was no significant difference between the use of omega-3 fish oil and olive oil (placebo).
Additionally, some researchers believe that gamma-linolenic acid may be beneficial for MS. But evidence of this effectiveness has not yet been obtained. Moreover, more negative results were obtained than positive ones.
THREONINE
There is evidence that the amino acid threonine could reduce muscle spasticity, which is often seen in multiple sclerosis.
Two small, randomized, blinded studies showed a modest but statistically significant reduction in spasticity in people taking threonine compared with those taking placebo. In one study, after 8 weeks of treatment of 26 patients, improvement was noted by doctors, but not by the patients themselves. In the second study, both doctors and some of the 33 participants reported a decrease in cramping and pain. Interestingly, more pronounced improvements were noted when using lower doses of threonine - 6 grams per day (compared to a daily dose of 7.5 grams per day). No side effects of threonine treatment were found in any study.
Symptoms of Multiple Sclerosis
The manifestations of multiple sclerosis are very diverse, since the disease affects the entire nervous system. The lesions turn out to be scattered in different parts; instead of nervous tissue, connective tissue is formed in these places, and the function that this area performed is lost, therefore all clinical manifestations are systematized according to the location of the lesion in the nervous system.
There are typical signs of multiple sclerosis and atypical, rare ones, which, however, should not be forgotten. Usually, one patient simultaneously exhibits signs of damage to different functional systems (due to the dispersion of the damage).
Typical manifestations
They represent a display of damage to the pathways of the nervous system. These are the so-called “classic” symptoms of multiple sclerosis.
Motor sphere
This group of symptoms includes damage to the pyramidal tracts, which occurs in 85-97% of cases, i.e. observed in almost every patient. It can be:
- paresis or paralysis - decreased muscle strength in the limbs. The lower extremities are most often affected. As the disease progresses, paresis can spread until all four limbs are affected;
- increased tendon reflexes (tested with a neurological hammer from the arms and legs) and reduction and loss of superficial ones (the latter is especially characteristic of abdominal reflexes);
- pathological symptoms - Babinsky, Gordon, Bekhterev, Zhukovsky and others. They are always checked by a neurologist during a routine neurological examination;
- increased muscle tone, so-called muscle spasticity. At rest, muscles become tense and hard to the touch. This symptom, along with muscle weakness, can make it difficult for patients to move (if it occurs in the legs) or prevent them from performing normal household self-care techniques (if it occurs in the arms);
- the appearance of clonus of the foot, hand and kneecaps. This is an extreme degree of increased reflexes. Clonus are rhythmic movements of the foot, hand, or kneecap. Caused by stretching of muscles or tendons. For example, foot clonus is caused by its maximum extension (by the doctor's hand) with the leg bent at the knee and hip joints. The foot is held in an extension position and makes involuntary flexion-extension movements, as if tapping the doctor’s hand. The presence of clonus in the hand and patella is examined in a similar manner.
Coordination system (damage to cerebellar pathways)
Similar symptoms develop in 62-87% of patients:
- gait disturbance – the patient “rocks” from side to side, staggers even on a flat surface. In later stages, this is accompanied by falls or even leads to the inability to move;
- decreased muscle tone is a characteristic symptom of cerebellar damage. If damage to the motor system predominates, then the tone will be increased, if the cerebellar tone will be decreased;
- missing - any targeted movements do not achieve their goal. If you ask a patient to hit the tip of his nose with a finger while his eyes are closed, he will poke it into his cheek, the wing of his nose, or even his eye. Such disorders interfere with self-care skills, eating, etc.;
- speech disorder - speech becomes abrupt, chanting, words are divided into separate syllables, which are pronounced separately and with emphasis on each syllable;
- violation of handwriting - it becomes uneven, extends beyond the boundaries of the lines;
- trembling of the limbs and head when performing movements;
- nystagmus - oscillatory, rhythmic, involuntary eye movements. It can be so pronounced that it gives the impression of “jumping” eyes. Because of this, vision may be impaired.
Damage to the brainstem and cranial nerves
Occurs in 36-81% of cases:
- limitation of eye mobility when looking to the sides, up, down;
- strabismus, double vision;
- violation of combined movements of the eyeballs: for example, when looking up, one eye looks up and the other deviates to the side. This is called internuclear ophthalmoplegia;
- weakness of the facial muscles (paresis of the facial nerve) - the face is distorted, the eye on the affected side does not close completely, lacrimation develops from it, food and water pour out of the mouth, it is impossible to smile, etc.;
- pain in the facial area like trigeminal neuralgia;
- unclearness, blurred speech, choking when eating, getting food and water into the nose, difficulty swallowing - the so-called bulbar symptoms (develop when the nuclei of the medulla oblongata are damaged);
- the development of retrobulbar neuritis is very common in multiple sclerosis (often the debut of the disease). Manifested by impaired visual acuity and the ability to distinguish colors. The difference in brightness and contrast of the image is no longer visible. In the patient’s field of vision, black dots, gray spots are seen, and sometimes there is a feeling as if you are looking into a pipe. Some half of the visual fields may disappear. Pupillary reactions to light are impaired. When examining the fundus, pallor of the optic nerve head (especially its temporal halves) is revealed, and optic nerve atrophy develops.
Sensory impairment
Happens in 56-92% of cases:
- disorders of deep sensitivity - the body loses control over the perception of its muscles, tendons, joints, i.e. the brain does not receive impulses from these structures. How does this manifest itself? For example, a doctor asks a patient to close his eyes. Touches one of the fingers or toes and makes a slight movement with this finger (bends, straightens, moves to the side). And the patient must say which finger the doctor touches, and in which direction the movement is made. If the patient cannot correctly determine this, then this means that he has disorders of deep sensitivity. Due to such disorders, walking worsens even more, since the patient ceases to feel the surface on which he moves;
- the presence of paresthesia (crawling sensation, itching, burning, numbness, etc.);
- areas of loss of pain and temperature sensitivity - when the patient does not feel the difference between hot and cold, between touching and pricking the skin with a needle;
- pain in muscles, spine.
Pelvic organ dysfunction
Occurs in 26-53% of cases:
- urinary disorders - urinary retention or incontinence (there may be a constant release of urine drop by drop, or there may be periodic emptying as it becomes full, only without a feeling of urge);
- violation of the act of defecation is characteristic of later stages of the disease. By analogy with urinary disorders, constipation or fecal incontinence are possible;
- sexual dysfunction - erectile dysfunction (impotence), lack of orgasm, decreased libido. In women, the menstrual cycle is disrupted.
Symptoms
The symptoms of MS relapses vary, depending on the affected area of nervous tissue. There are characteristic symptoms that indicate multiple sclerosis:
- Impaired vision, pain in the eye sockets.
- Paresthesia of the fingertips, felt as numbness and tingling in the hands.
- When tilting and turning the head, back pain occurs.
- Dizziness, nausea, vomiting.
- Hypotonicity of muscles. Weakness, constant urge to urinate, trembling legs.
- Symptoms of neuralgia: confusion, fatigue, headaches.
- Dysfunction of the reproductive system.
Deviations are present in a person from several days to several years. Symptoms intensify, a progressive form begins with new manifestations. The main difference between the relapsing stage is that clinical indicators increase gradually . Therefore, a person does not notice a serious diagnosis for a long time, citing fatigue from work or study.
After undergoing an examination by a neurologist, the following abnormalities are revealed:
- dysfunction of the vestibular apparatus, resulting in decreased spatial orientation and dizziness;
- damage to the optic, auditory, vestibular, trigeminal nerve;
- inability to make voluntary movements;
- insensitivity to cold or heat;
- psychical deviations.
A neurologist detects symptoms of multiple sclerosis by tapping the legs with a hammer. If a person has decreased muscle strength in the legs, it is necessary to undergo a full examination.
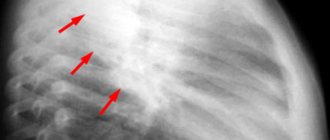
Diagnostics
Diagnosing multiple sclerosis is very difficult. This is facilitated by both the variety of symptoms and their ability to disappear (“flickering” symptoms) in the initial stages of the disease. To diagnose multiple sclerosis use:
- neurological examination to identify clinical symptoms;
- examination by an ophthalmologist with examination of the fundus and determination of visual fields;
- MRI of the brain and spinal cord using a high-power machine using contrast agents (allows you to detect foci of connective tissue - “plaques”);
- study of evoked potentials;
- oligoclonal antibodies in the cerebrospinal fluid (cerebrospinal fluid), which confirm the immunopathological process in the nervous system (can also be observed in other infectious diseases of the nervous system, for example, neuroAIDS).
Today, the generally accepted criteria for making a diagnosis are the criteria of McDonald et al., 2001. They include taking into account clinical symptoms and changes in MRI, evoked potentials, and cerebrospinal fluid.
Treatment
To select effective treatment, it is necessary to take into account many aspects of the course of the disease in a particular patient. Treatment for multiple sclerosis is highly individualized, since the symptoms (or combinations of symptoms) are different for all patients. But there are general principles that are followed when prescribing therapy for all patients with multiple sclerosis:
- treatment as early as possible;
- constant use of medications (even during remissions, to prevent the next exacerbation and slow progression);
- the use of agents that suppress the autoimmune inflammatory process, which prevents the formation of new lesions;
- combining different drugs to achieve greater effectiveness.
All treatment agents are divided into two groups: agents for pathogenetic treatment (affect the mechanism of development of multiple sclerosis) and symptomatic drugs. In addition, treatment is very different during the period of exacerbation and during remission.
Pathogenetic treatment
It is carried out both at the onset of the disease, during exacerbation, and in remission. The goal of such therapy is to stop the autoimmune inflammatory process and prevent myelin destruction.
Exacerbation
At this stage apply:
- Pulse corticosteroid therapy is a short course of large doses of hormones intravenously. Typically, methylprednisolone (Metypred, Solu-medrol) is used 500-1000 mg in 200-400 ml of saline intravenously at a rate of 25-30 drops per minute once a day (in the morning) for 3-7 days. The duration of the course and dosage depend on the severity of neurological disorders. To prevent the side effects of methylprednisolone, potassium preparations (Asparkam, Panangin) and a diet rich in potassium salts (bananas, baked potatoes, apples, raisins) are simultaneously prescribed; substances that protect the gastric mucosa (Ranitidine, Cimetidine, Almagel, Phosphalugel); antibiotics (since hormones reduce the body's defenses, and infection may occur). After pulse therapy, continue taking methylprednisolone tablets, starting with a dose of 24 mg, gradually discontinuing the drug;
- if pulse therapy cannot be carried out, then use Dexamethasone intravenously or intramuscularly 1 time per day, starting with 128 mg (64 mg, 32 mg depending on the severity of symptoms), gradually reducing the dose by 2 times every two days (64 mg 2 days, 32 mg for 2 days, 16 mg for 2 days, etc., as if gradually withdrawing the drug);
- plasmapheresis – purification of blood plasma from antibodies circulating in it. It takes about 2 weeks: during this time, 3-5 procedures are performed (with a break of several days). Using a special device, blood is taken from a vein and passed through a filter system. In it, the blood is divided into cellular elements and plasma. Then the cellular elements are mixed with donor plasma (or with artificial plasma substitutes), and in this form are returned to the patient through another vein. Sometimes plasmapheresis is combined with pulse therapy with hormones;
- human immunoglobulin for intravenous administration (Sandoglobulin, Pentaglobulin) 200-400 mg/kg per day infusions at a rate of 20 drops per minute for 5 days in a row;
- in case of ineffectiveness of hormones, with the steady progression of multiple sclerosis, cytostatics are used (Azathioprine, Cyclophosphamide, Cyclosporine A, Methotrexate, etc.), which suppress the autoimmune process. However, the use of cytostatics has a downside: they are very toxic. These drugs have many severe side effects. They lead to a sharp decrease in leukocytes, erythrocytes, platelets (which is accompanied by a decrease in the body's defenses, the development of anemia, blood clotting disorders), cause drug-induced hepatitis, hair loss, and lead to frequent nausea, vomiting, diarrhea;
- antiplatelet agents, drugs that improve blood circulation - Dipyridamole, Curantil, Pentoxifylline;
- if high titers of antibodies to the herpes virus are detected - Zovirax, Valtrex;
- interferon inducers – Cycloferon, Amiksin.
Remission
Multiple sclerosis is a disease that requires ongoing treatment, even during remission. Clinical symptoms may decrease and the condition may improve, but the process of myelin destruction will continue. To stop the autoimmune process, prevent the progression of the disease, and slow down disability, a special group of drugs is used: preventive (immunomodulatory) therapy drugs. International studies have proven their effectiveness in multiple sclerosis. These are β-interferon drugs (Avonex, Betaferon, Rebif) and glatiramer acetate (Copaxone). The choice of drug depends on the stage of the disease, the mechanism of action and, unfortunately, on the financial capabilities of the patient. Avonex is used 6 million IU once a week intramuscularly, Rebif 6 or 12 million IU 3 times a week subcutaneously, Betaferon 8 million or 16 million IU every other day subcutaneously, Copaxone 20 mg orally daily.
For this group of medications, it is very important to start taking them as early as possible: as soon as the diagnosis of multiple sclerosis is made, it is necessary to start taking them immediately and take them constantly, without interruption. This allows you to prevent the occurrence of new exacerbations, and therefore prevent new functional disorders in the patient. After all, preventing destruction is easier and more effective than treating the consequences. Thus, a person remains able to work for a long time and remains socially active. And this is what we strive for in the treatment of multiple sclerosis, since it is not yet possible to completely cure this disease.
Symptomatic treatment
This type of treatment involves the use of a wide variety of drugs to reduce the symptoms of multiple sclerosis that have already occurred. Symptomatic treatment is used both in the period of exacerbation and in the period of remission. Therapy is carried out asymptomatically:
How does RRMS differ from progressive forms of MS?
If the course of RRMS can be characterized as a relapsing form of MS, in which new foci of inflammation may periodically appear on MRI, then about progressive forms we can say that with them relapses occur much less frequently.
- People with RRMS have much more sclera (scars) in the central nervous system on MRI, and these sclera accumulate much more inflammation around them.
- People with SPMS have a larger number of sclera in the spinal cord, and the number of inflammatory foci around these sclera is less.
Women are observed with RRMS more often than men, approximately 2-3 times, while the number of women and men suffering from PPMS is approximately the same.
It is believed that RRMS is diagnosed at an earlier age.
- Most people with RRMS are diagnosed in their 20s and 30s, while PPMS is more often diagnosed in their 40s and 50s.
- The transition to SPMS usually occurs in people who have lived with RRMS for approximately 10 years.
The most common symptoms in people with RRMS are fatigue, numbness in the limbs, vision problems, spasticity, bowel and bladder problems, learning and memory problems. People with progressive forms of MS are most likely to experience the onset and worsening of movement-related symptoms. List of possible symptoms of MS.
Classification of drugs
Unfortunately, the still unknown reason for the aggressive behavior of one’s own immunity prevents pharmacologists from finding a cure for sclerosis. However, it is possible to significantly slow down its course, and a competent neurologist will definitely prescribe medications that preserve the patient’s quality of life.
All medications that are prescribed for multiple sclerosis are conventionally divided into:
- means for relieving acute conditions;
- drugs to inhibit the development of MS;
- medications intended to alleviate the condition of patients.
Immunosuppressors and cytostatics
For multiple sclerosis, substances that affect the immune system are used. By suppressing individual links, it is possible to control the activity of inflammation. We will talk in detail about such drugs below.
| Abagio First-line DMT Slows metabolism in B and T lymphocytes | Used for secondary relapsing and relapsing-remitting forms; Tablets of 14 mg are taken orally once a day; Nausea, diarrhea and headaches may occur during use. |
| Mitoxantrone Moderate effectiveness Antitumor drug | Used for RRMS, PPMS and SPMS. Disturbs the structure of DNA. Side effects: amenorrhea, urinary tract infections, hair loss, cardiac toxicity and the possibility of leukemia. |
| Cladribine | Relapsing-remitting multiple sclerosis. Tablet preparation. Side effects are minimal, no observation required, short course of treatment. |
| Methotrexate | Used in the treatment of exacerbations and for continuous use; A course of 7.5 mg per week of folic acid is recommended; A large number of side effects (fibrosis, cirrhosis of the liver). |
| Cyclosporine Used to prevent transplant reactions | Used for exacerbations; Dose 5 mg/kg for up to 3 months; Side effects: nausea, hypertension, tremor, headache. |
Relieving exacerbations
Corticosteroid hormones occupy a place in the first line of treatments for exacerbations of multiple sclerosis. When fighting a disease, they have undeniable advantages, suppressing the activity of the immune system that attacks its own myelin? and at the same time significantly inhibiting the inflammatory process.
Corticosteroids include:
- prednisolone (prescribed in tablets);
- methylprednisolone and dexamethasone (administered intravenously).
Unfortunately, these hormones cannot be prescribed for a long term - they have a number of severe side effects, and use in violation of the instructions can lead to death.
If glucocorticoids are powerless, blood purification is prescribed - plasmaphoresis. The patient's blood is passed through a machine that separates it into its component elements. The blood purification procedure lasts about an hour or so.
Inhibiting the development of the disease
Patients are prescribed so-called course-modifying drugs for multiple sclerosis (MSDs).
Interferon beta
Interferon injections are a time-tested treatment for MS that have proven themselves to be effective early in the development of the disease. Interferon beta 1a (injection into the muscle) and beta 1b (subcutaneous) are used for treatment. The main effect of these drugs is to reduce the permeability of the blood-brain barrier, allowing fewer immune cells to reach the brain cells. An additional advantage of interferons is that they protect neurons from damage.
Although they try to minimize the undesirable effect, it still exists - while taking it, a flu-like state and depression can develop. Interferons affect the composition of the blood, reducing the content of leukocytes and, accordingly, suppressing the immune system. Therefore, it is important to avoid sick people at this stage to avoid becoming infected. Not always suitable for children - immunoglobulins are more preferable in childhood.
Copaxone
When it was developed, it initially seemed like a cure for multiple sclerosis had been found. Copaxone is a polymer molecule similar to human myelin. It is injected subcutaneously, using it as a “bait” for immune cells - they leave myelin alone and begin to destroy Copaxone, which is similar to it.
In studies, this drug has not shown any advantage over beta interferons, but its side effects are rare and, as a rule, do not require additional correction.
Immunoglobulins
Second line drug after interferon. Unlike others, immunoglobulins for MS are actively used in childhood. It is administered intravenously, has virtually no side effects and is quite effective in inhibiting multiple sclerosis.
Tysabri
It's also called natalizumab. Its mechanism of action is to bind immune cell receptors. A drip is given with it every four weeks. Tysabri can be combined with interferon beta.
Due to the strong suppression of the immune system during treatment with natalizumab, there is a risk of activation of various diseases, the most dangerous of which is multifocal leukoencephalopathy.
Gilenia
Gilenya (the active ingredient is fingolimod) is an immune suppressant. It is used for relapsing-remitting MS. A side effect is infectious diseases, so during treatment it is necessary to frequently check for possible pathogens.
Gilenya prevents lymphocytes from leaving the lymph nodes, due to which in 70% of patients the effect of significantly reducing the frequency of exacerbations is achieved.
Abagio
The trade name of the substance is teriflunomide, tablets. An immune stimulant that can reduce the number of lymphocytes. It has a large number of side effects, including flu, hair loss, nausea, vomiting and toothache. Despite them, it is very effective compared to interferons.
Antitumor drugs
These include mitoxantrone (brand name Novantrone) and cyclophosphamide (Cytoxan). Traditionally, these drugs belong to chemotherapy and are taken for cancer. But in the case of multiple sclerosis, their ability to suppress the immune system is useful.
The side effects are severe and familiar from the frequent descriptions of cancer patients: nausea and vomiting, hair loss, anemia, bleeding and an increased risk of infection. Therefore, they are gradually moving away from using them, preferring the new drugs Tysabri and Gilenya.
Minocycline
This is an antibiotic that, according to the results of experiments by doctors from the United States, suppresses the inflammatory process in patients with MS. But don’t trust him too much - the substance is still in the testing stage.
Drugs with unproven effectiveness
Domestic doctors can prescribe a combination of lecithin and amixin to patients with multiple sclerosis. Their effectiveness, without being confirmed by reliable research, is rather doubtful.
There are also recommendations to use flurevits - “medicines”, the distributors of which promise miraculous rejuvenation of the body and relief from sores. Miracles, unfortunately, do not happen, and the effect of flurevits is not confirmed by clinical practice.
Course of the disease
The relapsing-remitting type of MS is found in people over 20 years of age. There are no manifestations before this age. The disease cannot be completely cured; remission can only be achieved through treatment. With this type of course, it occurs often and lasts 7-10 years.
During the period of exacerbation, painful sensations suddenly appear, last up to 5 days and disappear abruptly. A person stops feeling muscle weakness and pain.
The course of the disorder is individual, depending on the affected nerves.
- Loss of coordination is manifested by an unclear gait, trembling in the arms and legs, and changes in handwriting.
- Damage to the optic nerves is characterized by pain and double vision, decreased vision, erratic eye movements, and lack of peripheral vision.
- Disorders of the facial nerve are manifested by drooping corners of the mouth, changes in voice timbre, and changes in sensitivity in the head area.
Psychologically, people feel anxiety and obsessive disorders. Their memory and mood decrease, and depression appears.
After the onset of an attack, one or more symptoms may appear, or a new sign may develop. The patient's condition worsens. Hand tremors begin, legs become weak, speech becomes confused. An experienced neurologist will suspect neuralgia when a single symptom appears.
Improving the quality of life of patients
Muscle stiffness
This group is represented by only one medicine - fampira (trade name fampridine). Unfortunately, it is not registered as a medicine in Russia, so you will have to buy it through foreign pharmacies. Fampira relieves muscle stiffness caused by damage to nerve pathways and returns the patient the ability to move without assistance.
Muscle pain
Frequent muscle spasms, sometimes very painful, are relieved with the help of substances such as:
As a long-term (up to six months) action drug, botulinum toxin injections into the muscle can be used, the cosmetic version of which is known under the brand name Botox.
Chronic fatigue
MS patients often complain of chronic fatigue. Unfortunately, in our country there is practically nothing to treat it with - the Western drug of choice, Provigil (modafinil), is prohibited in the Russian Federation. There are still drugs based on amantadine, but its effect is weak and not in all patients.
Depression
Any chronic disease that requires combating it depletes the moral strength of the patient, and multiple sclerosis is no exception. In order to prevent the patient from losing heart (which is not useful for any disease), the doctor may recommend substances from the group of antidepressants, such as:
erectile disfunction
She often accompanies sick men. To correct sexual dysfunction, Viagra (sildenafil) or its analogues Cialis and Levitra are prescribed.
Paresthesia and hypoesthesia
A sudden painful and unpleasant increase in skin sensitivity, tingling, burning, or, conversely, a decrease in sensitivity, occurring due to disruption of the normal transmission of impulses along the nerves, is corrected with gamma-aminobutyric acid analogues gabapentin or pregabalin. In some cases, tricyclic antidepressants amitriptyline and nortriptyline may be prescribed.
Constipation
A frequent inconvenience. Removable with common bisacodyl, docusate or magnesium.
Urinary dysfunction
Urination disorder is observed in the vast majority of patients. Frequent or nighttime urinary incontinence, as well as various delays, occur. To help deal with this:
- darifenacin (Enablex);
- oxybutynin (ditropan);
- tamsulosin (Flomax);
- tolterodine (detrol).
So which medicine is better to take?
Without the consent of the doctor - nothing. Remember that our article is not a guide to action, but just a short reference book of the most common remedies used for sclerosis. Multiple sclerosis is a serious disease that is treated with potent substances with many side effects.
The simultaneous use of several potent drugs in itself causes a significant blow to the patient’s body. For effective treatment, suitable drugs must be selected. All this requires constant monitoring of the condition, which cannot be carried out at home.
If you have experience using drugs for MS, or know about a new drug, please share this information in the comments.
Treatment of multiple sclerosis (MS) is one of the most pressing problems of modern practical neurology. Due to the fact that the exact causes of the disease remain unclear, prevention and etiotropic treatment are impossible. At the same time, intensive research in recent years has led to the creation of new highly effective drugs that slow down or stop the development of MS and prevent the development of disability in patients. Therapy for multiple sclerosis is carried out in four main areas:
- 1) Treatment of exacerbations of the disease
- 2) Prescription of effective drugs that modify the course of MS (DMT, disease modifying therapy). The main goal of DMT is to reduce the frequency and severity of exacerbations, slow down or, ideally, completely stop the increase in disability, prevent the onset of MS progression or, if there is progression, slow it down. All currently existing DMTs affect only the immune system, blocking autoimmune aggression through various mechanisms. There are currently no drugs that restore damage to the central nervous system; restoration of lost functions is possible only through rehabilitation treatment - the third direction of MS therapy
- 3) Neurorehabilitation is a rapidly developing science, the main goal of which is to study the mechanisms of restoration of damage to the central nervous system and methods of influencing them.
- 4) Symptomatic therapy is aimed at relieving certain symptoms of the disease that interfere with the patient’s normal functioning. The possibilities for symptomatic treatment of MS are limited, however, neurologists in their treatment arena have drugs that affect spasticity, disorders of the pelvic organs (urgency, urinary retention, constipation, erectile dysfunction), and pathological fatigue.
A neurologist or multiple sclerosis specialist must, in close cooperation with the patient and doctors of related specialties, determine the necessary treatment and rehabilitation measures, monitor their effectiveness during dynamic observation, changing therapy in a timely manner (for example, if DMT is insufficiently effective, symptoms that need correction appear).
Diagnosis of RRMS
The criterion for diagnosing a relapsing-remitting course of MS is evidence of the presence of affected areas of myelin in at least two areas of the central nervous system (spread in areas) that occurred at different times (spread over time). And of course, other diseases that can lead to the same symptoms must be excluded.
When distribution in areas and distribution over time is proven (the fastest and most accurate method is MRI), as well as a neurological examination, a diagnosis can be made quickly.
In cases where lesions in two different sites are not confirmed or cases are not confirmed to have occurred at different times, a clinically isolated syndrome may be diagnosed. In this case, it may take time (several months, years) to establish a final diagnosis.
Treatment of exacerbations.
In the early stages of relapsing-remitting multiple sclerosis, mild exacerbations often resolve on their own. For the treatment of severe exacerbations of MS, corticosteroids (methylprednisolone, solumedrol, dexamethasone, ACTH drugs) remain the drugs of choice. Their action is aimed at reducing inflammation and reducing the increased permeability of the blood-brain barrier, which can reduce the duration of exacerbation and reduce the severity of neurological disorders. The greatest effect from the use of corticosteroids can be expected when the disease lasts less than 5 years. When severe repeated exacerbations of multiple sclerosis are resistant to corticosteroid therapy, Sandimmune (cyclosporine A) is sometimes used. This drug is recommended to reduce the activity of exacerbation and prevent subsequent severe exacerbations. The prescription of antioxidants, antiplatelet agents, angioprotectors, and proteolysis inhibitors in the treatment of exacerbations of MS is due to obvious biological expediency. These drugs (trental, chimes, vitamin C, vitamin E, glutamic acid, nootropics, Cavinton, thioctacid, berlition, contrical, etc.) are used according to generally accepted therapeutic regimens. Plasmapheresis is effective in combination with corticosteroids or cytostatics.
The insidiousness of the disease
Modern neuroimaging methods make it possible to detect foci of demyelination in the early stages. The standard examinations in this case are magnetic resonance imaging and, less common in our country, positron emission or radionuclide studies. However, no one goes for examination for no apparent reason. The insidiousness of multiple sclerosis is that clinical manifestations begin when at least 40% of neurons are affected; until this stage, the course is asymptomatic. Many newly identified cases have been described in which more than 50% of the nerve fibers were affected. It is clear that with such massive damage, the possibilities of healing are extremely limited. Detection of foci of demyelination in the early stages is an accidental finding, and it is not possible to change this in the near future.
In recent years, people have started talking about clinically isolated symptoms that cause medical caution. This may include numbness, weakness of a small muscle group, urinary retention, and blurred vision. Only one symptom appears, but it also “passes” without treatment within 2-3 days. During this time, almost no one gets to the doctor. It is possible to understand that this was the debut of a formidable disease only in retrospect, when a clear clinical picture unfolds several years later.
If you have unclear symptoms, it is always better to undergo an MRI.
Prevention of exacerbations.
The result of many years of research has been the emergence of a number of immunomodulatory drugs that actually reduce the frequency of exacerbations in relapsing-remitting, as well as remitting-progressive course of multiple sclerosis. The result of worldwide clinical trials conducted in a double-blind manner was evidence of a reduction in the frequency of exacerbations of MS by an average of 30% with regular use of these drugs. In addition, they, to varying degrees, slow down the rate of increase of irreversible disorders leading to disability. Positive clinical data in the treatment of multiple sclerosis with Copaxone and beta-interferon drugs (Betaferon, Rebif, Avonex), as a rule, coincide with MRI data showing a significant decrease in the number of active lesions and a decrease in the total volume of focal brain lesions. A similar effect was also noted in preparations containing large doses of immunoglobulins for intravenous administration (sandoglobin, etc.).
Types of flow
According to the international classification, the following types of multiple sclerosis are distinguished:
- relapsing – remitting;
- secondary - progressive;
- primary - progressive;
- progressive - recurrent.
The course can be benign and malignant. A benign course is considered to be one in which, after 15 years from the onset, the person has not become disabled. With a malignant course, there are practically no remissions.
Special types include rare diseases: Devic's neuromyelitis optica, Schilder's disease or diffuse cerebral sclerosis, Ballot's concentric sclerosis.
The remitting course is the most common, recorded in 90% of primary cases.
Graphically, the flow types look like this:
Types of multiple sclerosis
With the remitting type, exacerbations alternate with remissions, the overall decrease in quality of life increases gradually or remains at the same level. With each subsequent exacerbation, a new symptom may appear or an old one may recur. At least 30 days pass between exacerbations. The prognosis for this type of course is favorable; patients can remain functional for years or decades.
Treatment of secondary progressive multiple sclerosis.
Treatment for secondary progressive MS varies among three groups:
- patients with persistent exacerbations and active lesions accumulating contrast on MRI. For them, methotrexate or beta-interferon is recommended;
- patients with gradually steady progression; they are usually prescribed methotrexate or mitoxantrone;
- patients with rapidly progressing malignant course. Treatment with cyclophosphamide, cyclosporine A, azathioprine, methotrexate or mitoxantrone in combination with high doses of corticosteroids is possible.
How does RRMS develop?
The level of disease activity and degree of progression should be determined periodically by neurological examination and MRI. This knowledge can help the neurologist prescribe the necessary treatment and predict the expected results. For example:
- In the case of active and/or worsening RRMS, hospitalization with treatment aimed at extinguishing the latest exacerbations may well be necessary. This usually involves intravenous followed by oral methylprednisolone therapy.
- If there are no obvious deteriorations and new symptoms due to the treatment received, but new foci of inflammation are identified on the MRI, then it may be necessary to switch to another type of treatment, which allows you to consolidate the achieved results for a longer period.
- In the case when the course of RRMS is not active, without deterioration and without the emergence of new inflammation on MRI, we can say with confidence that the chosen type of treatment is effective.
Symptomatic treatment of multiple sclerosis.
Symptomatic therapy and medical and social rehabilitation include not only the restoration of motor and sensory functions, normalization of the mental state and ability to work, but also measures to restore the patient’s social activity to the maximum possible extent, maintain his independence, and actually improve the quality of life, which plays an important role in the correction of neurological manifestations in patients with MS. Depending on the area of application, therapy can be distinguished that corrects the following disorders:
- motor, coordination;
- neuropsychological;
- functions of the pelvic organs;
- pain, paroxysmal disorders.
Properly chosen symptomatic therapy not only improves the clinical condition and quality of life of patients, but also prevents the development of complications of multiple sclerosis, especially in the secondary progressive course of the disease, such as infectious diseases, disorders of autonomic functions and peripheral circulation, the formation of contractures and bedsores.