| Paralysis | |
| Schematic representation of dysfunction in paralysis | |
| ICD-10 | Sometimes classified as R29.8 Other and unspecified symptoms and signs related to the nervous and musculoskeletal systems |
| ICD-9 | 342, 343 and 344 |
| MeSH | D010291 |
Paresis
(from ancient Greek πάρεσις [paresis] “weakening”) is a neurological syndrome, a decrease in strength caused by damage to the motor pathway of the nervous system.
Paralysis
(Ancient Greek παράλυσις “relaxation”) or
plegia
(Ancient Greek πληγή “defeat, blow”) is a complete absence of voluntary movements, due to the same reasons as in the case of paresis. Some characteristic types of paralysis are designated by appropriate terms, for example hemiplegia, paraplegia.
Classification
| This section is missing references to information sources. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on June 6, 2020 . |
- According to the level of damage to the nervous system:
- central
- peripheral
- mixed
- psychogenic
- By severity:
- Easy
- Moderate
- Deep
- Paralysis
- Most common within one limb: Weakness of one muscle
- Weakness of a muscle group (flexors, extensors)
- Parts of the limb (distal or proximal)
- One limb (monoparesis)
In addition to paresis of skeletal muscles, the term is also applicable to the muscular membranes of internal organs: paresis of the intestines, bladder.
There are two scales for assessing the severity of paresis - according to the degree of decrease in muscle strength and the degree of severity of paresis, which are the opposite of each other:
- 0 points “muscle strength” - no voluntary movements. Paralysis.
- 1 point - barely noticeable muscle contractions, no movements in the joints
- 2 points - the range of motion in the joint is significantly reduced, movements are possible without overcoming the force of gravity along the plane
- 3 points - a significant reduction in the range of motion in the joint, the muscles are able to overcome gravity and friction (the possibility of the limb being torn off the surface)
- 4 points - slight decrease in muscle strength, with full range of motion
- 5 points - normal muscle strength, full range of motion
Based on the location of the lesion, two groups of paralysis are distinguished, which differ significantly in clinical manifestations:
- flaccid (peripheral) paresis and paralysis
- spastic (central) paresis and paralysis
- Mixed, having signs of both flaccid and spastic paresis.
The most significant features of peripheral paresis and paralysis are:
- Hypotonia up to atony (decreased tone) of muscles;
- Hypotrophy up to muscle atrophy due to cessation of autonomic innervation;
- Hyporeflexia up to areflexia - decreased severity of reflexes from the affected limb;
- Absence of pathological signs;
- Much less often, in some diseases, fasciculations occur - involuntary contractions of individual muscle fibers, which are one of the symptoms of damage to the large alpha motor neurons of the anterior horns of the spinal cord.
Central paresis is characterized by:
- Hypertonicity (increased muscle tone) of the spastic (or pyramidal) type, the “jackknife” phenomenon;
- No malnutrition;
- Hyperreflexia (increased intensity of deep reflexes), up to the appearance of clonus, as well as a decrease in superficial reflexes;
- Pathological reflexes (extensor: Babinsky, Oppenheim, Schaeffer, Gordon, Chaddock, Pussep; flexion: Rossolimo, Zhukovsky, Bekhterev, Mendel, etc.);
- The appearance of pathological synkinesis (friendly movements), for example, when a patient, voluntarily clenching a healthy hand into a fist, involuntarily repeats this movement with the affected hand, but with less force;
Symptoms of paresis
The signs and symptoms of paresis of different origins do not differ from each other (it is possible to determine the type only by special diagnostic measures).
- Hanging of the head, often forward, inability to keep the head straight;
- Weakness in the arms, up to their free hanging: difficulties in holding objects, in raising the arms, in keeping them suspended;
- Change in gait - waddling from one leg to another, lameness;
- Weakness of the legs, up to the inability to move independently;
- Difficulty when trying to stand up on your own;
- Weakness of the feet: “cock” or “chasing” gait – high raising of the foot with simultaneous sagging;
- Strengthening or, less frequently, weakening of reflexes from the limbs (depending on the location of the lesion).
Causes and mechanisms of disease development
| This section is missing references to information sources. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on June 6, 2020 . |
| This section is not completed. You will help the project by correcting and expanding it. |
Paralysis is not caused by any one etiological factor. Any damage to the motor pathway from a cortical neuron to a peripheral nerve can lead to impaired motor function.
If any part of the motor pathway is damaged - from a cortical neuron to a peripheral nerve - excitation is not transmitted to the muscle, and weakness occurs in the limb or other part of the body that the weakened muscle moved.
Symptoms
Vascular paresis is accompanied by congestion, visible if the vessels are accessible for visualization. This is diffuse hyperemia, and then cyanosis of the skin, which seems cold, hard, lifeless to the touch.
Chronic angiopathy leads to necrosis of tissues in which paretic vessels pass. For example, paresis of the veins of the lower extremities in alcoholics leads to a prolongation of the response of the Troyanov-Trendelenburg test not due to damage to the valves, but due to pareticity of the vessels. Paresis of cerebral vessels leads to the development of a stroke or (if the paresis resolves on its own) to symptoms of a transient ischemic attack.
Diagnostics
| This section is missing references to information sources. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on June 6, 2020 . |
| This section is not completed. You will help the project by correcting and expanding it. |
Detection of paresis occurs exclusively clinically without the use of additional instrumental studies. Muscle strength is assessed in comparison with the muscle strength of the examiner and the opposite part of the body. A scoring scale is used to assess limb strength. (see section Classification
) Less commonly, in the absence of gross paresis, it may not be noticeable during a standard resistance test. In such cases, paresis can be detected using the Barre test, when the patient is asked to hold his arms or legs in a suspended position for a long time. In this case, within 20 seconds the affected limb will gradually lower.
Features of diagnosis in children
At the initial stage of the formation of paresis, the child feels only some discomfort, which later develops into paralysis. If children have any acute diseases of the nervous system, paralysis is characterized by spontaneous and rapid development. With a disease of the peripheral nervous system, the child feels pain in places where paresis is present. In the event of an unexpected attack, it is necessary to provide first aid aimed at limiting the disease that provoked the paresis itself.[1][2]
Diagnosis and treatment
The diagnosis is rarely made by chance; complaints can only lead to suspicion of the presence of vascular paresis. Angiography is required - a contrast study of blood vessels using a fluoroscopic system.
Angiography allows you to see the current functional state of blood vessels, the presence of collateral blood flow, and determine the prevalence of vascular paresis. In some cases, computed tomography and MRI are used.
Treatment consists of normalizing vasomotor functions, treating the underlying disease, as well as eliminating symptoms that were caused by paresis.
Treatment and prevention
| This section is missing references to information sources. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on June 6, 2020 . |
| This section is not completed. You will help the project by correcting and expanding it. |
In complex treatment, it is necessary to use heat in combination with massage, which promote the development of active nerve impulses and improve tissue trophism. Massage is a kind of passive gymnastics. When the patient gains the ability to produce active muscle contractions, they begin to combine massage with active movements, gradually increasing the load, and include movements with resistance, which increase the volume and strength of the muscles. Massage used for flaccid paralysis must be strictly dosed.
Hardware methods
- Propriocorrection
Robotic methods
In the treatment of paresis caused by central damage to the nervous system, robotic complexes are widely used to help restore motor functions. Such systems are based on the theory of motor learning through repeated repetition of movements [3]. One of the methods of such treatment is HAL therapy.
Advantages of Yusupov Hospital
- The average experience of our neurologists is 14 years. Many have an academic degree and are doctors of the highest category;
- Well-developed area of rehabilitation treatment - modern equipment for mechanotherapy, experienced instructors;
- We adhere exclusively to the principles of evidence-based medicine and use the best practices of foreign colleagues;
- We did everything to make the patient feel comfortable in the clinic, to create a positive attitude towards recovery.
All this serves one goal - to achieve the maximum therapeutic effect in each patient, the fastest and most complete restoration of impaired functions, and improve the quality of life.
Notes
- Paresis
- Paresis // Great Soviet Encyclopedia: [in 30 volumes] / ch. ed. A. M. Prokhorov. — 3rd ed. - M.: Soviet Encyclopedia, 1969-1978.
- Rocco Salvatore Calabrò, Alberto Cacciola, Francesco Berté, Alfredo Manuli, Antonino Leo.
Robotic gait rehabilitation and substitution devices in neurological disorders: where are we now? // Neurological Sciences: Official Journal of the Italian Neurological Society and of the Italian Society of Clinical Neurophysiology. — 2016-01-18. — ISSN 1590-3478. — DOI:10.1007/s10072-016-2474-4.
Treatment of paresis
Treatment of paresis in diseases of the spine and spinal cord must be comprehensive, individual and aimed at eliminating the underlying disease that caused this paresis.
Drug treatments
- The use of broad-spectrum antibiotics to fight infection, especially purulent ones. Ceftriaxone is most often prescribed (dosage depends on the pathological condition);
- B vitamins to normalize nerve conduction;
- Prozerin is a drug that restores nerve patency.
Physiotherapeutic treatments
- Massage. Normalizes blood flow, nerve transmission, relieves increased muscle tone and stabilizes the spine;
- Electrical stimulation. Restores broken nerve connections, improves nerve conduction in sensory and motor branches of nerve endings;
- Gymnastics and exercise therapy. Restores movement in the limbs, strengthens and stabilizes the spine and muscular frame of the back. All exercises are selected and developed by the doctor individually and adjusted in the process of changes;
- Swimming. Being in the water and performing special exercises, and, if possible, swimming with the use of auxiliary objects, quickly relieves the vertebrae from the load, aligns and stabilizes the spinal column, strengthens the muscular frame of the back, improves blood flow and nerve conduction;
- Consultations with a psychotherapist and psychologist. They help find and solve psychosomatic problems, increase self-confidence, adapt to temporary or permanent movement disorders, and much more. This long-term work is quite effective if the patient takes an active part in it, and is not just a listener to the specialist’s stories.
Surgery
It is used quite often in cases of paresis and spinal pathology to eliminate the main cause of this symptom:
- Removal of the tumor;
- Removal of a foreign body (bone fragments, bullets, glass, etc.);
- Vascular operations (removal of a blood clot, suturing of a vessel, etc.);
- Removal of purulent foci, their sanitation and tissue cleansing;
- Installation of vertebral implants.
Traditional methods of treating paresis
Traditional medicine is a fairly good and effective aid to the main treatment, traditional. It strengthens the body, accelerates the effects of medications, improves the processes of restoration of nervous tissue, normalizes blood flow and has many other effects. However, its use as monotherapy is not advisable and threatens to worsen symptoms.
Tea from a collection of herbs. Mix 2 tablespoons of chamomile flowers, garden marjoram, rose hips and roots, thyme, medicinal veronica, laurel leaves and tannic sumac. Brew like regular tea. Drink 3-4 times a day, with the addition of honey to taste. The duration of treatment is at least 2 months.
Pine baths. You should take 1.5-2 kg of spruce, pine or other coniferous tree needles, fill them with 5 liters of water and boil for 30 minutes. Then leave for about 10-12 hours, filter and store in the refrigerator. Add 1.5-2 liters of this decoction to a warm bath (with a comfortable water temperature) and take a bath for 20 minutes daily. The course of treatment is 20-30 days.
Tetraparesis and tetraplegia: what is it?
Tetraparesis is a decrease in muscle strength in the arms and legs.
Tetraplegia is a complete lack of muscle strength in the limbs; in other words, it is paralysis in the arms and legs. This is the case when a person is immobilized and cannot move independently. Despite the serious picture of neurological impairment, this process does not always occur completely and irrevocably. It all depends on the disease caused by tetraparesis or tetraplegia.
Muscle strength in points: assessment in medical practice
Muscle strength in clinical practice is assessed on a 5-point scale. It is assessed during a medical examination and more often when assessing the neurological status by a neurologist and/or neurosurgeon.
Neurological status is an assessment of the state of neurological functions and the degree of their loss (if any).
- 5 points is full muscle strength and indicates the normal state of the neuromuscular system.
- 4 points is a mild decrease in muscle strength, called mild paresis
- 3 points - moderate decrease in muscle strength, moderate paresis
- 1 and 2 points - a pronounced decrease in muscle strength, called deep paresis
- 0 points - complete lack of muscle strength in the muscles being tested, called plegia or paralysis.
For assessment, muscle strength is determined in different muscle groups of the limbs. One of the simplest assessment methods is for the patient to squeeze the 2nd and 3rd fingers of the doctor’s hands. The assessment, in this case, is subjective, but has its own criteria.
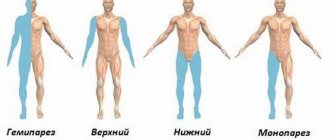
Power paresis is also divided depending on the number of limbs in which a decrease in muscle strength has occurred. Let's look at this in more detail below.
Paresis
Causes of paresis
After a stroke, complete paralysis or paresis may develop. It depends on how destructive the bleeding in the brain was or the disruption of blood flow and oxygen starvation of cells. Also of great importance is how quickly a person received medical care and which areas of the brain were most affected by a stroke.
Moreover, due to damage to certain brain areas, nerve impulses do not reach part of the body at all or do not reach completely, therefore, for example, the desire to strongly clench a fist is actually realized as a slight movement of the fingers.
Injuries to the base of the skull and muscle groups located in this area can also cause paresis. Moreover, in this case, paralysis of the facial nerve mainly occurs, which prevents a person from blinking, swallowing, chewing and speaking normally. Sometimes only one side of the body is damaged, while the other functions normally. In this case, paresis can last until the end of the patient’s life, and completely disappear over the course of several months or years.
Another factor contributing to the occurrence of paresis can be spinal cord injury. In this case, several muscle groups are affected, which stop receiving nerve impulses from the brain, and therefore stop functioning. Usually all muscles located below the damaged area are affected. Moreover, paresis in this case is cured quite rarely, only if the injury was not very serious.
Poisoning and intoxication
– another factor that can cause paresis. But, as a rule, this happens quite rarely due to the level of modern life.
Paresis can also be caused by certain diseases, such as Lyme disease or Alpers syndrome.