| Oculomotor nerve palsy | |
| Diagram of the optic nerves | |
| ICD-10 | H 49.0 49.0 |
| ICD-10-CM | H49.0 |
| ICD-9 | 378.52 378.52 |
| DiseasesDB | 2861 |
| eMedicine | oph/183 |
| MeSH | D015840 |
Oculomotor nerve palsy
is an eye condition resulting from damage to the oculomotor nerve or its branch. As its name suggests, the oculomotor nerve controls the bulk of the muscles that control eye movements. Thus, damage to this nerve causes the affected person's eyes to be unable to move. In addition, the nerve also controls the muscle of the upper eyelid and the muscles responsible for constricting the pupil (pupillary sphincter). Restrictions in eye movements are usually so severe that the affected person is unable to maintain normal eye alignment when looking straight ahead, resulting in squinting and resulting double vision (diplopia).
Oculomotor nerve palsy is also known as “oculomotor neuropathy.” [1]
Eye positioning[edit | edit code]
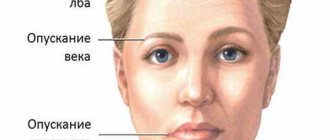
Complete oculomotor nerve palsy
results in a characteristic
downward and outward
. The eye will move outward and downward; outward because the lateral rectus muscle (innervated by the sixth cranial nerve) will receive muscle tone relative to the paralyzed medial rectus muscle. The eye will move downward because the superior oblique muscle (innervated by the fourth cranial nerve or trochlear nerve) is not antagonistic to the paralyzed superior rectus muscle, inferior rectus muscle, and inferior oblique muscle. The affected person will also have ptosis, or drooping eyelids, and mydriasis (dilated pupils).
It should be borne in mind, however, that the extensive structure of the oculomotor nerve means that damage suffered at different points along its path, or damage caused in different ways (compression from loss of blood supply, for example), will result in effects on different muscle groups, or different individual muscles, thus producing different patterns of presentation.
Compressive injury to the oculomotor nerve can cause compression of the parasympathetic fibers before the motor fibers become impaired, since the parasympathetic fibers travel along the outer surface of the nerve. Thus, it can lead to eyelid ptosis and mydriasis (dilation of the pupil) as a result of the compression of the parasympathetic fibers to a "down and out" position.
Complications
Since coordination of movements is impaired and falls become frequent, bruises and fractures are possible. As the pathology progresses, oligobradykinetic syndrome leaves patients bedridden after a few years.
If there is no proper care, such patients develop all the delights of bed rest - bedsores, joint contractures, congestive pneumonia. Such patients often experience sleep apnea, which can lead to death during sleep.
Due to decreased immunity, it is not uncommon for intercurrent diseases and infections to occur - pneumonia, cystitis, pyelonephritis, which becomes a serious complication for the patient. There is therefore a high risk of sepsis.
As paralysis progresses, choking appears and aspiration of food may occur. As a result, the patient becomes exhausted. Life expectancy usually does not exceed 10 years.
Reasons [edit | edit code ]
Oculomotor palsy can result from a number of different conditions. Oculomotor nerve palsy with a non-traumatic middle pupil is often called "medical third" (English medical third) for a similar effect on the pupil, known as "surgical third" (English surgical third).
Congenital oculomotor palsy [edit | edit code]
The origins of most congenital oculomotor palsies are unknown, and the medical term is often used idiopathically. There is some evidence of a familial predilection for this condition, particularly partial paralysis involving nerve separation with autosomal recessive inheritance. The condition may also result from aplasia or hypoplasia of one or more muscles controlled by the oculomotor nerve. It can also occur as a result of severe birth trauma.
Acquired oculomotor paralysis [edit | edit code]
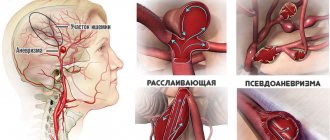
- 1. Vascular disorders such as diabetes, heart disease, atherosclerosis and aneurysm, particularly in the posterior communicating artery
- 2. Space occupied by a lesion or tumor, both malignant and non-malignant
- 3. Inflammation and infection
- 4. Trauma
- 5. Demyelinating diseases (multiple sclerosis)
- 6. Autoimmune diseases such as myasthenia gravis
- 7. Postoperative complications of neurosurgery
- 8. Cavernous sinus thrombosis
Ischemic stroke more selectively affects somatic fibers from parasympathetic fibers, while traumatic stroke affects all types more evenly. Thus, while almost all forms cause ptosis and disturbances in eye movement and pupillary movement, the disturbances are more often associated with trauma than with ischemia.
From the history
Until the mid-20th century, PSP was considered a consequence of epidemic encephalitis. But in 1963-1964. Canadian neurologists Steele and Richardson, together with pathologist Olshevsky, described a hitherto unknown neurodegenerative independent disease, which was not and was not associated with previous encephalitis.
The researchers presented 7 cases of pathology, which were united by the presence of akinetic-rigid manifestations of parkinsonism, pseudobulbar disorders, supranuclear ophthalmoplegia and dementia.
In the USSR, PSP was described later, only in 1980, using the example of 2 patients treated in the clinic of nervous diseases of Moscow State Medical University named after. THEM. Sechenov in Moscow. The incidence of the disease, according to various sources, ranges from 1 to 6 people per 100 thousand population.
After 80 years, the rate reaches 14.7 per 100 thousand population. This suggests that the risk of pathology increases with age. The manifest period manifests itself in pathology between the ages of 55 and 70 years; men get sick 2 times more often.
PSP refers to tauopathies, which also include Pick's disease and Alzheimer's disease, multiple system atrophy, and corticobasal degeneration. Therefore, these listed pathologies have some common symptoms. All of them are united by the formation of inclusions in neurons of a pathological protein - tau protein. This was revealed by molecular genetic studies.
In ICD-10, progressive supranuclear palsy is classified in the section of extrapyramidal and other motor disorders, in the subsection of other degenerative diseases of the basal ganglia, coded as G23.1.
Causes of pathology
Paresis can provoke a chronic inflammatory process of the ENT organs.
In a healthy organ, the oculomotor nerve provides innervation to the muscles that contribute to the mobility of the eyelid and eyeball. Under the influence of unfavorable factors, nerve conduction is disrupted, paralysis of the extraocular muscles develops and the eye becomes motionless. The main causes of pathology in adults:
- traumatic brain injury;
- cardiovascular diseases;
- aneurysm;
- diabetes;
- benign or malignant neoplasms of the head or face;
- rapid muscle fatigue (myasthenia gravis);
- autoimmune diseases;
- stroke.
At an early age, the pathology can be caused by meningitis.
Paresis of the eye muscles in children occurs under the following circumstances:
- birth injury;
- severe infectious diseases (meningitis, meningoencephalitis, measles);
- underdevelopment of the oculomotor muscles;
- heredity.
Return to contents
Symptoms: how to recognize the disease?
Healthy eyes move synchronously. Paralysis of the external muscles of the eye is characterized by the inability to fully move the organ of vision to the sides. If one eye moves normally, but the other lags behind, this may indicate the development of pathology. Paresis of the abducens ophthalmic nerve manifests itself as follows:
- splitting of objects;
- drooping upper eyelid;
- strabismus;
- unnatural dilation of the pupil and lack of its reaction to light;
- impaired eye mobility from side to side;
- inability to see objects that are at different distances;
- exophthalmos.
Return to contents
Prevalence of the disease
Progressive supranuclear gaze palsy is the most common type of atypical parkinsonism. It occurs in 5.3 cases per 100,000 population. It can be compared to ALS in terms of prevalence in the population. Progressive disease begins at 60-65 years of age. Death occurs within 6-7 years from the onset of symptoms. The cause is cardiac and respiratory disorders.
How is diagnosis carried out?
An ophthalmologist can recognize oculomotor nerve palsy. If necessary, you should consult a neurologist. The doctor conducts a visual examination, takes a medical history, and performs diagnostic procedures, such as:
- angiography of eye vessels;
- magnetic resonance and computed tomography;
- ophthalmoscopy;
- friendly and direct reaction of the pupils to light;
- checking the mobility of the eyeballs.
Return to contents
Treatment: which methods are effective?
Surgical intervention
Treatment for oculomotor nerve palsy involves surgery. The vertical or superior rectus muscle of the eye is moved to stabilize proper vision of objects. A drooping eyelid is also eliminated by hanging it from the forehead muscles with a silicone thread.
Physiotherapy
To strengthen the eye muscles and improve vision, a set of eye exercises is recommended, which includes the following exercises:
Bringing the organs of vision to the nose will help strengthen their muscular system.
- Move your gaze from the ceiling to the floor without moving your head.
- Look diagonally from the top corner of the room to the opposite bottom corner.
- Perform circular rotation of the eyes and frequent blinking.
- Bring the visual organs to the nose.
- Intensively squeeze and unclench your eyelids at a fast pace.
- Move your eyeballs up and down.
- Fix a black circle on the window glass at a distance of 30 cm from the eyes. Move your gaze from this point to objects outside the window: houses, trees, vehicles.
Return to contents
Drug therapy
After surgery, paralysis of the oculomotor nerve is cured with the help of eye drops to improve vascular tone and normalize blood circulation. The following drugs are recommended:
Vitamin complexes and dietary supplements are also effective for improving visual functioning:
Other methods
To treat abducens nerve palsy, doctors recommend the following treatment methods:
- Corrective glasses. They are prescribed to improve vision by a doctor individually, based on the patient’s health condition.
- Viewing stereo images. The benefit of the procedure is to strengthen the eye muscles, normalize blood circulation, increase the load on the nerve fibers, which improves the innervation of the eyes, and helps to speed up focusing when examining objects at different distances.
- Electrophoresis. It is characterized by the effect of electric current on nerve endings, which helps improve nerve conduction of the optic nerve.
Prevention
To avoid paralysis of the muscles and nerves of the left or right organ of vision, head and face injuries should be avoided. People who have problems with the heart or blood vessels are advised to undergo a routine examination by a doctor and carefully take prescribed medications. It is necessary to avoid stress - one of the main causes of stroke, which leads to paralysis of the eye structures. All chronic diseases that can cause pathology should be kept in remission.
The abducens nerve (vi pair of cranial nerves) belongs to the group of fibers of the central nervous system that are responsible for eye mobility. However, its functions are relatively limited. With neuropathy and abducens nerve paresis, external manifestations of the disorder are observed (the eye stops moving outward).
Used informative additional techniques
MRI for progressive supranuclear palsy - allows you to confirm the presence of cerebral atrophy in the anterior parts of the cerebral hemispheres, the midbrain tegmentum and the frontal region. MRI will also help differentiate a brain tumor, ALS, encephalitis, stroke, which can also be accompanied by parkinsonism and cognitive impairment.
EEG - with PSP, the rhythm of brain waves is slowed with dominance of D-waves in the frontal or frontotemporal region. Standard blood and urine tests are not carried out due to their lack of information.
Possible early criteria for progressive supranuclear palsy for doctors are:
- the disease begins after 40 years of age;
- the pathology is progressive in nature from the very beginning, and later its irreversibility is revealed;
- ophthalmoparesis;
- postural instability with falls.
To make a final diagnosis, histologically confirmed pathognomonic changes in brain tissue in PSP may play a role.
Neuropsychological testing is also necessary. It is carried out by such narrow specialists as a psychiatrist, neuropsychologist, who use special tests (MMSE scales, clock drawing test). This study reveals the extent of cognitive impairment. Supranuclear palsy is characterized by retardation of thinking, increased exhaustion, like any organic person. Intellectual impairments are moderately expressed.
Anatomy and functions
The nucleus of the abducens nerve is located in the midbrain. Its fibers further run along the basal surface and enter the region of the oblong section. Part of the abducens nerve extends towards the cavernous sinus and affects the outer lining of the carotid artery. After this, the fibers enter the upper fissure of the eye and reach the posterior surface of the organ of vision.
This anatomy is designed to perform a single function: to innervate the rectus lateral muscle, which is responsible for outward movement of the eye, with the abducens nerve.
Due to muscle mobility, a person can look to the sides without turning his head. When these functions are disrupted, strabismus develops.
The internal rectus muscle, which is an antagonist of the rectus lateral and innervated by other nerves, is responsible for moving the eyes towards the nose. Depending on which fibers are damaged, convergent or divergent strabismus is observed.
Causes
Abducens nerve neuropathy can be caused by complications of influenza, syphilis, encephalitis or diphtheria. In some cases, such disorders are observed due to the spread of a purulent process from the nasal sinuses or acute intoxication of the body caused by poisoning with ethyl alcohol or heavy metals.
Abducens nerve palsy in adults is caused by the following reasons:
- arterial hypertension;
- atherosclerosis;
- injuries in the skull area;
- diabetes.
However, it is not always possible to find out why paresis of the abducens nerve of the left or right eye occurred. In such cases, they talk about idiopathic causes of the development of pathology. Less commonly, this disorder is caused by:
- increased intracranial pressure or arterial hypertension;
- meningitis;
- multiple sclerosis;
- malignant tumor processes in the brain;
- giant cell arteritis;
- stroke;
- hydrocephalus (typical for children).
In children, paresis of the abducens nerve is observed against the background of benign brain tumors, after trauma or infection of the nose, ears or eyes.
Moreover, in a child, disorders often develop quickly and go away over time without causing complications.
Progressive supranuclear palsy
Degenerative diseases of the central nervous system may be associated with disorders of tissue biochemistry, as well as genetic characteristics. Thus, progressive supranuclear palsy occurs due to the accumulation of an abnormal protein in the brain tissue.
Typical manifestations of the disease include parkinsonism, swallowing disorders, insomnia and cognitive impairment. Highly effective treatment aimed at the etiology of the disease has not yet been developed, but therapy can suppress symptoms.
Consultation with a specialist will help the patient learn more about such a pathological condition as progressive supranuclear palsy: treatment, risks, complications, help and other aspects.
Basic information and forecast
Progressive supranuclear palsy is also known as Steele-Richardson-Olszewski syndrome. This is a degenerative disease of the tissues of the central nervous system, affecting cognitive functions, the visual apparatus and other anatomical structures.
The pathology was first described in 1964 as a condition that negatively affects primarily the eyeballs. Today, doctors know more about the clinical picture of supranuclear palsy, but the etiology is still not so well understood.
The disease usually manifests itself in the sixth decade of a patient’s life, but earlier manifestations are also possible. Therapy with proven effectiveness has not yet been introduced into medical practice.
https://www.youtube.com/watch?v=LZixMbUVkKE
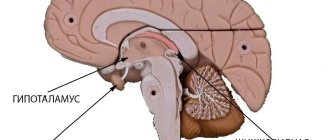
The clinical picture of supranuclear palsy is caused by the accumulation of an abnormal protein in brain cells. The so-called tau protein is predominantly localized in the nuclei of the organ, including the globus pallidus, red and subthalamic nuclei.
The main negative consequences of these biochemical changes include atrophic changes in brain tissue and a deficiency of mediators necessary to perform the functions of the nuclei.
The clumping of tau protein in tissues is thought to be due to genetic changes.
According to epidemiological data, progressive supranuclear palsy is one of the most common types of atypical parkinsonism. This means that such pathology can manifest itself as some signs of Parkinson's disease, as well as atypical signs.
The frequency of detection of the disease does not exceed 6 cases per 100 thousand people per year. The progressive course of paralysis often leads to disability of the patient.
Many patients who suffer from the disease for a long time die from complications, such as a blocked pulmonary artery or pneumonia.
Our boarding houses:
House of Kindness in Solnechnogorsk
Prognostic data have not been sufficiently studied. According to some studies, patients with supranuclear palsy live on average about 10 years after the onset of symptoms. There is conflicting information about the effect of patient age on the rate of progression of pathology.
Anatomical information
The brain is the main part of the central nervous system.
Anatomically and functionally, this organ is connected to the spinal cord, which allows you to control the main vital processes of the body, including movement, heartbeat and breathing.
Cranial nerves also connect peripheral structures, including the sensory organs, to the brain. In this regard, any disturbances in the functioning of this organ can cause serious complications.
At the histological level, the brain is predominantly formed by neurons and supporting structures, neuroglia. Neurons form branched networks with the help of long processes, while neuroglia ensure the maintenance of the functional units of the organ.
Many functions of the central nervous system are determined by the work of nuclei located in various parts of the brain.
For example, the cells of the red nucleus support coordination of movements, and the basal ganglia, in addition to motor activity, combine various functions of higher nervous activity.
As already mentioned, the development of supranuclear palsy is largely due to the improper formation of tau protein. Normally, this substance plays an important role in maintaining neuronal morphology by binding microtubules. Abnormalities of this protein have previously been identified in other degenerative brain diseases, such as Alzheimer's disease.
The pathogenesis is explained by the fact that during abnormal biochemical reactions, tau protein forms insoluble threads that interfere with the functioning of neurons. The exact reasons for such metamorphoses have not yet been identified. Moreover, experts are still not sure that the main source of supranuclear palsy is changes in the structure of the tau protein.
Causes
The etiology of supranuclear palsy is not well understood due to the lack of large studies. The identified molecular changes do not allow us to draw an unambiguous conclusion about the nature of the pathological condition.
Also, lack of information about the trigger mechanism of paralysis, doctors cannot develop effective preventive measures.
It is assumed that in addition to a hereditary predisposition to the disease, there are also risk factors associated with the patient’s lifestyle and environmental situation.
Since the formation of all proteins in the body occurs under the control of DNA, the genetic factor is the main form of predisposition to pathology.
Presumably, progressive supranuclear palsy is transmitted as an autosomal dominant trait associated with changes in the genes of chromosome 17.
The manifestation of the disease in old age may be partly due to natural degenerative processes in the neurons of the brain. Researchers have not identified a single case of supranuclear palsy in a patient under 40 years of age.
Symptoms and complications
The symptomatic picture develops gradually as the tissues of the central nervous system atrophy and the loss of mediators necessary for the functioning of the nuclei. In this case, the first manifestations of the disease are usually associated with impaired motor activity.
Main symptoms:
- Impaired sense of balance while walking. Signs range from mild gait disturbance to frequent falls.
- Inability to focus the gaze on a specific object. Patients also complain of difficulty moving their gaze downward and double contours of visible objects. Visual impairment causes the patient to become clumsy.
Additional signs and symptoms of supranuclear palsy may be similar to Parkinson's disease and dementia. These manifestations also progress over time.
Signs related to atypical parkinsonism:
- Uncertainty in your movements.
- Problems with speech and swallowing food.
- Increased sensitivity to light.
- Sleep disturbance.
- Loss of interest in different types of pastimes.
- Impulsive behavior, including inappropriate emotional displays.
- Impaired memory and intellectual functions.
- Inability to make decisions.
- Depression and anxiety.
- Facial expression disorder.
In later stages, life-threatening complications may develop. Such negative consequences include the following ailments:
- Dangerous injuries from falling.
- Aspiration pneumonia due to impaired swallowing reflex. Food particles penetrate the lung tissue and cause a dangerous infection.
- Respiratory failure due to neurodegenerative changes.
- Pulmonary embolism.
To prevent these complications, the patient requires careful care. In most cases, progressive supranuclear palsy indirectly causes complications specifically on the respiratory system.
Diagnostics
If you identify symptoms of a degenerative brain disease, you should consult a neurologist. The specialist will ask about your complaints, review your medical history, and conduct a physical examination.
Already during a general examination, the main symptoms of pathology associated with impaired coordination, cognitive and visual functions are revealed.
However, an accurate conclusion cannot be given without a differential diagnosis aimed at excluding similar conditions, such as Parkinson's disease and multiple system atrophy. Instrumental studies help clarify clinical data.
Prescribed diagnostic tests:
- Magnetic resonance imaging is a high-precision visual research method that allows you to obtain a three-dimensional image of brain structures. Identifying characteristic changes in the nuclei helps confirm the presence of the disease.
- Positron emission tomography is a radionuclide tomographic method that allows you to more accurately study the features of the patient’s brain.
After analyzing symptoms and visual examination data, the doctor can make a final diagnosis and conduct a consultation to select therapy.
Methods of treatment and rehabilitation
Since progressive supranuclear palsy remains a poorly understood disease, the main treatment is aimed at suppressing symptoms and improving the patient's quality of life.
Treatment options:
- Medicinal substances used in Parkinson's disease. These are drugs that increase the concentration of mediators in the central nervous system.
- Injecting Botox into individual muscles to suppress spasm.
- Prescription of glasses with bifocal or prismatic lenses.
Rehabilitation methods:
- Physiotherapy to improve the condition of the respiratory muscles.
- Special exercises to restore a sense of balance.
- Using special eye drops.
Thus, progressive supranuclear palsy, which often has a poor prognosis, is a common pathology among older people. It is important to contact a neurologist as early as possible for examinations and selection of therapeutic treatment methods.
Source: https://domdobroty.ru/progressiruyuschij_nad_yadernyj_paralich/
Symptoms of the disease
When the abducens nerves are damaged, muscle paralysis occurs. In this case, the nature of the symptoms is determined by the localization of the pathological process. As a rule, it manifests itself in the form of the following symptoms:
- decreased mobility of the eyes (or one eye);
- deviation of the eye to the side;
- attacks of dizziness;
- violation of orientation in space;
- gait disturbance;
- double vision of visible objects (diplopia).
However, if the pathological process occurs inside the brain stem (this condition is known as Fauville's palsy), the abducens and facial nerves may be affected simultaneously. Then the nature of the clinical picture changes. Moreover, with this disorder, not only impaired mobility of the eyeballs is noted, but also paralysis of the limbs.
Forecast
The prognosis for progressive supranuclear palsy is unfavorable, since there is a non-stop and irreversible increase and deterioration of clinical manifestations. The therapy provided is only symptomatic. Some of its effects are too short-lived, no more than 2 years, and even then, very relative.
Actual bed rest begins after 5-7 years. Death with progressive supranuclear palsy occurs due to the addition of intercurrent diseases, which is quite explainable by prolonged bed rest. These could be infections, aspiration pneumonia, kidney disease, etc.
The most disabling factor is postural disorders, and later, during bed rest, the consequences of inactivity such as bedsores and dysphagia increase.
Diagnostics
Diagnosis of paresis of the abducens nerve does not cause difficulties, since even at the initial stage of development of the pathological process, a displacement of the eye to the side is noted. In order to select the optimal treatment, it is necessary to establish the cause of the disease. For this purpose the following are assigned:
- angiography of eye vessels;
- MRI and CT of the brain;
- ophthalmoscopy.
Diagnostics checks the degree of mobility and the nature of the reaction to light of the affected eyes. If necessary, the complex of these measures is supplemented by other studies (general and biochemical blood tests), which make it possible to identify the causative factor.
Treatment methods
Treatment is selected taking into account the characteristics of the provoking factor. Often in the treatment of paresis, a technique is used that involves the introduction of Neuromidin directly into the affected tissue. This approach improves muscle contractility and prevents the development of complications.
The second commonly used treatment option for abducens ophthalmic nerve palsy is the administration of botulinum toxin. This substance helps prevent decreased mobility of the medial rectus muscle. This procedure is complemented by wearing a Fresnel prism, which is attached to glasses and helps eliminate diplopia and maintain binocular vision.
Prisms are not used in the treatment of patients with more serious lesions. In such cases, close the affected eye for a while. The method is not used in the treatment of children, as it can cause lazy eye syndrome.
The duration of wearing the bandage or Fresnel prisms is determined by the severity of the case. It takes an average of 9-12 months for the left or right eye to fully recover.
The general treatment of neuropathy of the abducens nerve of the eye is complemented by exposure to pulsed low-frequency current or electrophoresis with a 15% solution of Neuromidin. Viewing stereo images also demonstrates a good effect. This method is used to strengthen the extraocular muscles, increase the load on the affected nerves, and restore blood circulation in the problem area. Thanks to stereo images, it is possible to normalize the innervation of the visual organs.
Paresis therapy is often combined with eye exercises. The type of exercise is selected individually based on the characteristics of a particular case.
In complicated situations, instead of drug therapy, surgical intervention is used, during which the doctor moves the affected muscles, restoring the previous mobility of the eyeball. At the end of the procedure, eye drops are prescribed to tone the blood vessels and normalize blood circulation. Along with these drugs, it is recommended to take vitamin complexes (Blueberry Forte, Vitalux Plus and others).