A neurology clinic with a good reputation is Mosmed
Diseases of the nervous system are complex in nature, making them difficult to recognize. Symptoms can lead a layman on the wrong track, pointing to other diagnoses. The doctor encounters complaints about functional symptoms during an appointment in 70% of cases. Most often, people complain of chronic pain in joints and muscles, poor sleep and fatigue, loss of appetite or, conversely, insatiable hunger, dissatisfaction in intimate life, various neuroses associated with stress - the clinic of restorative neurology is looking for the causes of all these conditions. Autonomic disorders, manifested in the form of chronic fatigue, dizziness, fainting, shortness of breath, sudden outbursts of fear, are becoming common. The reason for this is the various life difficulties that a person faces, the frantic rhythm, and excessive stress. A weakened, exhausted body is susceptible to nervous system disorders.
Clinic of Restorative Neurology "Mosmed" is one of the best neurology clinics in Moscow
Our clinic’s specialists work with problems of varying complexity, often involving other doctors in solving them. Diagnosticians, psychiatrists, medical psychologists and psychotherapists often make a significant contribution to ridding the patient of the pathologies that worsen his life. The Restorative Neurology Clinic organizes consultations with various specialists. Moscow brought together leading experts in various fields of medicine. Many of them became the golden members of the departments of the Mosmed clinic - these are doctors known not only in the capital, but also beyond its borders. Non-drug treatment methods, which are widely practiced within the walls of the Mosmed clinic, play a significant role in the fight against pathological conditions of the nervous system. Patients of the Restorative Neurology Clinic (Moscow, Gabrichevsky, 5, building 3) can undergo a course of treatment in a hospital followed by continued outpatient observation. For out-of-town patients, as well as for those who need urgent consultations, remote Skype sessions are provided. Don't put off taking care of your health! Make an appointment!
Primary appointment with a neurologist: 1850 RUR.
Sign up Online 5% discount when registering from the site
COVID-19 and neuroscience
Coronaviruses are known for their ability to infect the nervous system and cause various neurological disorders, which have been described with MERS-CoV and SARS-CoV-1. With the increasing number of patients sick (and recovered) from the new coronavirus infection SARS-CoV-2, our understanding of the spectrum of its neurological manifestations is also improving. We've written about this before and now provide an updated and more detailed overview of neurological problems resulting from COVID-19, describing their pathophysiology and possible treatment. The review was published recently in the journal JAMA Neurology.
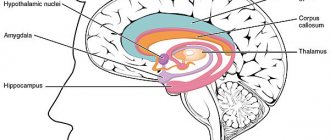
Distribution in the brain of the “gate of entry” for the new coronavirus SARS-CoV-2 – angiotensin-converting enzyme 2 (ACE2) receptors. Credit: Adeel S. Zubair et al. / JAMA Neurology 2020
As reported in various clinical cases, the routes of entry of the SARS-CoV-2 virus into the nervous system and tissue targets may be very different from each other. The virus is able to invade the nervous system via a transsynaptic transfer mechanism (similar to neurotransmitter transport). It is capable of infecting the endothelium (inner lining) of blood vessels or migrating inside leukocytes through the blood-brain barrier.
Therefore, the clinical manifestations of the nervous system vary somewhat. The most commonly described among them are headaches and loss of smell, but strokes, disturbances of consciousness, seizures and leukoencephalopathy (damage to the white matter of the brain) also occur.
Cunning by nature
Coronaviruses (CoVs) are large, enveloped RNA viruses that come in three varieties: alpha coronaviruses, beta coronaviruses, and gamma coronaviruses. They can infect humans, numerous animal species, and typically cause diseases of the upper or lower respiratory tract and gastrointestinal tract. However, some of them also have a special “love” for nervous tissues (tropism), since they also contain the receptors through which the virus can penetrate neurons.
Among all the well-studied coronaviruses that are capable of infecting people, including human coronavirus (HCoV), three types are tropic for nervous tissue: HCoV-229E, HCoV-OC43 and SARS-CoV-1.
The neuroinvasive potential of HCoV-OC43 has been particularly well studied. It thrives in nerve cell cultures in vitro, and not only neurons, but also glia (oligodendrocytes, astrocytes, microglia) are sensitive to it. In mouse models, HCoV-OC43 can enter the central nervous system (CNS) intranasally through olfactory neurons (intranasally) and spread rapidly throughout it. And neuronal damage is caused precisely by direct, virus-mediated, rather than immune-mediated damage.
Clinically, it develops into encephalitis and transient flaccid paralysis, multiple sclerosis (MS), the viral nature of which is demonstrated by the presence of viral RNA in brain tissue at autopsy. Although the mechanism of potential demyelination in HCoV-OC43 is unknown, it may be associated with an adaptive immune response against viral antigens that cross-react with myelin antigens.
During the 2002–2003 SARS pandemic, caused by the SARS-CoV-1 virus, neurological complications were also reported in some patients. A group of researchers from Taiwan reported 3 cases of axonal variant of Guillain-Barré syndrome and 5 cases of ischemic stroke. A clinical case of an epileptic seizure in a patient with a positive result of the cerebrospinal fluid polymerase chain reaction for SARS-CoV-1 was also described. In addition, the virus was detected in the brain tissues of people with SARS at autopsy, especially in the cytoplasm of neurons in the cortex and hypothalamus. In mouse models, SARS-CoV-1 also entered the central nervous system through the olfactory bulb and rapidly spread transsynaptically. The infection caused significant neuronal damage and death without significant inflammatory infiltration.
Middle East Respiratory Syndrome (MERS-CoV) first emerged in 2012, and since then, about 2,494 cases have been reported with a mortality rate of 34.4%. Unlike SARS-CoV-1 and SARS-CoV-2, MERS-CoV binds to the dipeptidyl peptidase 4 receptor in order to enter the cell. This receptor is present in large quantities in epithelial tissues, vascular endothelium and the brain. Accordingly, neurological symptoms in patients included headache, disturbances of consciousness and convulsions, as well as, in severe cases, acute disseminated encephalomyelitis, encephalitis and extensive ischemic strokes. However, the virus itself could not be detected in the human central nervous system.
"Doctor Evil"
The SARS-CoV-2 virus is very similar in structure to SARS-CoV-1. Both viruses have spike proteins on their surface to bind to the angiotensin converting enzyme 2 (ACE2) receptor of mammalian host cells and then use the enzyme (the transmembrane protease TMPRSS2) to enter. The presence of the ACE2 receptor in tissues determines the tropism of the virus. In humans, the receptor is expressed in airway epithelium, kidney cells, small intestine, lung tissue, and vascular endothelium throughout the body, including the central nervous system (although the “sites” in the brain with the most ACE2 are not fully understood).
ACE2 is expressed in both neurons and astrocytes and oligodendrocytes. It is concentrated in the substantia nigra, ventricles, middle temporal gyrus, posterior cingulate gyrus and olfactory bulb. Using cultured neurons, it was shown that ACE2 is expressed both on the surface of the cell membrane and in the cytoplasm. This situation raises concerns that SARS-CoV-2, like SARS-CoV-1, has considerable potential for infecting neurons and glial cells throughout the central nervous system.
However, it is not yet clear whether SARS-CoV-2 can be called neurotropic in humans. The virus can potentially enter the nervous system in several ways: through transsynaptic transfer from diseased to healthy neurons, through the olfactory nerve, through infection of the vascular endothelium, or through the migration of infected leukocytes across the blood-brain barrier.
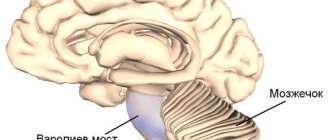
Diagrams of transsynaptic and olfactory propagation pathways. Credit: Adeel S. Zubair et al. / JAMA Neurology 2020
Spread of the virus through the blood-brain barrier (like a Trojan horse). Credit: Adeel S. Zubair et al. / JAMA Neurology 2020
There is not much information about neurological manifestations in patients with COVID-19. The Wuhan study looked at nervous system symptoms in 214 patients hospitalized with confirmed COVID-19. In a French systematic study, neurological symptoms were noted in 49 of 58 patients, which included confusion, encephalopathy and signs of motor corticospinal tract involvement on examination. In addition, they were found to have impaired blood supply to the brain.
The most common neurological symptoms associated with COVID-19, based on frequency of mentions, were headache and loss of taste and smell. Other descriptions included stroke, loss of consciousness, coma, seizures and encephalopathy.
It is possible that SARS-CoV-2, like its closest “relatives,” can penetrate the central nervous system, and potential encephalitis (inflammation of the brain) becomes a big problem in this case. However, there is currently no direct evidence of encephalitis secondary to SARS-CoV-2. A case of meningoencephalitis in a patient with suspected COVID-19 was last reported in Japan. An MRI of a patient with headache, fever and seizures revealed a diffuse increase in signal, indicating edema, in the right temporal lobe, hippocampal atrophy and ventriculitis, and SARS-CoV-2 RNA was detected in the cerebrospinal fluid.
Among severe lesions, authors often report acute vascular events. Patients who developed cerebrovascular flow disorders were significantly older and more prone to complications from COVID-19 due to comorbidity (a combination of different diseases). However, a study conducted in New York showed that younger patients (under 50 years of age) also developed strokes in the great vessels when diagnosed with COVID-19. That is, apparently, vulnerability does not depend on age.
The pathophysiology of the increased risk of acute cerebrovascular disease is likely multifactorial. If we summarize the results of laboratory tests in patients, we can note a significant increase in leukocytes, C-reactive protein, D-dimer, ferritin and lactate dehydrogenase levels. Severe cases were characterized by elevated levels of inflammatory markers and hypercoagulability (increased blood clotting).
Infection of vascular endothelial cells and subsequent vascular damage may also increase the risk of ischemic and hemorrhagic infarctions. By the way, many infections can do this, often “acting” through systemic inflammation, thrombosis or vasculitis. Autopsies of people who died from SARS-CoV-1 often found systemic vasculitis (inflammation of all blood vessels) and venular vasculitis in the brain.
Possible treatment for neurological disorders
There are currently many different drugs being tried to treat patients with COVID-19. Let’s leave their unproven effectiveness aside and talk about their action in relation to the nervous system.
Chloroquine and hydroxychloroquine
Chloroquine and hydroxychloroquine, originally developed as antimalarial drugs, prevent endosomal oxidation, which may stop the virus from entering the CNS via ACE2. But the US Food and Drug Administration (FDA) currently recommends caution when using these drugs due to their potential for cardiotoxicity. Neurological side effects include irritability, psychosis and peripheral neuropathy.
Tocilizumab
Tocilizumab is an anti-IL-6 receptor monoclonal antibody that limits cytokine release in patients with severe inflammatory diseases. There is limited retrospective data suggesting a possible benefit of this drug in COVID-19, as it has limited penetration into the CNS due to the blood-brain barrier. Neurological side effects may include headache and dizziness, and multifocal cerebral thrombotic microangiopathy has been reported rarely.
Remdesivir
Remdesivir is an inhibitor of viral RNA-dependent RNA polymerase. In vitro data showed that it was quite potent in blocking SAR-CoV-2. Early clinical observations also showed some benefit. There is little talk about potential neurological side effects, and clinical trials are currently ongoing.
Text: Anna Horuzhaya
Neuropathogenesis and Neurologic Manifestations of the Coronaviruses in the Age of Coronavirus Disease 2020 by Adeel S. Zubair et al. in JAMA Neurology. Published online May 2020.
doi:10.1001/jamaneurol.2020.2065