Deterioration of vision in many cases requires consultation not only with an ophthalmologist, but also with a neurologist, since neurological pathology is often the cause of vision problems. Specialists from the OkoMed clinic will talk about the connection between vision pathologies and neurological diseases
Peripheral syndromes.
1. Neural (neuritic) syndrome occurs if the trunk of a peripheral nerve is affected, and is characterized by a peripheral (neural) type of sensitivity disorder in the autonomous zone of innervation of a given nerve: anesthesia or hypoesthesia of all types of sensitivity, paresthesia, pain. The latter can be of a varied nature, constant or occur paroxysmally. Paroxysmal pain is mostly characteristic of neuralgia. As is known, most spinal nerves are mixed, therefore, in case of their damage, in addition to sensory disturbances, motor (peripheral paresis of the corresponding muscles) and autonomic-trophic disorders are observed.
2. Polyneuritic syndrome is characterized by multiple lesions of peripheral nerves. Disorders of all types of sensitivity occur symmetrically in the distal parts of the limbs. There is palpation pain in the nerve trunks, loss of reflexes, muscle atrophy and vegetative-trophic disorders.
3. Plexalgic syndrome is observed if the cervical, brachial, lumbar or sacral plexuses are affected. It is characterized by pain, paresthesia, loss of all types of sensitivity, motor and autonomic disorders in the area of those nerves that exit this plexus.
4. Radicular syndrome is caused by damage to the posterior spinal roots and is accompanied by a violation of all types of sensitivity of the segmental type. The area of these disorders is different than in the case of peripheral nerve damage, since the fibers of the dorsal root provide innervation to a specific area of the skin (dermatome). Radicular or segmental zones of sensitive innervation run on the skin of the trunk in circular stripes, and on the limbs in longitudinal stripes. For radicular lesions, pain and paresthesia in the corresponding segments are especially characteristic.
5. Ganglion syndrome occurs when the spinal node is damaged. For this localization of the process, girdle pain with irradiation along the corresponding root is typical. Along with the loss of all types of sensitivity according to the segmental type, a vesicular rash (herpes zoster) appears on the skin of the corresponding dermatome.
Classification of neurological symptoms
Neurological signs by their nature are divided into symptoms of prolapse
and
irritation
.
The study of traumatic brain injury, especially diffuse axonal brain injury, has also allowed us to identify symptoms of disconnection.
Let us present a brief description of the three classes of neurological symptoms.
Symptoms of prolapse are clinical signs of temporary or permanent insufficiency of any brain functions (central paresis of the limbs, aphasia, amnesia, hypalgesia, hemianopsia, etc.). Often found in acute, intermediate, and long-term periods of traumatic brain disease.
Symptoms of irritation are clinical signs of temporary or permanent redundancy of any brain functions (partial and generalized epileptic seizures, hyperesthesia, hyperacusis, hallucinations, trigeminal and meningeal pain, blepharospasm, hyperkinesis, etc.). They are more common in the long-term period of traumatic brain disease; they can be observed in acute and intermediate periods.
Symptoms of disconnection are clinical signs of a functional and/or anatomical disorder of connections between the cerebral cortex and subcortical-stem formations. They are characterized by disinhibition of subcortical, oral-stem formations. They are characterized by disinhibition of subcortical, oral-stem and spinal mechanisms with functional silence of the primarily intact cerebral cortex. Symptoms of dissociation are manifested by a complex of postural and generalized motor reactions, complex pathological reflexes, oral, oculomotor, pupillary and spinal automatisms, paroxysmal vegetative-visceral disorders. Symptoms of disconnection can also be observed in the structure of advanced dislocation and post-dislocation syndromes caused by intracranial hematomas and other volumetric traumatic processes, as well as after cerebral hypoxia, due to post-traumatic cerebrovascular accidents, etc.
Neurological symptoms caused by direct brain damage are classified as primary
, and those caused by brain reactions to damage (edema, dislocation, ischemia, etc.) are classified as
secondary
.
Based on their origin, there are 4 categories of neurological syndromes:
8. cerebral,
9. focal –
hemispheric, craniobasal, cerebellar
,
10. stem,
11. shell
.
General cerebral symptoms are clinical signs of organ damage to the brain. These include states of consciousness, symptoms of intracranial hypertension and hypotension, as well as symptoms caused by hypoxia, ischemia or intoxication of the brain. General cerebral symptoms are more typical for the acute period of TBI. The more severe the brain damage, the longer they last. An increase in ICP usually accompanies compression of the brain, as well as crush lesions, especially in the frontal lobes. Decreased ICP usually accompanies basal skull fractures with nasal or auricular liquorrhea.
The causes of cerebral symptoms are often extracranial injuries (shock due to combined head injury, fat embolism of cerebral vessels, internal bleeding, extensive myocardial infarction, severe lung damage, bilateral pneumonia, acute renal or liver failure, sepsis, gross disturbances of water and electrolyte balance, etc. ). Brain hypoxia often develops as a result of occlusion of the respiratory tract by vomit, saliva, etc. against the background of loss of consciousness at the time of injury.
General cerebral symptoms, which have a meningeal coloration, can be caused by purulent-inflammatory intracranial complications (post-traumatic meningitis, encephalitis, subdural empyema, brain abscesses, etc.).
Post-traumatic hydrocephalus, which occurs as a result of disturbances in cerebrospinal fluid circulation, may also underlie cerebral symptoms.
The development of cerebral symptoms is closely related to the brain’s reactions to TBI – its edema, swelling, and sometimes collapse.
Focal symptoms are clinical signs of local brain damage. Their manifestation and structure are closely dependent on damage to certain brain structures (frontal, temporal, parietal, occipital lobes, subcortical ganglia, cerebellum, brainstem, etc.). Their duration and severity are largely determined by the degree of traumatic destruction of the brain. In the acute period of TBI, focal symptoms (motor, sensory, speech, visual, statically coordinated, etc.) are usually combined with general cerebral symptoms, which often obscure them. In the intermediate and late periods of traumatic brain disease, they often appear in isolation. Focal symptoms underlie the topical diagnosis of TBI and its consequences.
Brain stem symptoms are clinical signs of damage to the brain stem. There are primary symptoms in case of damage to the brain stem at the time of TBI and secondary symptoms - due to dislocation of the brain stem, disorders of its hemodynamics, hypoxia, fat embolism, etc. Depending on the predominant level of pathology, clinical signs of damage to the midbrain, pons or medulla oblongata dominate.
Midbrain syndrome in TBI. The relatively mobile and massive cerebral hemispheres are connected by the relatively thin and less mobile midbrain and subtentorial formations. These topographic conditions are extremely important in TBI. Intense simultaneous acceleration of the brain at the time of injury, directed sagittally, laterally or at any angle, primarily leads to damage to the mesencephalic part of the brainstem. This applies both to the medulla itself and to the vessels supplying the trunk. As a result, one can observe the death of cellular formations and axons (axonal damage), brain edema, hemorrhages - from microscopic extravasators to large (on the scale of the trunk) foci of imbibition of the brain matter and hematomas. Thus, midbrain syndrome is formed.
Global damage to mesencephalic structures is incompatible with life. Therefore, with midbrain syndrome in victims, we are usually talking about either a moderate dysfunction of all midbrain systems, or a predominant lesion of one or another part of the midbrain. In this case, quadrigeminal, tegmental, peduncular syndromes, alternating syndromes affecting the formations of one half of the trunk are distinguished.
Quadrigeminal symptoms include disturbances in upward and downward gaze, vertical ocular distance, convergence disorders, bilateral impairment of pupillary response to light, and vertical, diagonal, or convergent spontaneous nystagmus.
Tegmental (“tegmental”) syndrome includes dysfunction of the III and IV cranial nerves, and only part of the oculomotor nuclei may be affected, which is expressed in paresis of individual muscles. The same symptom complex includes conduction disorders of all types of sensitivity, disturbances of muscle tone due to damage to numerous connections of the red nucleus and the substantia nigra. At the same time, coordination of movements is also disrupted, with “cerebellar” disorders in the limbs contralateral to the side of the tegmental pathology. Increasing damage to tegmental formations leads to decerebrate rigidity syndrome. At the same time, consciousness is impaired, hyperthermia and pathological breathing rhythms may be observed.
The base of the cerebral peduncles consists of the pyramidal and cortical-pontine tracts. Accordingly, peduncular syndrome is represented by contralateral movement disorders, and monoparesis can also be observed, since the somatotopic representation is preserved in the cerebral peduncles.
Midbrain syndrome can develop not only as a result of direct, primary damage to the midbrain, but also secondarily, in the case of dislocations of the formations surrounding it and deformations of the trunk itself. This can be with large hematomas, contusion lesions accompanied by perifocal edema, post-traumatic abscesses, hydrocephalus with a high level of occlusion, hygromas, etc. The participation of midbrain syndrome components in the clinical manifestations of diffuse axonal brain damage is mandatory. Dislocation midbrain syndrome, when compared with a similar bulbar syndrome, has a greater range of symptoms of initial, reversible manifestations and a longer duration of their existence before vitally dangerous and then irreversible processes of damage to the midbrain occur.
Bulbar syndrome is represented by clinical dysfunctions of the medulla oblongata or its individual formations.
Direct damage to the medulla oblongata causes primary bulbar syndrome: dysfunction of the V (segmental type), IX, X, XI, XII cranial nerves, pyramidal symptoms up to and including tetraparesis, disorder of all types of sensitivity, rotatory nystagmus, impaired coordination, statics, gait. Severe damage to all bulbar structures is incompatible with life.
Traumatic compression of the brain, dislocation hydrocephalus lead to the formation of secondary bulbar syndrome as a result of herniation of the cerebellar tonsils into the foramen magnum and compression of the medulla oblongata between them (dorsally) and the anterior edge of the foramen (ventrally). Secondary bulbar syndrome is often characterized by a rapid course. Following the manifestation
Initial reversible symptoms lead to an increase in life-threatening and then irreversible dysfunction of the caudal parts of the brain stem. Dislocation bulbar syndrome includes: pain in the occipital and cervical regions, forced position of the head, paresthesia in the caudal Zelder zones and in the innervation zones of the I-III cervical segments, dysarthria, dysphagia, dysphonia, vomiting, hiccups, bilateral pathological symptoms. Later, bradycardia, increased blood pressure, cyanosis, and acute muscle hypotension appear. Death can occur as a result of sudden cessation of breathing.
Hypothalamic syndromes are frequent components of the clinical manifestations of TBI, expressed in dysregulation of the pituitary-adrenal system, water-electrolyte homeostasis, etc.
In severe TBI, a full-blown hypothalamic syndrome is formed due to direct damage to the hypothalamus: with basal brain contusions, deep massive hemispheric crush lesions and hematomas, accumulation of blood at the base of the brain, hemotamponade of the cerebral ventricles.
With fractures of the base of the skull, direct trauma to the pituitary stalk, chiasm, and gray tuberosity may occur. In this case, sometimes a communication occurs between the cavity of the third ventricle and the basal cisterns. Meningeal and intracerebral hematomas, leading to a ventral displacement of the hypothalamus, can cause circulatory disorders in it, and as a result, the appearance of foci of necrosis. The supraoptic nuclei may be deprived of adequate blood circulation for some time, which can cause transient or persistent diabetes insipidus, combined with central hyperthermia, as well as certain mental disorders. In some cases, in the absence of obvious macroscopic changes, the manifestation of diencephalic pathology is provoked by impaired microcirculation and ischemia of varying severity.
Clinical symptoms of hypothalamic damage in this contingent of victims are formed already in the early stages of TBI: persistent or transient hyperosmolar-hypernatremic disorders (which, in cases resistant to targeted intensive therapy, are complicated by hypovolemia, renal failure), visceral-autonomic disorders; instability of blood pressure and temperature, diffuse disturbances of muscle tone. Direct damage to the hypothalamus can manifest as acute adrenal insufficiency. Against the background of hypothalamic disorders in severe TBI, trophic and septic complications and gastrointestinal bleeding occur.
In the clinic of moderate and mild brain contusions and even concussion, there are sleep-wake disturbances, visceral-vegetative and emotional-affective disorders, episodes of polyuria, transient hyper-hypoosmia.
Victims who have suffered comatose states or brain contusions of varying severity without coma often develop obesity of the adipose-genital type, sleep-wake rhythm disturbances, and other hypothalamic symptoms in the long term after TBI.
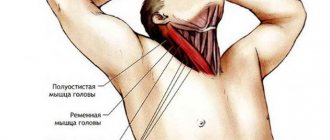
Meningeal symptoms are clinical signs of irritation of the meninges. Two of them are most widely used in the clinic: stiff neck (more precisely, the posterior cervical muscles) and Kernig’s sign (tonic tension of the flexor muscles of the hip and knee joints). In addition, meningeal or meningeal symptoms include: Brudzinski’s symptom (upper, middle, lower), general hyperesthesia, meningeal coloration of headaches, pain on percussion of the head.
The causes of meningeal symptoms in traumatic brain injuries are varied:
- irritation of the soft meninges by subarachnoid hemorrhage;
- irritation of the dura mater by epidural or subdural hematoma or depressed skull fracture;
- irritation of the membranes due to increased brain volume and intracranial hypertension;
- involvement of the meninges in the inflammatory process during purulent complications of TBI - meningitis, post-traumatic encephalitis, subdural empyema, abscess;
- damage to the tonogenic mechanisms of subcortical-stem formations due to injury or dislocation. Often different factors combine.
With subarachnoid hemorrhage and post-traumatic meningitis, neck rigidity and Kernig's sign are usually expressed equally. For intraventricular hematomas, bruises and dislocations of subcortical-trunk formations, dissociation of meningeal Kernig symptoms over stiff neck muscles (or the latter is completely absent) is more typical, which is explained by damage to the mechanisms of regulation of tonic reflexes located here. With hematomas of the posterior cranial fossa, the dissociation of meningeal symptoms along the body axis is characterized by the predominance of nuchal rigidity over the Kernig sign, which is explained by local irritation of the receptors of the V, IX and X pairs of cranial nerves innervating the dura mater subtentorially. The asymmetry of Kernig's symptoms has a certain significance for the lateralization of hemispheric hematomas and crush lesions; its predominance often corresponds to the side of the location of the traumatic substrate.
Spinal syndromes
Spinal syndromes are divided into segmental, conduction and segmental-conduction.
I. Segmental syndromes
1. Posthorn syndrome is characterized by a segmental dissociated type of disorder of pain and temperature sensitivity while maintaining muscle-articular sensitivity in the same area. Violations are always determined from one’s own side and at the level of damaged segments. Damage to the posterior horns may manifest as dull, poorly localized pain. In addition, the corresponding segmental reflexes are lost. Posthorn syndrome is characteristic of the clinical picture of syringomyelia, therefore this type of sensitivity disorder is also called syringomyelitic.
2. The syndrome of damage to the anterior white commissure of the spinal cord, like the previous one, also manifests itself as a segmental dissociated type of disturbance of pain and temperature sensitivity, but its disorders in this case are bilateral and symmetrical, determined 1-2 segments below the pathological focus. When the process is localized at this level, reflexes are preserved, since the integrity of the reflex arc is not violated. This syndrome can be caused by any intramedullary pathological process, but most often it is observed in the presence of syringomyelia, hematomyelia, and intramedullary tumors.
II. Conductor syndromes
1. Lesion syndrome of the lateral cord of the spinal cord is characterized by a conduction-type disturbance of pain and temperature sensitivity on the opposite side. In this case, anesthesia is determined 1-2 segments below the level of damage to the spinal-thalamic tract. This syndrome occurs due to extra- and intramedullary processes of compression genesis. Damage to the lateral cord also causes pyramidal pathology on the side of the lesion as a result of damage to the lateral corticospinal (pyramidal) tract.
2. Syndrome of damage to the posterior cord of the spinal cord is accompanied by complete or partial loss of muscle-articular and vibration sense. Due to the loss of proprioceptive sensitivity, sensitive, or spinal, ataxia occurs, which is determined in the Romberg position and when walking. The exclusion of visual control significantly increases sensory ataxia. It is objectified by bathyanesthesia, pseudoathetosis, and a miss when performing a finger-nose test. Disorders of muscle-articular sensitivity can manifest themselves as afferent paresis, i.e. motor function disorder. Most often, damage to the posterior cords is caused by tabes dorsalis and funicular myelosis.
III. Segmental conduction syndromes
1. Syndrome of transverse lesion of half of the spinal cord (Brown-Séquard syndrome). In this case, on the side of the lesion, disorders of proprioceptive sensitivity and central paresis or paralysis occur downward from the level of the lesion, and on the opposite side pain and temperature sensitivity is lost according to the conduction type. On the side of the lesion, segmental anesthesia of pain and temperature sensitivity in the corresponding dermatomes and movement disorders (peripheral paralysis with areflexia and muscle atrophy) also occur.
2. Extra- and intramedullary syndromes. Extramedullary syndrome begins with a stage of radicular pain and impaired sensitivity at the level of the lesion. Then the clinical picture of Brown-Séquard syndrome is formed. Moreover, due to damage to the lateral fibers of the spinal-thalamic tract, pain and temperature sensitivity disorders spread from bottom to top from the opposite side (ascending type of sensitivity disorder). As the pathological focus grows, conduction anesthesia is combined with radicular anesthesia and results in complete compression syndrome of the spinal cord. Such damage can be caused by spinal tumors and vertebral pathology.
Radicular pain is not typical for intramedullary syndrome. Sensitivity disorders initially have a segmental dissociated nature, and later, due to damage to the spinal-thalamic tract, they are joined by conduction disorders of superficial types of sensitivity, which spread from top to bottom on the opposite side (descending type of sensitivity disorder). As is known, this syndrome can be caused by intramedullary tumors and syringomyelia.
3. Syndrome of damage to the diameter of the spinal cord is characterized by a conduction type of disorder of all types of sensitivity below the level of the lesion. In addition to bilateral loss of sensitivity, lower central paralysis and dysfunction of the pelvic organs simultaneously develop. It is clear that the syndrome of complete transverse lesion of the spinal cord has its own differences and characteristics depending on the level of localization of the pathological process.
Treatment of the disease
As an independent disease, Horner's syndrome is not dangerous. However, its appearance indicates the presence of a pathological process in the body. It should be noted that the idiopathic form of the syndrome can go away on its own and therefore does not require special treatment. An acquired clinical syndrome resulting from a disease, on the contrary, requires careful diagnosis and subsequent treatment therapy. Indeed, despite the fact that the pathology itself does not pose a serious danger to human health, the cause of its development cannot be ignored. Therefore, the basis of treatment for Horner's syndrome is the identification and treatment of the underlying disease.
Bernard-Horner syndrome is treated with medications that are designed to make the nerves and muscles work. Only a specialist can choose the right drug, taking into account the cause of the disease and its duration, as well as the number of symptoms present.
However, there are some methods of treating this disease, which also has a negative cosmetic effect:
- Kinesiotherapy in combination with neurostimulation involves exposing the affected muscles and nerves to current pulses. Electrodes are applied to the skin, sending impulses to nerves, muscle fibers, and blood vessels. Thus, both smooth and striated muscles of the eyeball and its nerves are treated. But only an experienced specialist can carry out this procedure; moreover, it is quite painful and the patient must be warned about this in advance. This leads to active muscle contractions, improved blood supply, lymph circulation and innervation.
- Plastic surgery deals with the correction of pronounced cosmetic defects in Horner's syndrome. Experienced plastic surgeons will help restore the normal shape of the eyelids and palpebral fissure.
Horner's syndrome is a pathological condition that requires careful diagnosis and targeted treatment.
Diagnosis of the disease
To determine the presence and severity of Horner's syndrome, use:
- Cocaine drop test - Cocaine eye drops block the reuptake of norepinephrine, causing the pupil to dilate. Due to a lack of norepinephrine in the synaptic cleft, the pupil will not dilate in Horner's syndrome. Recently, a method has been presented that is more reliable and does not make it difficult to obtain cocaine. It is based on the use of apraclonidine (a sympathomimetic, α2-adrenergic agonist) in both eyes, which leads to the appearance of mydriasis on the side affected by Horner's syndrome.
- Oxamphetamine (paredrin) test. This test helps determine the cause of miosis. If the third neuron (the last of three neurons in the neural pathway that ultimately releases norepinephrine into the synaptic cleft) is intact, then amphetamine causes emptying of the neurotransmitter vesicle, thereby releasing norepinephrine into the synaptic cleft, leading to persistent mydriasis on the affected pupil. If the aforementioned third neuron is damaged, the amphetamine will have no effect and the pupil will remain constricted. However, there is no test to differentiate between damage to the first and second neurons.
- A test to determine the delay time of pupil dilation - determined using the direction of the light beam using, for example, an ophthalmoscope. Anisocoria is observed in Horner's syndrome.
- Magnetic resonance imaging, computed tomography, x-ray examination are used to identify pathological formations that contribute to the development of Horner's syndrome.
- Detailed blood test with leukocyte formula.
- Ultrasound and antiography of the carotid arteries if dissection is suspected (especially in the presence of neck pain).
- For lymphadenopathy, a lymph node biopsy should be performed.
- The duration of Horner's syndrome can be determined by anamnesis. The recent onset of the disease requires a more extensive examination. Horner's syndrome is benign in most cases. History: pain in the head, arm, previous stroke, surgery that could lead to damage to the sympathetic chain (eg, heart, chest, thyroid and neck surgery), head and neck trauma.
- Physical examination - check for enlarged supraclavicular lymph nodes or thyroid gland, or presence of a neck tumor.
It is important to distinguish ptosis caused by Horner's syndrome from ptosis caused by damage to the oculomotor nerve. In the first case, ptosis is combined with a constricted pupil (due to insufficient sympathetic innervation of the eye), in the second case, ptosis is combined with a dilated pupil (due to insufficient innervation of the sphincter of the pupil). In actual clinical work, these two different ptoses are fairly easy to distinguish. In addition to a dilated pupil, when the oculomotor nerve is damaged, ptosis is more severe, sometimes completely closing the entire eye. Ptosis in Horner's syndrome will be moderate or barely noticeable.
If anisocoria (difference in pupil size) is detected, the examiner doubts which of the pupils is dilated and which is narrowed relative to the norm, then in the presence of ptosis, the pathological pupil will be the one located in the same eye as the ptosis.