I pass out when I cough
You can change or supplement the material on the site.
Take care of your health, do not self-medicate. If you suspect any illness, consult your doctor.
For a person far from medicine, classification, in general, does not play any role. Most people in an attack with loss of consciousness, pale skin and falling see fainting, but they cannot be blamed for a mistake. The main thing is to rush to help, and the doctors will figure out what kind of loss of consciousness, so we won’t particularly try to convince the readers.
However, based on the classification, but taking into account the fact that not everyone knows its subtleties, we will try to determine the causes of fainting, which can be both trivial and serious:
- Heat is a different concept for everyone; one person feels tolerable at 40°C, while another feels a disaster, especially in a closed, unventilated room. Perhaps most often, such fainting occurs in crowded transport, where it is difficult to please everyone: some are windy, others feel ill. In addition, there are often other provoking factors (crush, odors).
- Prolonged absence of food or water. Fans of rapid weight loss or people forced to starve for other reasons beyond their control know something about hungry fainting. Syncope can be caused by diarrhea, persistent vomiting, or loss of fluid due to other circumstances (frequent urination, increased sweating).
- A sharp transition from a horizontal position of the body (stood up - everything swam before my eyes).
- Feeling of anxiety accompanied by increased breathing.
- Pregnancy (redistribution of blood flow). Fainting during pregnancy is a common occurrence; moreover, sometimes loss of consciousness is one of the first signs of a woman’s interesting situation. The emotional instability inherent in pregnancy against the background of hormonal changes, heat outside and in the house, fear of gaining an extra kilogram (hunger) provoke a decrease in blood pressure in a woman, which leads to loss of consciousness.
- Pain, shock, food poisoning.
- Nervous shock (why, before telling some terrible news, the person for whom it is intended will be asked to sit down first).
- Rapid blood loss, for example, donors lose consciousness during blood donation not because some volume of precious fluid has been lost, but because it left the bloodstream too quickly and the body did not have time to turn on the defense mechanism.
- The sight of wounds and blood. By the way, men faint from blood more often than women, it turns out that the fair half is somehow more accustomed to it.
- A decrease in circulating blood volume (hypovolemia) due to significant blood loss or due to the use of diuretics and vasodilators.
- A decrease in blood pressure, a vascular crisis, the cause of which may be the uncoordinated work of the parasympathetic and sympathetic parts of the autonomic nervous system, its inability to perform its tasks. Fainting is not uncommon in adolescents suffering from vegetative-vascular dystonia of the hypotonic type or in children in puberty with diagnosed extrasystole. In general, for hypotensive people, fainting is a common thing, so they themselves begin to avoid traveling on public transport, especially in the summer, visiting steam rooms in the bathhouse and any other places with which they have unpleasant memories.
- A drop in blood sugar levels (hypoglycemia) - by the way, is not necessary with an overdose of insulin in patients with diabetes. The “advanced” youth of our time know that this drug can be used for other purposes (increase height and weight, for example), which can be very dangerous (!).
- Anemia or what is popularly called anemia.
- Repeated fainting in children can be evidence of serious illnesses, for example, syncope is often a sign of a heart rhythm disorder, which is quite difficult to recognize in a young child, since, unlike adults, cardiac output is more dependent on heart rate (HR), than from stroke volume.
- The act of swallowing with pathology of the esophagus (a reflex reaction caused by irritation of the vagus nerve).
- Hypocapnia, which causes constriction of cerebral vessels, which is a decrease in carbon dioxide (CO 2) due to increased oxygen consumption during frequent breathing, characteristic of a state of fear, panic, and stress.
- Urination and cough (due to increased intrathoracic pressure, decreased venous return and, accordingly, limited cardiac output and decreased blood pressure).
- Side effect of certain medications or overdose of antihypertensive drugs.
- A decrease in blood supply to certain areas of the brain (ministroke), although rare, can cause fainting in elderly patients.
- Serious cardiovascular pathology (myocardial infarction, subarachnoid hemorrhage, etc.).
- Some endocrine diseases.
- Space-occupying formations in the brain that impede blood flow.
Thus, most often, changes in the circulatory system caused by a drop in blood pressure lead to loss of consciousness. The body simply does not have time to adapt in a short time: the pressure has decreased, the heart has not had time to increase blood output, the blood has not brought enough oxygen to the brain.
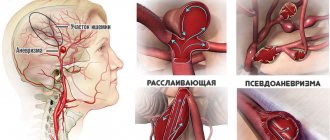
BETTOLEPSIA (Greek betto cough lepsis grasping, attack) is a disorder of consciousness, sometimes combined with convulsions, developing at the height of a cough attack. They are based on disturbances in the blood supply to the brain caused by increased intrathoracic pressure and hyperventilation.
More often observed in patients with pulmonary-cardiac insufficiency (see Cor pulmonale) and venous congestion in the brain (venous encephalopathy).
Even A. Klementovsky (1856) drew attention to the development of venous hyperemia of the brain during convulsive cough. Blue face when coughing I.F. Zion (1873) explained that blood from the veins cannot enter the vessels of the chest.
In children who died from whooping cough, the veins of the brain are dilated and the sinuses are overflowing with blood. Fainting conditions, described as respiratory attacks, occur both during crying and during laughter, especially in children (M. B. Zucker, 1947). Trousseau (A. Trousseau) observed “eclamptic attacks” associated with venous congestion in the brain in patients with whooping cough.
Charcot (J.M. Charcot) also described “laryngeal tabetic crises”, which were noticed by the St. Petersburg doctor Shershevsky back in 1881. We were talking about attacks of coughing with wheezing, during which the patient almost lost consciousness, fell and had epileptiform convulsions. The seizure repeated up to 6 times a day.
The larynx, according to Charcot, is the spasmogenic zone, irritation of which can cause a seizure. The severity of bettolepsy varies, and death is possible. Laryngoscopically, closure of the glottis was observed during the seizure. Charcot also described “laryngeal dizziness” in various diseases.
During a cough, the patient suddenly loses consciousness and falls, but soon comes to his senses. Sometimes epileptiform seizures are observed, which may be limited to one area of the body. Usually the seizure ends quickly without a period of mental disturbances, as with epilepsy.
Gowers (WR Gowers, 1896) described an elderly patient with a severe cough due to chronic bronchitis and emphysema. At the height of the coughing attack, the patient turned purple, short-term general clonic convulsions appeared without loss of consciousness, or the convulsions were of an epileptoid nature, or loss of consciousness occurred without convulsions. Govere describes this observation without connection with laryngeal spasm in the chapter on cerebral hyperemia.
In works of more recent times, there is almost no mention of impaired consciousness during coughing. By 1949, only 177 patients with cough-like syncope had been described. N.K. Bogolepov (1971) describes respiratory-cerebral epileptic seizures in patients with bronchial asthma and neuralgia of the superior laryngeal nerve, distinguishing between comatose and algic forms of bettolepsy.
M.I. Kholodenko (1941, 1963), who proposed the term “bettolepsy,” observed over 100 patients with this syndrome.
Fainting while coughing or simply after a coughing attack. Fainting is usually associated with severe and prolonged episodes of coughing. This disorder is much more common in adult men. Cough stimulates the autonomic reflexes of the nervous system. These reflexes connect the brain, heart and respiratory system.
article in PDF format
Tilt-test (passive orthostatic test) is a test with orthostatic load, which is aimed at identifying the connection between existing syncope and changes in blood pressure and cardiac activity. To conduct a tilt test, the patient is fixed on a special table, which is transferred from a horizontal to a vertical position with varying degrees of intensity to provoke fainting.
Therapy. A correctly conducted diagnostic search is the cornerstone of successful treatment of CS (while CS developing against the background of chronic bronchopulmonary diseases are quite benign, detection of cardiac pathology is associated with a worse prognosis). A decrease in relapses of syncope up to complete disappearance against the background of improvement in the clinical picture of the underlying disease is a characteristic feature of CS.
Of great importance is the elimination of the causes that directly cause cough, for example, smoking, the prescription of antitussives, and complex treatment of bronchopulmonary diseases. The role of normalizing the patient’s body weight when it is excessive is shown. The prognosis for CS depends on the underlying disease.
True causes and provoking factors
Factors that provoke cough fainting should also include some habits and features of life in the form of:
- wearing tight-fitting clothing;
- habits of quickly changing posture (with sudden jumping up after prolonged sitting);
- "passive smoking";
- tendency to anxious and suspicious, “psychically suffocating” states.
Hypoxia—oxygen starvation of tissues, in this particular case of the brain, is caused by any relatively long-term condition accompanied by:
- or a mechanical obstruction to breathing - the flow of oxygen;
- or caused by a lack of oxygen in the blood for another reason (defect of red blood cells in some anemias, for example).
In the variant of bettolepsy, these two factors in the development of hypoxia are combined. This is a mechanical obstruction of the airways damaged by acute or chronic pathology, and a prolonged period of circulation of oxygen-poor blood.
Time measured in minutes. Time that may be sufficient for the onset of irreversible changes in the brain.
Let us add to this basis what has developed over the years, but at an earlier age, coughing syncope does not develop - atherosclerotic degeneration of blood vessels, which in itself is the cause of chronic hypoxia. As well as associated episodes of excessive blood pressure. And also arrhythmia - momentary or permanent.
It is worth adding two more strokes to the canvas, adding the following to the causes of bettolepsy:
- endocrine pathology in the form of diabetes mellitus;
- chronic allergies to everything, which developed, among other things, as a result of excessive addiction to taking medications.
Anyone who has all these treasures of dubious value has an unusually high risk of developing cough epilepsy.
But... not everyone faints with a cough! And only 2% of adults experience various types of paroxysmal conditions! And children never suffer from this disease (with the exception of cases where whooping cough serves as a background).
For the development of cough fainting, one more condition is necessary - the presence of pathological impulses from reflexogenic zones:
- respiratory system;
- larynx (in particular, the areas of activity of the superior laryngeal nerve);
- carotid sinus, jugular veins, aorta;
- venous sinuses of the brain.
The reaction from the pressoreceptors located in these reflexogenic zones is a necessary link that closes the fatal chain - pathological impulses from them lead to an increase in the activity of the vagus nerve, contribute to the onset of bradycardia and the manifestation of a dangerous condition - Morgagni-Adams-Stokes syndrome.
Fainting is not a separate disease or diagnosis; it is a short-term loss of consciousness due to an acute decrease in blood supply to the brain, accompanied by a drop in cardiovascular activity.
Fainting or syncope, as it is called, occurs suddenly and usually does not last long - a few seconds. Absolutely healthy people are not immune from fainting, that is, one should not rush to interpret it as a sign of a serious illness; it is better to try to understand the classification and causes.
Pathogenesis
The pathogenesis of bettolepsy is not fully understood. Typically, paroxysmal conditions that occur at the height of the cough reflex have nothing to do with epilepsy. The hemodynamic theory explains most fully the changes that occur during coughing. There are three phases of cough: inspiratory, compressive and expiratory. In the compressive and expiratory phases, intrathoracic and intra-abdominal pressure increases sharply, resulting in a decrease in blood flow to the heart. This leads to a decrease in cardiac output and changes in cerebrospinal fluid pressure in the brain and spinal cord. As a result of a sharp increase in intrathoracic pressure, it increases in the peripheral arteries, veins and chambers of the heart, which leads to venous stagnation and causes bettolepsy.
There are other development mechanisms: stimulation of vagus nerve receptors, transmission of pathological impulses from reflexogenic areas of the respiratory tract and jugular veins. This kind of influence leads to changes in the functioning of the reticular formation, which is fraught with vasodepressor reactions and severe bradycardia with impaired consciousness.
Clinical manifestations
Clinical manifestations of bettolepsy can be of several variants: 1) short-term twilight consciousness that occurs during coughing; 2) fainting when coughing; 3) deep loss of consciousness combined with muscle cramps during coughing, and sometimes urinary and fecal incontinence.
The course and outcome of bettolepsy depend mainly on the general somatic condition of the patient. In patients with chronic cerebral circulatory insufficiency due to atherosclerosis or hypertension, an attack of bettolepsy can lead to structural damage to the brain with lasting consequences.
Clinical manifestations of bettolepsy can be of several variants: 1) short-term twilight consciousness that occurs during coughing; 2) fainting when coughing; 3) deep loss of consciousness combined with muscle cramps during coughing, and sometimes urinary and fecal incontinence.
Symptoms and clinic
A typical picture that precedes coughing fainting is purple discoloration of the skin of the face and visible parts of the upper half of the victim’s body at the peak of a coughing attack, with swelling of the veins overflowing with stagnant blood due to strain, followed by cyanosis.
Then fainting occurs - the body, without any “preliminary explanation,” falls to the floor.
The further fate of a person depends on the duration of fainting. But in any case, the victim’s skin turns pale, and in an unconscious state, suffocation stops along with coughing.
Depending on the depth of cerebral hypoxia that has developed, the following may occur:
- rapid return to consciousness (with the duration of fainting from seconds to a minute);
- the return to consciousness is longer, with the development of short-term tonic convulsions in the form of twitching of the limbs and a drop in the tone of the pelvic organs with incontinence of feces and urine.
The consequences of cough syncope depend on the severity of the somatic pathology predisposing to the development of bettolepsy - with deep-seated changes, damage to thin brain structures that are especially sensitive to hypoxia and fluctuations in the level of blood pressure and cerebrospinal fluid in the corresponding systems is possible.
Then it comes - the body, without any “preliminary explanation,” falls to the floor.
- rapid return to consciousness (with the duration of fainting from seconds to a minute);
- the return to consciousness is longer, with the development of short-term tonic in the form of twitching of the limbs and a drop in the tone of the pelvic organs with incontinence of feces and urine.
It is possible to have epileptiform convulsions in one of the areas of the body, as well as short-term “twilight” of consciousness during coughing suffocation without falling to the ground (on the floor), while maintaining the original position of the body.
Symptoms
The clinical picture of bettolepsy is variable in severity not only in different patients, but also in one patient during different attacks.
Typically, an attack of coughing syncope is accompanied by the following symptoms:
- a coughing attack occurs while standing or sitting, while eating or immediately after eating;
- cough can be triggered by strong odors, cold air, excessive laughter, frequent sneezing, defecation, heavy lifting, or tobacco smoke;
- against the background of a cough, the patient’s face turns red and then turns blue, veins swell in the neck;
- sometimes a harbinger of an attack can be a lung that occurs against the background of a cough;
- in the first minute of a cough attack, signs of fainting appear or loss of consciousness occurs, accompanied by a fall of the patient and cyanosis of the skin;
- after fainting, the skin becomes pale and the cough stops;
- the duration of fainting is several seconds or minutes;
- after this, the patient quickly returns to consciousness and recovers from the seizure (usually without medical assistance).
In some cases, an attack of coughing syncope is accompanied by convulsions, which are usually limited to one part of the body (for example, twitching in the limbs). Tongue biting is not observed during convulsions caused by bettolepsy. In rare cases, a seizure may lead to urinary or fecal incontinence.
During an episode of bettolepsy, the patient may sometimes experience the following symptoms:
- amnesia;
- headache;
- pain in the neck area.
Some experts identify the following variants of cough-brain syndrome:
- A seizure develops at the peak of coughing and is accompanied by sudden deep fainting and a fall of the patient.
- The seizure is accompanied by convulsions and, sometimes, involuntary bowel movements or urination.
- The seizures initially occur as in bettolepsy, and then are replaced by petit epileptic seizures, which can develop independently of the cough.
- Seizures of bettolepsy in patients with organic brain pathologies, accompanied by severe autonomic disorders.
- Seizures of bettolepsy in patients with a history of typical epilepsy.
What is bettolepsy, how is it treated and what are its consequences?
Despite the opinion of many, bettolepsy (cough-brain syndrome, cough fainting) has nothing in common with epilepsy, it is worth paying attention to this part of the word: -lepsy translated from ancient Greek means “grasp” or “tightness”.
But doesn’t the brain have to fight, unclenching the tight embrace of hypoxia? A deadly embrace in a fight to the death where lives are at stake? And in both cases?
Therefore, before repeating what others have said, you should think at least twice.
How to diagnose the disease
If similar symptoms are detected, the patient should consult a family doctor or neurologist. To make a diagnosis, you need to carefully collect anamnesis, study the medical history and draw up the correct examination plan. It is important to differentiate bettolepsy from similar diseases, for example, epilepsy.
To determine brain-cough syndrome, the following examination methods are used:
- Holter monitoring – recording of a cardiogram during the day. Allows you to evaluate the work of the heart in the body’s usual conditions, as well as the reaction to various situations. Helps determine the cause of loss of consciousness.
- Tracheobronchoscopy is an endoscopic examination of the respiratory tract. The condition of the mucous membrane, the presence of foreign bodies, and the diameter of the bronchial lumens are determined.
- Valsalva maneuver - helps to assess the state of the autonomic nervous system. The patient should exhale all the air, then inhale deeply and exhale again, holding the breath for at least 15 seconds.
- ECG.
- ECHO-KG.
To make a diagnosis, hospitalization in an inpatient department is not always necessary. Most often, the patient comes for examinations. The exception is severe cough fainting with severe convulsions. In this case, the patient may be referred to a specialized epileptology center to clarify the disease.
Diagnostic criteria and research methods
Since it is possible for a bettolepsy seizure to smoothly flow into a petit mal seizure, the treating neurologist needs to know exactly what pathology he is dealing with.
Therefore, important diagnostic criteria are the onset of cough syncope:
- without warning signs;
- during a coughing attack - in the first minute;
- absence of biting the tongue and secretion of foamy saliva from the mouth, as well as subsequent falling asleep characteristic of epilepsy.
To establish a true diagnosis, the previous actions of the person suffering from attacks are important - in the form of eating, defecation, excessive laughter-gelolepsy, as well as the influence of cold air and tobacco smoke on him. His age (mature or even older), as well as the presence of respiratory and vascular disorders, is important.
In addition to performing the Valsalva maneuver, the effect of using instrumental methods for studying the state of the nervous system and the body as a whole should be noted:
- EEG;
- ECG, EchoCG and Holter monitoring;
- blood pressure monitoring;
- X-ray and other methods for detecting respiratory pathology.
If necessary, an inpatient examination is carried out, including in cases of difficulty, in an epileptology center.
- ECG, EchoCG and Holter monitoring;
- blood pressure monitoring;
- X-ray and other methods for detecting respiratory pathology.
- without warning signs;
- during a coughing attack - in the first minute;
- absence of biting the tongue and secretion of foamy saliva from the mouth, as well as the characteristic subsequent fall asleep.
Diagnostics
If attacks of bettolepsy occur, the patient must contact his local doctor, who will refer him for a consultation with a neurologist. To make a diagnosis, a detailed analysis of the patient’s medical history and life is carried out, the nature of the attacks is carefully studied and an examination plan is drawn up, which allows one to identify the cause of coughing fainting and carry out a differential diagnosis of bettolepsy with other diseases (for example, epilepsy).
To identify cough-brain syndrome, the following types of examinations may be prescribed:
- Valsalva maneuver;
- Holter monitoring;
- measurement ;
- electrophysiological methods of intracardiac stimulation, etc.
In some cases, patients are advised to undergo tracheobronchoscopy.
The need for hospitalization of a patient in a hospital for examination and treatment is determined individually and depends on the possibility of identifying the causes of the development of bettolepsy in an outpatient treatment facility and the severity of the attacks. Sometimes, if the cause of consciousness disorders is unclear, the patient is advised to undergo examination at a specialized epileptological center.
Do you need help with cough fainting?
Usually, treatment for betolepsy as such is not carried out; assistance is provided only at the time of the attack. However, everything depends on the patient’s previous condition and the depth of his fainting.
Those present during a seizure, in order to quickly bring a person to his senses, can apply rubbing ammonia to the temples and take measures to inhale its vapors to the fainting person; Another strong-smelling substance (vinegar) can be used with the same success.
It is necessary to ensure a flow of fresh air, as well as take measures to remove a foreign body stuck within the pharynx.
If necessary, the method of forced ventilation of the lungs is used - the method of artificial respiration.
The rest is a task for the “emergency aid” team; when a seizure begins, it must be called immediately. For, after familiarization with the situation, only its employees can use injections of cardiotonic and vasoconstrictor drugs: Ephedrine, Mezatone, and for bradycardia - Atropine sulfate.
In all cases of the first attack of bettalepsia, hospitalization for diagnostic purposes is required, and further treatment of the underlying pathology is necessary under the supervision of the treating specialist: therapist, neurologist, cardiologist.
This section was created to take care of those who need a qualified specialist, without disturbing the usual rhythm of their own lives.
Bettolepsy is a transient disturbance of consciousness that occurs at the peak of a coughing attack. The main manifestation of the syndrome is cough syncope: short-term twilight consciousness, fainting, deep loss of consciousness, in some cases accompanied by convulsions, involuntary defecation and urination.
This is a rather rare pathological condition, which is also called cough-brain syndrome, cough syncope, laryngeal dizziness, cough syncope, respiratory attack. It is more often detected in men over 45 years of age, and is especially common among patients with pulmonary heart failure.
How does bettolepsy manifest?
The severity of bettolepsy symptoms may vary not only between different patients, but also within the same patient at different times. The disease attacks mainly older men; it can develop in children due to a cough, the cause of which is whooping cough. There are several variants of a cough-brain attack:
- The attack occurs at the peak of a strong cough. The patient loses consciousness and falls.
- Bettolepsy develops into epileptic seizures. They can already occur without a cough.
- Attacks that are accompanied by profound disturbances in the autonomic nervous system. Most often they occur in people with brain pathologies.
- Loss of consciousness is accompanied by convulsions, involuntary urination and defecation.
- History of seizures in patients with epilepsy.
Sometimes you can recognize the onset of bettolepsy and prevent the patient from falling:
- the face acquires a red and then bluish tint;
- lips become purple;
- the neck veins swell and pulsate greatly;
- the patient complains of dizziness.
Usually, loss of consciousness occurs before the end of the first minute of the attack, the patient stops coughing, falls and suddenly turns pale. If the patient does not have severe concomitant diseases, then consciousness resumes after a few minutes or even seconds. Most often, such patients do not require medical care.
After bettolepsy, memory disorders (amnesia), unpleasant, painful sensations in the neck, and headaches occur. Since an attack does not develop without an intense cough, it is important to know the factors that cause coughing:
- strong, prolonged laughter;
- inhalation of cold or hot air;
- sneeze;
- cigarette smoke or other irritating odors;
- smoking;
- lifting something heavy;
- the act of defecation during constipation.
What is bettolepsy, how is it treated and what are its consequences?
BETTOLEPSIA (Greek betto cough lepsis grasping, attack) is a disorder of consciousness, sometimes combined with convulsions, developing at the height of a cough attack. They are based on disturbances in the blood supply to the brain caused by increased intrathoracic pressure and hyperventilation. More often observed in patients with pulmonary-cardiac insufficiency (see Cor pulmonale) and venous congestion in the brain (venous encephalopathy).
Treatment for bettolepsy, like most other diseases, is aimed at getting rid of the cause of the attacks. Therefore, it is prescribed individually after a thorough examination. After an attack, symptomatic therapy is carried out using:
- ammonia;
- cardiotonic drugs;
- saturating the body with oxygen;
- vasoconstrictor medications;
- for severe bradycardia - atropine.
Read why oxygen starvation of the brain leads to loss of consciousness. Diagnosis, treatment and consequences of hypoxia.
Consequences of the disease
Bettolepsy is a fairly rare phenomenon. This diagnosis is made in approximately 2% of patients who present with similar complaints. Usually attacks do not lead to serious consequences. But this is not a reason to ignore the symptoms and not see a doctor. Since sometimes disturbances in the brain can occur, and with mild seizures, the patient can simply suffer from a fall.
The prognosis is generally favorable. Most often, it is enough to cure the provoking disease, and if this is not possible, then avoid severe coughing attacks. To do this, use antitussive drugs or, for example, breathing exercises.
The tactics for treating and preventing syncope depend on the cause of fainting. And these are not always medications. For example, with vasovagal and orthostatic reactions, the patient is first of all taught to avoid situations that provoke syncope. To do this, it is recommended to train vascular tone, carry out hardening procedures, avoid stuffy rooms, sudden changes in body position, men are advised to switch to urination while sitting. Usually, individual points are discussed with the attending physician, who takes into account the origin of the attacks.
Fainting caused by a drop in blood pressure is treated by increasing blood pressure, also depending on the cause of its decrease. Most often, this cause is neurocirculatory dystonia, so drugs that affect the autonomic nervous system are used.
Recurrent fainting, which may be of arrhythmogenic nature, deserves special attention. It should be borne in mind that they are the ones who increase the likelihood of sudden death, therefore, in such cases, arrhythmia and the diseases that cause it are treated in the most serious way.
It is impossible to say unambiguously about fainting states: they are harmless or dangerous. Until the cause is clarified, and attacks continue to bother the patient every now and then, the prognosis can be very different (even extremely unfavorable), because it completely depends on the nature of this condition. How high the risk is will be determined by a thorough history and a comprehensive physical examination, which can be the first step towards forever forgetting about this unpleasant “surprise” that can make a person lose consciousness at the most inopportune moment.
Consequences of the disease
Treatment
The main goal of treatment for bettolepsy is always aimed at treating the underlying disease that caused the development of cough syncope. An action plan is drawn up individually after all necessary examinations have been carried out.
During and after an attack of coughing syncope, symptomatic therapy is carried out, aimed at alleviating the patient’s condition. It may involve the use of the following means:
- ammonia;
- oxygen therapy;
- improving bronchial patency and antitussives;
- cardiotonic drugs;
- vasoconstrictors: Ephedrine, Mezaton;
- administration of Atropine sulfate (for bradycardia).
Cough fainting often frightens the patient and those around him. Their appearance should always be a reason to consult a doctor and conduct a comprehensive examination and treatment of the underlying disease that triggered the development of bettolepsy.
Be careful about your health and don’t put off visiting a specialist! Even a fall that accompanies loss of consciousness can cause serious injuries, and in some diseases, coughing fainting causes structural damage to brain tissue and irreversible complications. Remember this and be healthy!
- (gr. betto - cough) - a term proposed by M.I.
Kholodenko (1941) for paroxysmal conditions that occur at the height of coughing and are characterized by impaired consciousness, sometimes tonic convulsions. In most cases, paroxysms during coughing are not related to epilepsy, since they develop according to pathogenetic mechanisms characteristic of fainting states.
Venous stasis is not, apparently, the main factor in the development of disorders of consciousness when coughing.
Brain hypoxia
, which occurs with a prolonged cough, is caused by an increase in intrapleural pressure, a violation of venous blood flow in the superior vena cava system, a slowdown in pulmonary blood flow with an increase in intrapleural pressure, a decrease in the filling of the left ventricle with blood, a slowdown in cardiac activity, and a decrease in cardiac output.
Also important is the afferent impulse that occurs in the receptors of the respiratory tract during coughing and irritation of the receptors of the sinocarotid and aortic reflexogenic zones in connection with coughing movements.
Cases of cough
“
fainting
(bettolepsy) is quite rare and accounts for no more than 2% among patients with various types of paroxysmal conditions.
Classification
1. Short-term twilight disorder of consciousness. Usually lasts a few seconds and does not require emergency treatment. In this case, the underlying disease that caused the condition should be treated.
2. Short fainting at the height of coughing. Most often it lasts from 2 to 10 seconds. Treatment of the underlying pathology is necessary.
3. Prolonged loss of consciousness. Complicated by convulsions, involuntary urination, defecation. Often combined with organic brain damage with lasting consequences. Aggravating factors include alcohol, nicotine intoxication, and drug poisoning.
- Short-term twilight disorder of consciousness. Usually lasts a few seconds and does not require emergency treatment. In this case, the underlying disease that caused the condition should be treated.
- Brief fainting at the height of coughing. Most often it lasts from 2 to 10 seconds. Treatment of the underlying pathology is necessary.
- Prolonged loss of consciousness. Complicated by convulsions, involuntary urination, defecation. Often combined with organic brain damage with lasting consequences. Aggravating factors include alcohol, nicotine intoxication, and drug poisoning.
True fainting includes attacks of short-term loss of consciousness, which can be divided into the following types:
- The neurocardiogenic (neurotransmitter) form includes several clinical syndromes, and is therefore considered a collective term. The formation of neurotransmitter fainting is based on the reflex effect of the autonomic nervous system on vascular tone and heart rate, provoked by factors unfavorable for a given organism (ambient temperature, psycho-emotional stress, fear, type of blood). Fainting in children (in the absence of any significant pathological changes in the heart and blood vessels) or in adolescents during the period of hormonal changes often has a neurocardiogenic origin. This type of syncope also includes vasovagal and reflex reactions that can occur during coughing, urination, swallowing, physical activity and other circumstances not related to cardiac pathology.
- Orthostatic collapse or fainting develops due to a slowdown in blood flow in the brain during a sudden transition of the body from a horizontal to a vertical position.
- Arrhythmogenic syncope. This option is the most dangerous. It is caused by the formation of morphological changes in the heart and blood vessels.
- Loss of consciousness, which is based on cerebrovascular disorders (changes in cerebral vessels, cerebrovascular accident).
Meanwhile, some conditions called fainting are not classified as syncope, although they look very similar to it. These include:
- Loss of consciousness associated with metabolic disorders (hypoglycemia - a drop in blood glucose, oxygen starvation, hyperventilation with a decrease in carbon dioxide concentration).
- Epilepsy attack.
- TIA (transient ischemic attack) of vertebrogenic origin.
There is a group of disorders that resemble fainting, but occur without loss of consciousness:
- Short-term muscle relaxation (cataplexy), as a result of which a person cannot maintain balance and falls;
- Sudden onset of movement coordination disorder – acute ataxia;
- Syncopal states of psychogenic nature;
- TIA caused by impaired blood circulation in the carotid system, accompanied by loss of ability to move.
The most common case
Fainting of this kind in children and adolescents causes a lot of anxiety on the part of parents, who cannot be reassured only by the fact that such a condition is not a consequence of a serious pathology. Repeated fainting is accompanied by injury, which reduces the quality of life and can be dangerous in general.
1. Short-term twilight disorder of consciousness. Usually lasts a few seconds and does not require emergency treatment. In this case, the underlying disease that caused the condition should be treated.
Why does an attack occur?
The origin of bettolepsy is related to:
- with incorrect impulses that come from the nerves to the cough center;
- with pathological perception of information in the reflex zones of the respiratory tract.
This leads to disturbances in the autonomic nervous system and excitation of the tenth pair of cranial nerves (vagus), causing severe bradycardia.
During intense coughing, hyperventilation of the lungs occurs and intrathoracic pressure increases. Because of this, cerebral circulation is disrupted and various disorders occur: short-term loss of consciousness, convulsions, amnesia, severe headache.
Read about the causes of sudden loss of consciousness and first aid for the victim.
How cerebral vasoconstriction manifests itself: symptoms and complications of severe vascular spasm.
There is only one provoking factor – cough. But there can be many risks:
- diseases of the lungs and bronchi - tuberculosis, asthma, emphysema, chronic bronchitis, whooping cough;
- foreign body entering the respiratory tract;
- inflammation of the laryngeal nerve;
- pathologies of cerebral vessels - atherosclerosis, compression of the arteries due to osteochondrosis;
- alcohol and tobacco abuse;
- diseases of the cardiovascular system - cor pulmonale, venous stagnation of blood;
- unhealthy diet, unhealthy lifestyle.
It is extremely important to know the cause of the development of bettolepsy, since the severity of the attack and treatment largely depend on this.