Neurofibroma is a benign neoplasm that develops from nervous tissue in the peripheral nervous system. The frequency of occurrence in children and adults is the same - approximately one person per 4 thousand population. Usually the tumor is localized under the skin, where the nerve fiber passes. The disease is a multiple neoplasm.
Macroscopically, the tumor appears as a dense, tuberous node, the size of which varies from 1 mm to 2-3 cm. On a section, the neurofibroma is brown or pinkish in color. The tumor inside may contain small cysts.
Cutaneous neurofibroma clinic
Depending on the location of the formations and the clinical picture of their development, neurofibromas can be divided into two forms:
• neurofibroma of the skin, which is a peripheral form of the disease and manifests itself as a tumor of the skin and subcutaneous layer of tissue along the passage of the nerve, has several varieties in the form of Schwannoma, neuroma and plexiform neurofibroma;
• Another form of the disease, called central, is neurofibromas, which affect the nerve roots of the spinal cord and brain, having the ability to grow into them. In terms of their cellular composition, tumors of this type are the same as neuroma, neurofibroma, meninginoma and other neoplasms.
Course of the disease
Neurofibromatosis progresses very slowly. However, rather long periods of stability without the appearance of new formations and active growth of existing tumors can, under the influence of environmental factors, as well as changes in hormonal levels in adolescence, be replaced by rapid growth.
When to visit a specialist
Often, neurofibroma of the skin, due to its similarity with other formations, is mistakenly identified by the patient independently. Therefore, in a number of certain cases, an accurate diagnosis is necessary, for which you should definitely visit a specialist. After all, as with any other disease, identifying it in the early stages and timely initiation of treatment can significantly reduce the harmful impact of the disease on all systems of the body.
Thus, it is necessary to contact a medical institution in the following situations:
- when pregnancy is planned;
- if neoplasms are palpated in the places where the nerve passes in the subcutaneous layers;
- if pigmentation is noticed on the surface of the skin in the form of spots measuring at least five millimeters, the color of which varies in the beige-brown range;
- when spotty pigmentation of a coffee-milk color appears in the pits under the knee, under the armpit or in the groin area;
- hearing or vision is impaired or tinnitus appears;
- Balance problems arose, and I began to feel dizzy often.
Diagnostic measures
During a medical examination, in the vast majority of cases, skin neurofibroma is identified accurately. However, situations arise when the issue may be controversial and additional examination of a potential patient will be required. For this, the patient is referred to an eye doctor to examine the iris of the eye in order to identify the symptoms of the disease. To determine disorders of the skeletal system, it is advisable to prescribe an x-ray.
Therapeutic measures
Unfortunately, doctors cannot yet offer a complete cure for neurofibromatosis. However, it is quite possible to reduce the size of the tumor by using radiation therapy or removing the largest formations with a scalpel, which is a fairly effective measure in the fight against the progression of the disease. Considering the heredity of the disease, it would not be amiss to get advice from a genetics specialist before planning the birth of a baby.
What types of spots are there?
What is a stain? This is a part of the skin that differs in color. Tactilely, it is either smooth or has a small protrusion above the surface and is rough.
Spots can be divided into several groups:
- vascular - acquire a pink, red, purple color;
- pigment - brown and white colors;
- artificial - tattoos and permanent;
- lichen, etc.
Vascular spots
- Hyperemic caused by:
- inflammation in the body when blood vessels dilate. The spots can be in the form of roseola up to two cm or erythema - more than 2 cm;
- non-inflammatory etiology - often called spots of anger or shame. Caused by hyperemic vascular disorders during an emotional reaction. Places of occurrence: face, neck, chest.
- Hemorrhagic. Such spots appear due to mechanical stress, or are a sign of a disease affecting the vascular system.
A bruise or contusion goes away on its own within 10-14 days, and during this time the color changes from red to yellow, green.
Other manifestations need to be taken more seriously, since they generally require treatment.
3.Telangiectatic. The reason is telangiectasia or, more simply, asterisks that appear due to dilation of blood vessels.
Such formations are divided into 2 groups - congenital and acquired. The causes of the occurrence are different - from poor nutrition, bad habits, to serious problems with the cardiovascular system and gastrointestinal tract.
Pigmentation
The spots appear as dark or bright white patches of skin.
They are formed due to an increase or decrease in the amount of melanin pigment. Divided into:
- Hyperpigmented. Often they are congenital in nature - lentigo or birthmark. But they can be acquired - freckles, melasma. Characterized by increased pigmentation on the skin.
- Hypopigmented. On the contrary, they appear due to a lack of melanin pigment. They can also be congenital or acquired as a consequence of diseases - lichen, leucoderma, eczema, psoriasis.
- Moles.
Ringworm is a common skin disease. The cause is bacteria or viruses. The disease is characterized by changes in skin color, itching and pain. At the same time, immunity decreases.
Lichen spots can be of several types:
- Zhiber's lichen is pink or red in color with clear edges. The spot is flaky and itchy. The cause of the disease is the herpes virus of the sixth and seventh types;
- shingles - manifested by the appearance of red, inflamed spots with blisters;
- ringing - accompanied by itching, severe peeling, hair loss in the sore spot;
- pityriasis - damaged skin becomes pale and flaky;
- lichen planus - the spots become purple in color and spread not only on the surface of the skin, but also on the mucous membranes.
Red spots
Almost every person has experienced the appearance of red spots on the skin.
The reason for their occurrence may be:
- allergic reactions to foods, medications, household chemicals, ultraviolet radiation;
- skin diseases - dermatitis, etc.;
- avitaminosis;
- decreased immunity;
- infection - chickenpox, measles, scarlet fever;
- sexually transmitted diseases;
- stress.
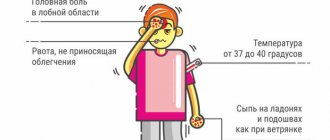
It is important to monitor your body temperature when red spots appear. If fever, sore throat, peeling, itching and burning begin, then you should definitely visit a dermatologist as soon as possible.
Light spots
Sometimes white spots appear on the skin; they may be slightly lighter than the skin and are most often temporary. Causes include abrasions, cuts, and skin infections.
However, sometimes such spots serve as a signal for more serious reasons - stress, chronic diseases, infections, burns of various etiologies.
Reasons for the development of the disease
In approximately half of cases, neurofibromatosis is inherited; in the remaining patients, the cause of the disease is a gene mutation.
Neurofibromatosis is classified as a group of diseases with a high degree of penetrance, that is, all people who are carriers of the pathological gene are considered sick.
However, the manifestations of neurofibromatosis are highly variable. That is, in the presence of a pathological gene, both minimally expressed symptoms and quite severe clinical cases can be observed.
If one of the parents has neurofibromatosis, the probability of transmitting the pathological gene to the offspring is 50%. If both parents are sick, the probability increases to 66.7%.
Macroscopy
Microscopically, the formation sometimes reaches large sizes and has a lobular structure. The examination reveals a well-defined capsule, in some cases it is completely absent. In relation to the nerve, it can be located either singly or multiple times.
If we talk about plexiform neuroma, then in this case we are talking about the fact that the tumor began to grow inside the nerve trunk, which leads to its thickening and further deformation. Microscopically, the formation consists of its own cells and connective tissue, and the ratio of both can be very different.
Can a neuroma become a malignant tumor? This happens relatively rarely and most often the disease lasts for a long time as benign.
Clinical picture
For most patients, the first symptoms of neurofibromatosis appear in childhood. The disease begins with the appearance of a large number of pigment spots, as well as tumor-like formations - neurofibromas.
The spots are multiple, have a smooth surface and a characteristic “coffee with milk” color. The spots are localized in large folds on the body. As neurofibromatosis progresses, the number of spots increases.
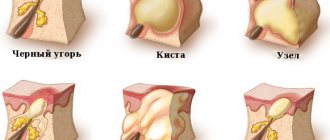
The second characteristic symptom is the appearance of neurofibromas. These are cutaneous or subcutaneous hernia-like protrusions that can grow up to several centimeters in diameter. Neurofibromas are painless; upon palpation, the fingers seem to fall into the void (this sign is called the “doorbell button” phenomenon). The color of neurofibromas is unchanged, sometimes the skin acquires a brown or pink-blue tint. The majority of neurofibromas are located on the torso, but tumors can appear anywhere, including on the face.
Sometimes diffuse neurofibromatosis develops, which is characterized by excessive proliferation of connective tissue and subcutaneous tissue. As a result, giant neurofibromas appear.
Multiple neurofibromas can appear not only on the skin, but also in the oral cavity, inside the skull and in the area of the spinal roots. Neurofibromatosis is often combined with various pathologies of the musculoskeletal system, endocrine, nervous and cardiovascular systems.
Forms
Depending on the presence of clear boundaries of the tumor, there are:
- Encapsulated neurofibroma, which forms in the thickness of large nerves. The capsule of the node is the nerve sheath. Since during the development of a tumor there is a random proliferation of nerve fibers, which are separated by bundles of collagen fibers, the nerve itself acquires a spindle-shaped shape in the affected part. In most cases, the location of encapsulated neurofibromas is soft tissue, retroperitoneum and mediastinum. A solitary encapsulated neurofibroma is a well-circumscribed, dense nodule that consists of a uniform gray-white or gray fibrous structure. Tumors located in soft tissues rarely reach large sizes (on average, a node in diameter does not exceed 4 cm).
- Diffuse (plexiform) neurofibroma, which is formed when small nerves are damaged and has the appearance of numerous nodes. This type of tumor does not have clear boundaries and in most cases is located subcutaneously and on the skin, but in some cases it is detected in the intermuscular layers. Often diffuse neurofibroma consists of elongated lemmocytes (Schwann cells). Pigment cells and receptors similar to Meissner and Vater-Pacini corpuscles may also be present. This most common neoplasm of peripheral nerves often occurs in association with neurofibromatosis type I.
The structure of all neurofibromas is a chaotic arrangement of nerve fibers located inside the perineurium, which are separated by connective tissue cells, but from a histological point of view, neurofibromas are divided into neurofibromas:
- Myxoid, the stroma of which contains a lot of mucin.
- Plexiform, which consists of numerous nerve bundles of irregular configuration. These nerve bundles are embedded in a matrix containing spindle cells, wavy collagen fibers, tissue basophils, and mucin.
- Consisting of structures resembling tactile bodies.
- Pigmented (melanocytic), which resembles dermatofibrosarcoma protuberans.
Types of disease
There are several types of neurofibromatosis.
- Neurofibromatosis type 1, which is known as Recklinghausen's disease, has four clinical subtypes. In the first case, patients develop predominantly neurofibromas, while in the second, large pigment spots predominate. There is also a mixed form, and a generalized one with the appearance of many small spots.
- Neurofibromatosis type 2 (central) develops due to the absence of a primary gene product, which probably inhibits the development of tumor growth. With this type of neurofibromatosis, skin manifestations may be minimal. Pigment spots appear in only 42% of patients, neurofibromas - in no more than 19%. This type of disease is characterized by the appearance of dense, painful and mobile subcutaneous tumors – neuromas. In most cases, patients develop bilateral acoustic neuroma, leading to deafness.
- Neurofibromatosis type 3 (mixed) is a rapidly progressive disease. Characterized by the formation of tumors of the central nervous system. The disease first appears at the age of 20-30.
- Neurofibromatosis type 4 is similar to the disease type 2, but differs in more intense skin manifestations in the form of the formation of numerous neurofibromas. There is a high risk of damage to the optic nerve and brain.
- Neurofibromatosis type 5 is segmental and is characterized by unilateral damage to a certain area of the skin.
- In neurofibromatosis type six, neurofibromas are not formed; the disease manifests itself only in the appearance of pigment spots.
- A separate (seventh) type of neurofibromatosis is a type of disease in which symptoms appear in adults, mainly after 20 years.
General information
The first description of neurofibroma was found in the work of Askenazy (1914) - the author described bronchial neurofibroma, which arose against the background of generalized neurofibromatosis.
Multiple neurofibromas are a characteristic feature of neurofibromatosis type I. This genetic disease was described by a number of researchers in the second half of the 19th century, but the first complete description of the clinical and morphological changes in this disease is considered to be the work of the German pathologist Friedrich von Recklinghausen (1882).
Since Friedrich von Recklinghausen described the disease long before the discovery of DNA, all diseases associated with the formation of multiple neurofibromas were for a long time called “Recklinghausen’s disease.”
After the genetic causes of neurofibromatosis were identified, this disease began to be differentiated by type.
Bronchial neurofibroma was also described in 1985 by H. Spencer, who analyzed 24 cases in his work.
In 1928, Starck described generalized pulmonary neurofibromatosis, which was observed in combination with cystic changes in the lungs.
In 1987, V. Riccardi made the first attempt at a pathogenetic approach to the treatment of genetically determined neurofibromatosis through the long-term use of ketotifen.
Neurofibroma occurs with equal frequency in children and adults. Most researchers note that this neoplasm is equally common in both sexes, but some authors point to a predominance of males (3:2).
In adults, in most cases, this tumor appears at the age of 20-30 years.
Neurofibromatosis is more often detected in older people, and solitary neurofibromas are more often formed in young people.
The prevalence of neurofibromatosis type I is 85% of all cases of this disease and is detected in 1:3000 - 1:4000 of the population, and neurofibromatosis type II is detected in every 50,000 newborns.
In soft tissues, in most cases, solitary (single) neurofibromas are detected.
11% of all described cases of neurofibromatosis were distinguished by malignant degeneration.
Diagnostic methods
Diagnosis of neurofibromatosis is based on the study of clinical manifestations. In order to establish a clinical diagnosis of Recklinghausen's disease, at least two of the following symptoms must be present:
- The presence of 6 or more characteristic pigment spots on the skin;
- The presence of two or more neurofibromas;
- The appearance of Lesh nodules on the iris.
- Presence of optic nerve glycoma;
- The presence of many small pigment spots in large skin folds;
- Presence of changes in the skeletal system.
- An established diagnosis of neurofibromatosis in one of the parents.
When diagnosing neurofibromatosis type 2, the presence of one of the following symptoms is taken into account:
- Acoustic neuroma detected by X-ray examination in the patient himself or in one of his parents.
- The presence of more than two neurofibromas.
- The presence of a tumor in the tissues of the spinal cord or brain.
A diagnostic sign of neurofibromatosis type 3 is the presence of neurofibromas on the palms.
Treatment
In some cases, radiation therapy is used for treatment.
For neurofibromatosis, symptomatic treatment is prescribed. In the presence of giant neurofibromas or when signs of malignant degeneration appear, radical removal of the tumors is necessary. If there are contraindications for surgery, radiation therapy may be used.
Surgical removal of neurofibroma is performed as an open operation to excise the tumors. The operation can be performed under local or general anesthesia. Low-traumatic endoscopic surgery is also possible for certain localization of neurofibromas.
If surgery is not possible, radiation treatment is performed. The tumor is exposed to radiation beams at a certain angle. When carrying out such treatment, the impact on healthy tissue is minimal.
Treatment with traditional methods
To alleviate the condition of patients with neurofibromatosis, traditional healers recommend taking an infusion of Japanese Sophora. The fruits of this plant should be brewed in a thermos overnight. Drink the resulting infusion throughout the day. You need to drink 600 ml of infusion per day, dividing this amount into 12 servings.
Causes and types of neurofibromatosis
The causes of Recklinghausen's disease are unknown exactly, but the main pathogenetic link is considered to be a genetic defect found on chromosome 17 in the first type of NF and on chromosome 22 in the second. The pathology is inherited in an autosomal dominant manner, which means that any owner of the gene will be sick; asymptomatic carriage is impossible. If one of the parents is diagnosed with Recklinghausen's disease, then the probability of having a child with the pathology is 50%. If both parents are sick, this figure increases to 66.7%.
Due to the hereditary mechanisms of pathogenesis, the disease is familial in nature, and among the relatives of the sick person there will certainly be those who already suffer from the pathology. In rare cases, NF develops in healthy families due to a spontaneous single mutation.
Studies of the role of the genetic factor have suggested that genes in which mutations appear normally have an anti-oncogenic effect. With pathology, their production of the neurofibromin protein, which is responsible for the proper differentiation and proliferation of cells in nerve endings, decreases or completely stops. In the absence of this protein, uncontrolled proliferation of cellular elements begins, and this applies not only to Schwann cells enveloping the processes of neurons, but also to fibroblasts, mast cells, and lymphocytes. At the same time, the composition of the intercellular substance, which in the tumor is represented by acidic mucopolysaccharides, also changes.
Based on the localization of neurofibromas, it is customary to distinguish several forms of pathology:
- Neurofibromatosis type 1, when the neoplastic process affects peripheral nerve endings, is a more common type of NF;
- NF type 2 involving the central nervous system (CNS) is much less common;
- NF type 3 is a very rare type and is accompanied by damage to the palms, auditory nerve, and brain tumors;
- NF type 4 is very rare, the symptoms are the same as in type 1, but there are no Lisch nodules.
With type 1 Recklinghausen disease, peripheral nerves are affected, characteristic spots and pigmentation disorders appear on the skin, the process is usually widespread, affects the optic nerves, the iris, and may be combined with bone defects. In type 1 NF, as a rule, there are known relatives who suffer or have suffered from this disease.
Neurofibromatosis type 2, which is more rare, is accompanied by damage to the auditory and optic nerves , usually bilateral, and the formation of tumors in the brain, while skin manifestations may not be too pronounced.
Neurofibromatosis in children is also caused by genetic mechanisms, and in a sick child, signs of the disease appear quite early. Typically, the manifestation of pathology occurs at the age of 3-15 years; a particularly high risk of progression is observed during periods of intensive growth of the child, when all cells multiply intensively, biochemical metabolic processes are actively taking place, which creates the preconditions for tumor growth, among other things.
The main symptoms of the disease in childhood do not differ from those in adults, but have some features. Peripheral, visual and auditory nerves, skin and internal organs are affected. The presence of a large tumor impairs the child’s growth, deformities of the limbs and curvature of the spine appear, the development of intelligence slows down, and a tendency to severe depression appears. Disturbances in the development of the musculoskeletal system are very characteristic of NF in children, because in adults the skeleton is already formed, and the tumor cannot have such an effect on the bones.
Premium Aesthetics – Coffee Stains
Premium Aesthetics Library
Coffee spots (café au lait spots, café au lait macules, CALMs) are hyperpigmented areas on the skin with jagged or smoothed edges, ranging in color from light to dark brown. In foreign literature they are often called “café au lait spots”, which is a combination of the French “café au lait” (coffee with milk) and the English “spots” (spots).
In our company you can purchase the following equipment for removing coffee stains:
In newborns, coffee spots occur with varying probability, depending on the skin phototype:
- 0.3% of children - phototypes I–III;
- 3% of children - IV phototype;
- 18% of children have V–VI phototypes.
Before puberty, such spots can appear with a probability of 13% in light-skinned people and 27% in dark-skinned people.
Etiology and pathogenesis
Coffee stains usually indicate that a patient has neurofibromatosis type I , a multisystem disease characterized by spots on the back, neck, and axillary areas, as well as skeletal dysplasia, benign or malignant tumors of the nerve sheaths (neurofibromas).
The average incidence of neurofibromatosis type I is 1:3000. Its main causes are considered to be mutations or deletions (loss of a section) of the NF1 gene. This gene is responsible for the production of neurofibromin 1, a protein that suppresses the occurrence of tumors of the nervous system.
A decrease in its synthesis leads to the appearance of neurofibromas and other clinical signs of the disease.
Coffee stains on the skin can also occur for the following reasons:
- Albright-McCune-Sternberg syndrome - premature puberty, multiple fibrous osteodysplasia, skin hyperpigmentation.
- Bourneville-Pringle disease - tuberculous sclerosis; a rare genetic disease in which multiple benign tumors form in organs and tissues.
- Fanconi anemia is manifested by a complex of symptoms, the most serious of which are hematological disorders and tumors.
- Coffin-Siris syndrome is characterized by aplasia or hypoplasia of the distal phalanx or nail on the fifth toe, developmental delay, mental retardation, coarse facial features, etc.
Cafe-au-lait skin spots may be the result of RAS mutations —changes in the RAS family of genes and proteins.
These are small GTPases (enzymes that bind and hydrolyze guanosine triphosphate, an energy substrate for RNA), which are involved in signal transmission from outside the cell and regulate cell division.
Some RAS mutations promote the emergence and metastasis of tumors.
In 50% of patients, the genetic mutations responsible for the appearance of coffee spots on the skin occur spontaneously. That is, the hereditary mechanism of transmission of the disease in this case is of indirect significance.
As for pathogenesis , coffee spots appear against the background of an increase in melanin production and the presence of giant melanosomes in the skin. In patients with neurofibromatosis type I, the number of melanocytes in age spots increases more significantly compared to other diseases.
Clinical manifestations
Diagnosis of neurofibromatosis type I is based on the search for key criteria - we can talk about the disease if at least 2 of 7 signs are present:
- Six or more coffee spots or macules on the skin with a diameter of more than 5 mm in children (before puberty) and more than 15 mm in adolescents and adults (after puberty) ( Fig. 1 ).
- More than two spots in the groin or armpit areas.
- Two or more typical neurofibromas or one plexiform neurofibroma.
- Optic nerve glioma.
- Two or more hamartomas of the iris are usually detected by an ophthalmologist using a slit lamp.
- Dysplasia of the sphenoid bone of the skull or pathologies of the long bones of the skeleton (for example, pseudarthrosis).
- Family history - the presence of neurofibromatosis in close relatives (father or mother, brothers or sisters).
Many of these signs are not present until puberty, making diagnosis difficult in children. Moreover, if a patient at risk reaches 10 years of age without the appearance of at least one symptom (for example, coffee stains), in the future he will almost certainly not have neurofibromatosis type I.
Neurofibromatosis type I should be distinguished from type II, in which the skin manifestations are relatively poor, but patients have a tendency to develop meningiomas and bilateral acoustic neuromas.
Other syndromes in which coffee stains may appear on the skin (some of them were listed above):
- Silver-Russell syndrome - growth retardation and psychomotor development, triangular face, shortened fingers, syndactyly, characteristic light brown spots on the skin, etc.
- Bloom's syndrome - dwarfism, reduced immunity, increased photosensitivity of the skin, coffee stains, etc.
- Gorlin-Goltz syndrome is a hereditary basal cell carcinoma of the skin with erythematous lesions and skeletal abnormalities.
- Maffucci syndrome is a benign overgrowth of cartilage tissue with bone deformation and dark vascular formations on the skin.
These are not all syndromes in which characteristic café-au-lait hyperpigmentation may occur on the skin. However, they are united by two important factors - relative rarity and overall severity, i.e. the presence of other signs (except coffee stains) that have a much more significant effect on the body.
In general, the following patterns are noted:
- Multiple small coffee stains indicate the presence of one of the above diseases (usually neurofibromatosis type I).
- Single large light brown spots, as a rule, are not associated with other pathologies and exist on their own.
Rice. 1. Coffee stains in the armpits and back (www.medscape.com)
Principles of treatment
Before starting treatment for coffee stains, more serious pathologies should be excluded. For this patient, it is necessary to carefully interview, carefully examine, and prescribe laboratory and instrumental studies. It is impossible to do this in a cosmetology office, so it is important to maintain continuity and maintain contact with doctors of other specialties.
If coffee stains are associated with any diseases, maximum efforts should be directed toward treating the underlying pathology. If coffee stains exist on their own, or the underlying disease has already been treated, but areas of hyperpigmentation remain, you can use hardware methods.
One such technique is the Q-switched alexandrite laser . In a study of 48 people, it showed good to excellent effectiveness in more than half of the patients (51.4%) after an average of 3.2 sessions.
Moreover, relapse was recorded in 10.4% of cases. Laser treatment for coffee spots carries a high risk of post-inflammatory hyperpigmentation - about 50%.
If this occurs, therapy should be discontinued until hyperpigmentation resolves.
IPL therapy has also been successfully used to treat coffee stains . Intense pulsed light (IPL) selectively destroys melanin in areas of excess accumulation, resulting in lighter skin.
Modern IPL devices, such as M22 (Lumenis), are equipped with light filters that allow the skin to be exposed to the required range of the radiation spectrum.
Thanks to this, IPL can be safely used to treat coffee stains on dark skin - up to Fitzpatrick phototype V.
It has been noticed that if the coffee stain is completely removed, then the risk of its reappearance is minimal. If the stain is partially removed, the probability of recurrence is 50%.
Other Indications
Source: https://www.premium-a.ru/disease/pigmentnye-dishromii/kofejnye-pyatna/
Symptoms of Recklinghausen's disease
NF is characterized by a very diverse clinical picture, damage to many organs in addition to the skin, and a progressive course. Complications are also possible, including fatal ones - malignant transformation, heart failure, lung failure, central nervous system damage.
Symptoms of the disease do not appear immediately, but sequentially at different age periods, so it can be problematic to suspect NF in young children. The only sign of pathology in the first years of life may be age spots, while other symptoms appear later, between 5 and 15 years.
NF can be provoked by external unfavorable factors and stressful conditions, such as:
- Adolescence and hormonal changes associated with it;
- Pregnancy and childbirth;
- Injuries;
- Acute infections and pathology of internal organs.
The progression of the disease can also be caused by medical procedures - massage, physiotherapeutic procedures, removal of small neurofibromas for cosmetic purposes. It is now customary to widely prescribe massage to babies in the first year of life, citing possible pathology of the musculoskeletal system, but it is during this period that it is most difficult to diagnose NF, the signs of which may be absent, so doctors dealing with young children should take this possibility into account and at least find out parents, whether there is an unfavorable heredity in relation to Recklinghausen's disease.
The course of NF varies greatly among different patients. It is impossible to predict exactly at what age and what specific manifestations it will appear. What causes the large differences in the clinical picture of the disease is still unclear.
The main symptoms of neurofibromatosis are:
- Dark spots;
- Tumor-like formations of peripheral nerves located subcutaneously;
- Lymphatic drainage disorders;
- Damage to the auditory and optic nerves;
- Skeletal anomalies.
Pigment spots are one of the most characteristic and early symptoms of neurofibromatosis. They are located on the skin of the torso, neck, and less often on the face, arms and legs. Their diameter exceeds one and a half centimeters, so seeing them in a newborn is not difficult. The color of the spots is light yellow to coffee, although they can also be blue-violet.
Peripheral nerve tumors are found under the skin in the torso, neck, head and limbs, are multiple, and their number is sometimes impossible to count. These neuromas constitute a significant cosmetic defect, disfiguring the surface of the body and face. Often, even in the presence of internal lesions or the brain, it is the cosmetic defect that becomes the main complaint of the patient.
Peripheral neuroma consists of Schwann cells, mast cells, lymphocytes and a connective tissue component; it is dense, often painless and easily dislocated when palpated. Possible pain and itching at the site of neoplasia growth. Its average size is about two centimeters, but there are large neurofibromas weighing several kilograms. The skin overlying a neurofibroma may be pigmented.
Neurofibromas can compress nerve trunks and blood vessels, leading to pain and impaired lymphatic drainage. Patients note an increase in the size of a limb, tongue, area of the face, or other part of the body, which is associated with stagnation of lymph. Compression of the mediastinal organs leads to shortness of breath, difficulty breathing, arrhythmias, and heart failure.
Plexiform neurofibroma can be diffuse, broad-based or hanging above the surface of the skin; it is usually soft in consistency and forms under the skin or in internal organs. These tumors can cause overgrowth of skin and tissue, forming large, hanging nodules covered with pigmented, wrinkled skin. In the depths of such a conglomerate, a tangle of thickened nerves can be felt. Plexiform neurofibromas on the head, face, and torso are disfiguring, and when located inside the body, they compress organs, disrupting their function.
Neurofibromatosis type I may be accompanied by skeletal abnormalities - curvature of the spine and impaired formation of the vertebrae, asymmetrical skull. A characteristic sign of this type of disease is a Lisch nodule - a whitish spot on the iris of the eye, which is present in more than 90% of patients.
Damage to the central nervous system is accompanied by tumors of the nervous tissue (gliomas, meningiomas), which compress it, spinal roots, and cranial nerves. Patients with such changes complain of headaches, mood lability, and the neurologist discovers a violation of the sensitivity of the sphere, coordination disorders, and speech. Neuromas of the optic or auditory nerve are dangerous due to visual impairment, glaucoma, and deafness.
In children, brain damage inevitably leads to delayed mental and intellectual development. Young patients are extremely susceptible to severe depression, which is very difficult to treat. Large intracranial neurofibromas can provoke seizures.
To make a diagnosis of NF, the doctor evaluates skin manifestations, the presence of peripheral tumor formations, and ascertains family history. A group of experts on neurofibromatosis identified signs that must be present in the subject to confirm neurofibromatosis, and identifying at least 2 of them allows us to reliably judge the development of the disease:
- 5 or more light coffee-colored spots more than 0.5 cm in diameter before adolescence;
- 6 or more spots one and a half centimeters in size after puberty;
- At least 2 Lisch nodules on the iris;
- Multiple small pigment spots in the folds of the skin;
- At least 2 any neurofibromas or 1 plexiform;
- Optic nerve glioma;
- Changes in bone tissue - dysplasia of the wing of the main bone of the skull, congenital thinning of the cortical layer of tubular bones;
- Presence among close relatives of patients with neurofibromatosis.
How to identify
First of all, neurofibroma is accompanied by pain along the nerve due to damage to the nerve fiber tissue. This pain spreads along the nerve itself.
The focal clinical picture of the tumor depends on the location of the tumor. For example, if the disease has formed in the area of the nerve fiber of an internal organ, the function of the latter is impaired. If the neoplasm is localized in the spinal roots, sensitivity disorders are observed.
Neurofibroma grows slowly, so it is difficult to detect in the early stages of development.