Description
Hydrocephalus. Increased accumulation of cerebrospinal fluid in the cerebrospinal fluid system of the brain. Hydrocephalus accompanies many congenital and acquired neurological diseases. Clinically, it is manifested by signs of increased intracranial pressure (headache, nausea, pressure on the eyes), symptoms of compression of brain structures (vestibular ataxia, visual impairment, mental disorders, epileptic seizures) and symptoms characteristic of the disease that caused it. Diagnosis of hydrocephalus includes radiography of the skull, ophthalmological studies, echo-EG (in infants - neurosonography), MRI or CT scan of the brain. Surgical treatment of hydrocephalus allows you to correct congenital anomalies of the cerebrospinal fluid system, remove intracranial formations that disrupt the circulation of the cerebrospinal fluid, and establish the outflow of cerebrospinal fluid from the cranial cavity.
Treatment (medicines)
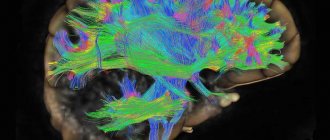
Liquor pathways.
The main principle of treatment for ICH is etiological, that is, elimination of the original cause that caused it. If necessary, an intracranial formation (tumor or hematoma) is removed, or the liquor system is shunted (for hydrocephalus). If the function of the respiratory system and consciousness is impaired, tracheal intubation with artificial ventilation (ALV) is performed, parenteral nutrition is established, and the water-electrolyte composition is balanced.
In preparation for surgical treatment, in order to reduce ICP, osmotic diuretics (mannitol, glycerol) are used, which promote the transition of water from extravascular spaces into the blood plasma; glucocorticosteroids (dexamethasone) to restore the blood-brain barrier (BBB); loop diuretic (furosemide).
The same conservative therapy is successfully used, and to reduce pressure on the optic nerve, decompression of the optic canal is performed.
You can thank me for the article by subscribing to the channel about neurology and neurorehabilitation. Thank you!
Additional facts
Hydrocephalus literally means “dropsy of the head.” In modern neurology, this is a common clinical syndrome that can be observed in many diseases, congenital anomalies or post-traumatic conditions of the brain. The occurrence of hydrocephalus is associated with certain disorders in the cerebrospinal fluid system of the brain. People of any age are susceptible to hydrocephalus. Hydrocephalus can occur in newborns, be congenital, develop in children and adults, and accompany atrophic processes occurring in the brain in old people. However, it is most often encountered in pediatric practice.
G91 Hydrocephalus
Etiology and pathogenesis
One should not think that this is a common disease and that normal pressure hydrocephalus should be suspected in every elderly patient with pelvic disorders: its prevalence does not exceed 4% among people suffering from various forms of dementia. Complicating the situation is the fact that the diagnosis of dementia itself has different criteria, and so far there is no uniform approach among scientists from different countries.
What is the cause of NG (normotensive hydrocephalus)? In approximately half of all cases, it was possible to prove that the patient had a history of:
- hemorrhages in the brain (both intraventricular and subarachnoid);
- various traumatic brain injuries;
- meningitis;
- perinatal damage to the central nervous system;
- volumetric formations in the cranial cavity (from castes and aneurysms to tumors);
- congenital anomalies of the liquor-conducting system - atresia, or underdevelopment of the Sylvian aqueduct;
- surgical neurosurgical interventions.
From this list it is clear that nothing specific leading to pathology was identified - the list turned out to be too “variegated”, and it must be taken into account that doctors were specifically looking for the cause. In 50% of cases, no possible factors were found at all. Considering this circumstance, we agreed to call this condition “idiopathic hydrocephalus.” The situation was saved, and the cause of Hakim-Adams syndrome was able to “officially” remain unknown.
Interestingly, without increasing ICP it is impossible to “inflate” the ventricles. How does the paradox of a normal ICP level arise with dilated ventricles? It turned out that episodes of elevated ICP exist, but they occur at the same time as spontaneous Prinzmetal angina - at night, during the REM sleep phase. The vessels dilate, and brain hyperemia occurs. The outflow of cerebrospinal fluid, which is functional in nature and is associated with changes in pressure indicators in different parts of the cerebrospinal fluid system of the brain, is also disrupted. During the daytime, as well as during the slow-wave sleep phase, this disorder does not occur.
Since episodes of increased ICP are temporary and not permanent, the symptoms of “stagnation” are not identified - it simply does not have time to develop.
How is this disease detected?
Anatomy and pathological anatomy
Normally, cerebrospinal fluid (CSF) is produced by the choroid plexus of interconnected ventricles of the brain. The largest amount of it is formed in the lateral ventricles, from where the cerebrospinal fluid enters the third ventricle, and from it through the Sylvian aqueduct into the fourth ventricle. Then the cerebrospinal fluid enters the subarachnoid (subarachnoid) space, which extends over the entire surface of the brain, and in the caudal direction passes the region of the craniovertebral junction and then surrounds the spinal cord along its entire length. The cerebrospinal fluid located in the subarachnoid space is constantly absorbed by the arachnoid (arachnoid) membrane of the spinal cord and brain and enters the blood.
Symptoms of normal pressure hydrocephalus
Initially, a walking disorder appears (“feet stick to the floor,” slow walking, difficulty starting movement, impaired balance/falling) over several months or years. Cognitive impairment (difficulty in thinking, memory loss) appears within 6–12 months. In the early period of the disease, urinary disorders occur.
An objective examination of the patient can reveal ataxia, apraxia of walking (85%), slow gait with legs wide apart (70%), acheirokinesia (10%), pyramidal hypertonicity in the legs (70%), paratonic rigidity (20%), hyperreflexia (30%), apathy/depression (50%), cognitive decline (40%).
Causes
Three pathological mechanisms lead to the accumulation of an excess amount of cerebrospinal fluid in the cerebrospinal fluid system of the brain: the production of an excess amount of cerebrospinal fluid, a violation of its absorption, or a disorder of the cerebrospinal fluid circulation. Hydrocephalus may be based on one of these mechanisms or a combination of them. The causes that cause disturbances in the functioning of the cerebrospinal fluid system can act during fetal development and cause congenital hydrocephalus or affect the brain after birth and cause the appearance of so-called acquired hydrocephalus. The causes of congenital hydrocephalus include malformations of the cerebrospinal fluid system (atresia of the foramina of Magendie and Luschka, defects in the structure of the subarachnoid space, stenosis of the Sylvian aqueduct, Dandy-Walker syndrome, etc.), craniovertebral anomalies (Chiari malformation, congenital basilar impression), intrauterine infections (toxoplasmosis , congenital syphilis, cytomegaly, rubella), birth trauma. Acquired hydrocephalus can occur as a result of inflammatory processes in the brain and its membranes (encephalitis, arachnoiditis, meningitis), traumatic brain injury, vascular disorders (bleeding into the ventricles, hemorrhagic stroke or intracerebral hematoma with blood breaking into the ventricles). Hydrocephalus often develops against the background of a colloid cyst of the third ventricle and intracerebral tumors (astrocytomas, germinomas, ganglioneuromas, etc.), which grow into the ventricles of the brain or compress the cerebrospinal fluid pathways, thereby disrupting the normal circulation of cerebrospinal fluid and its outflow from the cranial cavity. Separately, there is an atrophic (replacement) form of hydrocephalus, which occurs as a result of post-traumatic death or age-related atrophy of brain tissue. In this case, cerebrospinal fluid fills the space that is formed inside the skull as a result of a decrease in the volume of the brain. Atrophic hydrocephalus in old age can develop against the background of impaired blood supply to the brain due to atherosclerosis of cerebral vessels, hypertension, and diabetic macroangiopathy.
Treatment[ | ]
The main method of treating hydrocephalus is surgical. To reduce intracranial pressure, diuretics are prescribed as a therapeutic measure.
Bypass[ | ]
Schematic representation of a typical shunt
Since the 1950s, the standard treatment for any form of hydrocephalus has been shunt surgery to restore the movement of cerebrospinal fluid. After craniotomy, one end of the shunt, ending with a radiopaque catheter, is passed into the cavity of the dilated ventricle. The intermediate, longest part, made of silicone, is located subcutaneously. The distal end, also containing a catheter, opens into the abdominal or thoracic cavity to allow drainage. The shunt is equipped with a pump that automatically regulates the pressure of the cerebrospinal fluid [3] [4].. Since the mid-80s, endoscopic operations began to occupy a significant place in the treatment of hydrocephalus.
Treatment of occlusive hydrocephalus with shunting is quite effective, however, according to various sources, complications with this operation account for 40-60% of cases. In this case, depending on the cause of the dysfunction, the entire shunt or its parts must be replaced. Experience shows that most often complications requiring shunt revision occur in the period from six months to one year after surgery. Most patients who undergo bypass surgery will have to undergo several surgical procedures during their lifetime. In any case, at a minimum, you should expect two or more revisions - after all, the child is growing. After shunt operations, the patient becomes shunt dependent, that is, his entire future life will depend on the work of the shunt.
Complications of bypass operations[ | ]
- Occlusion (blockage) both in the ventricles of the brain and in the abdominal cavity.
- Infection of the shunt, ventricles of the brain, meninges.
- Mechanical damage to the shunt.
- Overdrainage (rapid discharge of cerebrospinal fluid from the ventricles) is often accompanied by rupture of convexital veins and the formation of hematomas.
- Hypodrainage (slow outflow from the ventricles) - surgery in this case is ineffective.
- Development of epileptic syndrome, bedsores of the abdominal organs, etc.
External drainage operations[ | ]
See also: Ventricular puncture
This is a method of removing cerebrospinal fluid from the ventricles of the brain from the outside, used as a measure of despair, and is accompanied by the greatest number of complications, especially increasing the risk of infection.
Endoscopic treatment of hydrocephalus[ | ]
Currently, endoscopic treatment of hydrocephalus is a priority in the world practice of neurosurgery. Types of surgical endoscopic interventions for hydrocephalus:
- endoscopic ventriculocisternostomy of the bottom of the third ventricle,
- aqueductoplasty,
- ventriculocystocysternostomy,
- septostomy,
- endoscopic removal of intraventricular brain tumor,
- endoscopic installation of a shunt system.
Other types of surgical interventions have not yet found widespread use in clinical practice.
Endoscopic ventriculocisternostomy of the bottom of the third ventricle[ | ]
This operation is widely used and accounts for about 80% of neuroendoscopic operations for hydrocephalus. The purpose of the operation is to create pathways for the outflow of fluid from the ventricular system of the brain (III ventricle) into the cisterns of the brain, through the paths of which fluid is reabsorbed (absorbed) as in a healthy person.
Indications for surgery:
- primary surgery for occlusive hydrocephalus with a level of occlusion from the posterior parts of the third ventricle and more distally;
- an alternative operation for complications of shunt operations with removal of a previously installed shunt system (instead of the operation of “revision of the shunt system”);
- post-traumatic hydrocephalus;
- mixed hydrocephalus (internal and external);
- operation of choice when removing the shunt system to achieve shunt independence;
Advantages of the operation compared to classic shunts:
- the operation restores the physiological (as in a healthy person) liquor flow from the ventricular system of the brain into the basal cisterns;
- there is no implantation of a foreign body (shunt system) into the body and thus the problems associated with it (infection, malfunction, the need for revisions) are eliminated;
- the risk of overdrainage and associated complications (subdural hematomas, hydromas, etc.) is significantly lower;
- less traumatic operation;
- the operation is more cost-effective for medical institutions;
- improving quality of life.
Surgery is virtually the only method of combating the disease. In most cases, drug methods can only slow down the course of the disease, but do not eliminate the root cause of the disease. If the operation is successful, an almost complete recovery with a return to normal life is likely.
Classification
According to the etiological principle, congenital and acquired hydrocephalus are distinguished. According to the mechanism of occurrence, hydrocephalus is classified into open and closed forms. Open hydrocephalus is associated with overproduction of cerebrospinal fluid or impaired absorption during normal cerebrospinal fluid circulation. Closed hydrocephalus is caused by a violation of the outflow of cerebrospinal fluid due to compression, partial or complete obstruction of any part of the cerebrospinal fluid system of the brain. Depending on where the excess accumulation of cerebrospinal fluid occurs, internal and external hydrocephalus are distinguished. Internal hydrocephalus is accompanied by the accumulation of cerebrospinal fluid in the ventricles of the brain. External hydrocephalus is characterized by excess cerebrospinal fluid in the subarachnoid and subdural space. According to the characteristics of its course, hydrocephalus is classified as acute, subacute and chronic. Acute hydrocephalus is characterized by rapid development, in which decompensation occurs a few days after the onset of the first signs of the disease. Subacute hydrocephalus develops within a month, and chronic hydrocephalus develops over six months. Of great clinical importance is the division of hydrocephalus into stabilized (compensated) and progressive (increasing). Stabilized hydrocephalus does not grow and usually occurs with normal cerebrospinal fluid pressure. Progressive hydrocephalus is characterized by worsening symptoms, is accompanied by an increase in cerebrospinal fluid pressure, does not respond well to conservative therapy and leads to atrophy of brain tissue.
Symptoms of idiopathic hydrocephalus
Fortunately, the clinical manifestations of the disease are much more definite than the possible causes. This is the “Hakim-Adams triad”: first, gait is impaired, later dementia progresses and its diagnosis is made, and only then pelvic disorders arise, among which urinary incontinence comes to the fore. Symptoms may vary in intensity, but variability is acceptable. What are the characteristics of each “member of the triad”?
Gait disorders
The gait of a patient with NG is uncertain: he overcomes turns poorly, moves in small steps, has difficulty maintaining balance and tries not to raise his legs above the floor. This gait is also called “sticky” or “magnetic”. Only the movements of the legs are striking; the patients’ arms are all right.
Patients gradually decrease their step height, and it becomes difficult for them to climb stairs. Starting a movement is just as difficult, and in order to turn, you need to perform several “preparatory” actions. In this case, the patient falls quite often. Noteworthy is the fact that the patient can make stereotypical “walking” movements with his legs, even while lying in bed or sitting.
Muscle tone does not determine the development of gait disorders and gait skills (gait apraxia). It can be diffusely reduced and remain physiological or elevated in a pyramidal or spastic type.
A characteristic feature that makes it possible to identify Hakim-Adams syndrome is a sharp improvement in the patient’s gait after he undergoes a lumbar puncture and a fairly large (20–40 ml) amount of cerebrospinal fluid is removed. This test is called a “tap test”. As noted, the removal of cerebrospinal fluid significantly improves the ability to maintain balance, and at the same time walking is restored.
Some scientists believe that the functions of the arms remain normal because their motor fibers extend further from the walls of the lateral ventricles of the brain than the fibers of the legs and undergo minimal morphological changes.
Dementia
Dementia, or a violation of higher cortical functions, manifests itself in this disease in full, usually after gait disorders. But often it precedes them, and in a nonspecific form: memory decreases and the speed of mental reaction slows down. Apathy begins. Subsequently, complacency arises, spontaneity appears, or the motivation for any type of activity decreases. There is disorientation in time, and in some patients, cognitive disorders transform into psychotic ones: hallucinations, a manic state appear, and even consciousness is impaired like delirium.
People around and relatives notice symptoms of “emotional atrophy”: patients stop showing any feelings. In severe cases of the disease, drowsiness, a stuporous state, and even akinetic mutism may develop. All this leads to the development of bedsores, the addition of a secondary infection and the death of the patient.
There is also a tendency to display a “frontal” psyche. The “frontal” nature of the disorder consists of a decrease in self-criticism, the appearance of foolishness, a tendency to flat and “greasy” jokes, as well as a violation of the sequence of actions. So, the patient can urinate first, and then unbutton his pants. Many researchers believe that this is due to the predominant damage to the anterior horns of the ventricles. As a result, the functioning of the frontal lobes in depth is disrupted, their associative and commissural connections with each other and with the corpus callosum are impoverished.
Symptoms
The accumulation of excess cerebrospinal fluid in a limited space of the cranium leads to increased intracranial pressure, which causes the most typical symptoms of hydrocephalus. In adults and older children, these include: intense headache that cannot be relieved by analgesics, nausea, vomiting, and a feeling of pressure on the eyeballs. These symptoms may occur acutely or increase gradually, being transient at the onset of the disease. Atrophic hydrocephalus often occurs without signs of increased intracranial pressure and is detected only with additional examination of the patient. In most cases, hydrocephalus is accompanied by neurological symptoms, which are caused both by compression of brain structures by expanded cerebrospinal fluid spaces and by the underlying disease that causes the development of hydrocephalus. The most common symptoms of hydrocephalus are vestibular and visual disturbances. The first includes vestibular ataxia, manifested by dizziness, unsteady gait, noise in the ears and head, and nystagmus. On the visual side, there may be a significant decrease in visual acuity, loss of certain areas of the visual fields, congestive optic discs; with prolonged hydrocephalus, atrophy of the optic nerves may develop. Hydrocephalus can occur with disturbances in the motor and sensory sphere: paresis and paralysis, increased tendon reflexes and muscle tone, decreased or complete loss of all types of sensitivity, and the formation of spastic contractures of the limbs. Occlusive hydrocephalus, caused by impaired circulation of cerebrospinal fluid in the posterior cranial fossa, is characterized by symptoms of cerebellar ataxia: impaired coordination and gait, large-scale disproportionate movements, changes in handwriting, etc. In children, due to the high compliance of the skull bones, there is no increase in intracranial pressure; they have hydrocephalus accompanied by an increase in the size of the skull. In newborns and young children, hydrocephalus is characterized by an overly large head size, bulging scalp veins, tension and lack of pulsation of the large fontanel, and swelling of the optic discs. The symptom of “setting sun” is often noted - restriction of upward movements of the eyeballs. There may be dehiscence of the sutures of the skull. Tapping on the skull is accompanied by a characteristic sound (the “cracked pot” symptom). In children in the first year of life, hydrocephalus leads to developmental delays. They later begin to hold their head up, roll over, sit up and walk. Children who have severe hydrocephalus are distinguished by a spherical shape of the head, its too large size, deep-set eyes, protruding ears, and thinning of the scalp. There may be decreased vision, increased muscle tone in the lower extremities, and disorders of the cranial nerves. Unlike adults, in childhood hydrocephalus is often accompanied not by emotional-volitional disorders, but by intellectual deficiency. Children with hydrocephalus are usually sedentary and obese. They are apathetic, lack initiative, and do not have the attachment to relatives characteristic of their peers. A decrease in the degree of hydrocephalus often leads to an increase in the child’s intellectual abilities and activity.
Hydrocephalus - description, symptoms (signs), diagnosis, treatment
Source: https://gipocrat.ru/boleznid_id34432.phtml
Hydrocephalus (dropsy of the brain) - excessive accumulation of cerebrospinal fluid in the ventricles of the brain and intrathecal spaces; manifested by symptoms of increased ICP • Occurs due to an imbalance between the formation and absorption of cerebrospinal fluid: less is absorbed than is formed. The cause may be an obstructive process in the ventricles or in the subarachnoid space, less often - true hyperproduction of cerebrospinal fluid (with villous plexus papilloma) • Characterized by excessive accumulation of cerebrospinal fluid in the ventricles of the brain or subarachnoid space with their expansion • In newborns it leads to an increase in the size of the skull and brain atrophy ( decreased metabolism in adjacent areas of the brain). Code according to the international classification of diseases ICD-10: Classification. By the presence of communication between the cavities of the ventricles of the brain and the subarachnoid space. • Non-communicating (obstructive) hydrocephalus is caused by a process that causes blockage of the ventricular system •• Acquired hydrocephalus ••• Tumors of the IV ventricle (medulloblastoma, ependymoma - with them all ventricles are dilated) and the Sylvian aqueduct (glioma of the midbrain tegmentum - the lateral and III ventricles are dilated, and the size of the IV ventricle is not changed) ••• Fibrosis of the arachnoid membrane due to meningitis or intraventricular hemorrhage •• Congenital hydrocephalus ••• Stenosis of the aqueduct of Sylvius in the presence of a septum and true narrowing (#307000, Xq28, L1 cell adhesion molecule gene L1CAM, 308840, À) . Congenital stenosis is characterized by a small size of the posterior cranial fossa. ••• Dandy-Walker syndrome is congenital atresia of the foramina of Magendie and Luschka. Characterized by cystic dilatation of the IV ventricle and cerebellar hypoplasia ••• Vein of Galen aneurysms (v. cerebri magna - Galeni) and other vascular malformations ••• Benign intracranial cysts (arachnoid and ependymal) ••• X-linked hydrocephalus is rare a form of congenital hydrocephalus in men. • Communicating (non-obstructive) hydrocephalus occurs when there is an obstruction in the cerebrospinal fluid circulation pathways distal to the exit from the fourth ventricle and at the level of the pachyonic granulations •• Acquired ••• Inflammation of the arachnoid membrane during meningitis and as a result of intraventricular hemorrhage (most often with birth trauma and in premature infants) • •• Venous thrombosis, stenosis of the dural sinuses ••• Trauma accompanied by subarachnoid hemorrhage, followed by inflammation of the arachnoid membrane ••• Normotensive hydrocephalus •• Congenital ••• Inflammation of the arachnoid membrane - intrauterine infection ••• Encephalocele ••• Agyria - developmental anomaly: absence of convolutions of the cerebral cortex; the cranial cavity is filled with cerebrospinal fluid. Separately, functional hydrocephalus is distinguished, which develops as a result of excessive formation of cerebrospinal fluid with villous plexus papilloma. This tumor may also itself obstruct the ventricular system, causing obstructive hydrocephalus. Small hemorrhages from it cause obstruction of the subarachnoid space (after removal of the tumor, hydrocephalus may persist). According to the predominant accumulation of cerebrospinal fluid • Internal (ventricular) hydrocephalus - hydrocephalus, characterized by the accumulation of cerebrospinal fluid mainly in the ventricles of the brain • External hydrocephalus - hydrocephalus with accumulation of cerebrospinal fluid predominantly in the subarachnoid space or (less often) in the subdural space in the presence of communication between the subarachnoid and subdural spaces • General hydrocephalus - hydrocephalus with accumulation of cerebrospinal fluid both in the ventricles and in the subarachnoid space. Symptoms (signs)Clinical picture • At the initial manifestations of the disease, the child becomes restless, then low mobility and poor appetite appear • A progressive increase in head circumference (up to 60 cm or more), thinning of the skin, dilation of the veins of the scalp • Divergence of the cranial sutures, tension, enlargement and bulging of the fontanelles , absence of their pulsation • Symptoms of intracranial hypertension due to the compliance of the skull in newborns and young children are not clearly expressed • With a significant increase in ICP - a symptom of the setting sun (the child’s eyes look down, the lower part of the iris is covered, a wide strip of sclera is visible from above; gaze paresis up) • The sound of a “cracked pot” during percussion of the skull • Swelling of the optic discs, subsequent decrease in visual acuity due to atrophy • Damage to the motor sphere: increased reflexes from the lower extremities, later - paresis • Developmental indicators lag behind normal, in advanced cases mental illness is inevitable retardation • A disease that occurs after 17–18 years of age is not accompanied by an increase in head size; signs of intracranial hypertension come to the fore. DiagnosticsResearch methods • X-ray of the skull: dehiscence of the sutures of the skull, deepening of finger-like impressions, thinning of bones (with prolonged hypertension), intracranial calcifications (as a result of congenital infections). Small sizes of the posterior cranial fossa suggest stenosis of the Sylvian aqueduct, large ones - Dandy-Walker syndrome • Ultrasound (neurosonography) indicates the degree of ventricular dilatation, intraventricular hemorrhage • CT helps determine the size of the ventricles, the location of obstruction of the cerebrospinal fluid pathways, and allows to identify associated anomalies • MRI is the most informative , indicated for the combination of hydrocephalus with tumors, vascular malformations, and multi-chamber ventricles • Angiography helps to identify vascular anomalies • If a congenital infection is suspected, serological tests are performed for rubella, herpes, CMV, Toxoplasma gondii and Treponema pallidum viruses. Differential diagnosis • Congenital macrocrania (normal head growth rate and family history of macrocrania) • Enlarged head with rickets (overgrowth of bone tissue of the skull and skeletal changes typical for rickets) • Volumetric intracranial formations (subdural hematomas, tumors). |
Diagnostics
The clinical symptoms of hydrocephalus are usually so characteristic that they allow the neurologist to suspect its presence during the first examination of the patient. To determine the degree and form of hydrocephalus, as well as to identify the underlying disease, additional examinations are performed: radiography, ultrasound, computed tomography or magnetic resonance imaging. X-rays of the skull in the case of hydrocephalus reveal thinning of the skull bones and divergence of the sutures between them; On the inner surface of the cranial vault, a symptom of “finger impressions” is observed. Hydrocephalus, caused by stenosis of the cerebral aqueduct, is accompanied by a decrease in the volume of the posterior cranial fossa on radiographs of the skull. Hydrocephalus with Dandy-Walker syndrome, on the contrary, is characterized by an increase in the volume of the posterior cranial fossa on craniograms. Hydrocephalus when one of the interventricular communications is closed is manifested by the asymmetry of the skull visible on the craniogram. However, in modern clinical practice, with the availability of more informative research methods, such as MRI, MSCT and CT of the brain, radiography has only an auxiliary value in the diagnosis of hydrocephalus. Among the ultrasound diagnostic methods for hydrocephalus, echoencephalography is used, which allows one to determine the degree of increase in intracranial pressure. In children of the first year of life, ultrasound scanning of the brain through an open fontanelle using ultrasonography is possible. An ophthalmologist assesses visual disturbances and the condition of the optic discs. As a rule, the list of ophthalmological examinations for hydrocephalus includes ophthalmoscopy, determination of visual acuity and perimetry. Tomographic diagnostic methods make it possible to determine the nature of hydrocephalus, identify the location of cerebrospinal fluid tract occlusion or an existing congenital anomaly, and diagnose the causative disease (tumor, cyst, hematoma). In case of hydrocephalus, the most informative use of MRI of the brain. In the absence of contraindications, to identify the causative disease, it is possible to perform a lumbar puncture followed by examination of the cerebrospinal fluid. If vascular disorders are suspected, MRA of cerebral vessels is indicated. Congenital hydrocephalus of infectious etiology requires PCR diagnostics to determine the type of infection that caused it.
Signs of illness
The main sign suggesting dropsy in a child is an increase in the size of the head. The following symptoms may also occur:
- breathing problems;
- frozen, prone to contraction muscles of the arms and legs;
- delay in the development of certain stages, for example, a child cannot learn to sit or crawl;
- bulging fontanelles, changing their shape;
- loss of appetite;
- refusal to move the head;
- The scalp is thin, veins are visible.
Congenital hydrocephalus in children can be manifested by a violation of the location of the pupil; it is located close to the lower part of the eyelid. This symptom is called the “setting sun symptom.” Convulsions and vomiting may also occur.
Treatment
The choice of treatment for hydrocephalus depends on its etiology. Conservative therapy is often carried out for acquired hydrocephalus caused by inflammatory diseases, previous TBI, or hemorrhage into the ventricles. The underlying disease is treated, and diuretics (acetazolamide, furosemide) are prescribed to reduce the degree of hydrocephalus and increased intracranial pressure. Congenital hydrocephalus usually requires surgery to correct the underlying malformation. If hydrocephalus is caused by the presence of a space-occupying process in the brain, then it can also be treated surgically. According to indications, removal of intracranial hematoma, surgery to remove tumors, opening or total excision of a brain abscess, separation of adhesions in arachnoiditis, etc. are performed. In cases where it is not possible to eliminate the cause of hydrocephalus, shunt operations are used: cystoperitoneal shunting, endoscopic ventriculocisternostomy of the bottom of the third ventricle, ventriculoperitoneal shunting, lumboperitoneal shunting, external ventricular drainage. They are aimed at creating additional pathways for the outflow of cerebrospinal fluid from the cranial cavity. Shunt operations can be performed as an addition to surgical treatment of the underlying disease if the operation fails to restore normal circulation of the cerebrospinal fluid.
Prevention
To prevent congenital hydrocephalus, pregnant women are carefully examined, especially if they are at risk. Women are advised to follow their daily routine, avoid stressful situations and overwork. Measures are also being taken to prevent infectious pathologies such as meningitis, encephalitis, syphilis and other diseases that lead to infection of the fetus and its abnormal development.
Newborns must undergo transcranial ultrasonography. This diagnostic procedure is done on the first day of life to exclude hemorrhages and congenital malformations of the central nervous system. When verifying intraventricular hemorrhages, neurosonographic monitoring is carried out every day.
When ventriculomegaly increases, children should be in intensive care under constant supervision. In some cases, it is advisable to immediately perform ventriculosubgaleal drainage in order to evacuate the cerebrospinal fluid.
In pediatric surgery, the most minimally traumatic method in the treatment of hydrocephalus is endoscopic ventriculostomy, which is performed for children over one year of age.
Description
Hydrocephalus. Increased accumulation of cerebrospinal fluid in the cerebrospinal fluid system of the brain. Hydrocephalus accompanies many congenital and acquired neurological diseases. Clinically, it is manifested by signs of increased intracranial pressure (headache, nausea, pressure on the eyes), symptoms of compression of brain structures (vestibular ataxia, visual impairment, mental disorders, epileptic seizures) and symptoms characteristic of the disease that caused it.
Diagnosis of hydrocephalus includes radiography of the skull, ophthalmological studies, echo-EG (in infants - neurosonography), MRI or CT scan of the brain. Surgical treatment of hydrocephalus allows you to correct congenital anomalies of the cerebrospinal fluid system, remove intracranial formations that disrupt the circulation of the cerebrospinal fluid, and establish the outflow of cerebrospinal fluid from the cranial cavity.
Symptoms by age
Typical symptoms of hydrocephalic syndrome are visual disturbances
Symptoms are caused by intracranial hypertension and hydrocephalus.
General signs of HS:
- nausea;
- vomit;
- headache;
- personality changes or epileptic seizures.
However, in children and adults, the symptoms of hydrocephalic syndrome differ significantly.
In infants
In a child under one year old with hydrocephalic syndrome, decreased muscle tone, weak tremor, and a positive Graefe sign (“setting sun”) are noted.
There is an increased increase in head circumference (about 1-2 cm monthly). The baby's head looks disproportionately large.
Sometimes a baby with hydrocephalic syndrome exhibits swelling of the optic disc.
In children and adolescents
Symptoms of HS in adolescents and children;
- visual impairment (strabismus, loss of visual field), decreased visual acuity to the point of blindness;
- fine motor skills disorders;
- disturbances in concentration;
- personality changes, behavioral problems (anxiety, impatience, categoricalness), hypersensitivity to noise;
- respiratory, speech and swallowing disorders;
- endocrinological (metabolic) disorders;
- early puberty before 8 years of age (very rare).
In adults
Symptoms of HGS in adult patients:
- cephalalgia, vomiting, dizziness in the morning;
- visual impairment (diplopia - double vision);
- convulsive conditions;
- severe fatigue;
- restless behavior.
Additional facts
Hydrocephalus literally means “dropsy of the head.” In modern neurology, this is a common clinical syndrome that can be observed in many diseases, congenital anomalies or post-traumatic conditions of the brain. The occurrence of hydrocephalus is associated with certain disorders in the cerebrospinal fluid system of the brain.
People of any age are susceptible to hydrocephalus. Hydrocephalus can occur in newborns, be congenital, develop in children and adults, and accompany atrophic processes occurring in the brain in old people. However, it is most often encountered in pediatric practice.
How is hydrocephalus treated?
Hydrocele of the brain often requires surgical treatment, performed under general anesthesia. Specialists resort to the following types of surgical intervention:
- palliative,
- radical.
During palliative surgery, a spinal or ventricular puncture is performed. For the treatment of young children, excess fluid is removed through the eye socket. Radical surgical methods include ventriculoperitoneal shunting, Küttner Wenglovsky's operation, and ventriculocisternostomy.
Treatment of cerebral hydrocele using medications brings positive results only in 40-45% of cases; it becomes relevant with small volumes of fluid and moderately high intracranial pressure.
For younger patients, diuretics are prescribed:
- Furosemide.
- Mannitol.
- Diacarb.
For the treatment of hydrocephalus of the brain in adults, magnesium sulfate and Asparkam are used. Antibiotic therapy, taking vitamin and absorbable medications, physiotherapy, and exercise therapy become mandatory.
In most cases, surgical treatment allows the patient to achieve complete recovery. If the cause of hydrocele in the brain is an aggressive cancerous tumor, timely surgery can prolong the patient’s life by several years.
Anatomy and pathological anatomy
Normally, cerebrospinal fluid (CSF) is produced by the choroid plexus of interconnected ventricles of the brain. The largest amount of it is formed in the lateral ventricles, from where the cerebrospinal fluid enters the third ventricle, and from it through the Sylvian aqueduct into the fourth ventricle. Then the cerebrospinal fluid enters the subarachnoid (subarachnoid) space, which extends over the entire surface of the brain, and in the caudal direction passes the region of the craniovertebral junction and then surrounds the spinal cord along its entire length.
Why is hydrocephalic syndrome dangerous?
Complications of hydrocephalic syndrome can negatively affect both the physical and mental state, which significantly reduces the patient's quality of life and can cause serious consequences.
There is often a strong increase in pressure in the skull, which can lead to headaches. In many cases, the pain spreads to other areas of the body.
Patients suffer from visual disturbances (nystagmus or diplopia).
In severe cases, epileptic seizures occur.
As the disease progresses, paralysis or sensory disturbances (neuropathy) may occur.
Sometimes gait disturbances occur.
The patient's daily functioning suffers. Patients often lose consciousness or fall into a coma.
Complications usually only occur if treatment is started too late or permanent brain changes occur.
Causes
Three pathological mechanisms lead to the accumulation of an excess amount of cerebrospinal fluid in the cerebrospinal fluid system of the brain: the production of an excess amount of cerebrospinal fluid, a violation of its absorption, or a disorder of the cerebrospinal fluid circulation. Hydrocephalus may be based on one of these mechanisms or a combination of them.
The causes that cause disturbances in the functioning of the cerebrospinal fluid system can act during fetal development and cause congenital hydrocephalus or affect the brain after birth and cause the appearance of so-called acquired hydrocephalus. The causes of congenital hydrocephalus include malformations of the cerebrospinal fluid system (atresia of the foramina of Magendie and Luschka, defects in the structure of the subarachnoid space, stenosis of the Sylvian aqueduct, Dandy-Walker syndrome, etc.
), craniovertebral anomalies (Chiari malformation, congenital basilar impression), intrauterine infections (toxoplasmosis, congenital syphilis, cytomegaly, rubella), birth trauma. Acquired hydrocephalus can occur as a result of inflammatory processes in the brain and its membranes (encephalitis, arachnoiditis, meningitis), traumatic brain injury, vascular disorders (bleeding into the ventricles, hemorrhagic stroke or intracerebral hematoma with blood breaking into the ventricles).
Hydrocephalus often develops against the background of a colloid cyst of the third ventricle and intracerebral tumors (astrocytomas, germinomas, ganglioneuromas, etc.), which grow into the ventricles of the brain or compress the cerebrospinal fluid pathways, thereby disrupting the normal circulation of cerebrospinal fluid and its outflow from the cranial cavity. Separately, there is an atrophic (replacement) form of hydrocephalus, which occurs as a result of post-traumatic death or age-related atrophy of brain tissue.
In this case, cerebrospinal fluid fills the space that is formed inside the skull as a result of a decrease in the volume of the brain. Atrophic hydrocephalus in old age can develop against the background of impaired blood supply to the brain due to atherosclerosis of cerebral vessels, hypertension, and diabetic macroangiopathy.
Types of hydrocephalus
Hydrocephalus, which develops in patients of different ages, can be:
- open,
- non-occlusive,
- aresorptive,
- biventricular,
- atrophic.
Open hydrocephalus is caused by slow absorption of cerebral fluid into the blood. The result is unbalanced production and resorption of cerebrospinal fluid, which the body restores due to increased pressure inside the skull.
Non-occlusive hydrocephalus leads to overflow of the cerebral ventricles with cerebrospinal fluid. With this type of pathology, a liquid substance accumulates in the ventricular system, or fills the subdural and subarachnoid space.
Aresorptive hydrocephalus tends to affect adults. With this type, the venous sinuses do not absorb enough cerebrospinal fluid. Biventricular hydrocephalus is caused by the closure of the openings in the 3rd ventricle.
The atrophic form of cerebral hydrocele is caused by a reduction in brain volume. This type of disease is mainly diagnosed in elderly people susceptible to hypertension, diabetic angiopathy, and atherosclerosis.
In addition to the listed forms of the disease, there is a mixed type of hydrocephalus - the accumulation of cerebrospinal fluid in several areas at once.
Classification
According to the etiological principle, congenital and acquired hydrocephalus are distinguished. According to the mechanism of occurrence, hydrocephalus is classified into open and closed forms. Open hydrocephalus is associated with overproduction of cerebrospinal fluid or impaired absorption during normal cerebrospinal fluid circulation. Closed hydrocephalus is caused by a violation of the outflow of cerebrospinal fluid due to compression, partial or complete obstruction of any part of the cerebrospinal fluid system of the brain.
Depending on where the excess accumulation of cerebrospinal fluid occurs, internal and external hydrocephalus are distinguished. Internal hydrocephalus is accompanied by the accumulation of cerebrospinal fluid in the ventricles of the brain. External hydrocephalus is characterized by excess cerebrospinal fluid in the subarachnoid and subdural space. According to the characteristics of its course, hydrocephalus is classified as acute, subacute and chronic.
Acute hydrocephalus is characterized by rapid development, in which decompensation occurs a few days after the onset of the first signs of the disease. Subacute hydrocephalus develops within a month, and chronic hydrocephalus develops over six months. Of great clinical importance is the division of hydrocephalus into stabilized (compensated) and progressive (increasing).
History[ | ]
Hydrocephalus was rarely described in ancient medical literature, although its existence and symptoms were well known. The father of medicine, Hippocrates, is considered the first physician to attempt to document the treatment of hydrocephalus. He recommended trephination to treat epilepsy, blindness and possibly hydrocephalus. The Greeks reportedly treated hydrocephalus by wrapping bark around the patient's head and inserting it into burr holes.
Evacuation of superficial intracranial fluid in children with hydrocephalus was first described in detail by Ibn Sina {Avicenna}. Due to poor understanding of the pathophysiology of hydrocephalus, initial attempts at therapy were sporadic and usually failed. Many practitioners relied on conservative therapy. Treatment attempts included a variety of drugs, laxatives such as rhubarb, calomel and oil, as well as various diuretics, head wraps, bloodletting and craniotomy[2].
Symptoms
The accumulation of excess cerebrospinal fluid in a limited space of the cranium leads to increased intracranial pressure, which causes the most typical symptoms of hydrocephalus. In adults and older children, these include: intense headache that cannot be relieved by analgesics, nausea, vomiting, and a feeling of pressure on the eyeballs.
These symptoms may occur acutely or increase gradually, being transient at the onset of the disease. Atrophic hydrocephalus often occurs without signs of increased intracranial pressure and is detected only with additional examination of the patient. In most cases, hydrocephalus is accompanied by neurological symptoms, which are caused both by compression of brain structures by expanded cerebrospinal fluid spaces and by the underlying disease that causes the development of hydrocephalus.
The most common symptoms of hydrocephalus are vestibular and visual disturbances. The first includes vestibular ataxia, manifested by dizziness, unsteady gait, noise in the ears and head, and nystagmus. On the visual side, there may be a significant decrease in visual acuity, loss of certain areas of the visual fields, congestive optic discs;
with prolonged hydrocephalus, atrophy of the optic nerves may develop. Hydrocephalus can occur with disturbances in the motor and sensory sphere: paresis and paralysis, increased tendon reflexes and muscle tone, decreased or complete loss of all types of sensitivity, and the formation of spastic contractures of the limbs.
Occlusive hydrocephalus, caused by impaired circulation of cerebrospinal fluid in the posterior cranial fossa, is characterized by symptoms of cerebellar ataxia: impaired coordination and gait, large-scale disproportionate movements, changes in handwriting, etc. In children, due to the high compliance of the skull bones, there is no increase in intracranial pressure; they have hydrocephalus accompanied by an increase in the size of the skull.
In newborns and young children, hydrocephalus is characterized by an overly large head size, bulging scalp veins, tension and lack of pulsation of the large fontanel, and swelling of the optic discs. The symptom of “setting sun” is often noted - restriction of upward movements of the eyeballs.
There may be dehiscence of the sutures of the skull. Tapping on the skull is accompanied by a characteristic sound (the “cracked pot” symptom). In children in the first year of life, hydrocephalus leads to developmental delays. They later begin to hold their head up, roll over, sit up and walk. Children who have severe hydrocephalus are distinguished by a spherical shape of the head, its too large size, deep-set eyes, protruding ears, and thinning of the scalp.
There may be decreased vision, increased muscle tone in the lower extremities, and disorders of the cranial nerves. Unlike adults, in childhood hydrocephalus is often accompanied not by emotional-volitional disorders, but by intellectual deficiency. Children with hydrocephalus are usually sedentary and obese.
Hydrocephalus in children :: Symptoms, causes, treatment and code according to ICD-10
Title: Hydrocephalus in children.
Hydrocephalus in children
Hydrocephalus in children.
Excessive accumulation of cerebrospinal fluid in the cerebrospinal fluid pathways of the brain, due to its increased production, impaired circulation or resorption.
Hydrocephalus in children is characterized by bulging fontanelles, divergence of bone sutures, increased head circumference, swelling of the saphenous veins of the head, exophthalmos, retardation in physical and psychomotor development, and signs of increased intracranial pressure.
Diagnosis of hydrocephalus in children includes NSG, Echo-EG, skull radiography, CT or MRI of the brain, radionuclide cisternography. Treatment of hydrocephalus in children can be conservative or surgical (endoscopic coagulation of the choroid plexus, ventriculostomy, CSF shunt surgery, etc.).
Hydrocephalus in children (“dropsy of the brain”) is caused by excessive accumulation of cerebrospinal fluid in the cerebrospinal fluid pathways (brain ventricles, basal cisterns, subarachnoid space), which leads to their expansion, increased intracranial pressure and compression of brain structures.
In child neurology and pediatrics, congenital hydrocephalus occurs in 1-4 children per 1000 newborns. In addition, hydrocephalus in children can accompany inflammatory processes of the nervous system (15-25%), birth and traumatic brain injuries (30-40%), brain tumors (75%).
The progressive accumulation of cerebrospinal fluid in the cranial cavity leads to atrophic changes in brain tissue, pronounced neurological and mental disorders in a child with hydrocephalus.
Hydrocephalus in children Hydrocephalus in children is classified depending on the etiological, morphological, clinical signs, and the level of cerebrospinal fluid pressure. Taking into account the polyetiological nature of hydrocephalus in children, it can be congenital, post-infectious, post-traumatic, associated with a tumor process or cerebrovascular pathology; sometimes the causes of hydrocephalus remain unspecified. According to morphological criteria, communicating (open) and occlusive (closed) hydrocephalus in children is distinguished. With open hydrocephalus, there is a discrepancy between the processes of formation (production) and absorption (resorption) of cerebrospinal fluid, while the ventricular and subarachnoid spaces communicate freely with each other. Depending on the mechanism of the disorder, there are hyperproductive, aresorptive, and mixed forms of open hydrocephalus in children with a predominance of production over resorption. Cases of occlusive hydrocephalus in children are associated with occlusion of the cerebrospinal fluid spaces at various levels, which is accompanied by their separation and expansion. Also, based on morphological characteristics, hydrocephalus in children is divided into intraventricular (internal), subarachnoid (external) and mixed.
Taking into account the level of cerebrospinal fluid pressure, hydrocephalus in children can be normotensive, hypertensive or hypotensive. According to the clinical course, hydrocephalus in children can be compensated, subcompensated, or decompensated; progressive, stabilized or regressing.
True congenital hydrocephalus in children is caused by abnormalities in brain development: primary stenosis or atresia of the cerebral aqueduct, Arnold-Chiari malformation type 1 or 2, Dandy-Walker syndrome, arachnoid cysts, hypoplasia of the subarachnoid spaces, abnormalities of the cerebral venous system (congenital aneurysm of the vein of Galen, etc.). Stenosis of the Sylvian aqueduct causes congenital hydrocephalus in 30% of all cases. Congenital hydrocephalus in children can be caused by intrauterine infections (toxoplasmosis, cytomegaly, rubella, herpes, congenital syphilis), thrombophlebitis of the veins and sinuses of the brain, and brain injuries. In the postnatal period, post-infectious hydrocephalus in children can occur due to bacterial meningitis, arachnoiditis, and encephalitis. The causes of post-traumatic hydrocephalus in children are usually intracranial birth injuries (subarachnoid, intraventricular hemorrhages) and traumatic brain injuries. The occurrence of hydrocephalus of tumor origin can be caused by the presence of papilloma, carcinoma, meningioma of the choroid plexus, ventricular tumors, tumors of the skull and spinal cord. Hydrocephalus associated with arteriovenous malformations of the brain occurs in childhood. Risk factors for the development of hydrocephalus in children are premature birth (up to 35 weeks), prematurity (weight less than 1500 g), narrow pelvis in the mother, the use of active obstetric aids, fetal hypoxia and asphyxia of newborns, pulmonary hypertension and other pathological conditions.
Violation of cerebrospinal fluid dynamics in hydrocephalus in children causes secondary changes in the brain, meninges, soft integument and skull bones. Pathological changes are represented by expansion of the ventricular cavities, flattening of the convolutions, smoothing of the furrows; atrophy of the choroid plexuses; edema, fibrosis, fusion of the meninges, etc.
Hydrocephalus in children can appear in the first days of life or develop later, at any age. The severity of symptoms of hydrocephalus in children is influenced by its form, rate of progression, the presence of intracranial hypertension syndrome, and the underlying disease. Severe forms of hydrocephalus associated with gross developmental disorders often cause the death of a child in the neonatal period. Early accompaniments of hydrocephalus in children may include restless behavior, tearfulness (monotonous crying “on one note”), and frequent heavy regurgitation. The main objective sign of hydrocephalus in children is the rapid rate of increase in the circumference of the head and its disproportionately large size, determined by anthropometry. During an external examination, attention is drawn to the bulging of the fontanelles, the divergence of the cranial sutures, the tension of the subcutaneous venous network of the head, and sparse hair growth. Children with hydrocephalus have a large head with a relatively small body, a small face with an overhanging forehead, and deeply located eye sockets. Neurological disorders in children with hydrocephalus may include nystagmus, symmetrical spastic paraplegia of the upper or lower extremities, and convulsive syndrome. Often there is exophthalmos, ptosis, Graefe's symptom (divergent strabismus with a downward displacement of the eyeballs - “setting sun symptom”). With hydrocephalus, children are delayed in motor development: they begin to hold their heads, roll over, sit and crawl late. The degree of intellectual impairment in children with hydrocephalus can vary from mild debility to idiocy.
Tearfulness. Vomit. Cramps. Nausea.
Using prenatal diagnostic methods (determination of alpha-fetoprotein in the pregnant woman's serum and amniotic fluid), hydrocephalus in the fetus can be detected already from the first trimester of pregnancy. Fetal ultrasound can detect hydrocephalus in a child at 16–20 weeks of pregnancy. In these cases, the issue of termination of pregnancy is decided. After birth, some children have hydrocephalus immediately detected in the maternity hospital by a neonatologist. In children in the first months of life, a reason that makes one think about hydrocephalus is an excess of the head circumference by 2 cm compared to the age norm. If such a tendency is detected, the pediatrician should refer the child to a pediatric neurologist or neurosurgeon for further diagnosis. Transillumination (diaphanoscopy) of the skull makes it possible to identify external hydrocephalus in children and exclude hydroanencephaly and subdural hygroma. In children under the age of 1 year, neurosonography is performed through the fontanel to assess the condition of the cerebrospinal fluid ducts. Using craniography, an increase in the size of the skull, divergence of sutures, and digital impressions are detected. The widespread introduction of brain CT has significantly narrowed the indications for skull radiography, ventriculography, pneumoencephalography, and radionuclide diagnosis of hydrocephalus in children. Computed tomography gives an idea of the state of the brain matter, liquor-containing cavities, the form and severity of hydrocephalus in children. For occlusive processes, the method of choice is MRI of the brain. Ancillary methods of neurological diagnostics include echoencephalography, EEG, and MR angiography of cerebral vessels. Children with hydrocephalus are advised to consult a pediatric ophthalmologist with ophthalmoscopy to timely identify the initial signs of optic nerve atrophy.
To assess the pressure of the cerebrospinal fluid, study its composition and conduct liquorodynamic tests, they resort to ventricular and lumbar punctures.
The basic principles of treatment of hydrocephalus in children are to reduce the production of CSF and normalize its circulation along the liquor-carrying pathways, including through the creation of bypass anastomoses. In order to reduce liquor production and intracranial pressure, dehydration therapy with diuretics, carbonic anhydrase inhibitors, and saluretics is carried out. With a progressive increase in hydrocephalus in children over 2-3 months (and sometimes earlier), the question of surgical intervention is raised. The optimal method of surgical intervention is determined by the etiology, form, and stage of hydrocephalus in children. Currently, all types of operations for hydrocephalus in children can be divided into 5 groups: • palliative interventions that temporarily reduce intracranial pressure and eliminate craniocerebral disproportion (lumbar and ventricular punctures, external ventricular drainage). • operations aimed at suppressing liquor production (clipping, coagulation of the choroid plexus). • operations aimed at restoring natural pathways of cerebrospinal fluid circulation or creating new pathways for cerebrospinal fluid outflow (removal of tumors, intracranial hematomas, ventriculostomy). • operations that activate liquor sorption (dissection of arachnoid adhesions, etc.).
• shunt operations involving the diversion of cerebrospinal fluid to other systems of the body (ventriculoperitoneal shunting, lumboperitoneal shunting, ventriculoatrial shunting, ventriculocisternostomy, cystoventriculoperitoneostomy, subduroperitoneostomy).
If it is impossible to perform standard shunting operations, atypical shunting interventions are performed - ventriculopleural, ventriculourethral ventriculobiliary shunting.
CSF shunt operations for hydrocephalus in children are associated with the risk of disruption of the functioning of drainage systems, overdrainage or inflammatory complications.
The possibility of curing hydrocephalus in children, prospects for the life and health of the child depend on a number of factors: causes, form of the disease, timeliness of diagnosis, success of conservative or surgical treatment. Overall, proper treatment is effective in about half of the cases. Acquired hydrocephalus in children has a worse prognosis than congenital hydrocephalus.
Recommendations for the prevention of hydrocephalus in children include careful pregnancy planning, early prenatal diagnosis, prevention of birth injuries, and monitoring of children at risk by a pediatrician and pediatric neurologist.
42a96bb5c8a2ac07fc866444b97bf1 Content moderator: Vasin A.S.
Source: https://kiberis.ru/?p=32724
Diagnostics
The clinical symptoms of hydrocephalus are usually so characteristic that they allow the neurologist to suspect its presence during the first examination of the patient. To determine the degree and form of hydrocephalus, as well as to identify the underlying disease, additional examinations are performed: radiography, ultrasound, computed tomography or magnetic resonance imaging.
X-rays of the skull in the case of hydrocephalus reveal thinning of the skull bones and divergence of the sutures between them; On the inner surface of the cranial vault, a symptom of “finger impressions” is observed. Hydrocephalus, caused by stenosis of the cerebral aqueduct, is accompanied by a decrease in the volume of the posterior cranial fossa on radiographs of the skull.
Hydrocephalus with Dandy-Walker syndrome, on the contrary, is characterized by an increase in the volume of the posterior cranial fossa on craniograms. Hydrocephalus when one of the interventricular communications is closed is manifested by the asymmetry of the skull visible on the craniogram. However, in modern clinical practice, with the availability of more informative research methods, such as MRI, MSCT and CT of the brain, radiography has only an auxiliary value in the diagnosis of hydrocephalus.
Among the ultrasound diagnostic methods for hydrocephalus, echoencephalography is used, which allows one to determine the degree of increase in intracranial pressure. In children of the first year of life, ultrasound scanning of the brain through an open fontanelle using ultrasonography is possible. An ophthalmologist assesses visual disturbances and the condition of the optic discs.
As a rule, the list of ophthalmological examinations for hydrocephalus includes ophthalmoscopy, determination of visual acuity and perimetry. Tomographic diagnostic methods make it possible to determine the nature of hydrocephalus, identify the location of cerebrospinal fluid tract occlusion or an existing congenital anomaly, and diagnose the causative disease (tumor, cyst, hematoma).
https://www.youtube.com/watch?v=ytdevru
In case of hydrocephalus, the most informative use of MRI of the brain. In the absence of contraindications, to identify the causative disease, it is possible to perform a lumbar puncture followed by examination of the cerebrospinal fluid. If vascular disorders are suspected, MRA of cerebral vessels is indicated. Congenital hydrocephalus of infectious etiology requires PCR diagnostics to determine the type of infection that caused it.
Symptoms[ | ]
A child with hydrocephalus
The most characteristic sign of hydrocephalus in newborns is rapid growth of head circumference, leading to a visually well-defined hydrocephalic shape of the skull, greatly increased in volume. Signs of hydrocephalus include a bulging, tense fontanelle, frequent tilting of the head, and a downward displacement of the eyeballs. In places where normal fusion of the skull bones has not occurred, rounded pulsating protrusions may form. Strabismus and nystagmus often occur. There is high excitability due to headaches, the child does not eat well, often cries, vomits, and is lethargic. Sometimes you may notice a decrease in vision and hearing.
Hydrocephalus in older age is characterized by headaches, especially in the morning, nausea and vomiting at the height of headache, dizziness; the size of the head is not increased. X-rays of the skull show destruction of the sella turcica and increased digital impressions. The most informative are magnetic resonance and computed tomography, which reveal sharply enlarged ventricles of the brain.
Tree of ICD-10 diagnoses
• Diseases of the nervous system.
- G00-G09 Inflammatory diseases of the central nervous system (Selected ICD-10 diagnosis)
- Subsections:
- G00 Bacterial meningitis, not elsewhere classified
- G01 Meningitis in bacterial diseases classified elsewhere
- G02 Meningitis in other infectious and parasitic diseases classified elsewhere
- G03 Meningitis due to other and unspecified causes
- G04 Encephalitis, myelitis and encephalomyelitis
- G05 Encephalitis, myelitis and encephalomyelitis in diseases classified elsewhere
- G06 Intracranial and intravertebral abscess and granuloma
- G07 Intracranial and intravertebral abscess and granuloma in diseases classified elsewhere
- G09 Consequences of inflammatory diseases of the central nervous system
- Related codes:
- G10-G13 Systemic atrophies affecting predominantly the central nervous system
- G20-G26 Extrapyramidal and other movement disorders
- G30-G32 Other degenerative diseases of the nervous system
- G35-G37 Demyelinating diseases of the central nervous system
- G40-G47 Episodic and paroxysmal disorders
- G50-G59 Lesions of individual nerves, nerve roots and plexuses
- G60-G64 Polyneuropathies and other lesions of the peripheral nervous system
- G70-G73 Diseases of the neuromuscular junction and muscles
- G80-G83 Cerebral palsy and other paralytic syndromes
- G90-G99 Other nervous system disorders
- G999* Diagnosis of diseases of the nervous system
• CNS infections. • Brain damage of an infectious-inflammatory nature.
Clinical picture
Symptoms indicating the development of normal pressure hydrocephalus:
- walking disorder (frontal apraxia): slower walking, shorter strides, decreased step height;
- impairment of cognitive abilities, reminiscent of signs of dementia - apathy, decreased concentration, loss of interest, memory problems, psychomotor slowing in general;
- incontinence disorder – first, intermittent disturbances in urinary continence up to incontinence, including fecal incontinence.
Symptoms can be expressed in different ways. Most often, gait disturbances appear first, which precedes cognitive disorders, and continuation disorders develop last.
Additional symptoms that may be present (headaches, tinnitus, psychoaffective disorders) are not typical, but do not exclude the diagnosis of NG. As a rule, they are typical for patients over 60 years of age, which is why these clinical manifestations can be attributed to aging and their occurrence may be underestimated by the attending physician.
Basic medical services according to treatment standards Select treatment using artificial intelligence
Doctor consultations | |
| Consultation with a surgeon any doctor – 811 clinic doctor Ph.D. – 261 clinics, medical sciences, professor – 163 clinics, ramn – 3 clinics | |