Causes
Hypertension or persistent arterial hypertension is the most common cause of hemorrhage in the ventricles of the brain. People suffering from atherosclerosis, blood diseases, and inflammation of the blood vessels in the brain are also susceptible to stroke.
Hemorrhage (blood leakage outside the vessels) is based on functional and organic changes in brain circulation. When blood pressure is constantly elevated or a hypertensive crisis occurs (a sudden and strong increase in blood pressure to 200/100), disorders associated with vascular tone occur. The walls of blood vessels are disorganized: penetration for solid elements of blood and plasma increases. Diapedesis occurs - the formation of formed elements outside the arteries.
The pathology is complicated by the fact that, as a rule, not just one vessel is damaged, but the entire brain network, which is why massive focal hemorrhages in the ventricles occur. Here a vicious circle is activated: a protective mechanism is triggered, in which the vessels dilate and lose their ability to spasm. The dilation of the arteries further enhances the permeability of plasma and red blood cells, which increases the amount of blood released.
In addition, when diapedetic hemorrhage occurs, blood clotting mechanisms are disrupted. In a normal wound, platelets and coagulation mechanisms are automatically sent to the site of bleeding, where they “patch” the wound. However, with hemorrhage into the ventricles, this process is switched off.
The ventricles are a hollow system connected by channels, so blood from one cavity of the ventricle gradually flows into another - this complicates the course of the pathology. In this case, bilateral neurological symptoms develop with the participation of symmetrical parts of the brain and ventricles.
A breakthrough of blood into the ventricles, namely III and IV, ends in death. Filling of the lateral ventricles has a favorable prognosis.
Classification
The classification of hemorrhages in the ventricles of the brain was developed more than 20 years ago and included in the International Classification of Diseases, 10th revision. According to ICD-10, IVH is divided into several stages: subependymal hemorrhage (SEH), SEC with spread to the lateral ventricles of the brain, SEC with spread to the ventricles and the substance of the brain. In clinical practice, specialists in the field of neurology distinguish 3 types of hemorrhages in the ventricles of the brain: hemorrhage in the lateral ventricles, in the third ventricle and in the fourth ventricle.
Hemorrhage into the lateral ventricle occurs from the brain tissue adjacent to it and is characterized by gradual filling of the volume of the lateral ventricles with the spread of blood into the third ventricle and beyond. With a large amount of bleeding, a significant increase in brain volume occurs with the development of bilateral neurological symptoms. If hemorrhage into the ventricles of the brain is accompanied by filling of only one lateral ventricle, it has a more favorable course and symptoms, reminiscent of ordinary parenchymal hemorrhage.
Blood breakthrough into the third ventricle occurs from medial foci of parenchymal hemorrhages. In this case, there is an acute development of neurological symptoms, often leading to death. Hemorrhage into the fourth ventricle arises from the dorsal brainstem or cerebellum. This type of hemorrhage into the ventricles of the brain is often fatal.
Symptoms and consequences
The clinical picture begins with a gradual impairment of consciousness: from a state of stunning to coma. The latter develops when blood has filled all the ventricles. Impaired consciousness is proportional to the filling of the ventricles with blood. Body temperature rises abruptly. At first it can rise to 40 C, suddenly drop to 37 and rise again, but to 42 C.
The second option for the onset of hemorrhage in the ventricles is the appearance of convulsions in the extremities, which occur spontaneously. In this case, the head is thrown back, the arms are bent, and the fingers are clenched.
The phenomena of cerebral edema are increasing. The pathology clinic is always the same for all patients. Edema is formed due to the presence of blood in the brain tissue, which increases intracranial pressure. This is manifested by a bursting headache, nausea and vomiting. The swelling provokes a displacement of the structures of the brain stem and brain, a dislocation syndrome occurs: breathing and heartbeat are upset, unconditioned reflexes are inhibited, the pupil does not respond to light.
Neurological symptoms occur due to damage and blood saturation of the medulla. Thus, the clinical picture shows hemiparesis (loss of muscle strength) on the opposite side. If all the ventricles are filled, muscle strength is weakened in all limbs.
- redness of the facial skin;
- heavy sweating;
- blue color of peripheral areas: fingers and toes;
- the patient is depressed, he has a fear of death;
- disorientation.
The consequences of a stroke are unfavorable: in most cases, patients fall into a coma, and then death occurs.
Hemorrhagic stroke: bleeding in the brain due to a ruptured vessel – Izvilina
» Articles from an expert » Brain
A stroke with cerebral hemorrhage occurs when a vessel ruptures, causing its contents to be released into the intracerebral space, saturating the nerve tissue. In this case, a hematoma is formed. It compresses the surrounding tissues, which blocks their nutrition and causes swelling with subsequent severe disorders that can lead to death or disability.
There are two types of stroke:
Ischemic stroke
- ischemic - with blockage of blood flow (for example, a blood clot), followed by cessation of nutrition to the affected area and necrosis of nervous tissue;
- hemorrhagic - with bleeding in the brain, when a hematoma is formed, squeezing them and causing swelling.
It is the latter that will be discussed further. Stroke with hemorrhage is an extremely dangerous condition that can be fatal. The overwhelming number of survivors receive disability. Impairments are possible in motor, visual, and speech.
Localization of hemorrhage
Wear and rupture of blood vessels can occur in any part, therefore the hematoma can be localized anywhere. In this regard, a classification according to location has been adopted.
- Intraventricular - possible when vascular accumulations located in the ventricles rupture. However, most often this is a secondary lesion, when blood from extensive hemispheric hematomas penetrates into the ventricular system. In this case, the cerebrospinal fluid pathways are blocked, which causes a violation of the outflow of cerebrospinal fluid from the cranial cavity, hydrocephalus, and subsequent cerebral edema. With such a development, the prognosis is extremely unfavorable, and the chances of survival are minimal. Death, as a rule, occurs within 1-2 days after blood enters the ventricles.
- Subdural (under the outer shell of the brain) - most often of traumatic origin, fall under the competence of neurosurgery.
- Subarachnoid (under the arachnoid membrane of the brain) - blood accumulates under the soft membrane formed by the vessels. At the same time, it spreads over the surface, sometimes involving nerve tissue in the process - in this case they talk about subarachnoid-parenchymal hemorrhage. The most common causes are aneurysms and vascular malformations.
- Intracerebral - one of the most severe cases, and the most common. Blood enters directly into the internal space. Bleeding in this location is almost always profuse and difficult to stop.
In the latter case, two development paths are possible:
- the formation of a hematoma - a cavity filled with blood, causing massive cell death in the lesion. Due to the complexity and highly specialized nature of nervous tissue, neurological deficits pose a risk of death. Clinical symptoms in this case are pronounced, and the prognosis is always unfavorable;
- hemorrhagic impregnation - in this case, the contents of the vessel get between the nerve cells. Their mass death does not occur. Most often, this development is caused by increased permeability of blood vessels of various origins.
Regardless of the location of the bleeding, the symptoms are similar. Differentiation of types is necessary to establish the feasibility of surgical intervention and prescribe the most effective drug therapy.
Causes
Hemorrhagic stroke, which is a cerebral hemorrhage, is not an independent disease. This is always a complication of some other disease or injury. There is a list of conditions that can lead to it:
- hypertensive in nature - when, as a result of prolonged, untreated or poorly controlled hypertension, the walls of arteries, veins or capillaries become thinner and more permeable; and as a result of a pressure surge, their walls rupture;
- venous in nature - due to blockage of the main or main veins, impairing the outflow of blood;
- traumatic nature - with various head injuries, the consequences depend on the location of the injury and the degree of damage;
- aneurysmal nature - due to aneurysm (loss of vascular elasticity), including congenital;
- medicinal in nature - due to taking anticoagulants, especially when the dose is exceeded or combined with alcohol;
- due to bad habits - alcohol, smoking, drugs (often cocaine);
- due to severe physical and mental overload.
Often the first attack is followed by a second, lasting from several days to a year. The first year is the most risky in terms of recurrent attacks. To prevent recurrence, lifelong medication is required.
Symptoms
The signs of an attack can be divided into those that are felt by the patient himself and those that are accessible to external observation. A stroke has a number of characteristic signs by which it is easy to recognize even a person who has never encountered such a phenomenon. Help for the victim is necessary at the first manifestations.
Internal signs
Hemorrhagic stroke is characterized by an acute onset. The main symptoms are associated with its development. Early recognition and timely assistance reduce the severity of the consequences. Developing bleeding is accompanied by:
- severe headache and burning sensation, which increase - as a reaction to the rupture of the vessel tissue and filling them with the contents of the cavities of the cerebral ventricles;
- nausea, vomiting;
- weakness, dizziness;
- photosensitivity;
- seeing the surroundings in red light;
- severe tension in the neck muscles;
- disturbances of consciousness - confusion, short-term loss of consciousness, with severe disturbances coma is possible;
- stupor and paralysis of the limbs, face or half of the body, an epileptic attack is possible.
With severe stress or overexertion, the onset may be an epileptic attack, while other signs may be absent.
External signs
People around you can judge the onset of a stroke by a number of visible signs:
- bluish pallor, or vice versa – redness of the face to a purple color;
- sagging of one side of the face, drooping of the corner of the mouth;
- paresis of gaze - it is turned towards the hemorrhage;
- dilated pupil of the eye on the side of hemorrhage;
- paralysis of the limbs (foot turned outward, inability to raise an arm);
- convulsions, epileptic seizure;
- loss of consciousness;
- tongue that is twisted or turned to the side;
- vomiting, involuntary emptying of the bladder and bowels.
Loss of consciousness
When a stroke begins, a person is unable to smile or say the simplest phrase. Often the consciousness is confused, the person does not understand the speech addressed to him.
Help with stroke
Survival and the likelihood of subsequent recovery directly depend on the speed of assistance. During the next 3 hours the patient's chances are highest. After their expiration, irreversible changes occur in the nervous tissues. Even if he survives, the patient's health and quality of life will significantly deteriorate.
First aid
First events:
- Calling an ambulance is mandatory;
- lay on a hard horizontal surface, slightly raising your head and turning it to the side;
- apply cold to the head;
- ensure the supply of fresh air;
- ensure temperature and blood pressure control.
Transportation is carried out stationary, in a horizontal position. Even if the symptoms are temporary, hospitalization is required.
Diagnostics
Upon admission to the hospital, an instrumental examination is prescribed:
- CT – high speed of examination, which is especially important when detected at an early stage;
- MRI is more informative than the previous method. Helps in early diagnosis, determines existing bleeding, allows you to predict the further development of pathology, and helps monitor the effectiveness of therapy.
Treatment
Treatment at the initial stage should be carried out in a specialized hospital, in the intensive care unit. In case of extensive hematomas, it is necessary to resort to trepanation as the only way to eliminate them. In some cases, this is the only chance to save the patient’s life.
The very first measures are aimed at restoring nutrition and oxygen supply to nerve cells.
When feeding is stopped, they begin to necrote within a few minutes, which leads to irreversible consequences. In the acute period, drugs are used that increase oxygen supply - for example, Actovegin.
During treatment, it is important to restore the patient as quickly as possible. Neuroprotectors and macropreparations are used in further therapy. For heart diseases and thrombosis, medications are prescribed to prevent thrombosis and, if necessary, anticoagulants.
Prevention
The disease is extremely serious and dangerous. It is much easier to avoid it than to treat it later. Prevention measures include:
Blood pressure control
- proper nutrition;
- monitoring weight changes (especially when you are overweight);
- control of blood pressure, preventing its increase;
- fight against atherosclerotic phenomena;
- getting rid of bad habits - smoking, alcohol;
- If possible, avoid stress and overexertion.
To prevent relapse, restorative and vitamin preparations are prescribed. Constant supervision by a specialist is required.
Consequences
After a hemorrhage, the ability to work is most often lost. It is important to maintain at least independence and the ability to self-care.
As a result of the disease, speech, vision, motor function disorders, paralysis or paresis of a body part, and loss of sensation in the limbs may remain. In addition to the immediate consequences, various complications are possible.
Mental disorders, disturbances of attention, memory, and thinking are also likely.
Complications
Complications can occur both in the acute period and over a long period after the onset of the disease. The most dangerous of them:
- a sudden breakthrough of blood directly into the ventricles of the brain;
- sudden development of occlusive hydrocephalus;
- sudden increase in swelling of brain tissue;
- violation of respiratory and circulatory functions.
There are a number of complications caused by prolonged lying down. They develop much later:
- congestive pneumonia - due to stagnation of blood or fluid in the lungs due to physical inactivity;
- sepsis – blood poisoning;
- urinary tract infections;
- bedsores;
- increased thrombus formation - especially in the affected limbs with the risk of blockage of the pulmonary artery;
- cardiac decompensation.
If movement and walking are impossible, adequate hygiene is necessary to prevent bedsores and sepsis.
Forecast
The prognosis depends on a number of factors:
- presence of complications;
- localization of the hematoma – a number of complications depend on it;
- timeliness of medical care;
- the efforts of the patient himself and his relatives during the rehabilitation period.
To avoid a relapse and recover as much as possible given the damage to brain function, you must strictly follow all the doctors’ instructions and take prescribed medications in a timely manner. Exercise therapy, massage and other physiotherapeutic measures play an important role in recovery.
Stroke
A blood vessel burst in the brain: signs, treatment, consequences
Intracerebral hemorrhage is a local, local focus of bleeding that appears as a result of a violation of the integrity of the arterial wall. If a vessel in the head bursts, life-threatening conditions may develop.
In medical practice, the term “intracerebral hemorrhage” is often used as a synonym for hemorrhagic stroke.
The proportion of deaths that occur if the supply vessels to the brain rupture exceeds 40% of cases.
Definition
If a vessel in the head bursts, the pathology is called intracerebral hemorrhage, which is reflected in the IBC-10 as section 161. Hemorrhagic stroke ranks second in prevalence after stroke developing of the ischemic type. Pathology is more often detected in patients aged 45-60 years. Statistics show that most patients are representatives of the Negroid and Mongoloid races.
The most common localization of hemorrhage is the cerebral hemispheres, basal ganglia, cerebellum, pons, and trunk. Hemorrhages that occur against the background of arterial hypertension are usually acute and extensive. Intracranial hematomas are space-occupying formations, which often tend to expand due to the growth of the pathological focus.
If a vessel in the head bursts, the consequences arise as a result of the mechanical effect of the space-occupying formation on the adjacent brain structures. An intracerebral hematoma compresses surrounding tissues, causing neurological symptoms.
Causes of rupture of blood vessels in the head
Intracranial hemorrhage most often occurs due to the rupture of a small vessel that has undergone atherosclerotic changes, with blood entering directly into the brain tissue. The main reason that provokes the pathological process when blood vessels in the head burst is long-term arterial hypertension (80-85% of cases).
Other causes of occurrence are associated with congenital and acquired vascular pathologies - atherosclerosis, aneurysms, arteriovenous and other types of vascular malformations.
Source: https://fiz-disp.ru/prochee/gemmoragicheskij-insult-krovoizliyanie-v-mozg-iz-za-razryva-sosuda.html
Diagnosis and treatment
Computed tomography can determine the location of the hemorrhage. In addition, the method detects a hematoma in the brain and its volume. For chronic hemorrhages, magnetic resonance imaging is used. A spinal tap is also performed. Cerebrospinal fluid reflects changes in the cavities of the ventricles. During hemorrhage, plasma and formed elements are found in the fluid.
Resuscitation treatment is aimed at maintaining the vital functions of breathing and heartbeat. The activities are also aimed at restoring brain function and eliminating symptoms. The main points of resuscitation actions:
- Elimination of cerebral edema with diuretics.
- Artificial maintenance of respiration using oxygen therapy.
- Anticonvulsant therapy with sibazon.
- Improving blood clotting: aminocaproic acid.
- Correction of water-salt balance and acid-base state by administering intravenous saline solutions.
Who is at risk?
Brain hemorrhage in newborns can be associated both with damage to the skull itself and with a lack of oxygen.
Prerequisites for DRC:
- Post-maturity or, conversely, under-maturity
. Premature babies are especially susceptible to intracranial hemorrhages, since their immature vessels do not yet have sufficient support in the tissues. In babies born late, the bones harden and the head is unable to adjust during birth. According to statistics, IVH occurs in every fifth premature baby and every tenth post-term baby. - The size of the fetal head does not correspond to the size of the birth canal
. In this case, natural delivery is contraindicated, because it is fraught with injury and hypoxia for the newborn baby. - Difficult pregnancy
(fetal hypoxia, intrauterine infection with various infections). - Difficult (protracted or rapid) labor
, breech presentation. - Incorrect actions of obstetricians during childbirth
.
He sees money for premium neonatology equipment so that other babies with health problems have a chance to survive their premature arrival into the world. Globally, we are becoming one of the best countries where the majority of children have the opportunity to live by the age of five. During this period, there are three deaths per thousand live births. The same ranking is shared with the Czech Republic. There are only three countries - Finland, Iceland and Luxembourg - with two deaths per thousand children under five.
But few of us can imagine what the first days, weeks and months of the life of such babies are like and what their parents experience during their life. All her events were observed almost every day by her father, David Laika. The scalpel penetrates my wife's body. The doctor's hands reach the wound for our daughter.
Based on the above, several risk groups can be identified.
The risk of cerebral hemorrhage in a child increases with:
- prematurity;
- low birth weight (less than 1.5 kg);
- oxygen deficiency (hypoxia);
- child's head injury during childbirth;
- breathing complications during childbirth;
- infections leading to blood clotting disorders.
If the child belongs to at least one of these groups, it is necessary to find out whether he has symptoms of intracranial hemorrhage.
A big hand like my index finger. The last few days have been a big change. Ala is twenty-first weeks pregnant. Unfortunately, it is not developing as well as it should. There are hematomas in the embryonic membranes, and the amniotic fluid is low. When we ask the doctor how serious it is for the child to survive, he says he doesn't dare give a clear opinion.
However, his voice seems pale. We have to get up in a few minutes to go to school and work, but it's faster than an alarm clock. This will wake me up that he has ruptured my amniotic fluid. September. Allah was in the hospital for fourteen days. Every day after school we spend it with Anezhka. I'm lucky to have insight into our work situation. They leave me until the end of the working day, they don't give me much. Agnes, however, he does better at school than at work.
Symptoms
Hemorrhage into the ventricles of the brain is manifested by rapidly developing depression of consciousness. In most cases, coma occurs in the first hours after a stroke. Only in the case of a gradual outflow of blood and a small volume of it, the patient’s consciousness over a long period of time can be preserved and lost gradually. In most cases, hemorrhage into the ventricles is accompanied by the development of meningeal symptoms and vomiting. With this pathology, the development of a vegetative symptom complex is typical, manifested by hyperhidrosis and chill-like tremor, pallor, and over time, hyperemia of the face, limbs and torso. As the disease develops, the initial decrease in temperature is replaced by severe hyperthermia, reaching high numbers.
One of the characteristic symptoms of intracerebral hemorrhage into the ventricles is considered to be a violation of muscle tone in the form of hormetonic syndrome or decerebrate rigidity. In the first case, a paroxysmal increase in muscle tone of the affected limbs occurs. An episode of hormetonia may be a response to external stimuli. In decerebrate rigidity, muscle tone is increased primarily in the extensor muscles. The patient lies with his back arched with his head thrown back, while his hands and fingers are bent, and his forearms are turned inward.
Very often, this pathology is accompanied by the formation of paresis of the limbs opposite to the parenchymal hemorrhagic focus, the appearance of motor automatisms in non-paretic limbs, increased tendon reflexes, the presence of pathological and absent abdominal reflexes, and dysfunction of the pelvic organs. With hemorrhage in the third ventricle, respiratory and circulatory disorders come to the fore; hormetonic syndrome can be bilateral in nature. Hemorrhage into the fourth ventricle may be accompanied by hiccups and difficulty swallowing, while the patient has no spontaneous movements, and the symptoms of hormetonia are rather weakly expressed.
What is hemorrhagic cerebral stroke
Hemorrhagic stroke is a condition characterized by an acute disorder of cerebral circulation associated with a violation of the integrity of cerebral vessels and blood entering the brain. The pathology is severe and poses a danger to human life. In the absence of timely and adequate assistance to the victim, the chance of life is zero.
Cerebral hemorrhage occurs suddenly, the vast majority of cases are diagnosed in individuals over 35 years of age.
As a result of damage to the blood vessels, a hematoma is formed, which puts pressure on the nerve tissue, and rapid development of edema is observed.
We will try to understand in this article in as much detail as possible with what this disease is, the causes of its occurrence, the characteristics of its course and treatment.
What is hemorrhagic stroke
This type of stroke occurs as a result of hemorrhage in the brain, provoked by an increase in the level of permeability of the vascular wall or its rupture. This concept should be distinguished from the definition of ischemic stroke, the latter is much more common (in 70% of patients). It is characterized by changes in blood vessels due to their blocking by blood clots, and the death of brain cells occurs.
Hemorrhagic stroke is a disease that has a rather severe course and often causes death. This feature is explained by the fact that the cerebral vessels do not collapse well, and this makes it difficult to stop the bleeding. The use of conventional hemostatic drugs does not give the desired result, because they are not endowed with the ability to penetrate the cerebral vessels.
The provoking factor for hemorrhage in the ventricles of the brain can be:
- a sharp increase in blood pressure;
- influence of stressful situations;
- physical overload;
- long stay in open sunlight;
- injury.
The intensity of the clinical picture depends on the diameter of the vessel that burst. The patient needs help as quickly as possible, this will significantly increase the chances of survival. Staying in specialized rehabilitation centers helps to restore lost functions to the maximum. In rare cases, recovery even occurs.
Classification: degrees and types of disease
The brain stem is responsible for transmitting commands to nerve endings throughout the body. It enables movement, breathing, swallowing and hearing. The brain stem contains centers responsible for blood circulation, thermoregulation and heart rate. This is precisely what explains why damage to the brain stem leads to the rapid death of a person.
In medical practice, it is customary to distinguish stroke by hemorrhagic type:
Primary. Its formation is provoked by an increase in blood pressure to high levels or a change in the elasticity of the vascular walls.
Secondary. Its occurrence is associated with rupture of an aneurysm, hemangiomas and other pathologies associated with blood vessels.
Depending on the duration of the pathology, the following stages of the disease are distinguished:
- acute - begins within 24 hours and lasts up to 3 weeks;
- subacute - starting from the 22nd day of illness and up to 3 months;
- early recovery - from 3 to 6 months;
- late recovery - from 6 months to a year;
- stage of long-term consequences - begins 12 months from the moment of hemorrhage.
Intracerebral hemorrhage is divided according to the hemotype and depending on the site of occurrence, it happens:
- subarachnoid - localized in the area between the hard, soft and arachnoid mater;
- peripheral;
- venticular - the affected area is the lateral ventricles;
- combined - several areas of the brain are involved in the pathological process at once (typical for extensive hemorrhage).
Acute intracerebral hemorrhage is more dangerous, because it leads to hematomas and edema, as a result of which brain tissue dies. Depending on the location, it is customary to distinguish the following types of hematoma:
- lobar - localized in one part of the brain, the cerebral cortex is not involved in the pathological process;
- media - the thalamus enters the affected area;
- lateral - the subcortical nuclei, which are localized in the white matter of the hemispheres, are involved in the pathological process;
- extensive (extensive hemorrhagic strokes are most often diagnosed) - located in several areas of the brain at once.
Microstroke is a condition characterized by damage to small areas of brain tissue. It usually occurs against the background of vasospasm due to hypertension and diabetes mellitus.
The clinical picture is manifested by changes in the patient’s neurological condition, but they disappear after 24 hours. It is important to carry out timely treatment.
Despite its fairly mild course and the absence of irreparable changes in the patient’s condition, a microstroke requires special attention, because it can be a harbinger of a major stroke.
Diagnostics
The diagnosis is made on the basis of a systematic assessment of the medical history, which contains information indicating the presence of blood diseases, previous hemorrhagic strokes, taking drugs that affect the blood coagulation system, acute onset and rapid development of severe clinical symptoms, as well as data obtained during neurological examinations and additional studies.
If hemorrhage in the ventricles of the brain is suspected, the patient is prescribed a magnetic resonance or computed tomography scan of the brain, a blood test with platelet count, and a coagulogram study. The patient may also require electrocardiogram and blood pressure monitoring.
Intracerebral hemorrhage
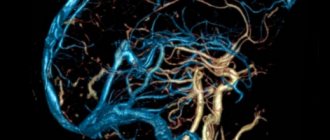
The brain has a very complex structure. In addition to gray and white matter, the brain contains structures filled with a special fluid called cerebrospinal fluid. The internal structures of the brain filled with cerebrospinal fluid are called the ventricles of the brain; there are only four of them: two lateral, a third and a fourth. Liquor is formed in the ventricles of the brain, flows through them, then enters the intrathecal spaces of the brain and spinal cord and is absorbed there into the circulatory system. Due to the immaturity of the entire brain, premature babies are at risk of rupture of fragile cerebral vessels and the development of hemorrhage in the brain, and most often this hemorrhage occurs in the ventricles of the brain.
Severity
There are several classifications of hemorrhages, most of them include 4 stages. Below is the gradation most often used in modern medicine:
Weighing just 730g, the chance of survival was approximately 30%. As soon as our little bundle was drawn into the world, they were taken away by excellent doctors - neonatologists. For Barunka, artificial ventilation and surfactants were prepared, a substance that previously existed in children, has a significant deficiency, which is used immediately after birth and helps cope with respiratory distress syndrome. It's a miracle, and doctors don't want to believe it, but Barunka doesn't need mechanical ventilation.
She is now in an incubator, has an umbilical catheter and has been given antibiotics to control the infection. The tube in it is bigger than she is. October We were with Aloy, the bravest woman in the world, to look at Barunka. Alice sees her for the first time and can't take her eyes off her. It's a miracle that doctors can save this tiny creature. We don't know how much it is because doctors don't measure it.
It is possible to establish one or another degree of hemorrhage only with the help of a special study.