Causes and risk factors
Brain hemorrhage in a newly born baby may be a consequence of a pathological pregnancy or birth trauma. The risk of intracranial hematoma exists in the first week of a child’s life. The main mechanisms influencing the formation of intracerebral hematoma in newborns:
- complicated pregnancy, in which the fetus suffers from intrauterine infection with microorganisms that damage the vascular walls, or from hypoxia (oxygen starvation);
- the birth of a premature or, conversely, post-term baby;
- a large fetus with inappropriate sizes of the baby’s head and the mother’s birth canal;
- childbirth with breech presentation;
- rapid labor;
- protracted labor process;
- the use of obstetric forceps, errors by medical workers during childbirth;
- delivery by caesarean section.
The importance of the VZhK problem
The importance of IVH pathology in newborn babies is due to a rather complex diagnostic study of the pathology, as well as its drug treatment. After all, many medications for the treatment of hemorrhage are not suitable for therapy in newborns.
Time also plays an important role in solving the problem, because the baby’s nerve centers are not yet sufficiently adapted to stress, so they simply may not be able to endure a negative situation.
In addition to children who were injured during the birth process, IVH pathology is quite often diagnosed in children born ahead of schedule.
And the shorter the period of intrauterine development of the baby, the higher the percentage of intraventricular hemorrhages.
In this situation, the complexity of brain hypoxia increases with a shorter period of intrauterine formation.
According to statistics:
- 50.0.0% of premature babies suffer from hemorrhage in the ventricles of the brain on the 1st day after birth;
- In 25.0% of infants, bleeding into the chambers of the cerebral ventricles occurs on the 2nd calendar day from the moment of birth.
If a child is born on time, then even with deviations from the normative course of the birth process, the probability of IVH ventricular hemorrhage does not exceed 5.0%.
Types of pathology
- Epidural hemorrhage. It occurs as a result of damage to blood vessels and bleeding in the space between the outer membrane of the brain and the bones of the skull. The cause is fractures, bruises, and compression of the cranial vault. Characteristic symptoms appear after a “light interval” of 3–6 hours. Then there is a dilated pupil on the affected side, depression of cardiac and respiratory activity, and convulsions. Treatment should begin immediately after the above symptoms are detected, otherwise the child will fall into a coma.
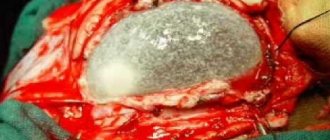
- Intracerebral (intracerebral) hemorrhage. The blood is shed directly into the brain tissue. Symptoms will depend on the location of the hematoma - the affected area of the brain ceases to control the body functions for which it is responsible.
- Intraventricular hemorrhage is one of the most severe hemorrhages, when blood fills the cavities of the cerebral ventricles, which are filled with cerebrospinal fluid (CSF). This complication is more often observed in newborns with severe prematurity. In mild cases there may be no symptoms. Moderate and severe course of the pathology threatens respiratory arrest and collapse (a sharp drop in blood pressure). Consequences may include hydrocephalus, loss of sucking, swallowing and tendon reflexes.
- Subdural hemorrhage occurs when blood vessels are damaged and blood flows into the space between the hard and soft membranes of the brain (more precisely, a hematoma forms under the hard membrane). In this case, characteristic symptoms are observed: the size of the head rapidly increases, hypertension occurs with hemorrhage in the sclera of the eyes and convulsions. This condition requires urgent measures to save and treat the newborn.
- Subarachnoid hemorrhage. Damage to blood vessels and bleeding in the slit-like space between the substance of the brain and its arachnoid membrane. With subdural hemorrhage, symptoms appear immediately and include agitation of the newborn with constant screaming, divergence of the eyeballs, increase in head size, and convulsions. The condition requires immediate action, but with timely assistance, the consequences for the proper development of the baby are minimal.
Pediatric neurosurgeon
Anonymous January 21, 2013, 1:32 pm
Hello!!! My daughter is currently (01/21/2013) 4.5 months old, Daria Pushkareva. I will provide an anamnesis of the disease: Clinical diagnosis: generalized intrauterine infection (CMVI + HSV). Congenital carditis with rhythm disturbance. NK 2 Art. O. cardiovascular failure. Interstitial nephritis. PPCNS, restoration p-d. Convulsive syndrome. date of birth 09/05/2012
On December 26, 2012, at an appointment with an Omsk neurologist, a general examination was carried out: the general condition was moderate, there were no meningeal signs, the neck was 36.5 cm, the skull bones overlapped each other in the area of the sutures.
Movements are chaotic, less active in farts. The hand is clenched, the first finger is inside the fist, the ASHT sags when supported by the arms and when traction is applied to the arms, support is not received. He can’t hold his head in a position on his stomach; he doesn’t hold it well in an upright position. Cranial nerves. Alternating strabismus, poor fixation of gaze. Muscle tone is reduced. Tendon reflexes are alive, identical on both sides. No pathological reflexes were obtained. DIAGNOSIS: Damage to the central nervous system of infectious origin (C M V + V P G). Recovery period. Disturbance of motor and psycho-emotional development. Forming craniostenosis. PROGNOSIS: cerebral palsy, nothing good can be expected, the most unfavorable was an MRI of the head, but since we have a concomitant diagnosis of congenital carditis, the cardiologist recommended doing a CT scan of the head. To do this, we went to Astana to the Republican Scientific Center of Neurosurgery for an appointment with M.R. Rabandiyarov. In this center we had a CT scan of the head: Conclusion of the computed tomography study. A series of CT tomogram scans obtained images of the sub- and supratentorial structures of the brain. Convexitally, hyperdensity areas are identified in the right parietal region on the right and the frontal region on the left. Up to 45 units N., up to 4 mm wide (parietal region); up to 3mm (frontal area). There is also deformation of the frontal bone. The midline structures are not displaced. The ventricles of the brain are not dilated, the lateral ventricles are symmetrical. The subarachnoid space of the cerebral hemispheres is expanded, convexital grooves are visible. The paranasal sinuses and cells of the mastoid processes of the temporal bones are developed correctly, their pneumatization is not impaired. Conclusion: CT signs of chronic subdural hematoma of the parietal region on the right and frontal region on the left, deformation of the frontal bones, external hydrocephalus. Rabandiyarov M.R. provided an advisory opinion: On the produced CT scans of the brain there is a picture of the atrophic process of the brain, microcephaly, mixed hydrocephalus, secondary craniostenosis. Surgical treatment is not indicated for the child. Treatment by a neurologist and rehabilitation are recommended. QUESTION: WHAT TO DO?????? Our neurologist prescribed Cortexin!!! She examined the child, there is dynamics!!! All the doctors in our city brush us off, citing the fact that even the Omsk neurologist told us that everything is bad!! My head is spinning, nothing is clear, there are a lot of diagnoses, the doctors give scientific explanations to my questions, which I, as a person without medical education, do not understand!!! I ask you to tell us in more detail and explain what awaits us, what to do and how to help the child!!! Thanks in advance for your answer!!! ReplyDelete
Symptoms of cerebral hemorrhages in newborns
Any type of cerebral hemorrhage in newborns is characterized by several common symptoms indicating the presence of pathology:
- lethargy, detachment, apathy in behavior;
- frequent regurgitation and vomiting;
- convulsions due to compression of brain tissue.
With hemorrhages in the deep parts of the brain, the following will be observed:
- depression to the point of complete absence of pupillary reaction to light;
- sudden dysfunction of the limbs on one (affected) side - hemiplegia;
- decrease in heart rate - development of bradycardia;
- development of hypothermia - decrease in body temperature;
- respiratory rhythm disturbance;
- falling into a state of deep coma.
For hemorrhages in the brain substance (gray and/or white):
- lack of coordination in space;
- increased excitability or severe inhibition;
- the appearance of hemiplegia;
- pathological foot syndromes (reflex extension of the toes when lightly tapping them).
For hemorrhage into the cerebellar tissue:
- impaired consciousness;
- constricted pupils;
- tension in the neck muscles with the head tilted back or to the side;
- persistent gaze deviation;
- uncontrollable vomiting;
- uncoordinated movements.
Germinal matrix and intraventricular hemorrhage
Category: Neonatology
Definition. HM/IVH predominantly develops in premature infants and is the most threatening complication that predicts lifelong neurological consequences in these patients. HM/IVH is caused by short gestation and the vulnerability of the immature cerebral vasculature. Perinatal stressors are typically associated with the development of HM/IVH.
In this case, the newborn at birth has asphyxia, hypoxemia, hypotension and acidosis.
The germinal matrix is located between the caudate nucleus and the epindyma of the lateral ventricle. As a rule, the GM is not normally visualized by ultrasound. When hemorrhage occurs in the brain, the structure becomes easy to identify with ultrasound and this
the condition is verified as a subepindymal hemorrhage arising between the thalamus and the head of the caudate nucleus. Bleeding may be limited to the germinal matrix or result from rupture of the wall of the lateral ventricle. The process can be one-sided or two-sided.
IVH is rare in full-term infants, but when it occurs, it is largely due to birth trauma. By postconceptional age (PCA) of 36 weeks, the germinal matrix in most children has involuted, although in some cases it may remain in a residual form.
Tests on neonatology and pediatrics with answers for advanced training.
Epidemiology. Specific incidence figures are unknown, but the incidence of HM/IVH is approximately 25-40% among all preterm infants. These estimates are based mainly on data from 1990-2000, but over the past decade there has been a decline in the lower end of the range of development of the above pathology by 2-20%.
The incidence varies depending on the stage of pregnancy, with the highest risk of developing HM/IVH in preterm infants with a birth weight of less than 750 g. Since IVH is rare in full-term newborns, the incidence rate in this category of children is extremely low and is associated with concomitant intrapartum trauma and asphyxia.
Pathophysiology. The germinal matrix is a poorly supported and highly vascularized region. The blood vessels (arterioles, venules, and capillaries) in this region of the brain are immature at birth and are particularly prone to hypoxic-ischemic injury.
These vessels have an irregular shape with pronounced areas of lumen and are prone to easy rupture. The germinal matrix undergoes involution into the PCV at 34 weeks and is thus vulnerable to the development of HM/IVH in preterm neonates. It is in this category of children that the amount of matrix is reduced, but not completely removed.
Premature newborns born later (gestational age 34-37 weeks) are also at less risk of developing IVH. Cerebral blood flow (CBF) fluctuations play an important role in the pathogenesis of HM/IVH, as pressure-mediated cerebral circulation occurs in preterm infants. A sudden increase or decrease in systemic
blood pressure can lead to an increase in BMC with subsequent rupture of germinal matrix vessels. A decrease in BMC can cause the development of ischemic damage to the vessels of the germinal matrix and surrounding tissues.
The unique anatomy of the deep veins at the level of the foramen of Monro and the open connection between the vessels of the germinal matrix and the venous circulation influence the occurrence of sharp fluctuations in cerebral venous pressure. In 80% of newborns with HM/IVH, periventricular hemorrhages are interrupted through the ependyma into the ventricular system of the brain.
Hemorrhage into the adrenal glands
This pathological condition in newborns occurs when obstetric forceps and other additional aids are applied during childbirth, as well as during breech presentation. While passing through the birth canal, the child receives trauma to internal organs and ruptured blood vessels. In this case, the “bright period” without any symptoms lasts about two days. Then there is a sharp deterioration in the condition of the newborn:
- muscle hypotonia or complete atony (lack of tone);
- intestinal atony;
- bloating;
- repeated regurgitation and vomiting;
- drop in blood pressure with depression of consciousness.
Methods for diagnosing hemorrhages:
- CT scan;
- spinal puncture followed by examination of cerebrospinal fluid;
- blood tests: coagulogram, general and detailed analysis;
- electroencephalography.
Observation and treatment of children with IVH
Taking into account the fact that intraventricular hemorrhages are considered to be the lot of premature babies, they are monitored in the neonatal intensive care unit, and then in the nursing department for small children who were born prematurely. It is very important to observe the correct regime in the department.
Doctors and nurses strive to schedule most of the manipulations at a constant time, so as not to unnecessarily disturb the children. After all, even measuring the weight of very premature babies outside the walls of the incubator is considered enormous stress for them and can cause IVH. The clinic staff takes very careful care of premature babies.
It should be taken into account that in addition to this pathology, the baby has many other associated problems: immaturity of the lungs and breathing problems, respiratory rate in newborns is disturbed, cardiovascular pathologies, difficulties in absorbing formula or breast milk, frequent layering of the infectious process, etc. .
Treatment
Therapeutic measures are aimed at stopping bleeding, normalizing the functioning of the central and peripheral nervous system, restoring the functioning of the respiratory, cardiovascular system, and adrenal glands, which suffer not only from hemorrhage directly into their tissues, but also from intracranial hematomas. Treatment methods may be as follows:
- infusions of blood substitutes (isotonic sodium chloride solution, Ringer's solution);
- administration of diuretics (Diacarb, Lasix);
- spinal puncture to reduce intracranial pressure;
- administration of hemostatic agents (aminocaproic acid, sodium etamsylate, Vikasol);
- for adrenal insufficiency - administration of the steroid drug Hydrocortisone (adrenal hormone);
- when excited - administration of tranquilizers and sedatives (Droperidol, Phenobarbital, Diazepam);
- administration of preparations with micro- and macroelements (potassium chloride, magnesium sulfate, calcium gluconate).
In extremely severe cases, surgical treatment is performed according to indications - excision of the hematoma.
Neurosonography
Neuroimaging is of primary importance in the early diagnosis of IVH and other intracranial defects. The obvious advantages of NSG are safety, speed, non-invasiveness, reliability, financial accessibility, absence of the need for sedation and radiation exposure, and the likelihood of repeated intra-vascular studies.
Transfontanel NSG is considered the main method for diagnosing IVH in newborns. In this case, recognition through the large fontanelle is mainly focused on assessing the state of supratentorial structures, including lateral structures and ventricles. More informative recognition is frontal, at the level of the foramina of Monroe; and parasagittal, at the level of the thalamocaudal notch.
View gallery
Diagnostic methods and criteria
For diagnosis in the presence of appropriate symptoms, it is usually used (using sound waves to detect vascular ruptures and bleeding). Blood tests are also taken to check for anemia, metabolic acidosis, and infections.
Instead of feeding him, he glides around like any other newborn. Today they are leaving home. We say Barunka bravely believes the worst is over. The doctors told us that our child had a small heart defect - a ventricular septal defect. This means that it mixes with oxygen and unoxidized blood, so it has more rapid breathing. We stood over the incubator, looked at Barunka, we cried, and the doctors tried to calm us down, that it was common that he had to empty between the cells to close most of the children.
When diagnosing a pathology of any degree, the specialist selects individual treatment for the patient.
Possibilities of modern medicine
If a child is found to have hemorrhage in the ventricles of the brain, he should be under the vigilant supervision of medical staff. The baby's condition is monitored to ensure his stability.
But we somehow came to optimism. Alas, milk begins to spray, but the onset of lactation is very, very slow. But he doesn't give up - every three hours he cleanses himself to begin lactation. A tube inserted into the stomach receives breast milk. An ultrasound of the head eliminated the intracranial hemorrhage, and sonic hearts performed by the child's cardiologist showed that the hole between the chambers was about 3 mm. If there were no growth in the future, this would have to be done by inserting an "umbrella" into the heart, which blocks the hole and prevents oxygenated and unoxygenated blood from mixing.
Basically, therapy for IVH is aimed at eliminating complications and consequences. If any diseases arise as a result of hemorrhage, appropriate treatment is prescribed.
Sometimes (if too much fluid accumulates in the brain), the following measures are applied:
- Ventricular
(through the fontanel) or (through the lumbar)
puncture
. - when a special drainage tube is inserted into the ventricles. It is pulled under the skin into the patient's abdomen, where excess cerebrospinal fluid is absorbed. The drainage system must remain in the body at all times, and the tube must be replaced if necessary.
It should be noted that for the majority of patients (with degrees 1 and 2 IVH) no therapy is required at all; one can count on a favorable outcome.
But the best thing is that Barunka was taken out of the incubator, and Al was able to bury her with all the pipes. I wished I had been there, but work is a lot of work. Al, however, is beaming with enthusiasm. He tells me that today he knelt with Bara. The parents fly up and place their naked child on their chest. Parents, thanks to kangaroos, create a stronger emotional connection with their child. At home we all talk about Barunka. Agnes wants her to see her. Alex expects her to want to see her again.
So we at least stage Barunka and then show the girls. Everything worked out so well. But Barunka had twenty-one breathless breaks last night. Doctors discovered that she had an infection. He gets a strong triple combination of antibiotics and waits for them. This is due to mechanical ventilation, which helps him get tired of breathing and better fight the infection.
Characteristic symptoms
There are not always visible signs of hemorrhage. Also, if a child has any of the following symptoms, then it is not at all necessary that this is due to IVH; they can also be caused by other diseases.
The most common symptoms of intraventricular hemorrhage in infants:
After the first flow of amniotic fluid, the water was replenished, but it soon drained. Doctors say that Barunka is due to this in a very stressful environment. She is not at peace yet, and she is in danger. In addition to site defects and other defects that can cause minimal amniotic fluid, water is most important for proper lung development.
It is clear that Barunka will be released into the world prematurely, and so in and then a week later, doctors will use corticosteroid injections, which help the baby's lung tissue heal faster. We pray that Barunka will survive. As far as God is concerned, we look to the time of the week from which our children are rescued if they have the slightest hope of survival. What happened that day, fairy tales, as we like it. At the age of 16, Barunka was born by Caesarean section during her week of pregnancy.
In premature infants, IVH manifests itself as a sharp and rapid deterioration of the condition on the second or third day after birth.
Prevention
Preventive measures to prevent premature birth or premature rupture of membranes, as well as to eliminate the risk of choriamnionitis, will help reduce the incidence of IVH.
Very often the cause of IVH is the use of obstetric forceps or vacuum extraction. In this case, the issue of a compelling need to use medical devices is resolved.
The development of a pathological condition can be prevented both postnatally and prenatally. In the first case, if there is a risk of a problem, hemostatic agents, pancuronium, vitamin K, phenobarbital, and indomethacin are prescribed.
This is interesting: Carcinoembryonic antigen: meaning and norm of the indicator
Prenatal prevention includes taking glucocorticoids. According to medical research, taking these dosage forms greatly reduces the likelihood of IVH in newborns.