This term has other meanings, see Delirium.
| Delirium | |
| ICD-10 | 05. |
| ICD-9 | 293.0293.0 |
| DiseasesDB | 29284 |
| MedlinePlus | 000740 |
| eMedicine | med/3006 |
| MeSH | D003693 |
Delirium
(Lat. delirium “madness, delirium”; deliro “mad, delirious”) is a mental disorder that occurs with impaired consciousness (from a darkened state to coma). Characterized by the presence of true, mainly visual, hallucinations and illusions, and, as a consequence, secondary delusions; the presence of emotional and affective disorders, senestopathies, difficult orientation in the outside world, disorientation in time. At the same time, awareness of one's own personality and dangers remains. The emotional state of the patient depends on the nature of the hallucinations occurring. After recovery from delirium, partial congrade amnesia occurs (real events and painful memories are amnesic). The patient can be dangerous to himself and others.
History of the study
| This section is not completed. You will help the project by correcting and expanding it. |
| This section is missing references to information sources. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on May 12, 2011 . |
Lindesay (1999) reports that the term “delirium” was coined by an ancient Roman scientist named Aulus Cornelius Celsus in the 1st century AD. e.
In the modern interpretation, the concept of “delirium” has lost its former psychopathological content, as a qualitative disorder of consciousness with true, mainly visual, hallucinations. The clinical picture of delirium, according to modern classifications of mental disorders ICD-10 and DSM-IV, includes a variety of states traditional for domestic psychopathology, both qualitative (delirium itself, amentia, oneiroid) and quantitative (stunning, stupor, coma) disorders of consciousness, as well as related with it impairments of cognitive and other mental functions.
Typology of disorders of consciousness
Disorders of consciousness are extremely heterogeneous, ranging from inhibition to excitation [18], in extreme cases of inhibition at times approaching comatose states, and in extreme cases of excitation resembling schizophreniform psychoses. Cognitive disorders also vary in severity, including both forms of cognitive impairment that are limited to attention disorders and forms with transient “focal” cognitive deficits.
Psychiatrists who have studied the clinical features of somatogenic psychoses have described a variety of manifestations of disorders of consciousness. In a systematic analysis of symptomatic psychoses, K. Bonhoeffer [19] distinguished delirious, amental and twilight disorders of consciousness. Following him, E. Kraepelin [20] mentioned delirium and amentia as manifestations of parainfectious psychoses. In later classifications, amentia could be classified as a type of delirium [4], which was confirmed by early observations that identified forms of delirium with more pronounced cognitive fragmentation [19]. Recent work conducted with the participation of a contingent of elderly patients in a multidisciplinary hospital [21] revealed several types of confusion, including delirium (37.9%), amentia (18.7%) and forms of confusion with confabulation (11.8%), approaching Korsakov's syndrome.
Despite the fact that the boundaries between different types of disorders of consciousness are blurred, the creation of a clinical typology has not only scientific, but also practical value. First, it equips the researcher with a more sensitive diagnostic tool that can capture individual differences while at the same time integrating them into delineated nosological units. Secondly, attention to various clinical manifestations allows us to evaluate their prognostic significance.
Another trend (and so far the prevailing one) is to follow the syndromic and statistical classification, which, without making a nosological distinction, combines a variety of post-stroke clouding of consciousness into the group F05.x “Delirium not caused by alcohol or other psychoactive substances” [22]. But even with a syndromic approach, clinical needs force us to consider syndromes that go beyond the usual somatogenic psychoses: for example, evening confusion in patients with dementia [23, 24].
Although foreign works do not distinguish between delirious, oneiric and amentive disorders of consciousness, such a distinction is of great practical importance, since different syndromes may have different etiologies and prognosis. Thus, delirious and oneiric symptoms are often found in infectious-toxic diseases [25].
The creation of a clinical typology for patients with brain damage primarily pursues a pragmatic goal - to distinguish disorders directly related to damage to certain structures from disorders the appearance of which is caused by secondary factors (biochemical post-ischemic cascade or intoxication of a somatic nature).
In this regard, the approach of the Russian neuropsychiatric school, which is used to classify the consequences of traumatic brain disease, is interesting [26]. The authors separate the syndromes of stupefaction (delirium, oneiroid, twilight changes in consciousness) from various forms of confusion (amnestic, amnestic-confabulatory, speech, etc.). The presence of confusion reflects predominantly the disintegration of cognitive functions (and certain damage to brain structures), while delirium and oneiroid are manifested by disorientation, closely associated with hallucinatory-delusional symptoms (and secondary toxic brain damage).
Classification
| This section is not completed. You will help the project by correcting and expanding it. |
Types of delirium:[1]
- drug delirium
- narcotic delirium
- organic delirium
- hysterical delirium
- senile delirium
- infectious delirium
- traumatic delirium
- delirium delirium
- professional delirium (characterized by a violation of orientation in the environment: the patient seems to be in his own working environment. Motor agitation is noted in the form of reproduction of habitual professional actions)[2].
- oneiric delirium (characterized by scene-like hallucinations of fantastic and mystical-religious content)[3][4]
- delirious delirium
- schizophrenic delirium
Etiopathogenesis
| This section is not completed. You will help the project by correcting and expanding it. |
| This section is missing references to information sources. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on May 12, 2011 . |
Delirium can be considered as a transient mental disorder reflecting acute brain failure due to diffuse metabolic disturbances. Delirium is a kind of physiological decompensation of brain functions, similar to the syndrome of heart, kidney or liver failure.
Delirium usually occurs due to disorders associated with various cerebral and general diseases, and it can also occur under the influence of a number of chemicals, during hypoxia, sleep deprivation, and during drug withdrawal. Typically, the causes of delirium are divided into three main groups:
- diseases of the central nervous system (for example, epilepsy, meningitis or encephalitis);
- systemic somatic diseases (for example, cardiac, pulmonary, renal or liver failure);
- intoxication (for example, neurotoxins in general infections, drugs, alcohol, medications).
Clinic
| This section is not completed. You will help the project by correcting and expanding it. |
| This section is missing references to information sources. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on May 12, 2011 . |
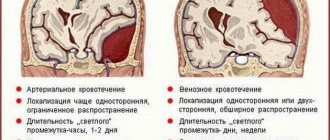
Delirium can occur at the highest stage of an infectious disease. Delirium caused by alcohol abuse is called “delirium tremens.” The duration of delirium can vary from a few hours to several weeks. Although memory of experiences during delirium is generally preserved, partial amnesia is often observed after delirium.
With delirium, the following somatovegetative disorders are noted:
- sweating
- fluctuations in body temperature
- blood pressure fluctuations
- muscle weakness
- tachycardia
- large-scale tremor
- unsteadiness of gait
Delirium in critically ill patients
Pukhnarevich Svetlana Anatolyevna Doctor - anesthesiologist - resuscitator, ICU No. 1
Impaired consciousness in a patient in critical condition occurs quite often in any clinic. A classic description of the two phases of traumatic shock by N.I. Pirogov in the middle of the 19th century, has not lost its relevance. Much of this description concerns the patient's mental state.
In the first, erectile, phase of shock, the patient develops simple psychomotor agitation. The patient is excited, restless, rushing about, screaming. In the second, torpid, phase, lethargy, apathy, indifference, and extreme passivity are noted. In both phases of shock, the patient, as a rule, does not know where he is and what is happening to him, that is, he is confused and disoriented. In modern medicine, a large number of studies are devoted to the problems of disturbances of consciousness in the postoperative period and in intensive care patients. In a general therapeutic clinic, changes in consciousness are detected in 20% of patients, mainly in the elderly. In intensive care units, disturbances of consciousness develop much more often - in 80% of cases.
Acute disturbances of consciousness are given great importance, since they are signs of increasing somatic distress or multiple organ failure. When analyzing modern literature, we were faced with the fact that almost the entire spectrum of disorders of consciousness, with the exception of comatose states, status epilepticus and dementia, is united by the concept of Delirium. In the domestic psychiatric literature, the term delirium refers to acute psychosis with disorientation, hallucinations, delusions, fluctuating, often anxious affect, motor and speech agitation.
What is delirium from a psychiatrist's point of view?
The classic psychiatric definition of delirium is: “Delirium (Latin Delirium: madness, insanity, from Delirare - deviate from a straight line, go crazy: de - separation, elimination; lira - ridge, furrow) is a type of clouding of consciousness, clinically manifested by an influx of visual hallucinations, bright sensual pareidolia (pareidolia is a type of visual illusion that consists in the formation of illusory images, the basis of which are the details of a real object, for example, figures of people and animals in the clouds, the image of a person on the surface of the moon) and pronounced motor excitation. The development of delirium indicates the presence of a somatic disease, infection or intoxication.” A state of disordered consciousness without clear signs of perceptual distortion is considered within the framework of confusion. The International Classification of Diseases (ICD-10) gives the following description of delirium: Delirium is an etiologically nonspecific syndrome characterized by a combined disorder of consciousness and attention, perception, thinking, memory, psychomotor behavior, emotions and sleep-wake rhythm. It can occur at any age, but is more common after 60 years of age. Delirium is a transient disturbance of consciousness that fluctuates in intensity. The onset of delirium is usually acute and fluctuates throughout the day. Recovery usually occurs within 4 weeks or less. However, fluctuating delirium lasting up to 6 months is not uncommon. The distinctions sometimes made between acute and subacute delirium are of little clinical significance and such conditions should be considered as a single syndrome of varying duration and severity (from mild to very severe). Delirium may occur during or precede dementia. For a definite diagnosis, mild or severe symptoms in each of the following symptom groups must be present:
a) altered consciousness and attention; reduced ability to direct, focus, maintain and shift attention);
b) global cognitive disorder (perceptual distortions, illusions and hallucinations, mainly visual; disturbances in abstract thinking and understanding with or without transient delusions, but usually with some degree of incoherence (incoherence - speech incoherence); disturbance of immediate reproduction and memory of recent events with relative preservation of memory for distant events; disorientation in time, and in more severe cases in place and one’s own personality);
c) psychomotor disorders (hypo- or hyperactivity and unpredictability of the transition from one state to another; increased or decreased flow of speech; horror reactions);
d) disorders of the sleep-wake rhythm (insomnia, and in severe cases - total loss of sleep or inversion of the sleep-wake rhythm: drowsiness during the day, worsening symptoms at night; restless dreams or nightmares, which, upon awakening, in an intermediate state, can continue as hallucinations – hypnopompic hallucinations, illusions of perception, “dreamy state”);
e) emotional disorders, anxiety or fears. Irritability, euphoria, apathy or bewilderment and confusion. A reliable diagnosis of delirium can be made even if its cause is unknown.
What is delirium, from the point of view of a resuscitator?
The resuscitation interpretation of the concept of delirium is broader than the psychiatric one, and, based on it, data have been obtained that delirium develops in 60-80% of resuscitation patients. From the point of view of a resuscitator, Delirium is an acutely developed clinical syndrome that is manifested by a change in the level of consciousness combined with decreased attention or disorganization of thinking. This definition reflects 5 fundamental aspects that make it possible to distinguish it from other conditions that are also manifested by changes in the level of consciousness and cognitive functions. First, delirium is purely a clinical syndrome. This means that it can and should be diagnosed during a clinical examination of the patient, and this does not require the use of any additional laboratory or instrumental methods. Secondly, delirium develops acutely, over a short period of time - from several hours to several days - and it is always associated with the impact of some stress factor - surgery, trauma, acute infectious process, severe pain, critical condition, etc. d. Another clinical indicator that highlights the acute development of delirium is instability of the level of consciousness during the preceding 24 hours of examination. The severity of the development of delirium allows for a differential diagnosis with dementia. These conditions also include changes in the level of consciousness, decreased attention and/or disorganized thinking, however, they exist chronically over a long period of time. At the same time, the presence of dementia or Korsakoff's syndrome in a patient does not exclude the possibility of developing delirium. On the contrary, severe premorbid cognitive changes significantly increase the risk of developing delirium when the patient is exposed to stress factors. Thus, if changes in cerebral neurological symptoms are chronic and stable, then the presence of delirium is excluded. Third, delirium always manifests itself as a change in the level of consciousness. From this postulate follow two important consequences for the diagnosis of delirium. First, the level of consciousness should be above stupor, and the patient should not be deeply sedated. The RASS scale is used for this purpose (Table 2).
The patient must have a RASS score between +4 and -3. At RASS -4/-5 the patient cannot be assessed for delirium. In this case, it is necessary to repeat the patient's assessment on the RASS scale over time. And, secondly, a patient who at the time of examination has a RASS score of 0 can have delirium only in one case - if during the days preceding the examination he had an unstable level of consciousness, that is, if he previously had any other RASS score, different from zero. Thus, if a patient has a RASS score of zero and has had stable neurological status in the previous 24 hours, then the patient does not have delirium; if the patient has a RASS score of -4/-5, then at the time of examination the patient is either in a coma or in deep sedation, which requires repeated RASS assessment over time. Fourth, attention must be examined to diagnose delirium. Decreased attention is the cornerstone of delirium. No loss of attention - no delirium. Two main types of attention disorders can be distinguished: 1) with difficulty attracting attention and 2) with the inability to maintain it. Fifth, the process of diagnosing delirium completes the identification of disorganized thinking or altered level of consciousness. With disorganized thinking, the patient answers incorrectly 2 or more of the following 4 questions: “Does a stone float in water?”, “Does a fish swim in the sky?”, “Is one kilogram heavier than two?”, “Can a hammer be used to hammer nails?” ?. Or: “Does a leaf float on water?”, “Do elephants live in the sea?”, “Is 2 kilograms heavier than one?”, “Can you cut down a tree with a hammer?” For some patients, especially neurocritical care patients, these questions may be too difficult to answer, so we believe the following test should be used to diagnose disorganized thinking. The patient is asked to show two fingers with his right hand, and after a few seconds - to show two more fingers with the other hand. A change in level of consciousness is indicated for any RASS score other than 0. However, these tests have limitations in patients with focal lesions of the left frontotemporal regions: they will not respond correctly and follow instructions due to aphasia. Thus, if a patient does not have obvious signs of thought disorganization and is rated zero on the RASS scale, then he does not have delirium, whereas with thought disorganization or RASS -3/+4 the patient is diagnosed with delirium. The interpretation of the definition of delirium described above is, in fact, an algorithm for diagnosing delirium.
And yet, what is delirium or the reasons for terminological confusion?
So, delirium is a clinical manifestation of acute brain dysfunction. In other words, delirium is a manifestation of acute cerebral organ failure. Just like an increase in creatinine levels in combination with oligoanuria are clinical manifestations of acute renal failure (ARF). However, unlike acute renal failure, which all doctors in all countries of the world and in any clinical situation, regardless of the cause that caused it, always call acute renal failure and nothing else, delirium is called differently in different clinical situations, in different countries. Here are just a few synonyms for delirium: “acute encephalopathy”, “acute brain syndrome”, “acute cognitive failure”, “reversible dementia”, “exogenous psychosis”, “acute cerebral failure”, “toxic encephalopathy”, “metabolic encephalopathy”, “ septic encephalopathy”, “alcoholic delirium”, “resuscitation psychosis”, etc.
The main reason for the terminological confusion is that for a long time, resuscitators were deprived of the opportunity to adequately diagnose acutely developed mental status disorders in a resuscitation patient. With the advent of multiple scales for assessing delirium, intensivists have the opportunity to unify their diagnostic approaches to patients who develop changes in the level of consciousness and mental disorders in the intensive care unit. However, the search for monitoring systems or neuroimaging methods that would allow diagnosing delirium and differentiating its different severity is an urgent medical engineering task. In the absence of a unified approach to diagnosing changes in mental status, there was naturally an attempt to link these changes to an etiological factor. This is how “toxic encephalopathy”, “metabolic encephalopathy”, “septic encephalopathy”, “alcoholic delirium” appeared. Another reason for the presence of such a variety of names for acute changes in consciousness are interdisciplinary differences in the understanding of biomedical phenomena. Thus, neurologists still prefer to use the term “encephalopathy” in combination with an indication of the etiological factor. While psychiatrists and resuscitators more often used the concept of delirium. And finally, there are linguistic specificities in the perception of the concept of delirium. Thus, in some countries, delirium was more often understood as alcoholic delirium, manifested by psychomotor agitation and agitation, while in others, this concept was understood as a distorted perception of reality, often accompanied by hallucinations and illusions, or changes in consciousness and mental status developing in the postoperative or post-traumatic period. The transition to a single language appears to be a matter of the future.
Etiology of delirium
Risk factors in patients with no structural changes in the brain. In the vast majority of cases, it is impossible to identify any one leading factor as the cause of the development of delirium. The etiology of delirium is always multifactorial, so it is customary to identify risk factors. At least 61 risk factors are described in the literature, however, it is methodologically correct to divide risk factors into three groups as in Table No. 4
Among these factors there are those that, given a certain severity of the critical condition, are almost guaranteed to lead to the development of delirium. Such factors include the presence of dementia in the patient, the use of benzodiazepines, and the development of infectious complications. It is known that dementia increases the risk of developing delirium by 6 times, while a higher educational level significantly reduces it. Likewise, severe infectious complications are such typical risk factors for the development of delirium that some authors consider delirium to be the earliest clinical manifestation of these complications. Based on this, there is a point of view that when delirium develops in an intensive care patient, first of all, it is necessary to exclude the presence of infectious complications.
The use of benzodiazepines increases the risk of developing delirium by 3 times. Each single administration of lorazepam increases the likelihood of developing delirium by 20%, and with a total daily dose of 20 mg, patients develop delirium in 100% of cases. Propofol is also considered a risk factor for the development of delirium, although to a lesser extent than benzodiazepines. Narcotic analgesics can cause delirium, especially when they are used primarily for sedation and in combination with benzodiazepines or propofol. However, it should be borne in mind that the presence of unrelieved pain syndrome is a powerful risk factor for the development of delirium. Therefore, adequate use of narcotic analgesics for effective relief of acutely developed pain syndrome will not only not lead to the development of delirium, but, on the contrary, will prevent its occurrence. The most dangerous combination in terms of the risk of developing delirium is the combined use of benzodiazepines and anticholinergic drugs or benzodiazepines and dopaminergic drugs. Today there are no sedative drugs that would reliably reduce the risk of developing delirium. At the same time, in some studies it was shown that when using alpha-sympathomimetic drugs, not only did the risk of developing delirium decrease, but there was a restoration of impaired cognitive functions.
Classification of delirium
Upon clinical examination, delirium is divided into hypoactive, hyperactive, mixed. In addition, a number of authors identify subsyndromal delirium. Hypoactive, hyperactive and mixed delirium are differentiated depending on the patient's RASS score. With RASS +1/+4, hyperactive delirium is diagnosed, with RASS 0/-3 - hypoactive, and if the patient is unstable within the RASS score +4/-3 delirium is mixed, which is detected most often. Subsyndromal delirium develops under the same clinical conditions as regular delirium. The identification of subsyndromal delirium is justified, since its diagnosis makes it possible to begin timely and adequate therapy without waiting for the deterioration of clinical symptoms and the formation of full-blown delirium. Patients with subsyndromal delirium occupy an intermediate position - between patients without delirium and delirious patients - in terms of severity of critical illness and outcomes. The concept of subsyndromal delirium is still not generally accepted. Borderline states between the normal level of consciousness and delirium have been and continue to be distinguished. However, they are called differently. They are unreasonably given various incorrect names, for example, “depressive disorders.” Sometimes authors give very confusing classifications of consciousness disorders. For example, Jurban A et al divided consciousness disorders in intensive care patients into coma, delirium and cognitive impairment. In this case, delirious and comatose patients, after separation, were again combined into one group, in order to then divide them into a subgroup in which consciousness was eventually restored, and a subgroup in which there was no recovery of consciousness and the patients died. In addition, patients with cognitive impairment were divided into patients with depression and patients without depression. However, sufficient clarity of consciousness is necessary for depression to develop. In essence, the authors described patients with subsyndromal delirium - the conditions in which changes in consciousness developed were no different from the conditions in which delirium developed, and all patients, when assessed on the ICDSC, had several points, and their treatment outcomes were worse. than in patients without impaired consciousness, but better than in patients with delirium. The disadvantages of creating your own classifications of disorders of consciousness are obvious. This is terminological confusion, the impossibility of reproducing the study design in other clinics, which will not make it possible to compare the severity of the patients’ condition, the results of treatment of these patients and outcomes, that is, the terminological confusion makes it impossible to conduct multicenter studies. But most importantly, patients do not receive adequate therapy.
The formation of ideas about the types of delirium allowed us to see differently the classification of disorders of consciousness in intensive care patients who initially did not have pathology of the central nervous system. With RASS -4/-5, the patient is diagnosed as comatose. Patients with RASS +4/-3 are assessed using the ICDSC method. With ICDSC 0 the patient has no impairment of consciousness, with ICDSC 1-3 the patient is diagnosed with subsyndromal delirium, with ICDSC ≥ 4 the patient has full-blown delirium. In other words, an intensive care patient without central nervous system pathology may have only three states of consciousness: lucid, comatose, or delirium. This separation has a direct impact on outcomes because if the patient is found to have impaired consciousness and is not in a coma, he or she should be started on therapy to correct delirium. A more complex situation arises when interpreting changes in the level of consciousness in neurocritical care patients, that is, in intensive care patients with initial damage to the central nervous system. Clinical interpretation of disturbances in the level of consciousness in neurocritical care patients is an urgent task, which should become the goal of further scientific research.
Treatment of patients with delirium
The primary goal in the treatment of a patient with delirium is early identification of the possible cause or probable risk factors and their immediate correction. Obviously, not all risk factors can be corrected. These include, for example, dementia preceding a critical condition or old age. However, there are a large number of significant and potentially modifiable risk factors. These are, first of all, homeostatic disorders, infectious complications, pain syndrome and all iatrogenic factors. Limit patient sedation while avoiding the use of benzodiazepines. The situations in which they are used must be narrowed to the correction of seizures and the treatment of delirium that has developed as a result of alcohol withdrawal. In the intensive care unit, rash restraint of patients should not be practiced. Having relatives near the patient can significantly reduce the need to restrain the patient. The nasogastric tube, urinary catheter and central venous catheter should be removed as soon as possible. In addition, it is very important that patients who use hearing aids or glasses in everyday life have the opportunity to use them while in intensive care. A clock and calendar with today's date mark should be located within view. The work of resuscitation should be structured in such a way that during the daytime the room is illuminated as much as possible with daylight, and in the evening and at night the lighting is dimmed. The maximum amount of routine medical procedures and care activities should be carried out during the daytime. Patients' nighttime rest time should be maximized as much as possible. It is necessary to carry out active rehabilitation measures with the patient, and they should begin as early as possible. These somewhat simple and logical measures should not be neglected, since they can significantly improve the situation.
Until recently, the basis for the pharmacological correction of delusions, hallucinations, and agitation have been antipsychotic drugs. The drug of choice has long been haloperidol, which is a classic representative of typical antipsychotics. In all international and national treatment guidelines for Delirium, it still remains a first-line drug. The main reason for this is that since 1957, when haloperidol was introduced into clinical practice, vast experience has been accumulated in the use of this drug. Overall, haloperidol is a relatively safe drug in patients with delirium. It blocks dopaminergic receptors, and this is the basis of its action. There are various forms of this drug, but in intensive care the parenteral form is most used. Haloperidol can be administered by intramuscular injection, intravenous bolus, and intravenous extended infusion, and even by extended subcutaneous infusion. Haloperidol does not achieve its maximum clinical effect immediately, but after a certain period of time, which, depending on individual characteristics, can range from several hours to several days of systematic use. The half-life is 12 – 35 hours. This is the reason for the difficulty of selecting an adequate dose. Most guidelines recommend an initial dose of haloperidol of 2.5–5 mg intravenously, followed by titration until clinical effect is achieved. Since haloperidol can begin to act only 30 minutes after intravenous administration, it is usually recommended to repeat its administration after 30–60 minutes. This is the so-called “titration method”. It is extremely difficult to name the maximum daily dose of haloperidol. There are reports of safe use of 975 mg of haloperidol per day. However, such overdoses of haloperidol do not provide therapeutic effects and are not advisable to use.
The main side effects of haloperidol are extrapyramidal disorders, cardiac arrhythmias, and neuroleptic malignant syndrome. Extrapyramidal disorders are the most common. It is known that with its parenteral administration, extrapyramidal disorders develop much less frequently than with enteral administration. When haloperidol is discontinued, extrapyramidal disorders in most cases quickly regress. However, in a number of situations, especially in patients with organic brain damage, acute dystonia develops, including akathisia (a clinical syndrome characterized by a constant or periodic feeling of internal motor restlessness and manifested in the patient’s inability to sit quietly for a long time in one position or remain motionless for a long time ), Kulenkamff-Tarnow syndrome (an irresistible urge to open the mouth and stick out the tongue; increased tone and convulsions of the masticatory and facial muscles and the muscles of the back of the head; hyperreflexia and hypersalivation; paroxysmal spasmodic torticollis, opisthotonus, bradypnea), oculogyric crises (episodic concomitant deviation of the eyes, usually upward and laterally, rarely downwards or strictly laterally). These disturbances can persist for a long time - from several hours to several days, or even weeks. With long-term use of haloperidol, it is possible to develop parkinson-like disorders that last for several months, sometimes years. In patients with a prolonged QT interval, haloperidol can cause multiform ventricular arrhythmia - Torsades de pointes - which, in turn, can transform into ventricular fibrillation. Torsades de pointes occurs more frequently with the use of high doses of haloperidol in patients with hypokalemia, hypocalcemia, hypomagnesemia and hypothyroidism. In these cases, it is necessary to discontinue haloperidol and use magnesium. Neuroleptic malignant syndrome is a serious complication with a 10% mortality rate. This is an idiosyncratic reaction in response to haloperidol, manifested by hyperthermia, severe muscle rigidity and lability of the autonomic nervous system. The diagnosis is made by excluding causes that lead to hyperthermia, metabolic acidosis and increased creatinine kinase levels. The basis of therapy is the use of dantrolene. In addition to these complications, sudden death syndrome has been described when using antipsychotics. This is the least studied syndrome, for which there is currently no explanation. One of the most interesting paradoxes is that, despite the long history of use of haloperidol, there are no randomized multicenter studies examining its use in patients with delirium. A separate interesting and challenging task is the treatment of patients with hypoactive delirium, which in Russian psychiatric manuals was called “silent confusion.” On the one hand, for these patients, as for patients with other types of delirium, antipsychotic drugs may be indicated. On the other hand, these patients have a reduced level of wakefulness, and both haloperidol and atypical antipsychotics should not be used in this category of patients, since their use may further reduce the level of consciousness. It may be more appropriate for this group of patients to prescribe cholinomimetic drugs (citicoline, ipidacrine, choline alfoscyrate, etc.), which should be confirmed or refuted by further research.
Impaired consciousness is a pressing problem in intensive care patients. Impaired consciousness in combination with multiple organ dysfunction worsens the outcome of the underlying disease. For a long time, there was no unified approach to describing impaired consciousness in an intensive care patient. As a result, a large number of synonyms have emerged that essentially describe impaired consciousness, but focus on individual etiological, pathogenetic or clinical components of this syndrome. The introduction of the CAM-ICU or ICDSC scales into clinical practice has made it possible to unify the diagnostic approach. As a result, most authors began to call disturbances of consciousness in intensive care patients delirium. This entered into certain classification and terminological contradictions with the ideas of the domestic psychiatric school, but the resuscitator now has a practical diagnostic tool that allows timely identification of impaired consciousness in patients. As a result, it has become possible to introduce into daily clinical practice a wide range of targeted interventions aimed at preventing and treating delirium in intensive care patients. Thus, the widespread introduction into domestic practice of approaches to the diagnosis, prevention and treatment of delirium in intensive care patients is appropriate.
Diagnostics
| This section is not completed. You will help the project by correcting and expanding it. |
| This section is missing references to information sources. Information must be verifiable, otherwise it may be questioned and deleted. You may edit this article to include links to authoritative sources. This mark was set on May 12, 2011 . |
The possibility of using formalized clinical-nominal scales to measure the severity of delirium symptoms over time in order to assess the effectiveness of treatment interventions and improve the diagnosis of this disorder is widely discussed in foreign literature. In everyday practice, the Confusion Assessment Method (CAM; Inouye et al., 1990) is a popular screening method for delirium, which takes into account the dynamics of the disorder. Also popular is the “Delirium Rating Scale-Revised-98” (Trzepacz PT et al., 1988; 1999) - a scale that allows you to quantitatively measure the severity of impairments in delirium according to 16 parameters (13 parameters - delirium severity subscale, 3 parameters - subscale, facilitating the differential diagnosis of delirium). More detailed in terms of studying basic neuropsychological functions is the Cognitive Test for Delirium (CTD; Hart et al., 1996). This test, as well as the Delirium Scale-Revised (DRS-R-98), allow their use even in cases where the patient's ability to interact with the examiner is limited due to intubation, immobility, or lack of speech.
Forecast
| This section is not completed. You will help the project by correcting and expanding it. |
The prognosis for patients is usually favorable, since delirium is a transient and reversible condition. The main task in alcohol or drug delirium is to combat intoxication. In case of infection - treatment of the underlying disease, etc. Thus, the severity and prognosis depend on the etiology and stage of the disease in which delirium occurs.
Alcoholic delirium: code according to ICD 10
According to the International Classification of Diseases (ICD), the code for alcoholic delirium is 10. This disease is typical for people with stages II and III of alcoholism, that is, abusing alcohol for 5–7 years. This condition is observed 1–3 days after the binge stops or on the 4th dash of the sixth day.
There are known cases of people experiencing delirium tremens as a result of poisoning with surrogate alcohol, even in those who did not suffer from addiction. The problem has become widespread also because the market is oversaturated with all kinds of counterfeits.
Also, if there is a traumatic brain injury or central nervous system disease, a person is more likely to develop delirium. For survivors of alcoholic psychosis, signs of delirium tremens can usually occur with even minor alcohol intake.
As part of the disease and the possibility of a mental disorder, sleep disturbances and anxiety are included. The duration of the acute condition, which is accompanied by confusion of mind, usually ranges from 3 to 5 days. In this case, the situation can develop in different ways.
A person deprived of normal sleep can simply fall into madness, showing inadequacy and danger to everything around him. Symptoms do not differ much across all stages of delirium delirium.