Anatomical structure of the neurovascular bundle of the neck.
The article will tell you what the recurrent nerve is, what its function is, signs of its damage and diseases accompanied by its dysfunction.
The laryngeal nerve plays an important role in the life of every person, as it innervates the muscles of the larynx, thereby participating in sound production. Next, let's look at its features.
Characteristics of the disease
With the development of a pathology such as neuralgia of the superior laryngeal nerve, the patient complains of unilateral pain localized in the throat.
As it progresses, unpleasant sensations begin to radiate to the ear area and along the lower jaw. Mostly attacks occur during eating or during the act of swallowing, and provoke coughing and malaise throughout the body. The patient's pain point can be felt on the lateral surface of the neck above the thyroid cartilage.
The active development of such neuritis ends with the swallowing reflex completely disappearing or decreasing and the sensitivity of the epiglottis being impaired. In addition, problems arise with the mobility of the affected part of the larynx, and this pathological condition is complemented by a narrowing of the glottis.
Location
The nerve is called "recurrent" because it innervates the muscles of the larynx, passing along a complex recurrent trajectory: it arises from the vagus nerve, which descends from the skull into the chest, and ascends back to the larynx.
In humans, the left laryngeal nerve arises from the vagus nerve at the level of its intersection with the aortic arch lateral to the ligamentum arteriosus. It goes around the arch of the aorta from behind, and rises in front of it in the groove between the trachea and the esophagus protruding from under it.
The right laryngeal nerve departs from the vagus nerve at the level of its intersection with the subclavian artery, bends around it from behind and rises in front of it along the lateral surface of the trachea.
The following branches depart from the laryngeal nerves: lower cervical cardiac nerves; tracheal branches (innervate the mucous membrane, glands and smooth muscles of the trachea); esophageal branches (innervate the mucous membrane, glands and striated muscles of the upper esophagus).
Features of clinical manifestations
In recent years, many specialists have paid special attention to the problem of neuralgia of the superior laryngeal nerve. Until now, it has not been possible to find out the main reason that may provoke its development.
- Vladimir Olegovich Afanasyev
- May 24, 2020
Doctors identify certain factors, the presence of which can cause pathology:
- patient age over 40 years;
- drug therapy with individual drugs for a long time;
- toxic effects on the body of bacteria and heavy metals;
- rare visits to the dentist;
- frequent hypothermia of the body.
Often, neuralgia of the superior laryngeal nerve develops when the following diseases are present in the human body:
- chronic otitis and sinusitis;
- various types of allergic reactions;
- disruption of the cardiovascular system;
- syphilis;
- tuberculosis;
- HIV.
Often, the development of neuralgia occurs when there is insufficient intake of B vitamins into the human body. In rare situations, mental disorders in a person become the cause of spasms in the jaw and throat.
The sensation of a lump in the throat can be caused by the following factors:
- A persistent inflammatory process in the pharynx and throat, for example, laryngitis, sore throat, pharyngitis, caused by a bacterial or viral infection.
- Damage to the central nervous system due to infection, and as a consequence, the occurrence of meningitis.
- Malignant and benign brain tumors.
- Paralysis of various origins.
- Osteochondrosis of the spine, especially if the cervical spine is affected.
- Unpleasant sensations may occur with uncontrolled use of certain medications.
- If a person has worked in hazardous work for a long time. Most often these are metalworking and pharmaceutical enterprises.
- The presence of bad habits, such as uncontrolled drinking, smoking and drug addiction.
- Constant stress, the presence of neurotic and depressive states.
If even one of the above factors is present, there is a high risk of developing pathology. It is important to remember that initial discomfort can be caused by infectious diseases. If stress is subsequently added to it, then we should talk about the psychological reasons for the development of this condition.
Symptoms of a lump in the throat may vary; there are a large number of them, depending on the root cause that provoked them. But only three types of such manifestations are applicable to a disease that appears as a result of neurotic disorders:
- Loss of sensation in the larynx. The patient feels numbness in the throat, and in severe cases, this condition affects the neck and shoulders. Often occurs after the patient has suffered severe hysteria.
- The spasm of the throat is so strong that it leads to suffocation. It is difficult for a person not only to speak, but also to breathe; eating or drinking becomes impossible. Usually appears as a reaction of the body to severe stress.
- The feeling of a constant lump in the throat occurs in people with an unstable nervous system, who are constantly anxious and the slightest stress unsettles them.
All of the above manifestations can occur either periodically or constantly. It all depends on the level of stress and the strength of the patient’s neurotic disorder. If such symptoms recur on a regular basis, their nature is not clear, they cause serious discomfort and the person understands that he cannot cope with them on his own, he should consult a doctor as soon as possible.
Left-sided localization of glossopharyngeal nerve neuralgia is recorded 3.5 times more often than right-sided localization, while with trigeminal neuralgia the right-sided one is more common. In 77% of patients, neuralgia debuts between the ages of 20 and 59 years, and only in 23% at a later age. The disease is approximately 2 times more common in women than in men. The duration of the disease ranges from 1 year to 20 years.
Symptoms of glossopharyngeal neuralgia are similar to those of trigeminal neuralgia and are characterized by painful attacks and the appearance of trigger zones. The leading clinical manifestation is short-term paroxysmal pain. Their duration may not exceed 1-2 minutes, but more often they last no more than 20 seconds. Patients characterize the pain as burning, shooting, reminiscent of an electric shock. Their intensity varies - from moderate to unbearable.
Most patients, reporting the onset of the disease, note that attacks occur suddenly in the midst of full health. Much less often, precursors of the disease appear in the form of various local paresthesias, usually several weeks and even months before the development of the disease.
Most often, attacks are provoked by talking, eating, laughing, yawning, moving the head, or changing the position of the body. As with trigeminal neuralgia, attacks most often occur in the morning, after a night's sleep, and less often at other times of the day. The number of attacks per day ranges from several to countless (neuralgic status). During this period, patients cannot not only talk and eat, but even swallow saliva.
Forced to sit or stand with their head tilted to the affected side, when an attack occurs, they press or strongly rub their hand on the parotid-maxillary or retromaxillary area on the side of the pain syndrome. Often exhausted from hunger and severely depressed, patients fearfully await the next painful attack. An increase in the daily number of painful attacks, as well as the duration of exacerbation, indicates the progression of the disease.
The primary localization of pain most often corresponds to the root of the tongue, pharynx, palatine tonsils, less often on the lateral surface of the neck, behind the angle of the lower jaw (in the retromandibular and submandibular regions or in front of the tragus of the ear). Often there are two areas of pain.
Trigger zones are one of the most characteristic signs of glossopharyngeal neuralgia and occur in most patients. Their most typical location is in the area of the tonsils, the root of the tongue, and their combinations are not uncommon; less often they are observed in other areas, for example, in the tragus of the ear.
The appearance of the trigger zone on the skin of the chin, the mucous membrane of the lower lip, the anterior 2/3 of the tongue, i.e. outside the innervation of the 9th pair, observed in patients with a combined form of neuralgia of the glossopharyngeal and trigeminal nerves. Often there is also a change in the location of the initial localization of pain and trigger zones during different periods of the disease and during its exacerbations.
The zones of pain irradiation, despite some differences, are quite defined. Most often, pain spreads into the depths of the ear, pharynx, and relatively rarely to the root of the tongue, anterior to the tragus and to the lateral parts of the neck.
During the period between painful paroxysms during the course of the disease, mild aching pain appears, as well as sensations of burning, tingling, tingling, the presence of a foreign body in the pharynx, root of the tongue or palatine arch.
Pain and paresthesia, persisting for quite a long time after the end of the acute period, intensify with physical and emotional stress, changes in meteorological conditions, hypothermia, etc.
Most often, damage to the recurrent nerve (neuropathic laryngeal paresis) is diagnosed on the left side after surgical manipulations on the thyroid gland, organs of the respiratory system, great vessels, in viral, infectious diseases, vascular aneurysms and oncological tumors of the throat and lungs.
The causes may also be mechanical injuries, lymphadenitis, diffuse goiter, toxic neuritis, diphtheria, tuberculosis and diabetes mellitus. The left-sided lesion is explained by the anatomical features of the location of the nerve endings that are injured during surgery. Congenital paralysis of the vocal cords occurs in children.
With neuritis of the recurrent nerve, inflammation of the nerve endings occurs against the background of viral or infectious diseases. The cause may be chemical poisoning, diabetes, deficiency of potassium and calcium in the body, thyrotoxicosis.
Central paresis of the recurrent laryngeal nerve occurs with damage to brain stem cells caused by cancerous tumors, atherosclerotic vascular lesions, botulism, neurosyphilis, polio, hemorrhage, stroke, and severe skull trauma. With cortical neuropathic paresis, bilateral damage to the recurrent nerve is observed.
During a surgical operation in the larynx area, the recurrent laryngeal nerve can be damaged by any instrument, excessive pressure with a napkin, compression of the suture material, resulting hematoma, or exudate. A reaction to disinfectant solutions or anesthetics may occur.
The main symptoms of damage to the recurrent nerve include:
- difficulties during the pronunciation of sounds: hoarseness of voice, decreased timbre;
- dysphagia – difficulty swallowing food;
- whistling, noisy inhalation of air;
- loss of voice;
- suffocation with bilateral nerve damage;
- dyspnea;
- impaired tongue mobility, sensitivity of the soft palate;
- numbness of the epiglottis, food enters the larynx;
- tachycardia, increased blood pressure;
- with bilateral paresis, noisy breathing;
- cough with gastric juice refluxing into the larynx;
- respiratory disorders.
Surgery on both lobes of the thyroid gland can lead to bilateral recurrent nerve palsy. In this case, paralysis of the vocal cords occurs, the person cannot breathe on his own. In such cases, a tracheostomy is required - this is an artificial opening in the neck.
With bilateral paresis of the recurrent nerve, the patient is constantly in a sitting position, the skin is pale, cyanotic, the fingers and toes are cold, and the person experiences a feeling of fear. Any physical activity leads to a worsening of the condition. After 2–3 days, the vocal cords occupy an intermediate position, forming a gap, breathing normalizes, but during any movement the symptoms of hypoxia return.
Coughing and constant injury to the mucous membranes of the larynx lead to the development of inflammatory diseases: laryngitis, tracheitis, aspiration pneumonia.
Neuralgia of the superior laryngeal nerve
Diseases
Translated from Greek, the term “neuralgia” means “nerve pain.” This is a fairly common inflammatory process that affects approximately 5% of the total population of the planet. Neuralgia develops, as a rule, in nerves located in narrow openings and canals.
Women are more susceptible to this disease than men. It is extremely rare that this diagnosis is given to children. Neuralgia, if it occurs in the superior laryngeal nerve, manifests itself in the form of painful sensations localized in the lower jaw and larynx.
The etiology of this pathology is not fully understood, but experts identify a number of factors that provoke the development of characteristic symptoms of the disease.
Symptoms of neuralgia of the superior laryngeal nerve
The disease is cyclical. That is, attacks alternate with periods of remission. The obvious symptoms that accompany neuralgia of the superior laryngeal nerve are outbreaks of burning pain. The duration of the spasms varies approximately from a few seconds to a couple of minutes. Attacks of neuralgia are characterized by the following features:
- sharp, burning pain in the larynx and corners of the lower jaw;
- laryngospasm (narrowing of the lumen of the ligaments);
- irradiation of pain to the chest, eye socket, ear, collarbone;
- spasms intensify when turning and tilting the head;
- attack of general weakness.
Symptoms such as constricting sensations in the chest area and pain in the sublingual area may also indicate that neuralgia of the superior laryngeal nerve is developing. Spasms cannot be relieved with conventional non-narcotic medications. Attacks of neuralgia are often accompanied by hiccups, coughing and increased salivation.
The pain becomes more intense when swallowing, yawning or trying to blow your nose. Patients also experience changes in heart rate. These disorders are caused by irritation of the vagus nerve. The occurrence of an abnormal heart rhythm indicates the progression of the disease, the development of pathological changes and the transition of neuralgia to the stage of neuritis.
If left untreated, peeling and redness of the skin may occur.
Many modern specialized specialists are working on the problem of neuralgia of the superior laryngeal nerve. However, the true cause of its occurrence has not yet been established. It is only known that there are factors that can provoke the development of this disease. The most common ones include:
- age over 40 years;
- systematic hypothermia (for example, frequent exposure to drafts);
- recent visit to the dentist;
- toxic effects of bacteria and heavy metals;
- long-term use of certain groups of medications.
In addition, various diseases can provoke the symptoms that accompany neuralgia of the superior laryngeal nerve. These include the following:
- diabetes;
- HIV;
- syphilis;
- tuberculosis;
- chronic otitis or sinusitis;
- diseases of the cardiovascular system, in particular atherosclerosis, anemia and hypertension;
- various allergic manifestations.
Neuralgia of the superior laryngeal nerve can also be caused by a lack of B vitamins. There have also been cases in medical practice when this disease was diagnosed in patients suffering from malabsorption of nutrients, as well as bulimia and anorexia. Mental disorders are also often accompanied by spasms in the jaw and throat.
It is worth saying that it is not possible to completely get rid of the disease. However, this does not mean that the disease should be left to chance. Frequent attacks of neuralgia of the superior laryngeal nerve can significantly affect a person: he becomes aggressive and irritable. This is how endless waiting for the next attack works. In some cases, neuralgia can even provoke depression or psychosis. Therefore, at the very first attacks, you should seek help from a specialist. The following doctors are involved in the diagnosis and treatment of neuralgia:
Very often, in order to find out the true causes of the development of the disease, you should visit the offices of an otolaryngologist and dentist, since it is necessary to exclude diseases of the teeth, ears, and nose. You should also be prepared for the fact that you may need to consult an oncologist. His help is required in cases where there is a suspicion of a brain tumor.
At the appointment, the specialist must familiarize himself with the clinical picture. To do this, he will carefully listen to the patient’s complaints and conduct a survey during which he will ask the patient the following questions:
A simple survey is often not enough for a doctor to make a final diagnosis. Therefore, he must write out a referral for hardware research methods. The diagnostic results will indicate the etiology of the disease and help in developing a course of therapy. Treatment of neuralgia of the superior laryngeal nerve should be comprehensive. It is compiled according to the individual characteristics of the patient.
Simple ways to improve memory
A recently released study of Catholic nuns...
What to do if you have a headache
It would not be an exaggeration to say that absolutely everyone knows headaches first-hand...
Temple swelling
The temple is an ordinary bone that cannot swell on its own. How right...
Dizziness during pregnancy
During pregnancy, many changes occur in a woman's body. They can...
Source: //bolezni.zdorov.online/nevrologija/nevralgiya/verkhnego-gortannogo-nerva/
Symptoms
Neuralgia of the superior laryngeal nerve is considered a cyclical disease in which the acute stage is followed by periods of remission. The most characteristic symptom that occurs with this pathology is an attack of sudden pain. The duration of such spasms can vary and can reach 2-3 minutes.
- Kirill Stepanovich Lavrentiev
- May 25, 2020
An attack of neuralgia of the superior laryngeal nerve usually causes the development of the following symptoms:
- sharp burning pain that occurs in the larynx and corners of the lower jaw;
- general weakness of the whole body;
- spread of pain in the chest, hearing organs, collarbone and orbit;
- decrease in the lumen of the vocal cords, that is, the development of laryngospasm;
- increased spasms with any turn of the head.
A feeling of stiffness in the chest may indicate the development of neuralgia of the superior laryngeal nerve in a patient. In addition, severe pain appears in the sublingual area, and spasms cannot be relieved with conventional non-narcotic medications.
Often, during attacks of neuralgia, the patient develops a cough, hiccups, and increased salivation. Swallowing, chewing and the desire to blow your nose are accompanied by increased pain, and a change in heart rate is also observed. The development of such disorders is associated with irritation of the vagus nerve.
An abnormal heart rhythm may indicate that the disease is actively developing and that neuralgia may progress to the stage of neuritis. In the absence of effective therapy, problems with the skin may appear, that is, they begin to peel off and turn red.
Experts identify four main forms of pharyngoneurosis, each of which has its own symptoms:
- anesthesia;
- hypoesthesia;
- hyperesthesia;
- paresthesia.
More details about the symptoms of each form of pharyngeal neurosis:
- Anesthesia of the throat is characterized by a decrease in the sensitivity of the larynx or its complete absence. The patient has difficulty swallowing. Typically, similar symptoms occur during hysteria. This may also indicate a blockage of the signal that is sent by brain cells to the larynx. This often indicates a malignancy in the brain, infection, paralysis or multiple sclerosis.
- Hypoesthesia. This form has similar symptoms to anesthesia, with the only difference being that it manifests itself more mildly. The patient can swallow, although the pharyngeal mucosa remains insensitive. Hypesthesia can occur against the background of previously suffered viral diseases or influenza. It will take some time for sensitivity to be restored. If the symptoms do not go away, but only worsen, it is imperative to consult a doctor. Neglect of treatment in some cases can lead to death, as if the sensitivity of the pharynx is lost, a person runs the risk of choking on food or water.
- Hyperesthesia. This form of pharyngoneurosis, on the contrary, is characterized by increased sensitivity. The patient complains of difficulty eating food. Symptoms of this form are constant pain in the throat, tingling and itching. Hyperesthesia can be a consequence of tonsillitis, tonsillitis or pharyngitis. Symptoms appear more clearly if a person has a smoking habit. Also, strong emotional overexcitation leads to breathing difficulties. All symptoms disappear when the emotional state returns to normal.
- Paresthesia. The symptoms of this form practically repeat hyperesthesia. The picture is complemented by the following signs: severe itching; feeling of numbness; sensation of a nervous lump in the throat. Patients also complain of constant headaches, the intensity of which increases when eating or swallowing. Paresthesia is typical for people who are characterized as emotionally unstable, with increased irritability. Often complaints of a lump in the throat come from women during menopause.
Evidence of evolution
The recurrent laryngeal nerve is present in all mammals, and like in humans, it departs from the vagus nerve coming from the brain, goes around the aortic arch or other large artery and goes back to the larynx. This route is especially pronounced in the giraffe: the total length of the recurrent nerve can reach four meters, since it passes through the entire neck back and forth (as part of the vagus nerve) and back (as an independent recurrent nerve), despite the fact that the distance from the brain to the larynx is only a few centimeters.
Such an inappropriate trajectory is in good agreement with the synthetic theory of evolution, and is not explained by alternative approaches, and therefore is considered as one of the evidence of evolution. Mammals inherited this structure of this nerve from fish, which lack a neck, and the homologous branch of the vagus nerve follows an optimal trajectory.
Treatment methods
It is possible to determine whether the recurrent laryngeal nerve is damaged after consulting an otolaryngologist, neurologist, neurosurgeon, pulmonologist, thoracic surgeon and endocrinologist. Diagnostic examinations for laryngeal paresis:
- Examination of the patient's larynx and collection of anamnesis.
- CT scan.
- X-ray of the larynx in frontal and lateral projection.
- During laryngoscopy, the vocal cords are in the midline position. During breathing and conversation, the glottis does not increase.
- Phonetography.
- Electromyography of the laryngeal muscles.
- Biochemical blood test.
Additionally, CT, ultrasound and radiography of the respiratory system, heart, thyroid gland, esophagus, and brain may be necessary.
It is important to differentiate paresis of the laryngeal recurrent nerve from other diseases that cause breathing problems:
- laryngospasm;
- blockage of blood vessels;
- stroke;
- multiple system atrophy;
- attack of bronchial asthma;
- myocardial infarction.
In case of bilateral paresis, the patient’s serious condition, or asthma attacks, emergency care is first provided, and then diagnostics are carried out and the necessary methods of therapy are selected.
Paresis of the laryngeal recurrent nerve is not a separate disease, so treatment begins with eliminating the causes that caused the pathology. When cancerous tumors grow, surgical removal of the tumor is required. An enlarged thyroid gland is subject to resection.
Emergency care is required for bilateral paresis, otherwise asphyxia may occur. In such cases, the patient undergoes a tracheostomy. The operation is performed under local or general anesthesia. A special cannula and tube are inserted into the trachea, which is fixed using a Chassignac hook.
Drug therapy includes taking antibiotics, hormonal drugs, neuroprotectors, and B vitamins. In the presence of an extensive hematoma, medications are prescribed that accelerate the resorption of the bruise.
Reflexology is carried out by influencing sensitive points located on the surface of the skin. The treatment restores the functioning of the nervous system and accelerates the regeneration of damaged tissues. Special sessions with a phoniatrist help normalize voice and vocal function.
With prolonged impairment of vocal functions, atrophy and dysfunction of the laryngeal muscles occur, and fibrosis of the cricoarytenoid joint is formed. This prevents speech restoration.
If conservative therapy is ineffective and there is bilateral recurrent nerve paresis, reconstructive surgery is indicated to restore respiratory function. Surgical intervention is contraindicated in old age, with malignant tumors of the thyroid gland, and the presence of severe systemic diseases.
The patient is carefully examined and the optimal treatment tactics are chosen. There are two ways to perform the operation: percutaneous and through the oral cavity. The volume of the vocal cords is increased by introducing collagen or Teflon. The therapy is carried out under the control of laryngoscopy; the doctor can monitor the progress of the procedure on a computer monitor. Laryngoplasty of the vocal tract allows you to partially or completely normalize speech, breathing, and increase the clearance of the vocal cords.
The laryngeal nerve is responsible for the motor function of the larynx and vocal folds. Its damage leads to speech impairment, difficulty breathing and swallowing food. Bilateral paresis can cause suffocation and death, so the disease requires urgent treatment. The prognosis for therapy is favorable.
In the absence of effective therapy, the initial stage of the disease proceeds rapidly. If you refuse treatment for a long time, the result is often the development of severe complications. When the pathology passes into an advanced form, problems with the functioning of the swallowing reflex gradually appear or it completely disappears.
To identify the cause that triggered the development of neuralgia, you should visit specialists such as an otolaryngologist and dentist. They will conduct a thorough examination of the patient in order to exclude the presence of pathologies of the nose, ears and teeth.
With such a disease, it may be necessary to consult an oncologist if the attending physician suspects a malignant tumor in the brain.
- Kirill Stepanovich Lavrentiev
- May 24, 2020
The final diagnosis is made taking into account anamnestic data and an objective examination, as well as based on the results of instrumental research methods. To determine the functional state of the vocal apparatus, diagnostic test methods can be used:
- bronchoscopy;
- computed tomography of the chest;
- laryngoscopy;
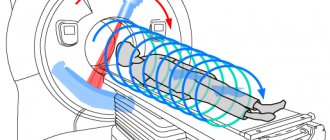
- MRI;
- needle electromyography of the larynx.
A careful study of the diagnostic results allows us to identify the cause of neuralgia of the superior laryngeal nerve and select the most effective course of treatment.
Diagnosis of neuropathic laryngeal paresis
The purpose of diagnosing neuropathic laryngeal paresis is not only to establish a diagnosis, but also to identify the cause of the paresis. For this purpose, the patient is sent for consultation
The article will tell you what the recurrent nerve is, what its function is, signs of its damage and diseases accompanied by its dysfunction.
The laryngeal nerve plays an important role in the life of every person, as it innervates the muscles of the larynx, thereby participating in sound production. Next, let's look at its features.
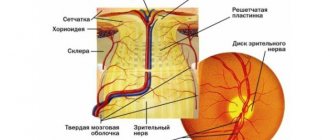
The laryngeal nerve is a branch of the X pair of cranial nerves. It contains both motor and sensory fibers. Its name is the vagus nerve, which gives branches to the heart, larynx and vocal apparatus of mammals, as well as to other visceral units of the body.
The name “recurrent” fully characterizes its course in the human body after leaving the cranium. There is one branch of the vagus nerve on each side of the neck, but their route is similar. It is interesting that, having left the cranial cavity, the recurrent nerve first runs to the chest, where, bypassing large arteries, it creates a loop around them, and only then returns to the neck, to the larynx.
For some, this route may seem pointless since it serves no function until it returns to the larynx. In fact, this nerve is the best evidence of human evolution (more details in the video).
It turned out that in fish this nerve innervates the last three pairs of gills, passing to them under the corresponding gill arteries. This route is quite natural and the shortest for them. During evolution, mammals acquired a neck, which was previously absent in fish, and the body acquired large sizes.
This factor also contributed to the lengthening of blood vessels and nerve trunks, and the appearance of, at first glance, illogical routes. Perhaps the extra few centimeters of the loop of this nerve in humans have no functional significance, but are of great value to scientists.
Attention! Just as in a person this nerve runs an extra ten centimeters, in a giraffe the same nerve runs an extra four meters.
Functional significance
In addition to the motor fibers themselves, as part of the recurrent nerve, going to the muscles of the larynx, providing the voice-forming function, it also gives branches to the esophagus, trachea and heart. These branches provide innervation to the mucous and muscular membranes of the esophagus and trachea, respectively.
The superior and inferior laryngeal nerves carry out mixed innervation of the heart through the formation of nerve plexuses. The latter includes sensory and parasympathetic fibers.
Classification of CAH symptoms
Depending on the type of receptors stimulated:
- exteroceptive, or superficial, sore throat,
- proprioceptive, or deep, sore throat.
Depending on the clinical course (duration):
- lightning sore throat,
- acute sore throat,
- short-term sore throat (quickly passing),
- acute recurring sore throat,
- chronic (long-term or constant, incessant) progressive sore throat,
- chronic (long-term or constant, ongoing) non-progressive sore throat.
Depending on the area and volume of pain perception:
- local, or localized, sore throat;
- systemic, or general, diffuse, sore throat.
Depending on origin:
- sore throat of peripheral origin;
- sore throat of central origin.
Depending on intensity:
- mild sore throat,
- sore throat of moderate intensity,
- sore throat of severe intensity.
Depending on the nature and quality of the subjective sensations that arise:
- paroxysmal, throbbing sore throat;
- pain in the throat: stabbing, shooting, dull, burning, jerking, boring, cutting, pressing, squeezing, tearing;
- sore throat: referred, projective, intermittent, reactive, radiating, phantom.
Depending on the degree of tolerance:
- sore throat is easily tolerated (mild),
- sore throat is difficult to bear (severe),
- the sore throat is intolerable (unbearable).
Based on the results of diagnostic measures and examination of the patient, all symptoms of damage to the recurrent nerve can be divided into:
- Unilateral paralysis of the left recurrent laryngeal nerve is manifested by severe hoarseness, dry cough, shortness of breath when talking and after physical exertion; the patient cannot talk for a long time, chokes while eating, and feels the presence of a foreign object in the mouth.
- Bilateral paresis is characterized by difficulty breathing and attacks of hypoxia.
- A condition simulating paresis develops against the background of unilateral damage to the recurrent nerve. In this case, a reflex spasm of the vocal fold on the opposite side is observed. The patient has difficulty breathing, cannot cough, or choke on food while eating.
A reflex spasm can develop when there is a deficiency of calcium in the blood; this condition is often found in people suffering from thyroid diseases.
Performing surgical laryngoplasty
If conservative treatment is ineffective, as well as against the background of bilateral paresis of the recurrent nerve, patients are prescribed reconstructive surgery to restore respiratory functions. Surgical intervention is not recommended in old age, and in addition, in the presence of malignant thyroid tumors or severe systemic pathologies.
Recurrent laryngeal nerve
| Recurrent laryngeal nerve | |
| Tracheobronchial lymph nodes, posterior view. The recurrent nerves are visible from above. | |
| |
| Latin name | nervus laryngeus recurrens |
| Innervation | |
| Catalogs | |
Recurrent laryngeal nerve
(lat.
nervus laryngeus recurrens
) - a branch of the vagus nerve (tenth pair of cranial nerves), which provides motor function and sensitivity of the structures of the larynx, including the vocal folds. This nerve belongs to the 6th branchial arch.
Treatment of pathology
If characteristic symptoms of such a disease appear, you should seek advice from a specialist and do not self-medicate. The doctor will conduct a comprehensive examination of the patient and select the necessary treatment, taking into account the stage of the disease and the individual characteristics of the patient.
Neuralgia of the superior laryngeal nerve requires complex therapy, and in the initial stages of its development, such a disease can be successfully treated. To eliminate this, the following procedures can be carried out:
- taking anti-inflammatory medications;
- acupuncture.
In addition, various physiotherapeutic procedures are widely used, for example, phonophoresis or ultrasound. By identifying the disease at the very beginning of its development and prescribing effective treatment, many complications can be avoided. If neuralgia of the superior laryngeal nerve is provoked by concomitant pathologies in the human body, their mandatory treatment is required.
When such a disease is detected in people of speaking professions, voice rest is necessarily prescribed for a certain time. Low-frequency pulsed currents are selected for the complex of treatment procedures involving the sanitation of the resulting focus of pathology.
The implementation of such treatment is determined by the stage of severity of discomfort, trophic changes in the mucous membrane and motor apparatus of the larynx.
To reduce pain, Novocaine is administered with certain types of currents. It is possible to perform electrophoresis with Novocaine on the lateral surface, inductothermy and darsonvalization.
To eliminate neuralgia of the superior laryngeal nerve, antiepileptic drugs, non-steroidal anti-inflammatory drugs and antiplatelet agents are used.
In addition, drug therapy can be supplemented by taking vitamins and using local anesthesia. It is often possible to get rid of painful paroxysm by lubricating the root of the tongue, pharynx and tonsils with a local anemetic.
Inflammation of the throat, inflammation of the larynx, symptoms, how and how to relieve inflammation, throat treatment
Each of us has experienced a sore throat at least once.
The pain occurs due to inflammation of the upper respiratory tract. This disease makes it difficult for a person to swallow and speak. Let's take a closer look at what causes the disease, what complications it threatens, and what to do if you have a sore throat. inflammation of the throat and larynx Causes of sore throat can be infectious or non-infectious. Moreover, the first group is much more common than the second. There are a huge number of pathogenic microbes that can settle on the mucous membranes of the oropharynx.
Most often, their entry there causes inflammation of the mucous membrane (inflammation of the larynx). The causative agents of the disease can be:
• Candida fungi usually occur in children under three years of age.
But in some cases they occur in adults. The danger of these pathogens lies in the likelihood of damage to the respiratory system due to too rapid spread. These fungi can destroy tissue. There may be complications from the heart and respiratory system;
• Staphylococci are most often aureus.
Causes the most serious lesions of the pharynx. An abscess and purulent tonsillitis may appear. Due to the rapid proliferation of bacteria and the creation of large conglomerates, getting rid of the problem is not easy. Treatment must be comprehensive;
• Streptococci cause the most serious forms of inflammation.
Slightly less dangerous than the previous group of pathogens. May affect blood composition. Inactive forms of the disease are most often caused by streptococci;
• uncharacteristic representatives of the flora (mycoplasma, ureaplasma, chlamydia, etc.).
May also cause a slowly developing form of sore throat. They are found infrequently, since it is very difficult for these organisms to get into the throat in the usual way;
• herpes viruses – the fourth and fifth types pose the greatest danger;
• human papilloma viruses;
• rotaviruses and adenoviruses.
Infectious diseases are highly contagious. To catch the virus, it only takes a few minutes to be near a sick person.
airborne disease
Main distribution routes:
• airborne: with microparticles of mucus, saliva when coughing, sneezing and mouth breathing; • contact-household: in the process of using the personal belongings of an infected person, failure to comply with hygiene measures.
Infection can occur due to the activation of bacteria or other microorganisms living in the body, which often occurs due to a weakened immune system. This can happen due to hypothermia or stress. Non-infectious causes are less common, but they can also cause a sore throat.
The most common:
• smoking, this bad habit causes a permanent thermal burn of the mucous membranes of the pharynx. As a result, the throat is constantly sore;
• frequent alcohol consumption - reduces immunity and causes chemical burns;
• inhalation of chemical vapors - this is faced by people working in hazardous industries;
• excessive tension of the ligaments;
• poor environmental conditions – dry and dusty air irritates the mucous membranes and provokes inflammation of the throat and larynx;
• mechanical damage;
• allergies;
• age-related changes in the throat and larynx;
• reflux – due to stomach diseases, part of the digested food is thrown back into the larynx. As a result, a burn of the mucous membrane occurs.
To identify the cause of pain, you need to consider these factors comprehensively.
types of diseases of the throat and larynx
Throat diseases include:
1. Tonsillitis or, as we more often call it, tonsillitis. The causative agents are bacteria, viruses or fungi. With tonsillitis, the back wall of the throat and tonsils become inflamed.
2. Pharyngitis. Its appearance is caused by infection, allergies, chemical burns or trauma. Causes difficulty breathing.
3. Pharyngomycosis is a disease of the velopharyngeal arch caused by a fungus. One of the types of pharyngitis.
4. Throat abscess. Causes severe discomfort and inflammation of the pharynx in the affected area. Artificial obstruction of the airways may occur, which is quite dangerous for the patient’s condition.
5. Bronchitis, pneumonia, developing too quickly and involving the oropharynx in the pathological process (this does not happen often).
6. Laryngitis - inflammation of the larynx.
7. Tracheitis - inflammation of the tracheal mucosa.
symptoms of inflammation of the throat The inflammatory process of the oropharynx can be caused by different pathogens, but the symptoms are always of a similar nature. First of all, it is pain in the throat and larynx, which becomes stronger when talking and eating.
The pain syndrome causes tickling, the patient feels a constant urge to cough. The cough is unproductive, superficial with the release of a small amount of mucus.
Another characteristic sign is a change in voice timbre. Due to inflammation of the ligaments, the voice becomes hoarse, making it difficult for a person to speak loudly.
Sometimes the ability to speak completely disappears, most often this happens with pharyngitis.
Also, with diseases of the oropharynx, a lot of mucus or pus is released, especially with sore throat. In addition, breathing difficulties of varying degrees can be observed. Throat diseases are characterized by an increase in body temperature. The indicators are quite high.
All these manifestations must be assessed comprehensively in order to diagnose the disease in a timely manner and provide the patient with competent assistance. If you have the symptoms listed above, you must immediately contact a therapist or otolaryngologist.
The doctor must conduct an examination to assess the patient's condition and prescribe treatment that will alleviate the patient's condition. The patient must voice all his complaints, which will be recorded in the medical history. Any details are important. The doctor examines the pharynx.
An inflamed throat looks reddened, the back wall looks loose, and plaque can be seen on the tonsils and palatopharyngeal arch. However, a simple examination is not enough to establish the cause of the disease.
The following studies are used for this:
• laryngoscopy – examination of the larynx, which is carried out exclusively under the supervision of a specialist; • allergy tests;
• PCR, as well as ELISA blood tests;
• serological tests; • inoculating a smear from the area of inflammation to identify the nutrient medium. This study will help determine which microorganism is the causative agent of the disease.
Other procedures may be used for diagnosis, or vice versa, their list may be reduced. This decision is made by the attending physician. If necessary, a consultation with another specialized specialist may be scheduled.
Source: //old-lekar.com/vospalenie-gorla-i-gortani-chto-delat-pri-vospalenii/
Prognosis and complications
If the pathology is detected in the initial stages, it can be successfully treated, and in a short time it is possible to get rid of the characteristic symptoms. If the patient does not seek help from a specialist for a long time, the consequences of neuralgia of the superior laryngeal nerve can become quite dangerous.
As the disease progresses to the last stage of development, a disruption in the functioning of the swallowing reflex and even a complete loss of the ability to eat may occur.
At the very beginning of its development, neuralgia of the superior laryngeal nerve can be easily eliminated, so when the first signs appear, it is important to immediately seek help from a doctor. To eliminate it, it is important to carry out complex therapy and follow all doctor’s recommendations.
0Share0Share0Share0Share0Share0Share
Differentiation of paresis from other diseases
It is extremely important to be able to differentiate paresis of the laryngeal nerve from other diseases that also cause breathing problems. These include:
- Laryngospasms.
- Blockage of blood vessels.
- The appearance of a stroke.
- Development of multiple system atrophy.
- Attacks of bronchial asthma.
- Development of myocardial infarction.
Against the background of bilateral paresis, as well as in severe conditions in patients and attacks of suffocation, first of all, emergency care is provided, after which diagnostics are carried out and the necessary treatment method is selected.
How to get rid of intercostal neuralgia of the chest
Pain on the left side in the area of the ribs is always alarming, as it is a harbinger of a heart attack or angina. However, this may also be a symptom of intercostal neuralgia. Contents Characteristics of the disease Symptoms Causes of development Diagnosis Treatment of pathology Prognosis ...
Neuralgia is a pathological process that can occur suddenly. Acute, sharp, paroxysmal pain can pierce any part of the body. The most common pathologies are: trigeminal neuralgia, intercostal neuralgia, sciatic neuralgia...
Intercostal neuralgia is one of the most common causes of chest pain. Pathology usually occurs in old and older age, but it is not excluded in young people and even children.…
In acute and chronic thoracic radiculitis, a number of symptoms coincide, while others differ.
Common manifestations are pain, increased sensitivity and soreness of the perivertebral area, and a defensive reaction in the form of muscle tension.
The pain intensifies with palpation, straining, coughing, sneezing, and careless movements.
To relieve them, the patient often takes a forced position, bending towards the lesion in order to reduce the pressure on the pinched roots.
Usually the pain is girdling, accompanied by a feeling of chest compression and difficulty breathing. In the acute form, the pain is sharp, sharp, and has the character of a lumbago.
Muscle tension is accompanied by increased tendon reflexes. Chronic radiculitis is manifested by pain of varying intensity and character, constant and paroxysmal.
Over time, the pain syndrome is accompanied by a feeling of numbness of the skin in the chest and arms, tingling, and “goosebumps.” Muscle hypertonicity is replaced by muscle weakness, motor reflexes are impaired.
With intercostal neuralgia, the localization and nature of pain depends on the level of which vertebrae and ribs the pinched nerves are located.
The manifestations of pain are so diverse that thoracalgia is often mistaken for various diseases of the internal organs.
Along with the main symptoms (pain in the paravertebral region, decreased sensitivity, muscle tension or strain, difficulty moving), additional symptoms may appear:
- symptoms of “acute abdomen” - pain in the upper part of the peritoneum, tension in the abdominal muscles, indigestion, heartburn, nausea;
- impaired swallowing function, sensation of a lump in the throat;
- pain in the sternum, numbness of the arm on the affected side, with left-sided thoracic radiculitis - symptoms of angina pectoris, coronary heart disease, with right-sided - pneumonia, pleurisy.
Acute or chronic radiculitis in the acute phase may be accompanied by an increase in temperature.
Many psychotherapist patients ask themselves whether it is necessary to spend the rest of their lives treating the symptoms of laryngeal neurosis, walking around the neighborhood or contemplating a cup on their own table?
Worth seeing: How to relieve constant tension in the head during neurosis?
The fact is that when the technique is fully mastered and begins to “work,” the neurosis tends to recede.
When a person leaves the house with a life-saving pill for, say, a vegetative nervous attack, then most often no attack happens to him.
The reason is that the psyche knows about the proximity and availability of the “saving pill”, so even if the autonomic system fails a little, a strong attack will not follow, since the absence of a person’s anxiety will not allow the failure to develop into an attack.
In the event that a person left a hypothetical effective pill at home and found out about it while being away from his own apartment, the likelihood that he will have an attack is very high.
And this is not a matter of the law of meanness - it’s just that anxiety caused by seeming helplessness without medicine will become a catalyst for a conflict between the sympathetic and parasympathetic systems, and a neurotic attack will develop with all the inherent symptoms, individual in each individual case.
Mastering the techniques for self-treatment of a lump in the throat due to neurosis will become that very “saving pill” that a person will always have at hand, that is, in the head.
This fact will deprive him of unnecessary anxiety, and a correctly and productively conducted psychotherapy session will reveal internal conflicts that provoke neuroses, and then the person will be psychologically healthy.
Glossopharyngeal nerve and what diseases occur with it
There are a huge number of diseases in modern neurology, and most of them are associated with inflammation or pinched nerves. This article will discuss the cranial nerve, which is called the glossopharyngeal nerve, its anatomy, functions, types of damage and treatment methods. However, first things first...
Anatomy and function of the nerve
The glossopharyngeal nerve (GN) is cranial and is considered the IX pair. From an anatomical point of view, it does not have the most complex structure, but it is not the simplest either. So, the anatomy of the glossopharyngeal nerve:
The nerve contains motor, parasympathetic and sensory fibers. The YAN consists of three sections:
- Tympanic nerve.
- Lesser petrosal nerve.
- Tympanic plexus.
In addition, like any cranial nerve, it has several branches, including:
- pharyngeal branches (innervation of the pharynx occurs together with the branches of the vagus nerve of the same name);
- carotid branch (innervates the carotid glomus);
- branch of the stylopharyngeal muscle (innervates this muscle);
- branches of the tonsils (innervate the tonsils, respectively, are located near them, are considered the shortest branches);
- lingual branches (located in the posterior third of the tongue and are responsible for the taste and general sensitivity of the tongue).
The carotid glomus is an anatomical formation located near the carotid artery, which is designed to regulate blood pressure. Dysfunction of this formation can lead to health problems.
The nuclei of the glossopharyngeal nerve are located at the back of the tongue and include:
- Salivary nucleus (parasympathetic).
- Nucleus of the solitary tract (responsible for taste).
- Double nucleus (motor).
An interesting feature of the topography of the nerve nuclei is the fact that not only the nerve fibers originate in them, but also in other, no less important cranial nerves. For example, the accessory nerve (the accessory nerve innervates the muscles responsible for turning the head and the trapezius muscles) or the vagus (innervates a large number of internal organs).
Anatomy of a nerve
The nerve circuit is quite simple, but the same cannot be said about the functions.
The main function of the glossopharyngeal nerve is undoubtedly the determination of taste, however, it is not the only one, since it was previously indicated that the nerve contains both motor and parasympathetic fibers.
The motor function consists of innervation of the stylopharyngeal muscle, which raises and lowers the pharynx. As for the parasympathetic function, these fibers contribute to the production of the salivary glands.
Also, a simple function includes the sensitivity of some areas inside the mouth (tonsils, palate, tympanic cavity, Eustachian tube).
Causes of neuralgia
Like any other, this nerve is predisposed to damage, and most of the reasons indicate the peripheral nature of the ailments (that is, not related to the central nervous system).
Main reasons
There are two subtypes of illnesses:
- Primary (hereditary predisposition, often an independent disease).
- Secondary (occurs as a result of a concomitant disease, does not develop independently).
Neuropathy or neuralgia of the glossopharyngeal nerve can occur under the influence of the following factors and diseases:
- atherosclerosis;
- ENT diseases (otitis, tonsillitis, sinusitis);
- infectious diseases (flu, acute respiratory infections);
- compression of the nerve at any stage of its passage (a tumor or wound may contribute to this);
- general intoxication of the body;
- vascular aneurysms;
- oncology in the larynx;
- pinched or damaged tonsils;
- vegetative-vascular dystonia.
In some cases, when the cause of the disease cannot be determined, the doctor makes a diagnosis of idiopathic neuralgia of the glossopharyngeal nerve. Treatment in such a situation is no different from usual.
Clinical manifestations
Glossopharyngeal neuralgia (neuritis) occurs more often in men over the age of 40 and has several characteristic symptoms, including:
- one-sided severe pain syndrome (paroxysm), which lasts up to three seconds (as a rule, the painful sensation begins to diverge from the root of the tongue, gradually moving to the tonsils, pharynx and ears);
- it is possible that the pain will radiate to the eyes, neck or lower jaw;
- dry mouth (this symptom is not permanent, but only at the time of the attack, and after the pain passes, strong salivation is observed. Depending on the human body, this condition may not manifest itself, if other secretory glands are working well, then the compression of the parotid gland will go unnoticed );
- problems with chewing or swallowing saliva (in most cases it goes unnoticed);
- loss of sensitivity to the position of the tongue in the mouth;
- loss of consciousness;
- tinnitus;
- dizziness;
- “flies” before the eyes;
- weakness in the body.
Autonomic symptoms are also present, including:
- Redness of the skin (on the neck and chin).
- The feeling of the presence of a foreign body in the throat (a rare manifestation), because of this sensation, the patient begins to be afraid to eat, as it seems to him that there is a foreign body in the throat. In this regard, mental disorders are possible.
A provoking factor for the development of internal pain syndrome can be:
- sudden movement of the head or tongue;
- irritation of the tongue from an excessively hot or cold drink;
- coughing;
- chewing food;
- conducting a conversation;
- yawn.
One of the hallmark symptoms of YAN is a change in taste. For example, the patient often begins to feel bitterness in the mouth.
The clinical picture mistakenly indicates to the doctor that the patient has cholecystitis and he refers him for a gastroenterological examination, instead of a neurological one.
Another symptomatic mistake can occur directly with the neurologist. Thus, the pain that is characteristic of glossopharyngeal neuralgia can easily be confused with idiopathic trigeminal neuralgia, and it is possible to distinguish these two diseases only with the use of instrumental diagnostics.
Treatment
Glossopharyngeal neuralgia is treated in several ways, including:
- Medication.
- Surgical.
Additionally, it is possible to use traditional medicine recipes. However, home treatment methods should not be used instead of drugs prescribed by the doctor, but together with them, in this case the therapeutic effect will be higher.
During the recovery period, it is possible to use physiotherapeutic procedures. It is also possible to use physiotherapy in conjunction with drug therapy.
Conservative treatment
Treating a patient with pills is not always bad, since conservative treatment causes less harm to the body, despite the fact that it takes longer. As a rule, a patient with glossopharyngeal neuralgia is prescribed:
- painkillers (the most important drug in therapy, since acute pain can drive you crazy. To eliminate pain, the patient is shown a 10% solution of cocaine, which is rubbed into the root, and if this does not help, novocaine 1–2% is injected under the root of the tongue. In addition In addition, they may additionally prescribe non-narcotic painkillers that are taken orally);
- sedatives, hypnotics, antidepressants and antipsychotics (prescribed for severe pain);
- anticonvulsants (carbamazepine, phenytoin);
- immunostimulating medications (the body absolutely needs support);
- vitamin complexes (traditionally, B vitamins are necessary for the nervous system, and a multivitamin complex, iron, etc. would also be useful).
As for physiotherapy, the following procedures have a good effect:
- diadynamic therapy (treatment with pulsed current 50–100 Hz);
- SMT therapy for the larynx and tonsils (modulated alternating current therapy);
- galvanization (exposure to direct current 50 mA);
- electrophoresis.
Surgical intervention
The main condition for surgical intervention is the lack of effect from conservative treatment. Inflammation of the glossopharyngeal nerve can take quite a long time to be treated, but after a while it will become clear to the doctor whether there are positive results or not.
There is only one correct operation - resection of the hypertrophied styloid process or removal of tissue that has grown over the nerve and thereby compressed it. This type of surgery is performed under general anesthesia.
As for the treatment of neuralgia in a child, there are no special differences, with the exception of a reduced dosage of medications and the exclusion of some drugs from the course.
ethnoscience
As you know, the best remedy for treating any disease (in fact, not all) is home medicine. In the case of inflammation of the lingual nerve, this rule applies. Below are several recipes that can be used in parallel with the main treatment, after consulting with your doctor.
Willow bark decoction
10 g of bark is boiled for 20 minutes, then cooled and taken up to five times a day, one tablespoon
Rare ointment
As you know, radish horseradish is not sweeter, so any vegetable will do for rubbing into the affected area. It is necessary to grate any of the vegetables on a fine grater and simply rub it into the place where the problem is felt.
Radish
Valerian tincture
1 tablespoon of valerian root (can be replaced with rue) is infused in boiled hot water for at least 30 minutes. You need to take the tincture once a day, one glass.
Salt compress
Dissolve two tablespoons of salt in warm water and from the resulting solution you can make salt compresses on the site of pain.
How is a sign formed?
The sensation of a coma forming in the larynx is compared with the detection of a foreign object in the respiratory lumen, which impedes the flow of air, disrupts swallowing movements, causing the development of local pain. A warning sign may appear as a result of neurogenic disorders or inflammation in tissues.
The inflammatory process is characterized by swelling of the tissues of the nasopharynx, hyperthermia, cough and chills. When the structures of the digestive tract are damaged, nausea, heartburn, a lump in the throat and belching of air, gas formation, an unpleasant taste in the mouth and pain in the abdomen appear.
Symptoms of the presence of a coma can be felt in combination with the following indicators:
- constriction of the throat;
- impaired breathing;
- presence of a foreign object;
- painful swallowing;
- frequent involuntary swallowing movements;
- lump in the area where the Adam's apple is located.
In some cases, the sensation that appears disappears spontaneously, but when combined symptoms form, it is necessary to take emergency therapeutic actions, the direction of which is based on the causal factor. When conducting diagnostics, a clinical picture is established that indicates an ongoing pathological deviation.
Symptoms of damage to this nerve
The main symptoms resulting from damage to the recurrent laryngeal nerve include the following:
- Difficulties when trying to pronounce sounds, which manifests itself in hoarseness of the voice and a decrease in its timbre.
- The development of dysphagia, in which swallowing food becomes difficult.
- Whistling, and also noisy inhalations of air.
- Complete loss of voice.
- Choking due to bilateral nerve damage.
- Presence of shortness of breath.
- Impaired general mobility of the tongue.
- Loss of sensitivity of the soft palate.
- Sensation of numbness in the epiglottis. In this case, food can enter the larynx.
- Development of tachycardia and high blood pressure.
- With the development of bilateral paresis, noisy breathing may be observed.
- The presence of a cough with the throwing of gastric juice into the larynx area.
- Respiratory disorder.
VSD and lump in throat: what is the connection?
You can get rid of the feeling of a lump in the throat by taking medications. Your doctor may prescribe the following medications:
- antidepressants that improve the metabolism of serotonin and norepinephrine (Citalopram, Coaxil);
- tranquilizers that help with stress (Mebicar, Afobazol);
- neuroleptics that calm, relieve hysterical attacks and severe agitation (Aminazin, Truxal).
If laryngeal neurosis is severe, then Mezapam, Phenazepam, Clonazepam are used. But they need to be used in small doses, because they are characterized by rapid addiction and poor withdrawal symptoms. The patient may experience weakness and panic.
For throat neurosis, vitamin complexes are prescribed. If this condition is caused by diseases of the spine, then massage, swimming, and physical therapy are recommended. They put Novocaine blockades and prescribe electrophoresis. A nerve block caused by an infection is treated with antibacterial drugs.
In most cases, laryngeal neurosis appears due to internal psychological problems. If a lump in the throat is caused by excessive irritability, imbalance, or hysteria, then you need to visit a psychotherapist who knows how to get rid of such negative emotions and will help stabilize the nervous system.
Sessions with a psychotherapist include the following:
- searching for the reason that caused the emotional conflict;
- learning to ignore such a reason;
- replacing it with a positive attitude.
Function and structure of the aortic arch and its branches
The blood supply to the human body is provided by the pumping option of the heart and two hemodynamic circles. The aorta is the functional origin of the great circle, which starts from the left ventricle.
The vessel is characterized by the largest lumen diameter (2.5-3 cm), wall density and the number of elastic fibers. In the thoracic cavity, the aorta passes through three sections - ascending, arches and descending.
The initial segment of the vessel ensures the delivery of blood to vital organs - the brain, heart and lungs.
The aortic arch is the intermediate part of the vessel, which is located between the bulb (located in the pericardial sac) and the descending section adjacent to the spinal column. The highest point of the segment is projected onto the edge of the manubrium of the sternum, where pulsation is noted in pathologies.
The convex part of the aortic arch faces upward, and the concave part faces downwards. In the thoracic cavity, the vessel intersects with the left main bronchus and passes into the descending section at the level of the fourth vertebra.
Topographic anatomy distinguishes three sections of the arch, the characteristics of which are presented in the table:
Vessel section Key structures
| Elementary | Superior vena cava on the right edge |
| Average |
|
| Terminal (final) | The isthmus of the aorta in the transition area (narrowed section), where coarctation, stenosis and other pathologies develop |
The ligament arteriosus is a collapsed vessel (ductus botallus), which in the prenatal period connected the aorta and the pulmonary trunk.
The middle aorta provides blood supply to the head, neck and chest cavity through the main branches and branching small arteries. The characteristics of the vessels are presented in the table:
Aortic branch Localization
| Brachiocephalic trunk | Along the anterior surface of the trachea, moving to the right from the main trunk. Branches at the level of the outer edge of the sternocleidomastoid muscle |
| Left common carotid artery | Directed up and to the left on the side of the neck |
| Left subclavian artery | It is part of the neurovascular bundle located behind the collarbone. Continues into the axillary region |
Histological characteristics – elastic type artery, consisting of three layers:
- internal (intima) – a smooth membrane, the surface of which prevents thrombus formation;
- middle (media) – a large number of elastic fibers that maintain vessel tone and wall density (protection against rupture at high pressure levels);
- external (adventitia) - a thin connective tissue membrane.
Functions
The aortic arch and its branches provide the delivery of oxygenated blood to other arterial trunks presented in the table:
Vessels Area of blood supply
| Carotid arteries |
|
| Subclavian arteries |
|
Additional functions of the vessel:
- discharge of blood from the pulmonary trunk during intrauterine development (with a closed pulmonary circulation);
- maintaining standard blood pressure levels.
Diagnosis of pathology
Vascular pathologies are one of the most common causes of disability in young people. Making a clinical diagnosis of aortic lesions requires additional research methods presented in the table:
Name of the survey Essence of the method What allows you to determine
| Duplex scanning (ultrasound) of the aortic arch |
|
|
| Aortography |
|
|
| Multislice computed tomography (MSCT) |
|
|
| Magnetic resonance imaging (MRI) |
|
|
The choice of method is determined by the patient’s complaints and age:
- Ultrasound is recommended for children;
- for adults, an MRI examination is considered the “gold standard”.
Before using contrast agents, the doctor must test for allergic reactions to dyes. Ignoring the order leads to life- and health-threatening consequences.
Contraindications to the use of contrast methods:
- allergy to dyes (the most common preparations contain iodine);
- renal failure;
- breastfeeding (allowed 48 hours after the procedure);
- blood clotting pathologies (hemophilia, thrombocytopathy and others);
- severe conditions of the patient (post-resuscitation illness, shock, agony);
- thyrotoxicosis;
- diabetes mellitus type II;
- high level of creatinine in the blood (a marker of impaired renal excretory function).
Major diseases of the aortic arch
Features of the structure and functions of the aortic arch, high pressure and turbulent blood flow contribute to the frequent formation of disorders. The most common pathologies and characteristic changes are presented in the table:
Disease Brief description
| Nonspecific aortoarteritis (Takayasu syndrome) | Vasculitis is an inflammatory disease of autoimmune origin. Leads to damage to the vessel, proliferation in the connective tissue and blockage of the lumen |
| "Cervical arch" | Congenital elongation of the aortic arch |
| Atherosclerosis | The appearance of lipid plaques on the vessel wall, prone to destabilization and rupture. Main reasons:
Sclerosis leads to aortic stenosis, dissection and aortic aneurysm |
| Coarctation | A congenital defect manifested in the form of segmental narrowing of the aorta. Most often located in the area where the arc transitions to the descending part. Requires surgical treatment |
| Hypoplasia | Underdevelopment of vascular tissue in the womb. Surgery required |
| Aneurysm | Local dilatation of a section of a vessel due to wall weakness. Requires elective surgical treatment due to risk of sudden rupture and massive internal bleeding |
| Right arc | Violation of organ formation in the embryonic period: the aortic arch turns not to the left, but to the right, and spreads over the right bronchus. In most cases no treatment is required |
| Calcinosis | Accumulation of calcium salts and hardening of the artery wall. The vessel becomes less elastic and fragile, which often leads to ruptures |
| Double arc | Congenital defect characterized by bifurcation of the aorta:
The departments are interconnected. Pathology requires surgical intervention |
| Delamination | Rupture of the aorta at the site of the aneurysm. The prognosis depends on the degree of damage. High mortality rate |
Cartilaginous skeleton
The study of the innervation of the larynx becomes easier if you know the cartilages that make up its composition. After all, the name of the nerve often corresponds to the name of the cartilage.
The main cartilage of the larynx is called the cricoid. In front it forms an arc, and in the back it looks like a quadrangular plate. Above it is the thyroid cartilage, which is the largest of all the structures of the larynx. This formation consists of two plates that unite at the front at a certain angle.
Another cartilage of the larynx is the arytenoid. In its shape, it resembles a pyramid, in which a base and an apex are distinguished. Moreover, the apex is facing upward and somewhat posteriorly, and the base is facing downward and anteriorly.
The epiglottis is located most superiorly - elastic cartilage. It closes the entrance to the larynx during swallowing, which prevents food from entering the airways.