What is brachial plexopathy?
Plexopathy is a disorder in the functioning of the nerve trunks that make up the plexus. A common cause of this condition is excessive stress on the shoulders, arms, or injury in the shoulder area.
Brachial plexus neuralgia is a very unpleasant condition caused by compression of nerve fibers, which is difficult to diagnose. The plexus itself does not become inflamed, but pain occurs due to inflammation or swelling of the surrounding tissues.
With brachial plexus neuralgia, muscle spasms occur after physical exertion, colds, or hypothermia. Since men have a higher level of stress than women, they are more often exposed to the disease.
On this topic
- Neuralgia
What is the danger of a pinched nerve in the leg?
- Natalia Sergeevna Pershina
- May 25, 2020
As a person ages, atherosclerotic changes occur in the blood vessels, so this disease usually occurs in older people. Quite often, brachial plexopathy is mistakenly confused with heart attacks.
The pain may suddenly subside for a while, but the attack may soon recur.
The following forms of this disease are distinguished:
- primary, occurs without causative diseases;
- secondary, occurs as a result of various diseases.
Painful sensations with neuralgia can be of a different nature: from piercing acute to unbearable burning. If the disease persists for a long time, serious complications can develop.
Departments
The spinal cord has the following parts:
- Coccygeal
- Sacral.
- Lumbar.
- Chest.
- Cervical.
Each part has segments. Pairs of spinal nerves extend along the entire length of the cord. There are 31 in total. The number of spinal nerves, depending on the segment, is as follows:
- Coccygeal - 1-3.
- Sacral – 5.
- Lumbar – 5.
- Infants – 12.
- Neck – 8.
Below, the spinal nerves form the cauda equina. During the growth of the body, the cord does not have time to reach the length of the canal. In this regard, the spinal nerves are forced to descend, exiting the foramina.
Causes
The main reason for the formation of brachial plexopathy is muscle spasms. Most often, these contractions occur after physical stress, injury, or hypothermia.
Also among the causes of the disease are the following:
- intoxication of the body: heavy metals, infectious in nature or due to alcohol consumption;
- impaired metabolism and excess weight;
- the course of concomitant diseases, such as diabetes mellitus or diseases of the gastrointestinal system;
- constant depression and stressful shocks;
- the formation of osteochondrosis of the thoracic or cervical spine.
Any of the above factors can provoke tissue swelling, which causes compression of the nerves and the development of plexopathy.
Symptoms
Brachial plexopathy can present with a variety of signs and symptoms.
Among the important signs are the following:
- Severe pain, the localization of which is difficult to determine due to its unclear boundaries. It is permanent in nature, in rare cases it is periodic. Pain can occur in the inner part of the arm and spread throughout the body, for example, under the shoulder blade or into the chest.
- Increased sweating in the area of the shoulder joint.
- Light twitching .
- Change in skin color The skin may turn pale or, conversely, turn red.
- Some restrictions of movement in the shoulder joint.
On this topic
- Neuralgia
13 Causes of Facial Neuralgia
- Natalia Sergeevna Pershina
- May 24, 2020
In most cases, damage to the brachial plexus is unilateral.
It can be noted that a characteristic feature of brachial plexopathy is that pain can continuously disturb the patient both day and night. A rather unpleasant moment can be the appearance of various neurological signs - weakening of some reflexes, sensory disturbances and others.
Superficial neck loop. Greater auricular nerve. Formation of spinal nerves
The cervical plexus (plexus cervicalis) is formed by the anterior branches of the four upper cervical spinal nerves (CI-C IV). In the plexus, in addition to the branches that form it, there are three loops and branches extending from them, which can be divided into three groups: cutaneous, muscular and connective ().
Cutaneous branches
. 1. The lesser occipital nerve (n. occipitalis minor) from roots C II - C III is directed to the posterior edge of the sternocleidomastoid muscle and, leaving it, follows upward and backward. The nerve branches in the skin of the occipital region and the upper edge of the auricle, bordering in front with the area of innervation of the greater auricular nerve and behind with the greater occipital nerve. It also connects with the branches of the facial nerve. 2. The great auricular nerve (n. auricularis magnus) from roots C III - C IV goes around the posterior edge of the sternocleidomastial muscle, goes up to the auricle, dividing into two branches: anterior and posterior. The anterior branch ends in the skin of the parotid gland and the concave surface of the auricle, the posterior branch ends in the skin of the convex surface of the auricle and in the skin behind the ear. The nerve has intermittent connections with the lesser occipital nerve and the posterior auricular nerve. 3. The cutaneous, or transverse, nerve of the neck (n. transversus colli), from roots C II - C III, bends around the posterior edge of the sternocleidomastial muscle, follows forward, dividing into a number of branches ending in the skin of the anterolateral region of the neck. It connects with the cervical branch of the facial nerve and forms a superficial cervical loop with it. 4. Supraclavicular nerves (nn. supraclaviculares) from roots C III -C IV emerge from the posterior edge of the sternocleidomastial muscle below the previous nerve, diverge in a fan-shaped manner, ending in the skin of the supraclavicular triangle. Topographically they are divided into anterior, middle and posterior supraclavicular nerves.
Muscular branches
can be divided into short and long. Short, or actually muscular, branches (CI -C IV) begin from individual cervical nerves and innervate the deep and almost all superficial muscles of the neck. The long branches include: the branch of the trapezius muscle (C II -C IV), which connects with the branches of the accessory nerve and together with them innervates the specified muscle; a branch of the sternocleidomastoid muscle (C II - C III), which connects with the branches of the accessory nerve going to the upper parts of the specified muscle, and the phrenic nerve (n. phrenicus) from the roots of C III - CV, the most powerful nerve of the cervical plexus. The latter is a mixed nerve, since, along with a large number of motor fibers, it contains sensory and autonomic fibers. Following the anterior scalene muscle in front of the subclavian artery, the phrenic nerve passes into the anterior mediastinum, where it sends branches to the pleura and pericardium. The left nerve lies closer to the anterior chest wall and approaches the diaphragm at the apex of the heart; the right one, located slightly deeper than the left one, penetrates the diaphragm near the inferior vena cava. Along its course, the nerve gives off a number of branches. The connecting branches connect the phrenic nerve with the middle and lower cervical ganglia of the sympathetic trunk, with the subclavian loop and with the perivascular nerve plexuses of nearby arteries. Sometimes the connecting branch with the subclavian loop is so long that it is called the periphrenic nerve. The branches of the pericardial sac, together with the vessels of the same name, penetrate into the thickness of the pericardial sac; pleural branches approach the mediastinal pleura in the region of the lung root; phrenic branches are the terminal branches of the nerve. Before insertion into the diaphragm, the nerve is divided into three branches: anterior, posterior and lateral, which form a network-shaped plexus in the thickness of the diaphragm; it sometimes connects with the branches of the intercostal nerves. In the anterior part of the tendon stretch there is a connecting branch between the right and left phrenic nerve. The phrenic-abdominal branches are the connecting branches between the phrenic nerve and some autonomic plexuses: the right and left inferior phrenic plexuses, pulmonary plexus, superior gastric plexus, and also approach the peritoneum, liver and anterior abdominal wall.
Connecting branches
The cervical plexus can be divided into three groups: 1) the connecting branch (C I) to the arch of the cervical loop (the branches extending from the loop innervate the group of infrahyoid muscles); 2) connecting branches from C II, C III and C IV, which approach the external branch of the accessory nerve, innervating the sternocleidomastoid and trapezius muscles; 3) connecting branches (CI-C III), approaching the upper and middle cervical nodes of the sympathetic trunk.
Pathology of the cervical plexus - see Neuralgia, Plexitis.
The sources from which the cervical plexus is formed are the anterior branches of the first four and five cervical spinal nerves.
Topography. The plexus is formed by connecting the anterior branches with three arcuate loops that lie on the muscles: the levator scapulae, the middle scalene, and the splenius cervicalis. The projection of the plexus falls on the level of the transverse processes of the first four cervical vertebrae.
Branches and areas of innervation. The branches are divided into skin, muscle and mixed - short and long. The exit of the short branches is projected along the posterior edge of the sternocleidomastoid muscle between the upper and middle thirds of its length, which is taken into account when performing local anesthesia. The long branch, the phrenic nerve, lies on the anterior scalene muscle and descends into the chest cavity between the subclavian vein and subclavian artery.
Each plexus (right and left) has the following branches.
Short cutaneous nerves - greater auricular, lesser occipital, transverse cervical nerve, supraclavicular. They innervate the skin of the head and ear (back), neck, upper chest, and shoulder girdle.
Motor (short muscle) nerves to the muscles - long of the head and neck, scalene; direct anterior and lateral muscles of the head; anterior intertransverse and levator scapulae.
The second group of muscle branches are long motor nerves, including:
- a deep cervical loop that occurs when the descending branch of the hypoglossal nerve connects with the muscle fibers of the 1st spinal nerve and the anterior branches of the 2nd and 3rd cervical spinal nerves - for the innervation of the infrahyoid muscles: sternohyoid, sternothyroid, omohyoid, thyrohyoid;
- the loop is located above the common carotid artery just above the intermediate tendon of the omohyoid muscle;
- superficial cervical loop - from the confluence of the cervical branch of the facial nerve and the upper branch of the transverse nerve of the neck - to innervate the subcutaneous muscle and skin of the neck;
- long muscle branches - to the trapezius and sternocleidomastoid muscles.
The mixed nerve, the phrenic nerve, is the longest, which descends along the anterior scalene muscle to the superior thoracic aperture. Between the subclavian artery and vein it penetrates the chest cavity, passes in the upper and middle mediastinum along the thymus and pericardium anterior to the roots of the lungs and enters the diaphragm. The right nerve in the upper mediastinum lies on the superior vena cava, and together with the inferior vena cava penetrates the abdominal cavity and innervates the liver and gall bladder through the celiac plexus. Phrenicus syndrome is known in clinical medicine. When pressing in the right hypochondrium on the projection of the inflamed gallbladder, the pain radiates to the neck.
The phrenic nerves give off sensory and secretory branches to the thymus gland, mediastinal and phrenic pleura, pericardium and heart, vena cava and root of the lung, liver and gall bladder, and peritoneum. The motor branches are directed to the diaphragm muscle. Additional sympathetic branches enter the nerve through connection with the subclavian sympathetic loop, stellate ganglion and celiac plexus to innervate the organs and vessels of the thoracic and abdominal cavities.
ANTERIOR BRANCHES OF THE SPINAL NERVES
POSTERIOR BRANCHES OF THE SPINAL NERVES
BRANCHES OF SPINAL NERVES
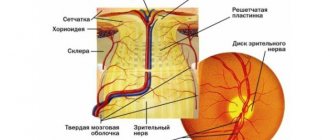
FORMATION OF SPINAL NERVES
There are 31 pairs of them, departing from the spinal cord by two roots: anterior (ventral, motor and autonomic) and posterior (dorsal, sensitive). In the area of the intervertebral foramen, the roots unite into one trunk - the mixed spinal nerve. The nerves, starting from the VIII cervical and ending with the II lumbar, contain sympathetic autonomic nerve fibers, which are axons of the autonomic nuclei of the lateral horns of the corresponding parts of the spinal cord. The sacral nerves contain parasympathetic nerve fibers - axons of the autonomic nuclei of the sacral spinal cord (segments S II -S IV).
After emerging from the intervertebral foramen, each nerve is divided into four branches: anterior, posterior, connective and meningeal.
The anterior branches innervate the trunk and limbs; the posterior branches innervate the muscles and skin of the back of the head, back and upper part of the gluteal region; the connecting branches are directed to the nodes of the border sympathetic trunk; meningeal sensory branches return to the spinal canal, innervating the spine and the membranes of the spinal cord.
The following posterior branches have individual names.
Posterior branch of the first cervical nerve - the motor suboccipital nerve, innervates the short muscles of the back of the head
· The posterior branch of the second cervical nerve is called the greater occipital nerve. This nerve is mixed and innervates the muscles and skin of the back of the head.
· The sensory fibers of the posterior rami of the lower lumbar and sacral nerves are called the superior and middle gluteal nerves, innervating the skin of the upper part of the gluteal region.
The anterior branches are the longest and thickest; after exiting, they connect with each other, forming the nerve plexuses: cervical, brachial, lumbar, sacral and coccygeal. Nerves that innervate the skin and muscles and internal organs of certain areas depart from the plexuses. The anterior branches of the thoracic SMN plexuses do not form.
Formed by the anterior branches of the first four cervical SMNs (C 1 -C 4). Located on the side of the transverse processes of the upper cervical vertebrae, on the deep muscles of the neck. Its nerves emerge from under the middle of the posterior edge of the sternocleidomastoid muscle and give off sensory, motor and mixed branches (nerves).
The lesser occipital nerve, sensory, ascends along the posterior edge of the sternocleidomastoid muscle and innervates the skin of the occipital and mastoid regions.
The large auricular nerve, sensitive, runs up the outer surface of the sternocleidomastoid muscle, goes around the back of the auricle, forming connections with neighboring nerves. Innervates the skin of the auricle, external auditory canal, face (side) and temporal region.
The transverse nerve of the neck, sensitive, transversely crosses the sternocleidomastoid muscle, pierces the platysma, and innervates the skin of the anterolateral region of the neck from the chin to the clavicle.
The supraclavicular nerves, sensory, descend in three bundles into the supraclavicular and subclavian regions, innervating the skin of these areas, the skin over the pectoralis major and deltoid muscles.
The motor nerves innervate the deep muscles of the neck and connect with the branch of the hypoglossal nerve (XII pair of cranial nerves), forming a cervical loop that innervates the muscles lying below the hyoid bone.
The phrenic nerve, mixed, descends down the anterior scalene muscle, enters the thoracic cavity through the superior thoracic aperture, reaches the diaphragm and passes into the abdominal cavity. Motor fibers innervate the diaphragm, sensory fibers innervate the pleura, pericardium and liver ligaments.
Cervical plexus,
plexus cervicatis ,
is formed by the anterior branches of the 4 upper cervical (Ci-Civ) spinal nerves (Fig. 179).
These branches are connected by three arched loops. The plexus is located at the level of the four upper cervical vertebrae on the anterolateral surface of the deep muscles of the neck (the levator scapulae muscle, the medial scalene muscle, the splenius muscle of the neck), being covered in front and
on the side by the sternocleidomastoid muscle.
The cervical plexus has connections with the accessory and hypoglossal nerves. Among the branches of the cervical plexus, muscle, cutaneous and mixed nerves (branches) are distinguished (see Fig. 177).
Motor (muscle) nerves (branches) go to nearby muscles: the long muscles of the neck and capitis, the anterior, middle and posterior scalene muscles, the anterior and lateral rectus capitis muscles, the anterior intertransverse muscles and the levator scapulae muscle. The motor branches of the cervical plexus also include the cervical loop,
dnsa cervicdlis .
The descending branch of the hypoglossal nerve is involved in its formation -
the upper root, radix superior [ anterior ],
containing fibers from the cervical plexus (G), and the branches extending from the cervical plexus -
the lower root, ra dix inferior posterior (
Ci-Ssh) . The cervical loop is located slightly above the upper edge of the intermediate tendon of the scapulohyoid muscle, usually on the anterior surface of the common carotid artery. Fibers extending from the cervical loop innervate the muscles located below the hyoid bone (subhyoid muscles: sternohyoid, sternothyroid, omohyoid, thyrohyoid).
Muscle branches extend from the cervical plexus, also innervating the trapezius and sternocleidomastoid muscles. The sensory (cutaneous) nerves of the cervical plexus arise from the plexus, bend around the posterior edge of the sternocleidomastoid muscle slightly above its middle and appear in the subcutaneous fatty tissue under the subcutaneous muscle of the neck. The cervical plexus gives off the following cutaneous branches: the greater auricular nerve, the lesser occipital nerve, the transverse cervical nerve, and the supraclavicular nerves.
1Great auricular nerve, n.
aurlculdris mdgnus ,
is the largest cutaneous branch of the cervical plexus. Along the outer surface of the sternocleidomastoid muscle, it is directed obliquely and forward to the skin of the auricle, external auditory canal and the region of the retromandibular fossa.
2The lesser occipital nerve, n.
occipitdlls minor ,
emerging from under the posterior edge of the sternocleidomastoid muscle, rises up along this muscle and innervates the skin of the inferolateral part of the occipital region and the posterior surface of the auricle.
3 The transverse nerve of the neck, p.
transversus SDS,
from the exit point at the posterior edge of the sternocleidomastoid muscle goes horizontally forward and is divided into
upper and lower branches, rr . superidres et inferiores .
It innervates the skin of the anterior and lateral areas of the neck. One of its superior branches connects with the cervical branch of the facial nerve, forming the superficial cervical loop.
4. Supraclavicular nerves, pp.
supraclavlculdres
(3-5), emerge from under the posterior edge of the sternocleidomastoid muscle, directed downward and posteriorly in the fatty tissue of the lateral neck. They innervate the skin in the supraclavicular and subclavian regions (above the pectoralis major muscle, see Fig. 177).
According to their position, medial, intermediate and lateral
(posterior)
supraclavicular nerves, pp. sup - raclaviculares mediates , intermedii et laterales .
,
The phrenic nerve,
p. phrenicus ,
is a mixed branch of the cervical plexus. It is formed from the anterior branches of the III-IV (sometimes V) cervical spinal nerves, descends down the anterior surface of the anterior scalene muscle and penetrates the chest cavity through the upper thoracic aperture (between the subclavian artery and vein). Initially, both nerves go in the upper mediastinum, then pass into the middle mediastinum, located on the lateral surface of the pericardium, anterior to the root of the corresponding lung. Here the phrenic nerve lies between the pericardium and the mediastinal pleura and ends in the thickness of the diaphragm.
The motor fibers of the phrenic nerve innervate the diaphragm, the sensory fibers - the pericardial branch, g.
pericar - diacus ,
- the pleura and pericardium.
Sensitive phrenic-peritoneal branches, rr . phrenicoabdominales ,
pass into the abdominal cavity and innervate the peritoneum covering the diaphragm. The branches of the right phrenic nerve pass, without interruption (in transit), through the celiac plexus to the liver.
166. Branches of the supraclavicular part of the brachial plexus, areas of innervation
.
The brachial plexus,
plexus brachidlis ,
is formed by the anterior branches of the four lower cervical (Cv-Cvni), part of the anterior branch of the IV cervical (Civ) and I thoracic (Thi) spinal nerves (see Fig. 179).
In the interstitial space, the anterior branches form three trunks: the upper trunk, truncus
superior ,
the middle trunk,
truncus medius ,
and
the lower trunk, truncus inferior .
These trunks emerge from the interscalene space into the greater supraclavicular fossa and stand out here, together with the branches extending from them, as the supraclavicular part,
pars supraclaviculdris ,
of the brachial plexus.
The trunks of the brachial plexus, located below the level of the clavicle, are designated as the subclavian part, pars infraclaviculdris ,
brachial plexus.
Already in the lower part of the large supraclavicular fossa, the trunks begin to divide and form three bundles, fasciculi ,
which in the axillary fossa surround the axillary artery on three sides.
On the medial side of the artery there is a medial bundle, fasciculus medialis ,
on the lateral side there is a lateral
bundle, fasciculus latera - lis ,
and behind the artery there is
a posterior bundle, fasciculus posterior .
The branches extending from the brachial plexus are divided into short and long. Short branches arise mainly from the trunks of the supraclavicular part of the plexus and innervate the bones and soft tissues of the shoulder girdle. Long branches arise from the infraclavicular part of the brachial plexus and innervate the free upper limb. Short branches of the brachial plexus.
R/short branches of the brachial plexus include the dorsal nerve of the scapula, the long thoracic nerve, the subclavian, the suprascapular, the subscapular, the thoracodorsal nerve, which arise from the supraclavicular part of the plexus, as well as the lateral and medial thoracic nerves and the axillary nerve, which originate from the subclavian part of the brachial plexus bundles.
1
Dorsal nerve of the scapula,
p. dorsalis scapulae ,
starts from the anterior branch of the V cervical nerve (Cv), lies on the anterior surface of the muscle that lifts the scapula. Then, between this muscle and the posterior scalene muscle, the dorsal nerve of the scapula is sent back along with the descending branch of the transverse cervical artery and branches into the levator scapulae muscle and the rhomboid muscle.
2
The long thoracic nerve,
n. thordcicus longus
(Fig. 180), originates from the anterior branches of the V and VI cervical nerves (Cv-Cvi), descends down behind the brachial plexus, lies on the lateral surface of the serratus anterior muscle between the lateral thoracic artery in front
and
the thoracodorsal artery posteriorly, innervates the serratus anterior muscle.
3
The subclavian nerve, n.
subclavius
(Cv), is directed by the shortest route to the subclavian muscle in front of the subclavian artery.
4
The
suprascapuldris nerve (Cv-Cvn) extends laterally. back. Together with the suprascapular artery, it passes through the notch of the scapula under its superior transverse ligament into the supraspinous fossa, and then under the acromion into the infraspinatus fossa. Innervates the supra- and infraspinatus muscles, the capsule of the shoulder joint.
5
Subscapular nerve,
n. subscapuldris
(Cv-Cvii);
runs along
the anterior surface of the subscapularis muscle, innervates this and the teres major muscles.
6
The thoracodorsal nerve,
n. thoracodorsalts
(Cv-Cvn), along the lateral edge of the scapula descends to the latissimus dorsi muscle, which it innervates.
7
Lateral imedial thoracic nerves,
nn . pectorales lateralis et medialis ,
start from. lateral and medial bundles of the brachial plexus (Cv-Thi), go forward, pierce the clavipectoral fascia and end in the greater (medial nerve) and lesser (lateral nerve) chest - "
nary muscles,
8
The axillary nerve,
n. axillaris ,
begins from the posterior
brachial plexus (Cv-Cvtn).
Along the anterior surface of the subscapularis muscle it goes down and laterally, then turns back and, together with the posterior circumflex humeral artery, passes through the quadrilateral foramen. After wrapping around the surgical neck of the humerus from behind, the nerve lies under the deltoid muscle. The axillary nerve innervates the deltoid and teres minor muscles, the capsule of the shoulder joint. The terminal branch of the axillary nerve is the superior lateral cutaneous nerve of the shoulder, n. cutaneus brachii lateralis supe rior
it goes around
The cervical plexus (plexus cervicales) is formed by the anterior branches of the four upper cervical (CI-CIV) spinal nerves. The anterior branch (CII) emerges between the anterior and lateral rectus capitis muscles, the remaining anterior branches emerge between the anterior and posterior intervertebral muscles, behind the vertebral artery.
Cervical plexus, its branches and innervated organs
| Nerves (branches) of the cervical plexus | Spinal cord segments | Innervated organs |
| Muscular branches | CI-CIV | Anterior and lateral muscles of the head; long muscles of the head and neck; levator scapulae muscle; scalene and anterior intertransverse muscles; sternocleidomastoid and trapezius muscles |
| Upper and lower roots of the cervical loop | CI-CIII | Sternohyoid, sternothyroid, omohyoid and thyrohyoid muscles |
| Lesser occipital nerve | CII-CIII | Skin of the lateral part of the occipital region |
| Greater occipital nerve | CIII | Skin of the auricle and external auditory canal |
| Transverse cervical nerve | CIII | Skin of the anterior and lateral areas of the neck |
| Supraclavicular nerves | CII-CIV | The skin of the lateral neck and collarbone area, as well as the skin over the deltoid and pectoralis major muscles |
| Phrenic nerve | Diaphragm, pleura, pericardium, peritoneum covering the diaphragm, liver and gallbladder |
The plexuses are located lateral to the transverse processes, between the origin of the anterior scalene muscle and the longus colli muscle (medially), the middle scalene muscle, the levator scapulae muscle, and the splenius colli muscle laterally. In front and on the side, the plexus is covered by the sternocleidomastoid muscle.
The cervical plexus has connections with the hypoglossal nerve via the anterior branches of the first and second cervical spinal nerves, with the accessory nerve, with the brachial plexus (via the anterior branch of the fourth cervical spinal nerve), with the superior cervical ganglion of the sympathetic trunk.
Muscular branches emerge from the cervical plexus that innervate the long muscles of the head and neck, the scalenes, the lateral and anterior rectus capitis muscles, the levator scapulae muscle, as well as the trapezius and sternocleidomastoid muscles. The cervical plexus also gives off fibers that form the lower root (radix inferior) of the cervical loop. The superior root (radix superior) of this loop is formed by the descending branch of the hypoglossal nerve. Fibers arising from the cervical loop innervate the superficial muscles of the neck located below the hyoid bone.
The sensory branches of the cervical plexus are the lesser occipital nerve, the greater auricular nerve, the transverse cervical nerve and the supraclavicular nerves. These nerves arise from the plexus, bend around the posterior edge of the sternocleidomastoid muscle and emerge from underneath it into the subcutaneous tissue. The longest nerve of the cervical plexus is the phrenic nerve.
- The lesser occipital nerve (n. occipitalis minor) is formed mainly by the branches of the second and third cervical spinal nerves. It exits under the skin at the posterior edge of the sternocleidomastoid muscle, goes upward and posteriorly and innervates the skin behind and above the auricle.
- The great auricular nerve (n. auricularis magnus) consists mainly of fibers of the third and to a lesser extent the fourth cervical spinal nerves. The projection of the exit of this nerve to the neck occurs at the border between the upper and middle thirds of the posterior edge of the sternocleidomastoid muscle. The greater auricular nerve divides into anterior and posterior branches, which run upward. The posterior branch
runs vertically upward and innervates the skin of the posterior and lateral surfaces of the auricle and the skin of the earlobe.
Some of the fibers pierce the cartilage of the auricle and innervate the skin of the external auditory canal. The anterior branch
of the greater auricular nerve runs obliquely forward and innervates the skin of the face in the area of the parotid salivary gland. - The transverse nerve of the neck (n. transversus colli) consists of fibers of the anterior branch of the third cervical spinal nerve. The nerve emerges from under the posterior edge of the sternocleidomastoid muscle, goes forward, gives off superior
and
inferior branches,
which penetrate the subcutaneous muscle of the neck and go to the skin of the anterior neck. The transverse cervical nerve anastomoses with the cervical branch of the facial nerve, the fibers of which enter the neck to innervate the subcutaneous muscle of the neck. - The supraclavicular nerves (nn. supraclaviculares) are formed mainly by branches of the fourth and partially fifth cervical spinal nerves. The supraclavicular nerves appear on the surface of the subcutaneous muscle of the neck at the level of the middle of the posterior edge of the sternocleidomastoid muscle, go down, fan out and innervate the skin above the clavicle and in the upper anterior region of the chest (to the level of the third rib). According to their location, medial, intermediate and lateral supraclavicular nerves are distinguished (nn. supraclaviculares mediales, intermedii et laterales).
- The phrenic nerve (n. phrenicus) is formed mainly by the anterior branches of the third and fourth cervical spinal nerves, descends vertically down the anterior surface of the anterior scalene muscle, passes into the chest cavity between the subclavian artery and vein, medial to the internal mammary artery. Next, the nerve goes next to the dome of the pleura, anterior to the root of the lung, under the mediastinal pleura. The right phrenic nerve
runs along the lateral surface of the superior vena cava, adjacent to the pericardium, and is located anterior to the left phrenic nerve.
The left phrenic nerve
crosses the aortic arch in front and penetrates the diaphragm at the border of the tendon center and its costal part. The motor fibers of the phrenic nerves innervate the diaphragm, the sensory fibers go to the pleura and pericardium (pericardial branch, r. pericardiacus). Part of the branches of the phrenic nerve - the phrenic-abdominal branches (rr. phrenicoabdominales) passes into the abdominal cavity and innervates the peritoneum lining the diaphragm. The right phrenic nerve passes in transit (without interruption) through the celiac plexus to the peritoneum covering the liver and gallbladder.
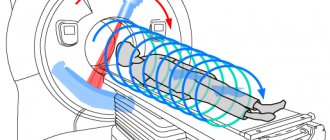
Diagnostics
Due to the similarity of the main symptoms of brachial plexopathy with various other diseases, it is difficult to diagnose. To make an accurate diagnosis, the doctor collects anamnesis and prescribes a diagnostic test.
Main diagnostic methods of the disease:
- Radiography. Using this method, it is possible to identify pathologies of the spine, for example, traces of trauma, osteochondrosis and others.
- Ultrasound examination (ultrasound) to detect the causes leading to damage to the brachial plexus.
- Computed and magnetic resonance imaging. These methods make it possible to detect factors predisposing to the occurrence of this disease (protrusion and hernia in the cervical spine)
- Electroneuromyography, which can be used to determine signs of nerve damage and the speed of impulse transmission along nerve fibers.
Notes[ | ]
- ↑ 1 2 3 4 5 6 7 Nerves
. Biological encyclopedic dictionary. / Ch. editor M. S. Gilyarov. - M.: Soviet Encyclopedia, 1986. - Mikhailov S.S.
Nerves // Great Medical Encyclopedia / ch. ed. B.V. Petrovsky. - M.: Soviet Encyclopedia, 1981. - T. 16: Museums - Nile. — P. 418. - ↑ 1 2 3 4 5 6 7 8 9 Nerves
. Brief medical encyclopedia / Ch. editor B.V. Petrovsky. - M.: Soviet Encyclopedia, 1989. - ↑ 1 2 Nerve fiber
. Biological encyclopedic dictionary. / Ch. editor M. S. Gilyarov. - M.: Soviet Encyclopedia, 1986. - ↑ 12
Kononova, Krol, 1931, stb. 659. - Autonomic nervous system // Brief medical encyclopedia / Editor-in-Chief Academician B.V. Petrovsky. — 2nd edition. - M.: Soviet Encyclopedia, 1989.
- ↑ 1 2 Cervical plexus
- article from the Great Medical Encyclopedia - ↑ 1 2 3 Fedyukovich N. I.
SPINAL NERVES // Human Anatomy and Physiology. - 2nd. - R. n/d.: Phoenix, 2003. - 416 p. — ISBN 5-222-03190-X. - Kononova, Krol, 1931, stb. 662.
- Kononova, Krol, 1931, stb. 662-663.
- Kononova, Krol, 1931, stb. 663-665.
- Neuritis
. Brief medical encyclopedia / Ch. editor B.V. Petrovsky. - M.: Soviet Encyclopedia, 1989. - Radiculitis
. Brief medical encyclopedia / Ch. editor B.V. Petrovsky. - M.: Soviet Encyclopedia, 1989. - Plexit
. Brief medical encyclopedia / Ch. editor B.V. Petrovsky. - M.: Soviet Encyclopedia, 1989.
Treatment
At the initial stage of neuralgia, treatment is quite simple and if all prescribed procedures are systematically followed, it will bring effective results.
On this topic
- Neuralgia
All types of pain in the shoulder blades and their treatment
- Natalia Sergeevna Pershina
- May 24, 2020
The main goal of any treatment method is to eliminate pain and factors that put pressure on the nerve. To achieve good results, the doctor needs to choose a technique that, first of all, should eliminate the disease itself that causes compression of the nerve in the shoulder area and help get rid of the resulting pain for a long time.
Regardless of the stage of the disease, treatment of brachial neuralgia should always be comprehensive. Medications should be taken in combination with various physiotherapeutic procedures.
Medications
To relieve inflammation and pain, the doctor prescribes certain medications.
Among the common ones are the following:
- Non-steroidal anti-inflammatory drugs. The most common of them are Diclofenac, Ketanov and Ibuprofen. These drugs can be prescribed both for topical use in the form of gels or ointments for rubbing into the shoulder, and for oral administration in the form of tablets. Local use of this group of drugs brings quick but short-term relief.
- Analgesics (painkillers) to relieve pain in the shoulder joint. The disadvantage of such therapy is the impossibility of taking them for a long period to avoid side effects. After some time, these drugs are replaced by ointments with anti-inflammatory and analgesic effects.
- Therapeutic drug blockade is carried out for pain of high intensity.
On this topic
- Neuralgia
6 facts about neuralgia of the ear
- Natalia Sergeevna Pershina
- May 24, 2020
Since quite often the disease occurs with depression, various antidepressants are prescribed to normalize the patient’s emotional state.
To achieve an effective result, vitamin injections are prescribed.
Additional Treatments
Complex treatment of brachial plexopathy promotes rapid and complete restoration of motor function of the arm.
In order for drug treatment to bring positive results, it is recommended to combine it with various physiotherapeutic procedures:
- ultrasound with hydrocortisone;
- acupuncture;
- therapeutic electrophoresis using novocaine.
A very important point from the first days of the onset of pain is to reduce the resulting swelling. To achieve this, the doctor may prescribe diuretics, for example, Veroshpiron. The latter has a mild effect on the body and does not contribute to potassium loss.
Strong diuretics (Furosemide or Torsemide), which have an excessive effect, can provoke cramps in the calf muscles. Therefore, they are not prescribed for this disease.
Also effective in the treatment of brachial plexopathy are physical therapy classes, a set of special exercises and gymnastics for the shoulder joints, therapeutic massage, spa treatment, mud wraps, and paraffin treatment. All physiotherapeutic procedures for the treatment of this disease must be carried out under the strict supervision of a specialist.
The patient’s strict adherence to all the doctor’s instructions and recommendations will allow the patient to reduce pain and discomfort from the first days of treatment and completely recover from the disease in a short period.
Internal Contents
The spinal cord contains white and gray matter. The latter consists of neurons. They form three columns in the halves of the spinal cord: lateral, posterior and anterior. In cross section, each of them looks like horns. There are narrow posterior and wide anterior horns. The lateral one corresponds to the vegetative intermediate column of the gray part. The anterior horns contain motor neurons, the lateral horns contain autonomic intercalary neurons, and the posterior horns contain sensory neurons. Renshaw cells are located in this same area. These are inhibitory neurons that slow down motor neurons from the anterior horns. The gray matter is surrounded by white matter, which forms the cords of the spinal cord. There are three of them in each half: side, rear and front. The cords consist of fibers running longitudinally. They, in turn, form bundles of nerves - pathways. Descending - extrapyramidal and pyramidal - are located in the anterior cords, in the white matter. In the laterals – ascending and descending:
- Lateral spinothalamic.
- Rear and anterior (Flexig and Gowers).
- Lateral (pyramidal) corticospinal.
- Red nuclear.
The white matter of the posterior cord includes ascending pathways:
- Burdach's bundle (wedge-shaped).
- Gaulle bundle (thin).
Consequences and possible complications
Plexopathy is a disease that tends to return with some frequency. If no treatment is given for this disease, exacerbations will become more severe, and the intensity of pain will increase. As the disease progresses, the pain becomes very long-lasting.
The most dangerous possible complication of this condition is the development of permanent damage to the nerve trunks. In this case, the patient will be bothered not only by unbearable pain, but also by impaired movement of the upper limbs. If it lasts for a long time, paralysis may occur.
To avoid the development of serious negative consequences, it is recommended to adhere to the rules of prevention:
- at the first signs of illness, consult a doctor;
- avoid heavy physical activity, carrying heavy objects on the shoulder;
- treat chronic diseases accompanied by metabolic disorders (diabetes mellitus, hypothyroidism, anemia, etc.).
Seeing a doctor in a timely manner and following his recommendations will help you fully recover from the disease.