The polio virus can develop in certain parts of the planet as an epidemic. A vaccine was developed several decades ago, but vaccinations cannot completely curb the development of the infectious process.
To achieve this, immunization of the population in different countries must be at least 95%. This result is unrealistic to achieve in developing countries with a small population.
Below is information about when the polio vaccine is given and which categories of citizens are subject to mandatory vaccination.
Disease Information
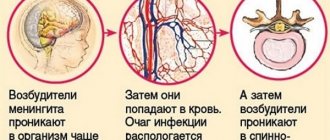
Poliomyelitis can be transmitted through the fecal-oral route. The pathology is also called the disease of dirty hands. In most examples, the disorder develops without symptoms or similar to ARVI, non-serious intestinal infections. Complex forms of polio are caused by virus penetration into the central nervous system and damage to brain cells.
The source of infection is considered to be people who are sick with any type of disease. The virus enters the environment along with feces and mucus from the oral cavity. People become infectious after completing the incubation period, when there are no various clinical manifestations of the disorder.
At this time, the infection is more dangerous for people. A person remains infectious for 2 months after recovery.
Infection occurs for the following reasons:
- Neglect of personal hygiene rules.
- Dirty water.
- Unwashed vegetables, fruits, berries.
Why do people need to be vaccinated?
Poliomyelitis is one of the oldest disorders that affects the body before the onset of disability. There are known cases when the virus enters the nervous system and provokes destructive transformations of neurons. Who should be vaccinated against polio? Vaccination is carried out for people, regardless of age category. If people are not vaccinated, they are at risk and can spread the infection.
At what age is the vaccine first introduced into the body? It is preferable to carry out the necessary procedures as soon as possible. At three months of age the first injection is given. Reasons why children are vaccinated so early:
- This virus is spread throughout the planet.
- After birth, children retain some immunity received from the mother’s body for a short period of time, but its stability lasts for about 5 days.
- The patient spreads harmful microbes in the environment throughout the entire duration of the illness, during full recovery, and for a long time after that. If you vaccinate a child, those around you will not be infected.
- The virus easily spreads through sewage and food.
- There is a possibility of transferring harmful microbes to insects.
- Since children's immune systems have not strengthened, the disease is more often diagnosed in them.
The long incubation period and a large number of complications after infection make the polio vaccine the only effective means of combating the pathology.
Vaccination scheme
Pediatricians have a vaccination schedule that they must adhere to. Each vaccination is given at a certain age. The polio vaccine is no exception. The instructions contain detailed information about this. The first vaccination is given to the baby when he is three months old. The second dose of the vaccine should enter the child’s body after another month and a half, and then another vaccination is given at 6 months.
To obtain a stable and reliable effect, revaccination must be carried out; it is done at 18 months and after another two months. The last time the vaccine should be administered to the body is at the age of 14.
In those countries where the virus that causes this disease has not been completely eradicated, the vaccine is given in the maternity hospital. It is not capable of creating long-term immunity, so full vaccination begins at two months.
You need to know that only five-time vaccination can provide reliable protection against this terrible disease. If for some reason the schedule for the vaccine to enter the body is disrupted, then there is no need to start all over again, but you can simply carry out the missing vaccinations.
Should children be vaccinated?
In the Russian Federation, the polio vaccine is included in the vaccination calendar and is always given to children in the first years of life. Today, protest movements are increasingly making themselves known, seeking to protect children from various injections. They believe that all vaccines only cause harm.
All parents need to think about whether they have ever encountered smallpox, polio, or measles. As a result of the extensive and widespread use of vaccinations, children can be saved from much suffering.
Directions for use and doses
S/c, i/m. Vaccination - 3 injections with an interval of 1 month, then revaccination - after 1 year and every 5-10 years.
Inactivated polio vaccines are injected into the body into the thigh or shoulder area. The injection is given intramuscularly. IPV is included in the National Calendar for the Prevention of Viral and Infectious Diseases. People are being vaccinated according to the approved schedule.
Scheduled vaccination schedule:
- The first dose is given to the baby at 3 months;
- The second injection is given at 4.5 months;
- The last time is vaccinated at six months.
Then revaccinations are carried out at 3 and 6 years. If the schedule is violated, they are immunized according to the standard schedule, maintaining intervals between vaccinations of 1.5 months. Since IPVs are produced in the form of a suspension, they do not require prior dilution. A single dosage is 0.5 ml.
Instructions for use of non-live polio vaccine:
- inspect the container with contents for compliance with quality standards. The liquid should be homogeneous and transparent;
- draw the solution into a sterile syringe;
- wipe the injection site (thigh or shoulder) with an antiseptic (70% alcohol);
- make a puncture, make sure that the needle gets into the muscle;
- administer the vaccine dose and remove the needle;
- again treat the puncture area with alcohol.
Vaccination schedule
The polio immunization scheme was created a long time ago and has not changed for several decades:
- Children were first exposed to polio vaccinations at three months of age.
- After 45 days, repeated vaccination is done.
- At six months of age, the baby is vaccinated again. If a non-live inactivated vaccine is used before this period, OPV can be given to a six-month-old child. These are drops for oral use.
- Revaccination is carried out at the age of one and a half years, then again after 20 months, then when the child turns 14.
When children do not go to school, they need to be vaccinated against this dangerous pathology. With this schedule, all children will be protected.
Where is the polio vaccine administered?
The introduction of the polio vaccine has its own characteristics. The live vaccine is administered orally - the pinkish liquid must be dripped onto the lymphoid tissue of the pharynx for children; for older children, the vaccine must be dripped onto the tonsils. This is necessary to prevent increased salivation, since getting the vaccine into the stomach neutralizes its effect (it will be destroyed under the influence of gastric juice).
Note! If the baby regurgitates, the vaccine administration procedure will need to be repeated.
The inactivated vaccine is administered to children intramuscularly in the thigh area or subcutaneously in the scapula area. For older children, the vaccine is administered intramuscularly, in the shoulder area.
Vaccine classification
Poliomyelitis vaccines are used in the immunization process:
- The oral polio vaccine is produced only in Russia based on weakened virus cells. The medicine is produced in the form of drops for use in the mouth. This polio vaccine protects the body from various types of the virus.
- Inactivated is developed from destroyed cells and is administered as an injection. Vaccines are safe for people and do not cause side effects. The vaccine is less effective than OPV, so polio may occur in certain groups of sick children.
For the purpose of immunization, combination drugs are normally used to protect the body from all kinds of infections. The following types of vaccines are used in our country:
- Tetranok.
- Infanrix hexa.
- Pentaxim.
IPV and OPV: what is the difference and what is better to vaccinate children
They commit IPV to children of all ages. Thanks to timely immunization, a person becomes protected from infection by pathogens that provoke the development of polio. This disease is very dangerous, especially for newborns and weakened individuals.
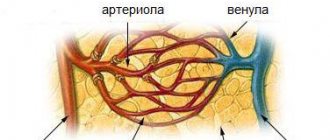
Poliomyelitis is a pathology associated with disorders of the central nervous system. As a rule, the virus is localized in the spinal cord. Children under five years of age are most susceptible to infection.
There are two forms of polio: non-paralytic and paralytic. The latter variant of the disease is accompanied by paralysis of the lower and upper extremities. In most cases, children do not fully recover and remain disabled for life. The virus can also infect the respiratory center. Then asphyxia occurs. The mortality rate from polio reaches 5-10%.
Until recently, pathology posed a serious threat to the inhabitants of the planet, causing epidemics and mass deaths. Today, thanks to vaccination, much fewer cases of virus infection are being recorded.
OPV is an oral multivalent vaccine. This drug contains a live but weakened virus. Today, in Russia, a polio vaccination scheme is used, which involves combining OPV and IPV (the first three doses are administered by killed people, and the subsequent ones by live vaccinations).
But you can choose to immunize only with inactivated drugs. Many parents are interested in what is better for the child, OPV or IPV.
To understand, it is necessary to compare the two types of vaccines. OPV is available in the form of oral drops, and IPV is available in the form of an injection solution. In terms of the child’s perception of immunoprophylaxis from a psychological point of view, live vaccinations are better (the child does not experience pain or fear, since the drug is dripped onto the tongue).
In terms of safety, IPV is preferable. Because OPVs contain live virus, they can cause vaccine-associated polio. The list of contraindications for inactivated vaccinations is smaller than for attenuated ones. For example, the latter should not be used in cases of immunodeficiency.
Vaccine Imovax Polio
The difference lies in the price. If you want to save money, you should choose OPV. Such vaccinations are usually given free of charge at local clinics. To immunize with IPV, you will have to pay for the drug and the services of medical staff.
Many parents prefer IPV and wonder whether OPV can be replaced with an inactivated vaccine. Doctors give a positive answer. But experts warn that OPV, unlike IPV, additionally protects against wild polio virus.
How is the vaccine activated?
Vaccination involves the use of weakened or dead virus cells. The human body can produce immune bodies that spread throughout the body through the circulatory system. When interacting with an infection, leukocytes begin to react and antibodies appear. For immunity to be sufficiently stable, you only need to get the virus into the body once.
The entry of weakened cells into the body provokes a reaction from the immune system, minimizing the likelihood of infection. Until recently, to obtain lifelong resistance to the disease, but today the strains have become diverse. Therefore, only OPV can provide good protection against infection. To ensure immunity remains for life, you need to administer the vaccine 6 times.
Poliomyelitis is...
This disease is considered quite rare today, but has not been completely eradicated, so it is better to play it safe. Poliomyelitis is caused by viruses and provokes the development of paralysis, which leads to disability for life.
This disease can cause respiratory and cardiovascular failure to develop, because paralysis of the muscles involved in respiratory movements occurs. This condition can ultimately lead to death.
To date, there is no medicine that can completely cope with the disease, so the only salvation is the polio vaccine.
This vaccine has been used in world medical practice since 1955, which has allowed many countries to completely get rid of this terrible disease. Currently, only a few countries remain sources of this infection.
Possible contraindications
It is not recommended to administer OPV to babies in the following cases:
- A malignant tumor has been discovered.
- Chronic disorders are getting worse.
- The presence of acute diseases.
- HIV infection.
- Neurological diseases.
- Malformations of organs.
- Pathologies in different systems.
If you want to vaccinate a person with a runny nose, you must first study the nature of this disorder. Practice states that this condition cannot be called a contraindication.
People should not be vaccinated in the following situations:
- Allergy to streptomycin, polymyxin B.
- Allergy to vaccines and injections given before.
- Neurological disorders.
Is it possible to get infected
Unvaccinated children pass the vaccine on to each other . For this reason, during collective vaccination using drops in the mouth, children are quarantined for several weeks.
There are known situations where younger children got the disease from vaccinated older children, or virus cells were found in pregnant women. To prevent anything like this from happening, you need to adhere to personal hygiene, use less shared bathrooms and bathrooms.
Possible side effects
When polio vaccinations are given, the following side effects are likely:
- Swelling at the injection site.
- The pain lasts about 2 days.
- Enlargement of lymph nodes.
- Hives, a rash appears on the skin and itches.
- Quincke's edema.
- Muscle tissues and joints begin to ache.
- Anaphylactic shock.
- Heat.
- Convulsions and fever.
- High level of excitability for 2 weeks after the injection.
The above reactions occur rarely and are caused by neglect of vaccination rules. Sometimes the medicine can be administered to a baby with a weak immune system or who has just recovered from an illness.
Consequences of anti-polio immunization
Normally, there are no complications after receiving the polio vaccine. But a reaction to immunization is possible.
Live (oral, drops) polio vaccine (OPV) may cause a slight increase in body temperature (up to 37.5ºC) for 14 days after vaccination.
After inactivated vaccination (IPV), which is given by injection, 5-7% of patients may experience swelling at the injection site (up to 8 cm in diameter), 1-4% of children experience a slightly elevated temperature in the first two days, and children may become restless .
Serious, although rare, complications such as seizures and encephalopathy are possible after vaccination. The latter concept means that the vaccine led to pathological damage to the brain caused by the death of nerve cells due to oxygen deficiency. Symptoms of encephalopathy are varied and are determined by its form and stage. Initially, lethargy and disturbances in sleep, hearing, and vision are observed; the muscles are in good shape. Afterwards, serious headaches, nausea, dizziness, disturbances of consciousness, even mental disorders, and paresis will come. Treatment of encephalopathy is long-term and complex.
Parents also note such reactions (complications) after vaccination as diarrhea and nausea, lethargy and drowsiness.
The probability of contracting polio as a result of vaccination is extremely low - 1: 2,500,000.
You should immediately consult a doctor if you experience the following during the post-injection period:
- lethargy;
- itching or hives;
- shortness of breath, difficulty breathing and swallowing;
- temperature rise above 39ºС;
- convulsions;
- swelling of the face.
Vaccination will protect your child from polio. Frequency of polio vaccination.
Poliomyelitis, or infantile spinal paralysis, is an acute infectious disease caused by an intestinal enterovirus and accompanied by damage to the gray matter of the medulla oblongata and spinal cord. The main route of transmission, as with all intestinal infections, is fecal-oral, but infection by airborne droplets is also possible.
It is often asymptomatic and is especially active in the autumn-summer months, although cases of infection are recorded throughout the year. There is no specific antiviral treatment for polio; the only way to prevent this terrible disease is vaccination.
Diagnosis of the disease
In various situations, not counting the paralytic form of the disease, the infection is determined in the laboratory. First, the components of stool are studied using PYR to identify pathogenic RNA. If the result is positive, a blood test is done to check for antibodies to poliovirus.
Acute infectious disorders are indicated by a high concentration of immunoglobulins M. They are produced in the first days of infection. A high concentration of immunoglobulin G indicates a previous disorder within 2-3 months.
Blood tests show different results during the development of an acute infection. The amount of hemoglobin decreases, leukocytes multiply faster and ESR is stimulated. When the meningeal form of the disorder develops, a puncture of the spinal canals is performed and cerebrospinal fluid is taken for examination. Poliomyelitis RNA is detected in the cerebrospinal fluid using PCR, and the concentration of protein and lymphocytes increases.
Treatment
Polio treatment is carried out by infectious disease specialists; in the paralytic form of the disease, they refer patients to neurologists. Patients are sent to a hospital for treatment and isolated from others for at least 40 days.
In the acute phase of the disease, bed rest is required. There are no special antiviral agents available to treat this disease. Immunoglobulin, various vitamins and medications that strengthen the nervous system provide a general strengthening effect.
Children after polio need mandatory rehabilitation so that the nerve structures of the spinal cord resume their activity. For this purpose, physiotherapy, exercise therapy, and massage procedures are carried out.
Recommendations and Cautions
Let's list the main ones:
- Before vaccination, you need to make sure that the baby is healthy and there are no contraindications. For this purpose, children should be examined by pediatricians.
- You need to take a toy or something else with you to the hospital to distract your child from the uncomfortable procedure.
- Before vaccination, there is no need to give children new foods for 3-4 days. It is not recommended to change your diet within a week after the injection.
- The vaccination schedule must be adhered to so that immunity does not deteriorate.
Unvaccinated babies can get the virus and become infected from vaccinated ones. The weakened virus is released approximately 30 days after vaccination. To prevent your child from picking up the infection, you need to maintain personal hygiene and remember that polio is transmitted by the fecal-oral route.