Everyone knows that the human brain is the main organ not only of the nervous system, but of the entire organism. It is the coordinator and regulator of all life processes; it is responsible for our instincts, perception of the outside world and behavior. The brain is a very complex and finely organized structure; the slightest changes can lead to irreversible changes. Therefore, any damage to this organ is extremely dangerous! One of the most unfavorable conditions is compression.
Causes
Considering the fact that compression of the brain is a serious pathology, you will need to know the reasons for its occurrence. In some cases, a person has the opportunity to prevent this condition. It is enough to know why it may appear so that you can influence this process.
The most common cause of compression is the formation of a hematoma in the head. There are only four types: intraventricular, subdural, epidural, intracerebral. A hematoma can be caused by either a head injury or a ruptured blood vessel.
The cause can also be a fracture of the skull, part of the bones that occurs during trauma. Damaged areas can put pressure on the brain and cause negative symptoms. There may also be a rupture of the subarachnoid cisterns, and there may also be an accumulation of air in the head due to an injury. Sometimes diseases such as adenoma or glioma can lead to pathology.
There are a number of other reasons that lead to compression of the human brain. This could be a hemorrhagic stroke, an abscess inside the head, hydrocephalus. Often, the disorder occurs due to cysts and brain tumors, which, as they grow, exert pressure on the brain tissue.
People are advised to treat various pathologies in a timely manner, as well as undergo diagnostics. Then it will be possible to prevent compression of the brain, or take timely measures to eliminate it.
Diagnosis of the disease: Brain compression
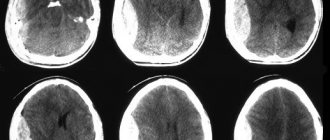
An epidural hematoma on a computed tomogram looks like a biconvex, less often plano-convex, zone of increased density adjacent to the calvarium. The hematoma is limited in nature and, as a rule, is localized within one or two lobes. With venous sources of bleeding, it can spread over a considerable distance and have a crescent shape.
A subdural hematoma on a computed tomogram is often characterized by the presence of a crescent-shaped zone of altered density, plano-convex, biconvex or irregular in shape. Often subdural hematomas spread to the entire hemisphere or most of it. Intracerebral hematomas have the appearance of round or elongated zones of homogeneous intense increase in density with clear boundaries. Hematomas are formed both as a result of direct damage to the vessel and as a result of angioonecrosis at the site of a crush injury to the brain. Intraventricular hematomas are detected by a zone of intense homogeneous increase in density, in its topic and shape corresponding to a particular ventricle of the brain.
Intracranial hemorrhages in victims with severe anemia may have a density similar to that of the brain. Blood clots are characterized by a higher density than liquid blood. They are more clearly differentiated from surrounding tissues. Intracranial hematomas containing fresh, uncoagulated blood may have the same density as the brain or even lower density on a computed tomogram, against the background of which, with an epidural hematoma, displacement of the dura mater may be detected.
With subsequent liquefaction of the contents of hematomas, degradation of fibrin in blood clots, and disintegration of its pigments, a gradual decrease in the density of the hematoma occurs, making it difficult to diagnose hemorrhages, especially in cases where the absorption coefficient of altered blood and the surrounding brain matter become the same. This is followed by a phase of reduced density, during which the absorption coefficient of the spilled blood approaches the density of the cerebrospinal fluid.
Symptoms
Symptoms of brain compression can be different, because much depends on the individual characteristics of the patient, as well as on the severity of the condition. Signs may appear immediately after the injury, or they may appear over time.
For example, there is a bright period after a TBI when the patient feels much better. It can last on average from half an hour to several hours, but after it unpleasant symptoms of brain compression occur.
Characteristic manifestations: consciousness is impaired, headaches appear, vomiting and nausea, slow pulse, temperature rises, epilepsy, it is impossible to move the eyeballs, blood pressure increases, and dizziness occurs.
Symptoms may depend on the cause of the compression, the location of the mass and its size, as well as the rate of growth. If a person develops a pathology after a head injury, then a “lucid gap” may occur.
At such a moment, the patient may not experience impaired consciousness, but the brain tissue is affected. If compression occurs with a subdural hematoma, then the “bright period” lasts from five to seven days, and then unpleasant symptoms only appear.
Intracerebral hematomas are rare and, as a rule, they do not reach large volumes. They can occur if there is a head injury. In this case, the symptoms will be acute, and they will appear immediately. Intraventricular hematomas in most cases do not manifest themselves . They can form against the background of intracerebral disorders as soon as a head injury occurs.
After the “light period” has passed, the patient most often begins to vomit, and the condition takes a turn for the worse. There may be symptoms such as delusions, hallucinations, disturbed sleep, and very severe pain in the brain.
After all this, lethargy, apathy, and lethargy begin. Consciousness is also impaired, and the patient may fall into a coma. Malfunctions occur in the cardiac and respiratory systems, as well as in blood vessels.
If negative manifestations occur that indicate compression of the brain, then you should immediately consult a doctor. You should not put off visiting the hospital until later, because this can lead to irreversible consequences.
A person may even become disabled, or the pathology will lead to death. If there is compression of the brain, it is necessary to promptly diagnose and begin therapy.
Diagnosis
The diagnosis is established on the basis of anamnesis, wedge, pictures, as well as results obtained using instrumental studies. During an ultrasound examination of the brain (see Echoencephalography), a shift of the median echo signal to the healthy side and the absence of pulsation of echo signals are noted. On the EEG you can often see a local decrease in bioelectrical activity, respectively patol. focus and its disorganization up to a flat curve with severe decompensation. The angiographic picture indicates both the localization and type of patol. process, and for the presence of vasospasm, signs of hydrocephalus and brain dislocation (displacement of the main trunks of the cerebral arteries). With chronic process, using skull radiography, one can identify signs of intracranial hypertension, pronounced finger-like impressions, and an expanded sella turcica. Computed tomography (see Computed tomography) in most cases provides accurate information about both the nature and localization of the patol. focus, and about the state of the ventricles of the brain and the phenomena of its dislocation.
Examination of cerebrospinal fluid does not provide accurate data on the presence of intracranial hematoma; the liquid can be either colorless or blood-stained; the cerebrospinal fluid pressure can be increased, less often normal or decreased. It should be noted the danger of a spinal puncture (see) for diagnosing S. g.m. caused by an intracranial hematoma, especially in the phase of occlusion of the cerebrospinal fluid tract, since a decrease in the cerebrospinal fluid pressure in the subarachnoid space of the spinal cord after the puncture can lead to the emergence or increase symptoms of brain herniation.
Diagnosis and treatment
To diagnose head compression, CT and MRI are used. The disease puts a person's life at risk. For this reason, it is important to conduct an immediate examination to confirm the presence of a disorder.
It is not always possible to immediately understand why compression of the brain occurred , as well as how severe it is. Therefore, you must first be examined by a doctor and provide information about the injury.
If the patient is unconscious, the doctor checks with loved ones how this happened. To confirm the disease it is necessary to undergo research.
MRI reveals the exact location of the injury and various brain disorders. The study shows the severity of the injury and the condition of the skull. This examination is considered informative and at the same time safe, so it is mandatory for patients.
The only negative is that to get accurate results you will have to spend from 30 minutes to 1.5 hours. If the patient is in an inadequate state, then the procedure will have to be abandoned or think about using anesthesia.
helps determine where the damage is located. Also finds displacement in the head and swelling. They are prescribed to undergo craniography, which is an x-ray without contrast agent.
There are other diagnostic methods that identify compression of the brain and its cause. A research method such as echoencephalography finds and determines displacement in the cranium.
In addition, a person may be prescribed a general blood test, as well as an examination by an ophthalmologist and some other doctors. Everything will depend on the patient’s condition, as well as on what symptoms he is complaining about.
The most important thing is not to trigger the pathology, because when the brain is compressed, the functioning of the organ is disrupted. The sooner the disease is identified and eliminated, the greater the chance of a successful outcome.
Instrumental diagnostic methods
Instrumental diagnostic methods should be limited to only the most urgent and necessary studies. For example, echoencephalography and lumbar puncture have proven their informativeness. The first can detect a mass effect with a displacement of the middle M-echo, the second will reveal that the cerebrospinal fluid pressure is increased and there is blood in the cerebrospinal fluid. But neuroimaging techniques are now available, so such studies are no longer necessary. MRI or CT scan of the brain is prescribed to the patient depending on the indications, and sometimes both of these studies are performed. Spiral CT of the brain is used in emergency situations, which reduces diagnostic time.
CT helps to assess the dislocation of cerebral structures and diagnose cerebral edema, its location, type and size. Perfusion CT reveals cerebral perfusion and blood flow, and secondary ischemia. Areas of cerebral ischemia, areas of contusion and dislocation of brain tissue are determined using MRI of the brain, which is more sensitive. Diffusion-weighted MRI is used to study the state of brain pathways and determine the degree of their compression.
First aid
If compression of the brain occurs, the person may need to provide first aid. Sometimes negative symptoms appear immediately, so it is important to do everything to ensure that the patient’s condition does not worsen.
As already mentioned, pathology often occurs due to traumatic brain injury. In this situation, it will be necessary to take action even before the ambulance arrives.
What to do:
- If the victim is unconscious or cannot get up, it is better not to touch him. The exception is the situation when he is in an unsafe place. Then he should be moved to a place where he will not be in danger.
- Now you will need to call an ambulance, briefly describing the situation.
- If there is compression of the brain, it will be necessary to carefully place the person on his back. When the patient is unconscious, his head should be turned slightly to the side. This is necessary so that he does not choke on his vomit.
- If possible, apply something cold to your head.
- If there is no breathing or heartbeat, resuscitation will be required. It is important to be able to properly perform cardiac massage, as well as artificial respiration. You may have to ask the people around you if they have similar skills.
- You need to monitor your breathing until the ambulance is on its way. When there is a wound, it will be useful to apply an aseptic dressing to it.
- In order to transfer an injured person, a rigid stretcher is usually used.
As soon as the ambulance arrives, doctors will be able to draw a conclusion about the patient’s condition. If there is compression of the brain, you need to go to the hospital, because it will be important to immediately get diagnosed and begin treatment.
Classification
Compression of the brain occurs due to a decrease in the size of the intracranial cavities due to their filling with space-occupying formations. This type of pathology is conventionally divided into two forms of compression:
- non-increasing;
- growing.
Non-growing include options when pressure is exerted on the brain by bone fragments formed as a result of a depressed fracture of the bone structures of the skull. This category also covers situations where brain compression is caused by pressure from other foreign objects. Non-increasing compression differs from the other option in that the unnatural structure in the brain itself does not tend to increase in volume - its size remains static. It must be remembered that all non-growing formations can take on a growing character due to the addition of other cerebral anomalies, causing significant compression of the brain and displacement of its structures. Such a secondary pathological mechanism is the characteristic formation of edema (excessive accumulation of fluid), which causes an increase in brain volume and an increase in pressure inside the skull.
Growing include all types of hematomas in the intracranial space (formations in the substance or around the brain). Pathological cavities of liquid or clotted blood are formed with open or closed head injuries. Hematomas are differentiated based on their location into types:
- epidural;
- subdural;
- intracerebral.
Subdural hematomas are diagnosed if the accumulation of blood is localized in a narrow area between the dura and arachnoid membranes of the brain. Acute subdural hematomas are a common consequence of head injuries caused by a fall from a height or an accident.
Chronic subdural hematomas are detected several weeks after the incident and become symptomatic gradually. These types of pathological formations more often occur in people who abuse alcohol, elderly patients, patients taking antiplatelet agents or anticoagulant drugs. It should be noted that many people who have been diagnosed with chronic subdural hematoma do not associate the symptoms they experience with any recent trauma.
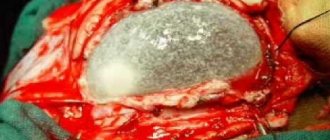
Epidural hematomas are an accumulation of blood in a cylindrical closed space between bone structures and the dura mater of the brain. They are diagnosed much less frequently than formations in the subdural region. Massive and rapidly increasing in size epidural hematomas are a consequence of arterial bleeding that occurs if the branches of the middle meningeal artery are damaged. Small venous epidural hematomas do not pose a threat of premature death.
Intracerebral hematomas are collections of blood inside the brain itself. In traumatic conditions, they arise as a result of the fusion of contusions that occur with a sudden indirect impact on the body. In most cases, it is not possible to accurately determine when one or more contusion lesions become a hematoma. Subsequently, the victim often experiences a significant increase in intracranial pressure.
Therapy
As already mentioned, patients undergo treatment in the hospital, since compression of the brain is a dangerous disease. Doctors can eliminate the causes with medications; in rare cases, surgery is required. During the operation, formations, hematomas and bone fragments in the head are removed .
As soon as the patient feels better, hemostatic and dehydration treatment is prescribed. The patient also uses antibacterial agents if there are purulent lesions. It is extremely important to monitor the functioning of the heart, and also to prevent cerebral edema.
It is often necessary to take nootropics and neuroprotectors in order to restore damaged brain tissue and restore their functions. In addition, the person is prescribed sedatives, as well as medications against seizures. Everything will depend on the condition of the patient.
When therapy is carried out, the doctor carefully monitors the patient's intracranial pressure and breathing. If drug treatment does not help, then surgery is performed. It is used if there are severe symptoms or the epidural hematoma exceeds one and a half centimeters.
If it happens that an acute hematoma appears, then excess blood is removed and bleeding in the brain is stopped.
Only a neurosurgeon will be able to say for sure whether surgery will be required . If it is possible to do without it, then it is not carried out, because it can pose a threat to life. In any case, if there is compression of the brain, you cannot do without professional help.
Forecasts
When the brain is compressed, it is difficult to say unequivocally what consequences await a person. Everything will depend on how serious the injury is, because the worse the condition, the higher the likelihood of death.
When using modern treatment methods, there is a greater chance of saving the patient. But at the same time, the surviving people in most cases become disabled.
Even after proper therapy, a number of complications may occur. Epilepsy, serious speech disorders, and problems with motor function are possible. The psyche is often disturbed, a person receives various disorders that affect the quality of life. For this reason, you may need to talk to a therapist later.
It should be understood that compression of the brain is dangerous to human life and health. If you do not implement therapeutic measures, then there will be practically no chance of a successful outcome. At best, a person will receive a severe degree of disability, and at worst, death will occur. The sooner you see a doctor, the better it will be for the patient. It is recommended that after any head injury you get checked out at a hospital because symptoms may not appear immediately. Preventing complications is the best way to keep your health in good condition.
Breath
There are also characteristic signs of compression of the brain. The breathing rhythm is upset. Tachypnea (increased frequency) reaches sixty breaths per minute, inhalation and exhalation are accompanied by noise, Cheyne-Stokes breathing occurs. Heart rate decreases, bradycardia is fixed at a level of forty beats per minute and below, blood flow speed drops, which leads to arterial hypertension. All this is accompanied by congestive pneumonia and pulmonary edema. The patient hears moist rales. The skin of the limbs and face becomes cyanotic. Body temperature rises to 41 degrees. Meningeal symptoms are present. The terminal stage is characterized by tachycardia and arterial hypotension. The pulse is threadlike, there are episodes of apnea (breathing occurs with delays), the duration of which increases. Contusion and compression of the brain are also manifested by other signs.