Electroencephalogram of the brain - definition and essence of the method
is a recording of the electrical activity of neurons in various brain structures, which is made on special paper using electrodes.
Electrodes are placed on different parts of the head and record the activity of a particular part of the brain. We can say that an electroencephalogram is a recording of the functional activity of the brain of a person of any age. The functional activity of the human brain depends on the activity of the median structures - the reticular formation and the forebrain, which determine the rhythm, general structure and dynamics of the electroencephalogram. A large number of connections of the reticular formation and forebrain with other structures and the cortex determine the symmetry of the EEG, and its relative “sameness” for the entire brain.
An EEG is taken to determine the activity of the brain in case of various lesions of the central nervous system, for example, with neuroinfections (poliomyelitis, etc.), meningitis, encephalitis, etc. Based on the results of the EEG, it is possible to assess the degree of brain damage due to various causes and clarify specific location that has been damaged.
The EEG is taken according to a standard protocol, which takes into account recordings in a state of wakefulness or sleep (infants), with special tests. Routine tests for EEG are:1. Photostimulation (exposure to flashes of bright light on closed eyes).2. Opening and closing the eyes.3. Hyperventilation (rare and deep breathing for 3 to 5 minutes).
These tests are performed on all adults and children when taking an EEG, regardless of age and pathology. In addition, additional tests may be used when taking an EEG, for example:
- clenching your fingers into a fist;
- sleep deprivation test;
- stay in the dark for 40 minutes;
- monitoring the entire period of night sleep;
- taking medications;
- performing psychological tests.
Additional tests for EEG are determined by the doctor–
who wishes to evaluate certain functions of the human brain.
Symptoms
Disturbances in the functioning of the brain at first do not appear as clearly as other diseases associated with internal organs. In patients with severe and moderate diffuse changes, the following is noted:
- Decreased performance.
- Psychological problems, neurosis, psychosis, depression.
- Inattention, deterioration of memory, speech and mental abilities.
- Hormonal disorders.
- Slowness, lethargy.
- Susceptibility to colds.
- Nausea, frequent headaches.
The listed signs often go unnoticed, as they can easily be attributed to overwork or stress. In the future, the symptoms become more pronounced and more severe.
What does an electroencephalogram show?
An electroencephalogram reflects the functional state of brain structures in various human states, for example, sleep, wakefulness, active mental or physical work, etc. An electroencephalogram is an absolutely safe method, simple, painless and does not require serious intervention.
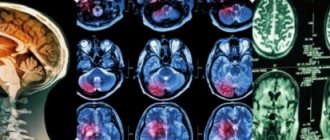
Today, the electroencephalogram is widely used in the practice of neurologists, since this method makes it possible to diagnose epilepsy, vascular, inflammatory and degenerative lesions of the brain. In addition, EEG helps to determine the specific location of tumors, cysts and traumatic damage to brain structures.
An electroencephalogram with irritation of the patient by light or sound makes it possible to distinguish true visual and hearing impairments from hysterical ones, or their simulation. EEG is used in intensive care units for dynamic monitoring of the condition of patients in a coma. The disappearance of signs of electrical activity of the brain on the EEG is a sign of human death.
Symptoms and diagnosis of diffuse changes
Mild or severe BEA imbalance is detected by several methods. To make an accurate diagnosis, a specialist analyzes the results of the following studies:
- Examination of the patient, information about injuries, chronic diseases, genetic predisposition, symptomatic manifestations.
- Electroencephalogram (EEG), which allows you to see the cause of the deviations. To do this, a cap with electrode sensors is placed on the patient’s head. They record impulses and display them on paper in the form of waves.
- MRI of the brain is prescribed in the presence of bioelectrical activity. If it is fixed, then there is a reason for the deviation, which can be seen on tomography (tumor, cyst).
- Angiography. Prescribed to a patient with vascular atherosclerosis.
This type of research is based on recording the electrical activity of neurons in various parts of the brain. The research procedure consists of recording the patient's condition during sleep or wakefulness using various loads:
- Light ones.
- Shumovykh.
- Respiratory.
With lesions of the cerebral cortex, neurological abnormalities are observed, since this area is responsible for nervous activity. Sometimes one or several zones are damaged.
- If changes occur in the occipital part, then the patient experiences hallucinations.
- Damage to the anterior central gyrus provokes twitching of the limbs.
- With changes in the posterior central gyrus, patients experience numbness and tingling in parts of the body.
If the EEG cannot determine where the seizures occur, then changes in the BEA of the cerebral cortex will still be recorded. Pathology will manifest itself in the following indicators:
- Heterogeneous patency of neurons.
- Irregularly asymmetrical waves.
- Polymorphic activity.
- Pathological biowaves exceeding the norm.
To make a diagnosis, it is necessary to identify deviations in all monitoring indicators. But even if diffuse changes are recorded, this does not mean that the patient is sick. An imbalance of BEA may indicate depression, stress, or drinking large amounts of coffee or alcohol on the eve of the examination.
It is believed that the bioelectrical activity of the brain is disorganized if external signs appear, reflected in the behavior and reaction of the patient, and also if these changes are confirmed or preceded by hardware diagnostics. Often, the bioelectrical activity of the brain is first tested using a hardware method, after which suspicions arise, and only then do patients pay attention to behavioral and cognitive symptoms:
- sudden changes in mood from good to bad - and vice versa,
- decreased self-esteem,
- loss of interest in previous hobbies,
- slower performance of usual work,
- rapid onset of fatigue when performing even basic actions.
In general, the history of cerebral changes in BEA is also typical for other diseases of the central nervous system. A person describes his condition as a general malaise and may not correlate the symptoms with the first signs of diffuse changes in BEA (especially if the symptoms listed above are accompanied by dizziness and headaches, “jumping” blood pressure).
If diffuse changes are significant, and if a significant decrease in the threshold of convulsive readiness is recorded, then it is considered that the person is predisposed to epilepsy.
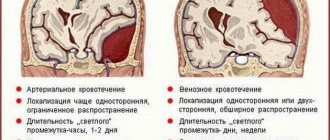
Common causes of changes - atherosclerosis, encephalitis, meningitis, toxic brain damage - are usually reflected in tissue necrosis, inflammation, edema, and scarring. And these pathologies, in turn, are recorded using EEG. In case of a general cerebral lesion, three types of pathological processes are recorded on the EEG, the most significant of which is considered the first, but the diagnosis is made in the presence of all three signs of the pathological process, namely:
- polymorphic polyrhythmic (multiplicity of rhythms) activity in the absence of regular dominant bioelectrical activity,
- disruption of the normal organization of the electroencephalogram, which is expressed in irregular asymmetry with simultaneous disturbances in the distribution of basic EEG rhythms, phase coincidence of waves in symmetrical parts of the brain, amplitude relationships,
- diffuse pathological oscillations (alpha, delta, theta, exceeding normal amplitudes).
Often the EEG is dominated by signs of a symptom complex that appears with lesions of the hypothalamus and pituitary gland (diencephalic syndrome). Decoding the EEG readings does not allow us to see the reason for the appearance of abnormal data. A slight malfunction in the BEA when diagnosed using EEG can also be recorded in a healthy person.
Examples of EEG conclusions:
- “Significant diffuse changes in the BEA of the brain associated with dysfunction of the midline structures. Reducing the threshold of convulsive readiness. The focus of pathological activity, including paroxysmal activity, is in the right frontotemporal region.”
This means that there is a predisposition to epilepsy and seizures. There are lesions in the cerebral cortex that exhibit increased BEA, which can lead to various types of epileptic seizures.
- “The BEA of the brain is somewhat disorganized. During hyperventilation, flashes of pointed theta and alpha waves, deformed single complexes in the frontal leads of the “sharp-slow wave” type are recorded. No pronounced interhemispheric asymmetry was recorded.”
This result, together with the results of the REG, which indicate a continued decrease in pulse blood filling during functional tests, reveals signs of circulatory disorders in the brain.
- “Alpha rhythm over both hemispheres. Amplitude – up to 101 µV on the right and up to 99 µV on the left. Maximum – 57 µV on the right and 54 µV on the left. The dominant frequency is 9.6 Hz with dominance of the alpha rhythm in the occipital leads. Slow theta waves over both hemispheres. In the anterior frontal region – 53 µV, in the frontal – 56 µV, in the parietal – 88 µV, in the central – 81 µV, in the posterior temporal – 55 µV. Signs of a moderate stage of irritation of the midline structures of the brain and cortex. No paroxysmal activity or stable interhemispheric asymmetry was recorded.”
To clarify and identify catalysts for deviation, magnetic resonance imaging (MRI) is used.
When bioelectrical activity is disorganized, the causes of deviations exist, even if they are not immediately obvious. MRI helps identify them. Vascular atherosclerosis is detected by angiography. Tomography demonstrates irritative changes caused by a tumor and helps to establish the nature of the neoplasm.
Diagnostics
Diffuse changes in the bioelectrical activity of the brain are determined in several ways. For better diagnosis, a specialist analyzes the results of such examinations:
- A visual examination of the patient is carried out, chronic diseases, genetic predispositions, and other symptoms are identified.
- The EEG procedure makes it possible to determine the cause of deviations. For this purpose, a set of electrode sensors is placed on the patient’s head.
- MRI is performed to detect bielectric activity. When it is fixed, there is a reason for the deviation, which is displayed on the tomography.
- Angiography is performed if the patient has atherosclerosis.
Where and how to do it?
An electroencephalogram for an adult can be taken in neurological clinics, in departments of city and regional hospitals, or at a psychiatric clinic. As a rule, electroencephalograms are not taken in clinics, but there are exceptions to the rule. It is better to go to a psychiatric hospital or neurology department, where specialists with the necessary qualifications work.
Electroencephalograms for children under 14 years of age are taken only in specialized children's hospitals where pediatricians work. That is, you need to go to the children's hospital, find the neurology department and ask when the EEG is taken. Psychiatric clinics, as a rule, do not take EEGs for young children.
In addition, private medical centers specializing in the diagnosis and treatment of neurological pathologies also provide EEG services for both children and adults. You can contact a multidisciplinary private clinic, where there are neurologists who will take an EEG and decipher the recording.
An electroencephalogram should be taken only after a full night's rest, in the absence of stressful situations and psychomotor agitation. Two days before the EEG is taken, it is necessary to exclude alcoholic beverages, sleeping pills, sedatives and anticonvulsants, tranquilizers and caffeine.
Bringing BEA to normal
https://www.youtube.com/watch?v=nfLe2u2t4WM
If diffuse changes in the brain are detected in a timely manner and proper treatment is prescribed, then indicators of general cerebral activity can be returned to normal. Often patients do not pay attention to the symptoms of the disorder and seek medical help late, when the disease is already in an advanced stage.
Treatment for changes in BEA consists of drug therapy or surgery (depending on the disease). For vascular diseases, it is recommended to adhere to proper nutrition, fight excess weight, and strengthen blood vessels with homeopathic medicines.
- Statins lower cholesterol levels. They are prescribed only by an experienced specialist, as they have a negative effect on the liver
- Fibrates help reduce lipid synthesis, preventing the further development of atherosclerosis. These drugs have a negative effect on the gallbladder and liver.
- Nicotinic acid lowers cholesterol levels and improves antiatherogenic properties.
Treatment methods
A correct conclusion about the patient’s condition allows you to make prescriptions, avoid pathology and consequences, and resume stable cellular functioning. Diffuse polymorphic disorganization is subject to treatment in certain institutions; this cannot be delayed - complications are possible.
The level of damage affects the process of renewing natural connections. With a lower value, treatment shows better results.
The recovery plan is formed taking into account the factors of the fall of the BEA. Brain activity returns to normal easily at the beginning of the development of atherosclerosis.
Cases involving irradiation and intoxication are considered dangerous.
Doctors prescribe complex treatment with drugs to remove the main cause, neurological, psychopathological syndromes, stabilize processes and cerebral circulation.
Restoration of stable blood circulation is achieved using different groups of medications:
- calcium ion antagonists;
- nootropics;
- pentoxifylline - normalizes blood microcirculation;
- metabolic, vasoactive substances;
- sedatives and others.
Treatment of BEA disorders includes methods: magneto-, electro-, balneotherapy.
Electroencephalogram for children: how the procedure is performed
Taking an electroencephalogram in children often raises questions from parents who want to know what awaits the baby and how the procedure goes. The child is left in a dark, sound- and light-proof room, where he is placed on a couch. Children under 1 year of age are kept in their mother's arms during EEG recording. The whole procedure takes about 20 minutes.
To record an EEG, a cap is placed on the baby's head, under which the doctor places electrodes. The skin under the electrodes is wetted with water or gel. Two inactive electrodes are placed on the ears. Then, using alligator clips, the electrodes are connected to the wires connected to the device - the encephalograph. Since electrical currents are very small, an amplifier is always needed, otherwise brain activity will simply not be recorded. It is the small current strength that is the key to the absolute safety and harmlessness of EEG, even for infants.
To begin the examination, the child's head should be placed flat. Anterior tilt should not be allowed as this may cause artifacts that will be misinterpreted. EEGs are taken for infants during sleep, which occurs after feeding. Wash your child's hair before taking the EEG.
Do not feed the baby before leaving the house; this is done immediately before the test so that the baby eats and falls asleep - after all, it is at this time that the EEG is taken. To do this, prepare formula or express breast milk into a bottle that you use in the hospital. Up to 3 years of age, EEG is taken only in a state of sleep.
Typically, the EEG is recorded as a background curve, and tests with opening and closing the eyes, hyperventilation (slow and deep breathing), and photostimulation are also performed. These tests are part of the EEG protocol, and are performed on absolutely everyone - both adults and children. Sometimes they ask you to clench your fingers into a fist, listen to various sounds, etc.
Opening the eyes allows us to assess the activity of inhibition processes, and closing them allows us to assess the activity of excitation. Hyperventilation can be carried out in children after 3 years of age in the form of a game - for example, asking the child to inflate a balloon. Such rare and deep inhalations and exhalations last for 2–3 minutes. This test allows you to diagnose latent epilepsy, inflammation of the structures and membranes of the brain, tumors, dysfunction, fatigue and stress.
Today, the cost of taking an electroencephalogram in state medical institutions ranges from 400 to 1,500 rubles. In private medical clinics, the cost of an electroencephalogram may be higher, which is determined by the pricing policy of the institution, the qualifications of the specialist and other factors.
Alcoholism is a complex disease.
Why do doctors generally prohibit drinking alcohol? Alcohol is the most harmful, most popular, unique, legalized narcotic poison on the globe, when used, step by step, many essential functions of the cerebral cortex and higher parts of the central nervous system turn into ruins. Large doses of strong alcohol significantly disrupt the activity of the brain, which significantly inhibits the coordination of movement, has an adverse effect on vision, speech...
Discussion
Alcoholism is not only a disease, but also an addiction. I noticed that people addicted to alcoholism can come to their death sooner or later, or return to a sober life. It is important to fight alcoholism, since there is a large drinking population in the Russian Federation. Honey will help those who want to get rid of addiction. specialists. These are the best narcologists and therapists, with extensive experience in treating various diseases. It has become easier to make an appointment in a private or public clinic in your region if you use this doctu.ru doctor review service.
25.11.2015 14:34:52, Neurology in children
The fact is that in order to work, it absolutely needs an uninterrupted supply of oxygen. This is why when breathing stops, the brain dies first. Already after 5-6 minutes of clinical death, irreversible changes occur in it; the personality ceases to exist. Few people know that the brain is the first to age. Age-related changes in metabolic processes in its tissues begin at approximately 25-30 years of age. It is not for nothing that after thirty, many people, fortunately, not all lose their former learning ability and creativity. Almost everyone experiences other symptoms of brain aging. Who among quite young people is not familiar with a temporary weakening of memory, attention, and concentration; irritability and drowsiness caused, for example, by stress in the family or rush hour at work...
What kind of examinations are these? An absolutely safe and reliable method is neurosonography (ultrasound examination of the brain through the large fontanel). This study will help not only to see changes in the structure of the brain and signs of increased intracranial pressure, but also to evaluate blood flow through the main vessels of the brain. An even more reliable method is nuclear magnetic resonance of the brain (NMR), however, this study for children is carried out under general anesthesia, so it is carried out only for sufficiently compelling indications. In this case, consultations with an ophthalmologist and a neurosurgeon are also necessary. “Homework” for parents K...
During the course of the disease, the following periods are distinguished: acute (from birth to 1 month); early recovery (from 1st to 4th month); late recovery (from 4 months to 1 year); residual consequences or outcome (after 1 year). It should be noted that the earlier treatment is started, the smaller the changes that occur in the brain, the more favorable the outcome and the less severe the consequences. If treatment begins only in the residual period, then the effect of treatment is minimal. Now let's talk a little about the reasons that can lead to the development of perinatal encephalopathy. About the reasons for the development of PEP There is no doubt that giving birth to a healthy child... ...Childbirth is the most physiological process and, at the same time, the biggest risk factor in the development of PEP. Any deviations in childbirth can cause brain damage (premature and late, rapid labor, and, conversely, weakness of labor; the birth of two or more children; “caesarean section” - here the brain suffers during the period of anesthesia; entanglement of the child with the umbilical cord around the neck ). Therefore, how a woman prepares for childbirth mentally and physically will determine her health and fate... ...And now let’s take a closer look at the clinical manifestations of various syndromes. Clinical manifestations of the syndromes Syndrome of increased neuro-reflex excitability is more common with mild brain damage (as a rule, at birth such children have 6-7 Apgar scores) and is manifested by restless, superficial sleep; prolongation of periods of wakefulness, uncharacteristic for newborns; difficulty falling asleep; frequent “unreasonable” crying; tremor (twitching) of the chin and limbs; increased reflexes; shuddering; higher...
Discussion
With my first child I had PEP and a bunch of other diagnoses, I had a difficult labor with stimulation for 3 days…. We were treated from 4 months, very intensively, everything was corrected... At 2 and 3 years old we had febrile convulsions, at 3.5 we were diagnosed with ICP, then ADHD, behavioral problems (((we visited an osteologist, we are being treated by a neurologist, psychiatrist, psychologist... We also gained weight planovalgus .. The daughter was born well, but received 7/8 .. She slept constantly, from 2 weeks there were profuse cramps, leg tremors, her eyes bulged, but she was calm, at 2 months according to the NSG there was a small accumulation of fluid and increased blood flow, they put PEP and medications , the massage did not help, there was a slight tone and her body was pulled to the right in an arc, at 5 months according to the NSG they diagnosed foci of hemorrhages and intracranial hypertension... then we went to an osteopath.. After her, after 3 weeks the tone began to go away and the daughter began to straighten up (she had dislocation of the first cervical vertebra and some other bone above the palate, which caused problems with sucking, and I didn’t take the pacifier).There was no fluid at the NSG at 7 and 8 months! The hemorrhage lesions decreased by millimeter, one resolved. My advice. If you see that your child has any signs, even the slightest, go to an osteopath! A common problem (but not always) is injury to the neck during childbirth and a consequence of impaired blood flow... and further down the chain! Don’t spare money for your child and look for a good specialist in the registry of osteopaths! Now our daughter and I haven’t been diagnosed yet, but the neurologist told us to forget it! The child is developing perfectly! The osteopath also told me to leave my daughter alone, everything is fine with her now)) I regret that my son and I didn’t get into the hands of an osteopath until a year ago... he also had problems with his neck, but the manual was right ((with pain, fears... just like now I know... he just shouldn’t have been under such stress, he had to be gently influenced.
10/14/2016 23:33:18, Tatyana
the child is 6 months old, the pregnancy is full-term, the birth is uncomplicated, there are no problems from the point of view of pediatrics and neurology, but for several days now the tip of the tongue has begun to stick out. With what it can be connected?
05/08/2008 22:11:18, Ekaterina
...). There are many classifications of hydrocephalus, but these are the main ones and are used most often. Manifestations of hydrocephalus Impaired circulation and absorption of cerebrospinal fluid leads to its excessive accumulation and increased intracranial pressure. This manifests itself differently in children under 2 years of age and in older children. The main symptom of the development of hydrocele in children under 2 years of age is accelerated growth of head circumference. The sutures of the skull in babies have not yet healed, and the size of the head increases because the bones of the skull are pushed apart from the inside by the growing brain. In the same way, a balloon increases in volume when we inflate it. There is a graph for head circumference growth. It needs to be measured every one to two months, this is done by the local pediatrician during preventive...
Concussion in a child. Symptoms of a concussion, methods of diagnosing and treating a concussion
Discussion
my son was 5 years old when he received a concussion. He fell from a height of about 1.5 meters in the children's town. He hit the back of his head. I immediately took a taxi to the hospital... They did an X-ray there, ruled out a hematoma, gave me furasemide with asparkam and They suggested we go home! I insisted that they leave us in the hospital overnight under the supervision of doctors, after all... Now, after reading the article, I was horrified!!! How serious is all this... Even at that moment I clearly understood what a CONCUSSION was... but DOCTORS convinced me otherwise... Now my child is 8 years old. I think it’s worth raising this issue and examining it? Please tell me. Thanks for the article.
My daughter is 1 year 2 months old, she was admitted to the hospital with a diagnosis of a concussion, after a sleepless night and the disgusting attitude of the medical staff, I had to write a statement and leave there, besides, the children's department is very noisy, everything is new and naturally the baby could not sleep for a long time , was hysterical. At three in the morning she was woken up by very noisy nurses and until the moment of our evacuation, the child could no longer sleep (I’m talking about the peace that the hospital provides) At this age, the child is still better off at home, in a familiar environment, considering that everyone is at home life according to the regime. Strengthened control and diagnosis, that’s what I personally am for, and special thanks to such “caring” medical workers as in the Petrozavodsk Children’s Hospital...
12/20/2008 17:14:41, Svetlana
Electroencephalogram rhythms
The electroencephalogram must show a regular rhythm of a certain type. The regularity of rhythms is ensured by the work of the part of the brain - the thalamus, which generates them and ensures the synchronization of the activity and functional activity of all structures of the central nervous system.
The human EEG contains alpha, beta, delta and theta rhythms, which have different characteristics and reflect certain types of brain activity.
The alpha rhythm has a frequency of 8 – 14 Hz, reflects a state of rest and is recorded in a person who is awake, but with his eyes closed. This rhythm is normally regular, the maximum intensity is recorded in the area of the back of the head and the crown. The alpha rhythm ceases to be detected when any motor stimuli appear.
The beta rhythm has a frequency of 13 – 30 Hz, but reflects states of anxiety, restlessness, depression and the use of sedative medications. The beta rhythm is recorded with maximum intensity over the frontal lobes of the brain.
The theta rhythm has a frequency of 4–7 Hz and an amplitude of 25–35 μV, reflecting the state of natural sleep. This rhythm is a normal component of the adult EEG. And in children this type of rhythm on the EEG predominates.
The delta rhythm has a frequency of 0.5 - 3 Hz, it reflects the state of natural sleep. It can also be recorded in a limited amount during wakefulness, a maximum of 15% of all EEG rhythms. The amplitude of the delta rhythm is normally low - up to 40 μV. If there is an excess of amplitude above 40 μV, and this rhythm is recorded for more than 15% of the time, then it is classified as pathological.
Such a pathological delta rhythm indicates a dysfunction of the brain, and it appears precisely over the area where pathological changes develop. The appearance of a delta rhythm in all parts of the brain indicates the development of damage to the structures of the central nervous system, which is caused by liver dysfunction, and is proportional to the severity of the disturbance of consciousness.
How does it manifest itself?
A typical feature of diffuse axonal brain injury is that the patient remains unconscious from the moment of injury. This is accompanied by a variety of symptoms of severe brain damage. These include:
- generalized postural-tonic reactions;
- decreased pupillary response to light;
- weakened or absent corneal reflexes;
- oculomotor disorders;
- positive meningeal symptoms;
- tetraparesis of the limbs;
- hyperreflexia;
- pathological change in muscle tone from diffuse hypotension to attacks of reflex tonic muscle contraction;
- periodically occurring motor agitation (sometimes anesthesia is required to relieve it);
- dysfunction of the autonomic nervous system (hyperhidrosis, increased body temperature, drooling);
- disorders of cardiovascular activity and breathing.
The duration and depth of coma can be different, which significantly affects the prognosis:
- If the patient is in a coma for less than 7 days, then there is a possibility of a good recovery in the future.
- When the coma lasts more than 7 days, the probability of severe disability increases sharply in the structure of outcomes.
After the acute period has passed, exit from a coma occurs in two main ways:
- A more favorable outcome leads to spontaneous opening of the eyes with the ability to track and fixate the gaze. At first the patient sleeps more, but over time the periods of wakefulness increase. Gradually consciousness is restored and regression of pathological symptoms is observed.
- Another option for exiting a coma has a more severe course. In this case, a transition to a vegetative state occurs, which can be short-term or persistent, lasting from a day to several months. Such patients suddenly open their eyes, but they have no voluntary movements of the eyeballs, fixation of gaze and following simple instructions are impossible. Breathing and blood circulation are stable. When the cerebral cortex is depressed, brainstem, subcortical and spinal automatisms are disinhibited. In response to any external stimuli, a person develops uncoordinated defensive motor reactions.
If patients emerge from a vegetative state after such an injury, they develop new neurological symptoms (discoordination of movements, hyperkinesis, ataxia, etc.) and mental disorders (dementia, adynamia, aggression).
Preventive measures
As a preventative measure, experts recommend:
- Do not overuse caffeine-containing drinks.
- Give up bad habits.
- Avoid overheating and hypothermia.
- Exercise.
- Be careful from blows and bruises, as the consequences of head injuries take quite a long time to heal and are not always successful.
Negative changes in BEA also indicate the presence of neoplasms, therefore, in case of alarming symptoms, consultation with a neurologist is necessary. Diffuse changes in the brain cannot be treated independently. An incorrectly selected drug or an incorrectly chosen dosage can lead to disability or death.
Causes and morphology of DAP
The most common causes of TBI in DAP:
- severe bruise on windshields in an accident;
- a fall;
- hit with a heavy object;
- concussion syndrome in children, in which the brain is severely bruised after a sharp shaking, as well as a beating or fall.
DAP syndrome is the result of contusions caused by angular acceleration of the head. In this case, there may not be a direct collision with the object of injury.
As a result, some patients do not have skull fractures or other visible wounds, which makes diagnosis somewhat difficult. Statistics show that it is oblique damage that leads to axonal damage and the occurrence of DAP.
Morphologically, this injury is characterized by the following three foci of damage:
- brain;
- corpus callosum;
- brainstem and diffusely distributed ruptures.
The first two focal signs are macroscopic, which are located in the form of a hematoma up to five mm, looking like torn tissue with bloody edges. A few days after TBI, the lesion becomes pigmented and then scars. A wound in the corpus callosum may resolve with the formation of a vascular cyst.
Axonal disorders in trauma
Electroencephalogram results
The result of the electroencephalogram is a recording on paper or in computer memory. The curves are recorded on paper and analyzed by the doctor. The rhythm of EEG waves, frequency and amplitude are assessed, characteristic elements are identified, and their distribution in space and time is recorded. Then all the data is summarized and reflected in the conclusion and description of the EEG, which is pasted into the medical record. The EEG conclusion is based on the type of curves, taking into account clinical
available to humans.
Such a conclusion must reflect the main characteristics of the EEG, and includes three mandatory parts: 1. Description of the activity and typical affiliation of EEG waves (for example: “The alpha rhythm is recorded over both hemispheres. The average amplitude is 57 µV on the left and 59 µV on the right. The dominant frequency is 8.7 Hz.
The alpha rhythm dominates in the occipital leads”).2. Conclusion according to the description of the EEG and its interpretation (for example: “Signs of irritation of the cortex and midline structures of the brain. Asymmetry between the hemispheres of the brain and paroxysmal activity were not detected”).3. Determining the correspondence of clinical symptoms with EEG results (for example: “Objective changes in the functional activity of the brain were recorded, corresponding to manifestations of epilepsy”).
Bioelectric activity of the brain: basic rhythms
Bioelectrical activity is literally the electrical vibrations of the brain. The neurons that create a huge network in it have their own electrical wave. These waves are recorded by EEG, and the data obtained through the study can tell a lot about the state of health and psyche of an individual.
Biowaves (or rhythms of brain activity) are divided depending on amplitude and frequency:
- beta waves - 14-40 Hertz, amplitude - up to 20 µV;
- alpha - 8-13 Hz, wave amplitude - 5-100 µV;
- gamma - above 30 Hz, occasionally up to 100 Hz, amplitude - up to 15 μV;
- delta - 1-4 Hz, amplitude - 20-200 µV.
Decoding the electroencephalogram
Decoding an electroencephalogram is the process of interpreting it taking into account the clinical symptoms present in the patient. In the process of decoding, it is necessary to take into account the basal rhythm, the level of symmetry in the electrical activity of brain neurons of the left and right hemispheres, the activity of the commissure, EEG changes against the background of functional tests (opening - closing the eyes, hyperventilation, photostimulation). The final diagnosis is made only taking into account the presence of certain clinical signs that concern the patient.
Decoding the electroencephalogram involves interpreting the conclusion. Let's consider the basic concepts that the doctor reflects in the conclusion and their clinical significance (that is, what these or those parameters can indicate).
Alpha - rhythm
Normally, its frequency is 8–13 Hz, the amplitude ranges up to 100 μV. It is this rhythm that should prevail over both hemispheres in healthy adults. Alpha rhythm pathologies are the following:
- constant registration of the alpha rhythm in the frontal parts of the brain;
- interhemispheric asymmetry above 30%;
- violation of sinusoidal waves;
- paroxysmal or arc-shaped rhythm;
- unstable frequency;
- amplitude less than 20 μV or more than 90 μV;
- rhythm index less than 50%.
Pronounced interhemispheric asymmetry may indicate the presence of a brain tumor, cyst,
or a scar at the site of an old hemorrhage.
High frequency and instability of the alpha rhythm indicate traumatic brain damage, for example, after a concussion or traumatic brain injury.
Disorganization of the alpha rhythm or its complete absence indicates acquired dementia.
About delayed psycho-motor development in children they say:
- alpha rhythm disorganization;
- increased synchrony and amplitude;
- moving the focus of activity from the back of the head and crown;
- weak short activation reaction;
- excessive response to hyperventilation.
A decrease in the amplitude of the alpha rhythm, a shift in the focus of activity from the back of the head and crown, and a weak activation reaction indicate the presence of psychopathology.
Excitable psychopathy is manifested by a slowdown in the frequency of the alpha rhythm against the background of normal synchrony.
Inhibitory psychopathy is manifested by EEG desynchronization, low frequency and alpha rhythm index.
Increased synchronization of the alpha rhythm in all parts of the brain, a short activation reaction is the first type of neuroses.
Weak expression of the alpha rhythm, weak activation reactions, paroxysmal activity - the third type of neuroses.
Beta rhythm
Normally, it is most pronounced in the frontal lobes of the brain and has a symmetrical amplitude (3–5 μV) in both hemispheres. Pathology of the beta rhythm is the following signs:
- paroxysmal discharges;
- low frequency, distributed over the convexital surface of the brain;
- asymmetry between hemispheres in amplitude (above 50%);
- sinusoidal type of beta rhythm;
- amplitude more than 7 μV.
The presence of diffuse beta waves with an amplitude no higher than 50-60 μV indicates
Short spindles in the beta rhythm indicate encephalitis. The more severe the brain inflammation, the greater the frequency, duration and amplitude of such spindles. Observed in a third of patients with herpes encephalitis.
Beta waves with a frequency of 16–18 Hz and high amplitude (30–40 μV) in the anterior and central parts of the brain are signs of delayed psychomotor development of a child.
EEG desynchronization, in which the beta rhythm predominates in all parts of the brain, is the second type of neurosis.
Normally, these slow waves can only be recorded on the electroencephalogram of a sleeping person. In a state of wakefulness, such slow waves appear on the EEG only in the presence of degenerative processes in the tissues of the brain, which are combined with compression, high
and lethargy. Paroxysmal theta and delta waves in a person in a state of wakefulness are detected when the deep parts of the brain are damaged.
In children and young people under 21 years of age, the electroencephalogram may reveal diffuse theta and delta rhythms, paroxysmal discharges and epileptoid activity, which are normal variants and do not indicate pathological changes in brain structures.
What do disturbances in the theta and delta rhythms on the EEG indicate? Delta waves with high amplitude indicate the presence of a tumor.
Synchronous theta rhythm, delta waves in all parts of the brain, bursts of bilateral synchronous theta waves with high amplitude, paroxysms in the central parts of the brain - indicate acquired dementia.
The predominance of theta and delta waves on the EEG with maximum activity in the occipital region, flashes of bilateral synchronous waves, the number of which increases with hyperventilation, indicates a delay in the psychomotor development of the child.
A high index of theta activity in the central parts of the brain, bilateral synchronous theta activity with a frequency of 5 to 7 Hz, localized in the frontal or temporal regions of the brain indicate psychopathy.
Theta rhythms in the anterior parts of the brain as the main ones are an excitable type of psychopathy.
Paroxysms of theta and delta waves are the third type of neuroses.
The appearance of high-frequency rhythms (for example, beta-1, beta-2 and gamma) indicates irritation (irritation) of brain structures. This may be associated with various cerebrovascular accidents, intracranial pressure, migraines, etc.
This parameter in the EEG conclusion is a complex descriptive characteristic regarding brain rhythms. Normally, the bioelectric activity of the brain should be rhythmic, synchronous, without foci of paroxysms, etc. At the conclusion of the EEG, the doctor usually writes what specific disturbances in the bioelectrical activity of the brain were identified (for example, desynchronized, etc.).
What do various disturbances in the bioelectrical activity of the brain indicate? Relatively rhythmic bioelectrical activity with foci of paroxysmal activity in any area of the brain indicates the presence of a certain area in its tissue where excitation processes exceed inhibition. This type of EEG may indicate the presence of migraines and headaches.
Diffuse changes in the bioelectrical activity of the brain may be normal if no other abnormalities are detected. Thus, if in the conclusion it is written only about diffuse or moderate changes in the bioelectrical activity of the brain, without paroxysms, foci of pathological activity, or without a decrease in the threshold of convulsive activity, then this is a variant of the norm.
In this case, the neurologist will prescribe symptomatic treatment and put the patient under observation. However, in combination with paroxysms or foci of pathological activity, they indicate the presence of epilepsy or a tendency to seizures. Reduced bioelectrical activity of the brain can be detected in depression.
How to treat
A patient with this disease is treated in the intensive care unit.
The management tactics for patients with diffuse axonal brain damage involve complex intensive therapy. As a rule, victims are transferred to artificial ventilation. No matter how severe their condition, the use of surgical treatment methods is not justified. Indications for surgery can only be identified concomitant focal injuries that cause compression of the brain (intracranial hematomas, depressed fractures).
The main directions of conservative therapy are:
- maintaining normal functioning of breathing and circulation;
- prevention of complications and secondary brain damage;
- parenteral nutrition;
- correction of disturbances in water-salt metabolism and acid-base balance;
- psychostimulant therapy after recovery from coma;
- physical therapy exercises to combat paresis and prevent contractures (immobility of joints).
The recovery period after an injury can last indefinitely, so such patients require constant supervision by a specialist and long-term rehabilitation.