Polyneuropathy is the clinical manifestations of multiple lesions of peripheral nerves of different nature.
Often toxic substances of exogenous or endogenous origin act as a damaging factor for polyneuropathy.
The resulting toxic polyneuropathies (TP) have a common clinical picture and treatment approaches. Depending on the time of exposure and the characteristics of contact with the toxic agent, an acute or chronic form of the disease develops.
The relevance of toxic damage to the nervous system is due to the expansion of human contacts with harmful production factors, the progressive deterioration of the environmental situation and the decrease in the quality of food products produced using new technologies.
The proportion of accidents caused by uncontrolled drug intake is growing. In addition, the cause of pathology of peripheral nerves is often infectious pathogens that exert neurotropic effects through toxins.
Factors of occurrence
External factors include:
- HIV infection.
- Hermes.
- Diphtheria.
Different types of medications are used for treatment. Tonic neuropathy can occur as a result of a lack of vitamin B6 or E. Some chemicals can also cause harm:
- Lead.
- Arsenic.
- Alcohol.
- Organophosphorus preparations.
Complications may occur:
- Diabetes.
- Myeloma.
- Waldenström's syndrome.
- Diffuse connective tissue disorders.
Complaints that such patients make in most examples:
- Tingling in arms and legs.
- Sensitivity problems.
Symptoms worsen as tonic neuropathy develops. You can compare this state with the feeling of wearing socks and gloves. If the disease progresses further, the following may occur:
- Cramps.
- Swelling in the arms and legs.
- Trophic transformations of the skin, darkening.
Endogenous toxic polyneutropathies
This type of disease occurs in most cases due to dysfunction of the endocrine glands, as a result of a deficiency of necessary hormones, or when the functions of other internal human organs are impaired. The following types are distinguished:
- Diabetic polyneuropathy can begin acutely, progress slowly or quite rapidly. It first appears as pain and loss of sensation in the limbs.
- Polyneuropathy associated with paraproteinemia and dysproteinemia occurs mainly in older people and is associated with diseases such as multiple myeloma and macroglobulinemia. Clinical manifestations are expressed in pain and paresis of the lower and upper extremities.
- Polyneuropathy also develops in diffuse type connective tissue diseases: periarthritis nodosa, rheumatoid arthritis, systemic lupus erythematosus, scleroderma.
- Hepatic polyneuropathy is a consequence of diabetes and alcoholism and has similar clinical manifestations.
- Neurological disorders in gastrointestinal diseases are associated with pathology of the digestive organs, leading to vitamin deficiencies. Celiac disease can provoke polyneuropathy, which is expressed in psychomotor impairment, epilepsy, visual disturbances, and ataxia.
Clinical picture
Initially, toxic polyneuropathy is accompanied by symptoms such as numbness of the arms and legs. In the first stages, the lesion affects the distal sections. As the disease progresses, proximal areas are affected.
With this diagnosis, tingling and goosebumps often appear on the skin. Often patients do not pay attention to such signs. As the disease worsens, symptoms increase. In addition to deterioration in sensitivity, problems with motor activity may appear. Patients complain of a feeling of heaviness and fullness in the arms and legs.
The later stages are characterized by more pronounced symptoms. Symptoms of autonomic disorders appear. They arise in the form of a decrease in the trophism of the skin and the appearance of all kinds of pigmentation. In a complex condition, patients find it difficult to move independently or perform simple activities in everyday life.
Causes
The cause of toxic polyneuropathy of the lower extremities is various intoxications of the whole body with the development of a specific pathological process in the peripheral nerves.
The pathological mechanism of TP is based on the toxic effects of certain external or internal factors, leading to the destruction of the myelin sheath and the axial cylinder of the nerve trunks.
The lesion mainly affects the distal parts of the extremities due to a number of predisposing factors:
- high degree of development of differentiated functions of the hands and feet (in evolutionary terms);
- the greatest susceptibility of these departments to metabolic changes in the body;
- high probability of developing hypoxia when compensatory mechanisms fail;
- insufficiently developed barrier function towards toxic substances.
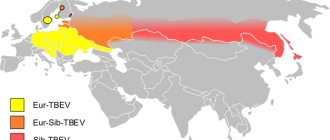
The points of application of different neurotoxicants may be different. For example, organophosphate poisons cause diffuse damage to the central and peripheral nervous system. Arsenic, mercury, organic solvents and carbon disulfide selectively act on sensitive nerve endings.
Hexochloraphene, lead, arsenic, tellurium and thallium mainly interfere with the motor functions of peripheral nerves.
Exogenous toxic polyneuropathy
As mentioned above, these types of disease manifest themselves under the influence of the environment:
- Toxic trace elements.
- Metals.
- Reagents.
- Medicines.
Like another type of polyneuropathy, these disorders manifest themselves in acute and chronic forms.
Diphtheria polyneuropathy
From the name of the pathology, it can be determined that it appears after a complex form of diphtheria, which is accompanied by exotoxins. Often this phenomenon occurs in adults.
In this case, there is an impact on the membranes of the nerve fibers of the skull and their deformation. Signs of the disease appear in the first week or 4 weeks after infection. They are characterized by deterioration in the functioning of the optic nerves, swallowing function, speech, and may experience breathing problems or tachycardia. In any situation, the signs disappear after 2-4 weeks or after several months.
Herpetic polyneuropathy
This type of pathology manifests itself due to the activity of Epstein-Barr viral cells, ordinary herpes of 1 or 2 degrees, chickenpox, cytomegalovirus.
Young children most often become infected with this infection. After an illness, the immune system is strengthened. When the body's protective functions become worse, polyneuropathy may appear with a rash throughout the body.
Polyneuropathy due to HIV infection
Neurological complications occur in 2/3 of patients with HIV infection. They often appear in the last stages of the disease. The body stops working normally due to a whole list of problems:
- Secondary infection.
- Neoplasms.
- Side effects after medications.
As a result, neurological disorders occur. Sometimes the sensitivity of the legs worsens, and lower back pain appears. Such disorders can be fatal.
Lead polyneuropathy
This type of pathology manifests itself due to lead poisoning that enters the human body through inhalation or the gastrointestinal tract. the substance is deposited in the liver and bone tissue. Toxic polyneuropathy of the lead form manifests itself as follows:
- Lethargy.
- Fatigue increases.
- My head hurts.
- Attention and memory deteriorate.
- Limbs shake and hurt.
- Colitis appears.
- Anemia.
This disease is characterized by damage to the radial and peroneal nerves.
Arsenic polyneuropathy
Arsenic enters the human body simultaneously with insecticides, drugs and dyes. This disorder is an occupational disorder for people involved in metal smelting. If a harmful component enters the body only once, vascular hypotension, nausea, and vomiting appear.
After 2-3 weeks, polyneuropathy occurs, which is characterized by muscle weakness in the leg.
When another arsenic poisoning occurs, it affects sensitivity and motor skills. If a person receives a harmful component into the body on a regular basis, hypersalivation and vascular problems occur. Arsenic polyneuropathy is detected by analyzing trace elements contained in urine, nails and hair. Recovery of patients after pathology lasts several months.
Alcoholic form of the disease
In medicine, there is an opinion that toxic polyneuropathy as a result of alcohol intoxication is not studied very well. The principle of influence is not entirely clear. The main reasons include thiamine deficiency and developing gastroduodenitis. Such disorders are aggravated by alcohol abuse. Alcohol has a destructive effect on the nervous system.
Signs of alcoholic form:
- Pain in the calves gets worse when you press. Paresthesia primarily appears in distal areas.
- A little later, weakening and numbness of the arms and legs occurs.
- The paretic muscular system rapidly atrophies.
- Deep reflexes become worse, and the areas where they appear increase.
- A disorder of superficial sensitivity occurs, as if the person was wearing gloves and socks.
- Intensification of symptoms in the absence of therapy causes symptoms similar to the manifestation of syphilis.
Often, alcoholic neuropathy occurs rapidly after severe hypothermia. This variety is characterized by extensive transformations in the nervous system. Patients often experience redness of the skin and other complaints.
Vasomotor, secretory and trophic disorders are considered to be the cause of worsening sweating, swelling of the arms and legs, darkening of the skin and increased temperature.
Pain in the alcoholic form of the disease may worsen for several months. If you start treatment in time, you can completely get rid of the pathology.
Therapeutic techniques:
- Physiotherapy.
- Use of proserine.
- Vitamins.
Types of polyneuropathy (polyneuritis)
Diabetic polyneuropathy
Diabetic polyneuropathy is a type of nerve damage that occurs from intoxication of the body as a whole as a result of tissue metabolism disorders in patients with diabetes.
The leading factor in the occurrence of diabetic neuropathy (polyneuropathy) is angiopathy accompanying diabetes, which leads to impaired regional circulation. Depending on the level of nerve damage in diabetic neuropathy (polyneuropathy) and alcoholic polyneuritis, sensory disturbances (numbness, tingling, burning and goosebumps), pain and muscle weakness in the patient will be at different levels.
Microvascular complications of diabetes mellitus:
Retinopathy | Neuropathy | Nephropathy |
| Peripheral neuropathy:
Autonomic (autonomic) neuropathy:
|
|
Macrovascular complications of diabetes mellitus:
Coronary complications | Cerebrovascular complications | Peripheral vascular diseases |
|
|
|
Alcoholic polyneuropathy
Alcoholic polyneuropathy is a type of nerve damage that occurs in patients who abuse alcohol for a long time.
Toxic polyneuropathy, polyneuropathy as a result of chemotherapy
Most toxic polyneuropathies manifest as distal axonal degeneration, which develops gradually over time in the patient. The causes of toxic polyneuropathy are varied and include medications, heavy metals, occupational factors, and environmental substances. Newer anticancer drugs, antiretrovirals, or excessive use of other medications (especially pyridoxine (vitamin B6)) can also cause toxic polyneuropathy. When assessing the patient's condition, there is usually a connection between the time of administration and dosage of a toxic substance with the onset of clinical manifestations of toxic neuropathy. In general, the administration of small doses of a drug over a long period of time is less toxic to the body than large doses administered over a short period of time, even if the total doses are equal.
Onset of disease (occurring after administration of a toxic agent) followed by recovery or at least a delay in further development of the pathological process (after cessation of administration of the toxin) is the best evidence of the presence of toxic polyneuropathy (together with other typical symptoms and signs of neuropathy caused by the suspected toxic substrate) . Neuropathy may initially appear and may continue to progress after the administration of the toxic substance is stopped. This phenomenon of the development of a pathological process by inertia occurs when taking antitumor drugs platinum, benzene drugs, nucleoside reverse transcriptase inhibitors or pyridoxine (vitamin B6).
Clinical analysis of the disease history includes identifying the connection between the moment the toxin enters the patient’s body and the onset of:
- motor and sensory symptoms of nerve damage
- other concomitant disease that may cause toxic neuropathy
- symptoms of general intoxication
A nerve biopsy sometimes reveals signs characteristic of this type of nerve injury:
- osmophilic inclusions in the Schwann cell during intoxication with amiodarone, peroxyline and chloroquinoline (a synthetic analogue of quinoline, used to treat malaria)
- peri-nodal axonal massive edema in benzene neuropathy
Levels of certain toxins can be detected in certain types of body tissue:
- heavy metals can be detected in urine (arsenic, thallium), in hair and nails (arsenic)
- laboratory analysis of plasma levels of administered drugs may also be useful in establishing the diagnosis of toxic neuropathy
Source: www.minclinic.ru
Diagnosis and treatment
To correctly diagnose the disease, you need to collect anamnesis. For this purpose, the doctor determines the patient’s working conditions, possible interactions with chemical components, and how often alcohol is consumed. Taking an anamnesis is of great importance, especially in a situation where the patient has recently changed several jobs.
During neurological studies, it is not always possible to obtain comprehensive information regarding the etiology of the disease. A person can only determine damage to peripheral nerve endings. Using special equipment and tools, it is necessary to determine the process of disruption of the transmission of bioelectric impulses. But the causes of polyneuropathy cannot be determined.
In some situations, doctors prescribe a peripheral nerve biopsy . Thanks to this, it will be possible to become familiar with the structural transformations that occur in neurons.
Therapeutic techniques are determined to obtain the following results:
- Renewal of the structure of nerve fibers.
- Increasing bioelectric activity in problem areas.
- Normalization of motor activity of arms and legs.
- Preventing the development of the disorder.
For therapy to be successful, you need to get rid of different types of interaction with the provoking agent. When the cause is a disorder of the endocrine system, you need to be more careful in treatment.
Many medications are used to stabilize the peripheral nerves. To begin with, specialists prescribe medications that help restore the myelin sheath of the nerve trunks. Vitamin B is used for these purposes.
A good effect can be achieved due to the action of drugs that help strengthen the conductivity of impulses. Ipigrix is often prescribed for this purpose.
In the acute form of the disorder, the use of glucocorticoids is justified. Of the medications included in this list, you need to consider Dexamethasone. If autoimmune activity develops during the disease, plasmapheresis should be used. When patients respond well to physical therapy techniques, electrical stimulation can be used.
Thanks to this, it will be possible to improve the condition of peripheral nerves and restore the conduction of signals.
First aid
In order to prevent the development of this dangerous pathology of the retina, in case of poisoning with methyl alcohol or other dangerous substances, it is necessary to take timely measures to cleanse the body. The poison can be removed by artificially inducing vomiting, gastric lavage and taking laxatives. In case of acute neuropathy caused by methyl alcohol poisoning, it is important to use an antidote - ethyl alcohol. This drug is administered intravenously by drip. In order not to harm the body, use a 10% solution, which is prepared at the rate of 1 g of ethyl alcohol per 1 kg of the patient’s body weight. It is also recommended to take pure vodka internally, 50 g 3 times a day for 3 days.
Hemodialysis is considered the best treatment for toxic neuropathy
and the use of 4% sodium bicarbonate solution. The drug is administered intravenously to eliminate tissue acidosis, a serious consequence of methyl intoxication.
To maintain the body and improve the condition, patients with signs of toxic neuropathy are prescribed vitamins C and B, heart medications, and hemodez.
If symptoms of toxic neuropathy are detected, you must call an ambulance or, without delay, independently seek advice from a neurologist, toxicologist and ophthalmologist.
Prognosis and complications
The outcome of the disease is determined by its form and duration of interaction with toxic components. Timely initiation of treatment is of no small importance for prognosis. In the acute form of the disease, it is often possible to obtain a good treatment result with complete elimination of symptoms. This can only be true with correct and timely diagnosis.
With quality treatment, a chronic disease does not develop and does not bother patients much. With proper treatment, the course of the disease can be controlled. Patients with this diagnosis can survive for a long time. A negative outcome is possible with acute intoxication, saturation of the body with toxic substances.
As a result, there is a possibility of developing kidney or liver failure. If problem conditions are not treated promptly, the likelihood of death increases.
Classification of violation
It is fundamentally important for the diagnosis and treatment of TP to distinguish between chronic, subacute and acute forms of the disease. The first of them imply the development of pathological changes over 60 days or more; in the subacute form, the process develops in a period of 40 to 60 days. And acute toxic damage to peripheral nerves is diagnosed when the clinical manifestations of the disease appear before 40 days from the moment of contact with the causative factor.
Depending on the origin of the toxic substance, two large groups of TP are distinguished:
- caused by exogenous intoxications;
- caused by endogenous toxic substances.
The first group of TP is represented by diphtheria polyneuropathy, damage to the peripheral nervous system due to herpetic and HIV infections, lead, arsenic and organophosphate polyneuropathies, as well as alcoholic and drug-induced polyneuritis.
The group of endogenous TP includes polyneuropathies that developed against the background of diabetes mellitus, connective tissue diseases, dysproteinemia, uremia, liver failure and gastrointestinal diseases.
Prevention
To prevent such violations, you need to work in compliance with safety rules. For this purpose, you need to use protective equipment and not linger in an environment saturated with toxins.
It is necessary to promptly get rid of diseases that cause various complications in the form of endogenous factors. It is advisable to come for examination at least once a year.
Toxic polyneuropathy is a serious disease that requires timely support. Therefore, if various symptoms of such a disorder occur, you need to contact specialists who will select the right treatment methods.
Features of treatment of the disease
Toxic polyneuropathy, the treatment of which primarily comes down to eliminating the causes of its occurrence, should be considered comprehensively.
Depending on the type of disease and the severity of its course, the following medications are prescribed:
- "Tramadol" and "Analgin" - for severe pain.
- "Methylprednisolone" - for particularly severe cases of the disease.
- “Pentoxifylline”, “Vazonit”, “Trental” - to increase blood flow in the vessels of nerve fibers.
- B vitamins.
- "Piracetam" and "Mildronate" - to enhance the absorption of nutrients by tissues.
The following physiotherapeutic methods can be used:
- electrical stimulation of the nervous system;
- massotherapy;
- magnetic stimulation of the nervous system;
- indirect effects on organs;
- hemodialysis, blood purification.
- Exercise therapy.
It is up to the doctor to decide which method of treating polyneuropathy is most appropriate in a particular case. It is absolutely impossible to ignore the symptoms of the disease. Acute polyneuropathy can become chronic, which threatens loss of sensation in the limbs, muscle atrophy and complete immobility.