Diabetes mellitus is one of the most common diseases today. The clinical course of the disease is often accompanied by the occurrence of chronic complications, and one of them is diabetic polyneuropathy.
Diabetic polyneuropathy code ICD 10 (international classification of diseases, 10th revision), in some cases leads to gangrene and subsequent amputation of the affected limb. As a result, the patient must understand that the effectiveness of treatment largely depends on at what stage of the disease the patient sought help from a doctor.
Symptoms and diagnosis
NAION usually appears suddenly and immediately after waking up. Patients notice blurred vision in one eye. The vision in this eye is obscured by a dark shadow, often only the upper or lower half of the vision is visible, usually the area closer to the nose. It doesn't cause pain. At about 6 months after a heart attack, 42.7% of patients' visual acuity improves by 3 or more lines on the Snellen chart (chart with smaller letters on each bottom line). In addition, in 12.4% of patients, vision deteriorates by 3 lines or more. Involvement of the other eye occurs in approximately 15% to 20% of patients with NAION within 5 years.[1] Fortunately, it may not be very destructive, since visual acuity may remain only moderately impaired. Additionally, most cases of NAION involve loss of only half of the visual field (either the upper or lower half of the visual field, but not both). Several cases of NAION have resulted in almost complete loss of vision.
Arteritic AION is similar in presentation to non-arteritic AION and patients aged 50 or older diagnosed with NAION should be evaluated to rule out AAION (symptoms: painful jaw muscle spasms, scalp weakness, unintentional weight loss, fatigue, myalgia, and loss of appetite). Additionally, patients with NAION over the age of 75 should have blood tests done frequently anyway.
Diabetic polyneuropathy of the lower extremities: treatment with drugs, symptoms
Diabetic polyneuropathy (ICD-10 code – G63.2* or E10-E14 p.4) is the presence of signs of damage to the nervous system in patients with diabetes mellitus, if other causes of pathology are excluded. The diagnosis can be established even in the absence of complaints from the patient, when the lesion is identified during the examination.
Diabetic polyneuropathy is not confirmed based on a single clinical sign. Modern WHO recommendations say that diagnostics should determine the presence of at least two manifestations of damage in order to confirm the pathology of the nervous system against the background of the “sweet disease”.
If the process occurs in individual nerve fibers, then we are talking about neuropathy. In case of multiple lesions, polyneuropathy develops. Patients with type 1 diabetes mellitus “get” complications in 15-55% of cases, type 2 – 17-45%.
Classification
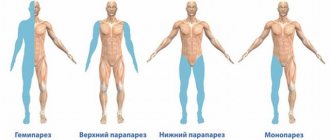
The division of polyneuropathy is quite complex, since it combines a number of syndromes. Some authors prefer to classify the lesion depending on which parts of the nervous system are involved in the process: peripheral (spinal nerves) and autonomic (autonomic) forms.
Another widely used classification:
- Polyneuropathy is rapidly reversible (temporary, occurring against the background of sudden surges in blood sugar).
- Stable symmetrical polyneuropathy: damage to thick nerve fibers (distal somatic); damage to thin fibers; Autonomous type defeat.
- Focal/multifocal polyneuropathy: cranial type; compression type; proximal type; thoracoabdominal type; neuropathy of the extremities.
Important! Peripheral damage to thick nerve fibers, in turn, can be sensory (affects sensory nerves), motor (motor nerves), sensorimotor (combined pathology).
Causes
High blood sugar levels, characteristic of diabetics, can pathologically affect the condition of small vessels, causing the development of microangiopathy, and large arteries, provoking macroangiopathy. The changes that occur in large vessels are similar to the mechanism of formation of atherosclerosis.
Angiopathy is the main link in the development of nerve damage in diabetes mellitus
Regarding arterioles and capillaries, everything happens differently here. Hyperglycemia activates the action of the enzyme protein kinase-C, which helps to increase the tone of the walls of blood vessels, thickens their membrane, and enhances blood clotting processes. Glycogen, mucoproteins and other substances of carbohydrate nature begin to be deposited on the inner wall of arterioles and capillaries.
The toxic effects of glucose may also be different. It attaches to proteins, making them glycated, which causes damage to vascular membranes and disruption of metabolic, transport and other vital processes in the body. The most famous glycated protein is hemoglobin HbA1c. The higher its indicators, the less oxygen the body cells receive, and tissue hypoxia develops.
Diabetic polyneuropathy occurs due to damage to endoneurial (located in the connective tissue layer between the nerve fibers in the nerve trunk) vessels. This is supported by the proven relationship between the thickness of vascular membranes and the density of fibers in the nerve. The process involves neurons and their processes, which die due to metabolic disorders in the body of diabetics.
Provoking factors
The following factors contribute to the development of polyneuropathy in diabetes mellitus:
- violation of self-control of blood sugar levels;
- long period of underlying disease;
- high blood pressure;
- high growth;
- elderly age;
- presence of bad habits (smoking, drinking alcohol);
- dyslipidemia;
- genetic predisposition.
Features of the pathological process with multiple lesions of nerve fibers
Stages
Depending on the severity of the manifestations, the following stages of damage are distinguished, on the basis of which the necessary treatment of polyneuropathy is determined:
Angiopathy in diabetes mellitus
- 0 – no visual data;
- 1 – asymptomatic complication;
- 1a – there are no complaints from the patient, but pathological changes can already be determined using diagnostic tests;
- 1b – there are no complaints, changes can be determined not only by specific tests, but also by a neurological examination;
- 2 – stage of clinical manifestations;
- 2a – symptoms of the lesion appear together with positive diagnostic tests;
- 2b – stage 2a + weakness of the dorsal flexors of the feet;
- 3 – polyneuropathy complicated by disability.
Symptoms
The symptoms of diabetic polyneuropathy are directly dependent on the stage and form of its development, as well as the therapy used.
Sensory disorders
Characteristic manifestations of sensory pathology. They can be determined solely by diagnostic tests (subclinical form) or become patient complaints (clinical form).
Patients suffer from pain. The pain can be burning, baking, shooting, throbbing.
Its appearance can be triggered even by factors that do not cause discomfort in healthy people.
Important! Diabetic polyneuropathy of the lower extremities is characterized by similar manifestations on the feet and legs, since the endoneurial vessels are affected first.
The patient may complain of numbness, a feeling of goosebumps, a burning sensation, and increased sensitivity to cold, heat, and vibration.
Physiological reflexes are preserved, but pathological ones may be absent.
As a rule, sensory disorders are symmetrical. When an asymmetric pathology appears, the pain syndrome begins in the pelvic area and goes down the thigh. This is accompanied by a decrease in the volume of the affected limb, a violation of its proportionality in relation to the rest of the body.
Impaired pain sensitivity is one of the striking symptoms of polyneuropathy
Combined pathology
The development of sensorimotor polyneuropathy in most cases has a chronic course. Diabetics complain of the following symptoms:
- feeling of numbness;
- pain of a different nature;
- impaired sensitivity up to complete absence;
- muscle weakness;
- absence of physiological and appearance of pathological reflexes;
- night cramps of the lower and upper extremities;
- lack of stability when walking.
A frequent complication of chronic processes in combination with mechanical damage is diabetic foot, a pathological condition in which the lesion affects all structures, including cartilage and bone elements. The result is deformation and gait disturbance.
An important point is to differentiate the diabetic sensorimotor form from alcoholic polyneuropathy.
Autonomous defeat
Nerve cells that are localized in internal organs can also be damaged. Symptoms depend on which organ or system is affected.
Pathology of the heart and blood vessels is manifested by orthostatic hypertension, pulmonary edema, and impaired sensitivity to physical activity. Patients complain of irregular heart rhythm, increased blood pressure, shortness of breath, and cough.
Lack of timely treatment can lead to death.
Heart rhythm disturbance is a possible symptom of autonomic pathology
Damage to the gastrointestinal tract is manifested by paresis, decreased tone of its parts, disruption of normal microflora, and reflux disease. Patients suffer from attacks of vomiting, heartburn, diarrhea, weight loss, and pain.
Polyneuropathy of the genitourinary system is accompanied by bladder atony, urine backflow, sexual dysfunction, and secondary infections are possible. Pain appears in the lower back and above the pubis, urination becomes frequent, accompanied by pain and burning, body temperature rises, and pathological discharge from the vagina and urethra appears.
Other lesions:
- disruption of sweating processes (increased or sharply reduced, even completely absent, work of the sweat glands);
- pathology of the visual analyzer (the pupil decreases in diameter, visual acuity sharply decreases, especially at dusk);
- Adrenal polyneuropathy has no symptomatic manifestations.
Diagnostics
Before prescribing treatment for diabetic polyneuropathy of the lower extremities, the patient is examined not only for neurological issues, but also by an endocrinologist to clarify the level of compensation for the underlying disease.
Important! After the doctor collects an anamnesis of the patient’s life and illness, an examination of the general condition and neurological diagnosis is carried out.
The specialist clarifies the level of different types of sensitivity (temperature, vibration, tactile, pain). For this purpose, cotton wool, monofilaments, hammers with a brush and a needle at the end, and tuning forks are used.
In special cases, material is collected via biopsy for further histology. Neurological examination also includes the following methods:
- Evoked potentials - nerve fibers are stimulated, the responses to which are recorded by a special device.
- Electroneurography is a diagnostic method that is used to determine the speed of propagation of nerve impulses from parts of the central nervous system to receptors.
- Electromyography is an examination that clarifies the state of impulse transmission from nerve cells to the muscular system.
Determination of impulse transmission is an important diagnostic method
Laboratory diagnostic methods are mandatory: clarification of glycemic levels, biochemical analysis, indicators of C-peptide and glycated hemoglobin. If an autonomic lesion is suspected, the patient is prescribed an ECG, echocardiography, cardiac ultrasound, vascular Dopplerography, ultrasound of the gastrointestinal tract, endoscopy, and x-ray.
The state of the urinary system can be determined by daily urine analysis, Zimnitsky and Nechiporenko analysis, as well as by ultrasound, cystography, cystoscopy and electromyography.
Features of treatment
For the treatment of diabetic polyneuropathy, correction of blood sugar levels is a prerequisite. This is done by an endocrinologist who reviews insulin therapy regimens and the use of glucose-lowering drugs. If necessary, medications are replaced with more effective ones or additional medications are prescribed.
The diet is adjusted and the required physical activity regime is selected. The doctor gives advice on how to maintain blood pressure and body weight within acceptable limits.
The following groups of medications are prescribed:
- Alpha-lipoic acid derivatives are the drugs of choice. They are able to remove excess cholesterol and stop the toxic effects of external factors on the liver and blood vessels. Representatives - Berlition, Lipoic acid, Thiogamma. The course of treatment is at least 2 months.
- B vitamins – improve the functioning of the central and peripheral nervous system, help normalize the transmission of neuromuscular impulses (Pyridoxine, Cyanocobalamin, Thiamine).
- Antidepressants - used to reduce painful symptoms (Amitriptyline, Nortriptyline). They are prescribed in small doses, gradually achieving the required therapeutic effect.
- Aldose reductase inhibitors - positive aspects in therapy with drugs of this group were identified, but they did not live up to all the hopes placed on them. Used at the discretion of the attending physician (Olrestatin, Isodibut, Tolrestat).
- Local anesthetics are used to relieve pain in the form of applications. The effect appears after 10-15 minutes.
- Anticonvulsants – Carbamazepine, Finytoin. This group requires careful dosage selection. Start with small doses and increase over several weeks.
Derivatives of alpha-lipoic (thioctic) acid - drugs for normalizing the condition of blood vessels and eliminating discomfort in diabetic damage to the nervous system
Folk remedies
Diabetic polyneuropathy can be treated not only with traditional medicine, but also with various remedies and infusions prepared at home.
Recipe No. 1
Lay out pre-prepared nettle stems. The patient should trample on them for at least 7-10 minutes a day.
Recipe No. 2
Mix crushed burdock roots and blueberry leaves. 3 tbsp. pour the resulting mixture with a liter of boiling water and leave for at least 8 hours. Next, put on fire and simmer for another 3 hours. After the broth has cooled, it needs to be strained. Drink the resulting amount of liquid throughout the day.
Recipe No. 3
A glass of oats is poured with 1 liter of boiling water. Leave for 10 hours, then boil the mixture for at least 40 minutes. Remove from the stove and send to a warm place. Then filter and take a glass half an hour before each meal.
It must be remembered that it is impossible to get rid of polyneuropathy using folk remedies without traditional medicine and control over blood sugar levels. But the combined effect of these factors can lead to a favorable outcome of the pathology.
Last updated: April 18, 2018
Source: https://sosudy.info/diabeticheskaya-polineyropatiya
Causes and risk factors
The use of injury mechanism for NAION is quite controversial. However, experts in the field have reached a consensus that most cases present two main risk factors. Firstly, predisposition in the form of the type of shape of the optical disc. The optic disc is where axons from retinal ganglion cells gather to form the optic nerve. The optic nerve is a bundle of axons that carry visual signals from the eyes to the brain. This optic nerve must penetrate the wall of the eye, and the opening to accommodate it is usually 20-30% larger than the diameter of the nerve. In some patients, the optic nerve is almost the same diameter as the hole at the back of the eye, and the optic disc appears "full" when viewed under ophthalmoscopy. A full disk also qualifies as a "risk disk." Despite the risk factor, the vast majority of people with full discs do not experience NAION.
The second major risk factor is more general cardiovascular risk factors. The most common are diabetes mellitus, hypertension and high cholesterol. While these factors predispose a patient to develop NAION, the most common factor noted is a sudden drop in blood pressure during sleep (nocturnal hypotension)—which is why at least 75% of patients first discover vision loss when waking from sleep. These vascular risk factors lead to ischemia (poor blood supply) in part of the optic nerve head. The disc then swells and overflows the optic disc opening, leading to compression and increased ischemia.
Because both eyes tend to have a similar appearance, an optometrist or ophthalmologist should look at the good eye to assess the anatomical predisposition. An unaffected eye has a 14.7% risk of NAION over five years.[3]
A number of studies have been devoted to the connection between the use of Viagra and NAION.[4][5][6][7][8][9]
Symptoms of the disease
Diabetic polyneuropathy often affects the nerves of the lower extremities. The symptoms of this pathology themselves can be divided into two groups: initial and late.
Initial symptoms include:
- Minor tingling in the extremities
- Numbness of the lower extremities, especially during sleep
- Decreased sensation in affected limbs
It is also worth highlighting that patients rarely pay attention to the primary symptoms of the disease and turn to specialists only with late pathological manifestations.
Late symptoms are expressed as follows:
- Severe pain in the legs
- Weakening of the foot muscles and deformation
- Changing nail thickness
- Due to constant pain – insomnia and chronic fatigue
Treatment
It was believed that there was no recognized treatment that could reverse the damage caused by NAION. However, a recent large study showed that when patients were treated with high doses of corticosteroids in the early stages of NAION in eyes with an initial visual acuity of 20/70 or worse diagnosed within 2 weeks of disease onset, there was a 70% improvement in visual acuity in the group , treated compared with 41% in the control group.[10] This study and, naturally, a review of the history of NAION studies (Ophthalmology 2008; 115:298-305) showed that visual acuity may improve up to 6 months, but not after that. To minimize the risk of further deterioration of vision in the fellow or other eye, it is important to reduce risk factors. Common sense dictates that one should try to control cardiovascular risk factors for many reasons, including protecting against this second eye. Sudden vision loss requires ophthalmological consultation. If NAION is suspected, consultation with a neuro-ophthalmologist will be required.
There is a lot of research currently looking for ways to protect the nerve (neuroprotection), or even generate new fibers in the optic nerve.[11][12][13][14][15] There is no current clinical trial for the treatment of NAION. There is still no evidence that so-called neuroprotectors have any beneficial effect in NAION.
In addition to such research, patents have been filed for Pfizer, the University of Southern California, Otsuka Pharmaceutical and other individual inventors for innovations related to the treatment of anterior ischemic optic neuropathy.[16]
Methods for diagnosing pathology
The examination is carried out only by an ophthalmologist. Partial atrophy has similar symptoms to cataracts and amblyopia, so only a specialist can make an accurate diagnosis. Diagnostics necessarily includes testing visual acuity, examining the fundus through the pupil, assessing color perception , and also:
- spheroperimetry - precise determination of the boundaries of the field of view;
- perimetry - identification of the affected part of the nerve;
- video ophthalmography - studying the degree of nerve damage.
To increase the information content, the patient is prescribed laboratory diagnostic methods - blood tests (general and biochemistry), tests for borreliosis and syphilis.
ICD 10. Class VI. Diseases of the nervous system (G50-G99)
Excludes: neuralgia NOS (M79.2) neuritis NOS (M79.2) peripheral neuritis during pregnancy (O26.8) radiculitis NOS (M54.1)
G60.0 Hereditary motor and sensory neuropathy Disease: • Charcot-Marie-Toots • Dejerine- Sotta Hereditary motor and sensory neuropathy, types I-IY. Hypertrophic neuropathy in childrenPeroneal muscular atrophy (axonal type) (hepertrophic type). Roussy-Levi syndrome G60.1 Refsum disease G60.
2 Neuropathy in combination with hereditary ataxia G60.3 Idiopathic progressive neuropathy G60.8 Other hereditary and idiopathic neuropathies. Morvan's disease. Nelaton's syndromeSensory neuropathy:• dominant inheritance• recessive inheritanceG60.9 Hereditary and idiopathic neuropathy, unspecified
G61.0 Guillain-Barre syndrome. Acute (post-)infectious polyneuritis G61.1 Serum neuropathy. If necessary, identify the cause, use an additional code for external causes (class XX). G61.8 Other inflammatory polyneuropathies G61.9 Inflammatory polyneuropathy, unspecified
G62.0 Drug-induced polyneuropathy If it is necessary to identify a drug, use an additional code for external causes (class XX). G62.1 Alcoholic polyneuropathy G62.2 Polyneuropathy caused by other toxic substances If it is necessary to identify a toxic substance, use an additional code for external causes (class XX). G62.
G63.0* Polyneuropathy in infectious and parasitic diseases classified in other headings Polyneuropathy in: • diphtheria (A36.8) • infectious mononucleosis (B27. - ) • leprosy (A30. - ) • Lyme disease (A69.2 ) • mumps (B26.8)• herpes zoster (B02.2)• late syphilis (A52.
1)• congenital syphilis (A50.4)• tuberculosis (A17.8)G63.1* Polyneuropathy in neoplasms (C00-D48)G63.2* Diabetic polyneuropathy (E10-E14 with a common fourth sign .4)G63.3* Polyneuropathy in other endocrine diseases and metabolic disorders (E00-E07, E15-E16, E20-E34, E70-E89)G63.
4* Polyneuropathy with malnutrition (E40-E64)G63.5* Polyneuropathy with systemic connective tissue lesions (M30-M35)G63.6* Polyneuropathy with other musculoskeletal lesions (M00-M25, M40-M96)G63.8* Polyneuropathy in other diseases classified elsewhere. Uremic neuropathy (N18.8)
Peripheral nervous system disorder NOS
Excluded: botulism (A05.1) transient neonatal Myasthenia gravis (P94.0)
G70.0 Myasthenia gravis If the disease is caused by a drug, an additional code of external causes (class XX) is used to identify it. G70.1 Toxic disorders of the neuromuscular junction If it is necessary to identify a toxic substance, an additional code of external causes is used (class XX). G70.2 Congenital or acquired myasthenia G70.8 Other neuromuscular junction disorders G70.9 Neuromuscular junction disorders, unspecified
Excludes: multiple congenital arthrogryposis (Q74.3) metabolic disorders (E70-E90) myositis (M60. -)
G71.0 Muscular dystrophyMuscular dystrophy:• autosomal recessive childhood type, reminiscent of Duchenne or Becker dystrophy• benign [Becker]• benign scapuloperoneal with early contractures [Emery-Dreyfus]• distal• glenohumeral-facial• limb-girdle• ocular muscles• oculopharyngeal [oculopharyngeal]• scapulofibular• malignant [Duchenne] Excluded:
congenital muscular dystrophy:• NOS (G71.2)• with specified morphological lesions of muscle fiber (G71.2) G71.1 Myotonic disorders. Myotonic dystrophy [Steiner]Myotonia:• chondrodystrophic• medicinal• symptomaticCongenital myotonia:• NOS• dominant inheritance [Thomsen]• recessive inheritance [Becker] Neuromyotonia [Isaacs].
• central nucleus• mininuclear• multinuclearDisproportion of fiber typesMyopathy:• myotubular (centronuclear)• nemaline [disease of the nemaline body]G71.3 Mitochondrial myopathy, not elsewhere classifiedG71.8 Other primary muscle lesionsG71.9 Primary muscle lesion, unspecified. Hereditary myopathy NOS
G72 Other myopathies
Excludes: congenital arthrogryposis multiplex (Q74.3) dermatopolymyositis (M33. -) ischemic muscle infarction (M62.2) myositis (M60. -) polymyositis (M33.2)
G72.0 Drug myopathy If it is necessary to identify a drug, use an additional code for external causes (class XX). G72.1 Alcoholic myopathy G72.2 Myopathy caused by another toxic substance If it is necessary to identify a toxic substance, use an additional code for external causes (class XX). G72.
G73.0* Myasthenic syndromes in endocrine diseasesMyasthenic syndromes in:• diabetic amyotrophy (E10-E14 with a common fourth sign .4)• thyrotoxicosis [hyperthyroidism] (E05. - )G73.1* Eaton-Lambert syndrome (C80)G73.2 * Other myasthenic syndromes with tumor lesions (C00-D48)G73.
3* Myasthenic syndromes in other diseases classified in other headings G73.4* Myopathy in infectious and parasitic diseases classified in other headings G73.5* Myopathy in endocrine diseases Myopathy in: • hyperparathyroidism (E21.0-E21.3) • hypoparathyroidism ( E20. — ) Thyrotoxic myopathy (E05. — ) G73.
6* Myopathy in metabolic disorders Myopathy in:• glycogen storage disorders (E74.0)• lipid storage disorders (E75. -) G73.7* Myopathy in other diseases classified in other headings Myopathy in:• rheumatoid arthritis (M05-M06) • scleroderma (M34.8)• Sjögren's syndrome (M35.0)• systemic lupus erythematosus (M32.1)
Excludes: autonomic nervous system disorder due to alcohol (G31.2)
G90.0 Idiopathic peripheral autonomic neuropathy. Syncope associated with irritation of the carotid sinus G90.1 Familial dysautonomia [Riley-Day] G90.2 Horner's syndrome. Bernard(-Horner) syndrome G90.3 Multisystem degeneration. Neurogenic orthostatic hypotension [Shay-Drager] Excludes: orthostatic hypotension NOS (I95.1) G90.8 Other disorders of the autonomic nervous system G90.9 Disorder of the autonomic nervous system, unspecified
G91 Hydrocephalus
Included: acquired hydrocephalus Excluded: hydrocephalus:• congenital (Q03. -)• caused by congenital toxoplasmosis (P37.1)
G91.0 Communicating hydrocephalus G91.1 Obstructive hydrocephalus G91.2 Normal pressure hydrocephalus G91.3 Post-traumatic hydrocephalus, unspecified G91.8 Other types of hydrocephalus G91.9 Hydrocephalus, unspecified
If it is necessary to identify a toxic substance, an additional external cause code (Class XX) is used.
• abortion, ectopic or molar pregnancy (O00-O07, O08.8) • pregnancy, labor or delivery (O29.2, O74.3, O89.2) • surgical and medical care (T80-T88) neonatal anoxia (P21. 9) G93.2 Benign intracranial hypertension Excluded: hypertensive encephalopathy (I67.4) G93.3 Fatigue syndrome after a viral illness.
Benign myalgic encephalomyelitisG93.4 Encephalopathy, unspecifiedExcluded: encephalopathy:• alcoholic (G31.2)• toxic (G92)G93.5 Compression of the brainCompression }Incarceration} of the brain (trunk)Excluded: traumatic compression of the brain (S06.2)• focal ( S06.3)G93.
6 Cerebral edema Excluded: cerebral edema: • due to birth trauma (P11.0) • traumatic (S06.1) G93.7 Reye's syndrome If necessary, identify an external factor, use an additional code for external causes (class XX). G93.8 Other specified brain lesions brain Radiation-induced encephalopathy If it is necessary to identify an external cause, use an additional code for external causes (Class XX). G93.9 Brain damage, unspecified
G94.0* Hydrocephalus in infectious and parasitic diseases classified in other headings (A00-B99) G94.1* Hydrocephalus in tumor diseases (C00-D48) G94.2* Hydrocephalus in other diseases classified in other headings G94.8* Others specified brain lesions in diseases classified elsewhere
Excludes: myelitis (G04.-)
G95.0 Syringomyelia and syringobulbia G95.1 Vascular myelopathies. Acute spinal cord infarction (embolic) (non-embolic). Thrombosis of the spinal cord arteries. Hepatomyelia. Non-pyogenic spinal phlebitis and thrombophlebitis. Spinal cord edema Acute necrotizing myelopathy Excluded: spinal phlebitis and thrombophlebitis, except non-pyogenic (G08) G95.
2 Spinal cord compression, unspecified G95.8 Other specified diseases of the spinal cord. “Spinal” bladder NUDMyelopathy: • drug • radiation If necessary, identify an external factor, use an additional code for external causes (class XX). Excluded: neurogenic bladder: • NOS (N31.