Hydrocephalus Hydrocephalus is an increased accumulation of cerebrospinal fluid in the cerebrospinal fluid system of the brain. Hydrocephalus accompanies many congenital and acquired neurological diseases. Clinically, it is manifested by signs of increased intracranial pressure (headache, nausea, pressure on the eyes), symptoms of compression of brain structures (vestibular ataxia, visual impairment, mental disorders, epileptic seizures) and symptoms characteristic of the disease that caused it. Diagnosis of hydrocephalus includes radiography of the skull, ophthalmological studies, echo-EG (in infants - neurosonography), MRI or CT scan of the brain. Surgical treatment of hydrocephalus allows you to correct congenital anomalies of the cerebrospinal fluid system, remove intracranial formations that disrupt the circulation of the cerebrospinal fluid, and establish the outflow of cerebrospinal fluid from the cranial cavity.
Hydrocephalus
Hydrocephalus
Hydrocephalus literally means “dropsy of the head.” In modern neurology, this is a common clinical syndrome that can be observed in many diseases, congenital anomalies or post-traumatic conditions of the brain. The occurrence of hydrocephalus is associated with certain disorders in the cerebrospinal fluid system of the brain. People of any age are susceptible to hydrocephalus. Hydrocephalus can occur in newborns, be congenital, develop in children and adults, and accompany atrophic processes occurring in the brain in old people. However, it is most often encountered in pediatric practice.
Literature
| Hydrocephalus in Wiktionary |
| Hydrocephalus at Wikimedia Commons |
- Arendt A. A. Hydrocephalus and its surgical treatment. M., 1948.
- Irger I. M. Neurosurgery. M.: Medicine, 1982.
- Kushel Yu. V. Conference “Children’s neurology and neurosurgery”.
- Romodanov A. P., Mosiychuk N. M. Neurosurgery. Kyiv: Vyshcha School, 1990.
- Hydrocephalus. Edited by Sadip Pant and Iype Cherian. InTech, February 24, 2012, 226 p. (Open access book).
- Rekate HL, The definition and classification of hydrocephalus: a personal recommendation to stimulate debate. Cerebrospinal Fluid Research 2008, 5:2doi:10.1186/1743-8454-5-2.
To improve this article it is desirable:
|
Anatomy of the cerebrospinal fluid system
Normally, cerebrospinal fluid (CSF) is produced by the choroid plexus of interconnected ventricles of the brain. The largest amount of it is formed in the lateral ventricles, from where the cerebrospinal fluid enters the third ventricle, and from it through the Sylvian aqueduct into the fourth ventricle. Then the cerebrospinal fluid enters the subarachnoid (subarachnoid) space, which extends over the entire surface of the brain, and in the caudal direction passes the region of the craniovertebral junction and then surrounds the spinal cord along its entire length. The cerebrospinal fluid located in the subarachnoid space is constantly absorbed by the arachnoid (arachnoid) membrane of the spinal cord and brain and enters the blood.
Reasons for development
In the human brain there are free spaces that are filled with cerebrospinal fluid (a special liquid). Outside the brain is the subarachnoid space, and inside is the ventricular system, cisterns and brain aqueduct.
The adult body contains from 120 to 150 ml of cerebrospinal fluid. The liquid is renewed every few hours. Its production occurs in the choroid plexuses of the brain, and absorption occurs in the veins through special villi and arachnoid cells.
Entering the cavities, the cerebrospinal fluid washes the surface of the brain from all sides, after which it is absorbed into the venous system. In a healthy person, the amount of fluid produced is equal to the amount absorbed. If any stage of this physiological process fails, hydrocephalus may develop.
Hydrocephalus can be caused by the following conditions:
- Infectious and inflammatory diseases of the central nervous system - encephalitis, meningitis, ventriculitis.
- Brain tumors.
- Acute vascular diseases of the brain - ruptured aneurysms, arteriovenous malformations, subarachnoid hemorrhages, thrombosis, strokes.
- Head injuries and their consequences.
- Encephalopathies of various origins.
- Congenital malformations of the nervous system - fusion of the foramina of Luschka or Magendie, stenosis of the cerebral aqueduct, stenosis of the cerebral venous system.
- Complications after surgical interventions include swelling and compression of the cerebrospinal fluid channels and blood vessels.
Causes of hydrocephalus
Three pathological mechanisms lead to the accumulation of an excess amount of cerebrospinal fluid in the cerebrospinal fluid system of the brain: the production of an excess amount of cerebrospinal fluid, a violation of its absorption, or a disorder of the cerebrospinal fluid circulation. Hydrocephalus may be based on one of these mechanisms or a combination of them. The causes that cause disturbances in the functioning of the cerebrospinal fluid system can act during fetal development and cause congenital hydrocephalus or affect the brain after birth and cause the appearance of so-called acquired hydrocephalus.
The causes of congenital hydrocephalus include malformations of the cerebrospinal fluid system (atresia of the foramina of Magendie and Luschka, defects in the structure of the subarachnoid space, stenosis of the Sylvian aqueduct, Dandy-Walker syndrome, etc.), craniovertebral anomalies (Chiari malformation, congenital basilar impression), intrauterine infections (toxoplasmosis , congenital syphilis, cytomegaly, rubella), birth trauma.
Acquired hydrocephalus can occur as a result of inflammatory processes in the brain and its membranes (encephalitis, arachnoiditis, meningitis), traumatic brain injury, vascular disorders (bleeding into the ventricles, hemorrhagic stroke or intracerebral hematoma with blood breaking into the ventricles). Hydrocephalus often develops against the background of a colloid cyst of the third ventricle and intracerebral tumors (astrocytomas, germinomas, ganglioneuromas, etc.), which grow into the ventricles of the brain or compress the cerebrospinal fluid pathways, thereby disrupting the normal circulation of cerebrospinal fluid and its outflow from the cranial cavity.
Separately, there is an atrophic (replacement) form of hydrocephalus, which occurs as a result of post-traumatic death or age-related atrophy of brain tissue. In this case, cerebrospinal fluid fills the space that is formed inside the skull as a result of a decrease in the volume of the brain. Atrophic hydrocephalus in old age can develop against the background of impaired blood supply to the brain due to atherosclerosis of cerebral vessels, hypertension, and diabetic macroangiopathy.
Types of dropsy
The classification of hydrocephalus of the brain is quite complex, with blurred diagnostic boundaries. Until recently, this disease belonged exclusively to children, but today it has been proven that it is possible to develop dropsy in adults.
Clinical manifestations of dropsy are divided into groups:
- The mixed form is severe, the volume of fluid increases inside and outside the brain. The prognosis is unfavorable. Violations cause epileptic seizures, convulsions, and paralysis of the limbs.
- Atrophic hydrocephalus of the head develops against the background of traumatic brain injury. The ventricles increase symmetrically, the volume of gray and white matter decreases. A month after the injury, changes become noticeable. This is a natural reaction of the body. The prognosis of the post-traumatic form of the disease is unfavorable.
- Hydrocephalus vicarious - the ventricles enlarge, but the anatomical structure of the brain does not change. The prognosis is favorable if detected at an early stage. In the vast majority of cases, the development of the disease can be stopped and the situation stabilized.
- Hypotrophic hydrocephalus develops as a reaction to a malnutrition of the brain, when soft tissues lack nutrients. A person has a headache and vestibular functions are impaired. The condition is aggravated by nausea and vomiting.
- The compensatory form appears when the acute stage of the disease has passed. The volume of fluid in the ventricles stabilizes, but their volume remains increased. There is no treatment.
- Non-occlusive form - changes do not cause hypertension. The nature of the disorders is not clear, the inflow and outflow of cerebrospinal fluid remains at the same level, the circulation of cerebrospinal fluid is within acceptable limits.
- Partial form - an increase in fluid volume causes neurological changes. A characteristic symptom of the disease is epileptic seizures.
- Discirculatory hydrocephalus - a lack of cerebral circulation is diagnosed, often accompanied by atrophic processes.
Classification of hydrocephalus
According to the etiological principle, congenital and acquired hydrocephalus are distinguished.
According to the mechanism of occurrence, hydrocephalus is classified into open and closed forms. Open hydrocephalus is associated with overproduction of cerebrospinal fluid or impaired absorption during normal cerebrospinal fluid circulation. Closed hydrocephalus is caused by a violation of the outflow of cerebrospinal fluid due to compression, partial or complete obstruction of any part of the cerebrospinal fluid system of the brain.
Depending on where the excess accumulation of cerebrospinal fluid occurs, internal and external hydrocephalus are distinguished. Internal hydrocephalus is accompanied by the accumulation of cerebrospinal fluid in the ventricles of the brain. External hydrocephalus is characterized by excess cerebrospinal fluid in the subarachnoid and subdural space.
According to the characteristics of its course, hydrocephalus is classified as acute, subacute and chronic. Acute hydrocephalus is characterized by rapid development, in which decompensation occurs a few days after the onset of the first signs of the disease. Subacute hydrocephalus develops within a month, and chronic hydrocephalus develops over six months.
Of great clinical importance is the division of hydrocephalus into stabilized (compensated) and progressive (increasing). Stabilized hydrocephalus does not grow and usually occurs with normal cerebrospinal fluid pressure. Progressive hydrocephalus is characterized by worsening symptoms, is accompanied by an increase in cerebrospinal fluid pressure, does not respond well to conservative therapy and leads to atrophy of brain tissue.
Causes
The main causes of anomaly in an adult include the following:
- Hemorrhage - may be the result of a ruptured aortic aneurysm. Also the cause is a hematoma breakthrough. As a result, blood enters the lining of the brain or into the ventricles.
- Inflammatory damage to brain structures is a consequence of neuroinfections. Systemic diseases are also provoking factors. These include encephalitis, sarcoidosis, and meningitis. Sometimes neurosyphilis is the cause of the problems.
- Tumors in the brain - they can be benign or malignant.
- Metastases to the brain.
- Traumatic brain injuries.
- Helminthic infestation – provoking factors are cysticercosis and echinococcosis.
- Vascular encephalopathy - its appearance can be caused by arterial hypertension, atherosclerosis, diabetes.
- Cystic cavities in the ventricles.
- Toxic encephalopathy is a consequence of poisoning with substances that have a toxic effect on the nervous system.
Signs of hydrocephalus in adults
The accumulation of excess cerebrospinal fluid in a limited space of the cranium leads to increased intracranial pressure, which causes the most typical symptoms of hydrocephalus. In adults and older children, these include: intense headache that cannot be relieved by analgesics, nausea, vomiting, and a feeling of pressure on the eyeballs. These symptoms may occur acutely or increase gradually, being transient at the onset of the disease. Atrophic hydrocephalus often occurs without signs of increased intracranial pressure and is detected only with additional examination of the patient.
In most cases, hydrocephalus is accompanied by neurological symptoms, which are caused both by compression of brain structures by expanded cerebrospinal fluid spaces and by the underlying disease that causes the development of hydrocephalus. The most common symptoms of hydrocephalus are vestibular and visual disturbances. The first includes vestibular ataxia, manifested by dizziness, unsteady gait, noise in the ears and head, and nystagmus. On the visual side, there may be a significant decrease in visual acuity, loss of certain areas of the visual fields, congestive optic discs; with prolonged hydrocephalus, atrophy of the optic nerves may develop.
Hydrocephalus can occur with disturbances in the motor and sensory sphere: paresis and paralysis, increased tendon reflexes and muscle tone, decreased or complete loss of all types of sensitivity, and the formation of spastic contractures of the limbs. Occlusive hydrocephalus, caused by impaired circulation of cerebrospinal fluid in the posterior cranial fossa, is characterized by symptoms of cerebellar ataxia: impaired coordination and gait, large-scale disproportionate movements, changes in handwriting, etc.
In some cases, hydrocephalus is accompanied by mental disorders, which in adults are more often manifested by disorders of the emotional-volitional sphere: emotional instability, neurasthenia, causeless euphoria with a rapid transition to a state of indifference and apathy. With a sharp increase in intracranial pressure, aggressive behavior is possible.
Principles and methods of treatment
The main method of radical treatment of cerebral hydrocephalus is surgery. During the operation, the patient is fitted with a special shunt, which allows excess cerebrospinal fluid to be drained into the bloodstream. As a result, fluid leaves the cranial cavity freely. Intracranial pressure normalizes, and the symptoms of the disease disappear.
All operations aimed at eliminating hydrocephalus can be divided into 2 large groups. The first group includes interventions with the release of cerebrospinal fluid into the vascular bed:
- installation of a shunt between the ventricles or cisterns of the brain and the abdominal cavity (this shunt is called ventriculoperitoneal);
- implantation of a shunt connecting the brain and atria;
- installation of a shunt connecting the skull with the pleural cavity;
- implantation of a tube connecting the cranial cavity to the bladder;
- connection of the peri-cerebral spaces with the venous bed.
The second group includes methods of so-called internal bypass. In this case, channels are created in the cranial cavity for the free passage of cerebrospinal fluid. These include:
- Torkildsen operation (ventriculocisternostomy) - a silicone catheter is installed between the lateral ventricles and the occipital cistern, which is passed along the occipital region under the skin.
- Endoscopic ventriculostomy of the third cerebral ventricle. With this type of intervention, the bottom of the interpeduncular cistern is dissected in the area of the gray tuberosity. As a result, a free passage for liquid is formed.
- Stenting of the Magendie and Luschka holes - installation of special expanding elements (stents).
- Plastic surgery of the aqueduct is the expansion of its lumen to ensure normal flow of cerebrospinal fluid.
- Fenestration (dissection) of the interventricular septum. This creates an opening through which cerebrospinal fluid can circulate freely.
The opinions of specialists regarding this method of treatment today are ambiguous. Even if the operation is successful, this is not a lifelong guarantee of getting rid of hydrocephalus. In children, the head can grow, the size and proportions of brain structures can change, which affects the state of the cerebrospinal fluid flow. In addition, shunts and catheters can become clogged, become infected, etc. To avoid the development of complications, it is necessary to constantly be observed and treated by a neurosurgeon, undergo regular examinations and promptly eliminate all negative changes.
Drug therapy
In some cases, surgical treatment can be replaced with conservative treatment. For this purpose, diuretics are used, which remove excess fluid from the body, thus reducing intracranial pressure. This method is suitable for the treatment of acquired forms of the disease (post-traumatic, developed against the background of inflammation or hemorrhage in the cerebral ventricles). Diuretics can also be used in complex therapy in preparation for surgery. In this case, their use is a forced emergency measure to prevent the death of the patient.
For treatment, the drugs Furosemide, Diacarb, Mannitol, Fonurit are used. The use of these medications does not eliminate the cause of the disease and is only an auxiliary measure.
If the cause of hydrocephalus is an inflammatory process, antibacterial and anti-inflammatory drugs are prescribed.
Treatment of hydrocephalus of the brain in an adult includes means to improve the trophism of brain tissue. The patient is prescribed metabolites, nootropics and vascular drugs - Actovegin, Vinpocetine, Glatilin, Cortexin, Semax, etc.
Signs of hydrocephalus in children
In children, due to the great flexibility of the skull bones, there is no increase in intracranial pressure; hydrocephalus in them is accompanied by an increase in the size of the skull. In newborns and young children, hydrocephalus is characterized by an overly large head size, bulging scalp veins, tension and lack of pulsation of the large fontanel, and swelling of the optic discs. The symptom of “setting sun” is often noted - restriction of upward movements of the eyeballs. There may be dehiscence of the sutures of the skull. Tapping on the skull is accompanied by a characteristic sound (the “cracked pot” symptom). In children in the first year of life, hydrocephalus leads to developmental delays. They later begin to hold their head up, roll over, sit up and walk.
Children who have severe hydrocephalus are distinguished by a spherical shape of the head, its too large size, deep-set eyes, protruding ears, and thinning of the scalp. There may be decreased vision, increased muscle tone in the lower extremities, and disorders of the cranial nerves. Unlike adults, in childhood hydrocephalus is often accompanied not by emotional-volitional disorders, but by intellectual deficiency. Children with hydrocephalus are usually sedentary and obese. They are apathetic, lack initiative, and do not have the attachment to relatives characteristic of their peers. A decrease in the degree of hydrocephalus often leads to an increase in the child’s intellectual abilities and activity.
In adolescence, hydrocephalus often occurs acutely against the background of an infectious disease, mental or physical trauma. At the same time, it is accompanied by intense headache, repeated vomiting, and bradycardia. There may be attacks of loss of consciousness, sometimes convulsive attacks. In some cases, episodic psychoses with hallucinatory or delusional syndrome are observed.
Symptoms of hydrocephalus
Congenital dropsy is diagnosed much less frequently than acquired dropsy. Usually, at the age of six months, pediatricians note that the baby’s head circumference and shape differ from the norm.
- The head circumference exceeds the child's chest circumference.
- The head takes on a pear-shaped shape, the elongation of the skull is visually noticeable, while the skin is expanded, the skin is thinned, the fontanel is enlarged,
- The child eats poorly, is extremely nervous, and cries often. During crying or bathing, the baby's chin and upper limbs may shake.
- Spasticity of the lower extremities, hyperreflexia and the presence of pathological reflexes.
- Epileptic seizures.
The symptoms of hydrocephalus in children over 2 years of age and adult patients are somewhat different:
- Severe headache, including nausea and vomiting. The pain intensifies when the patient changes a horizontal position to a vertical one.
- Fainting.
- An ophthalmological examination reveals a congestive optic disc.
- Memory and consciousness disorders, loss of already acquired skills, inability to learn new ones.
- Optical-spatial agnosia develops - it is difficult for a person to determine which object is closer/further, lower/higher.
Diagnosis of hydrocephalus
The clinical symptoms of hydrocephalus are usually so characteristic that they allow the neurologist to suspect its presence during the first examination of the patient. To determine the degree and form of hydrocephalus, as well as to identify the underlying disease, additional examinations are performed: radiography, ultrasound, computed tomography or magnetic resonance imaging.
X-rays of the skull in the case of hydrocephalus reveal thinning of the skull bones and divergence of the sutures between them; On the inner surface of the cranial vault, a symptom of “finger impressions” is observed. Hydrocephalus, caused by stenosis of the cerebral aqueduct, is accompanied by a decrease in the volume of the posterior cranial fossa on radiographs of the skull. Hydrocephalus with Dandy-Walker syndrome, on the contrary, is characterized by an increase in the volume of the posterior cranial fossa on craniograms. Hydrocephalus when one of the interventricular communications is closed is manifested by the asymmetry of the skull visible on the craniogram. However, in modern clinical practice, with the availability of more informative research methods, such as MRI, MSCT and CT of the brain, radiography has only an auxiliary value in the diagnosis of hydrocephalus.
Among the ultrasound diagnostic methods for hydrocephalus, echoencephalography is used, which allows one to determine the degree of increase in intracranial pressure. In children of the first year of life, ultrasound scanning of the brain through an open fontanelle using ultrasonography is possible.
An ophthalmologist assesses visual disturbances and the condition of the optic discs. As a rule, the list of ophthalmological examinations for hydrocephalus includes ophthalmoscopy, determination of visual acuity and perimetry.
Tomographic diagnostic methods make it possible to determine the nature of hydrocephalus, identify the location of cerebrospinal fluid tract occlusion or an existing congenital anomaly, and diagnose the causative disease (tumor, cyst, hematoma, etc.). In case of hydrocephalus, the most informative use of MRI of the brain.
In the absence of contraindications, to identify the causative disease, it is possible to perform a lumbar puncture followed by examination of the cerebrospinal fluid. If vascular disorders are suspected, MRA of cerebral vessels is indicated. Congenital hydrocephalus of infectious etiology requires PCR diagnostics to determine the type of infection that caused it.
Overdiagnosis
Currently, the diagnosis of “hypertensive-hydrocephalic syndrome” is one of the most common diagnoses made by pediatric neurologists. However, in most cases, overdiagnosis occurs and the child does not require any drug treatment. When making such a diagnosis, constant monitoring of the child’s development is required: first of all, it is necessary to regularly monitor both the growth of head circumference and the size of the ventricles of the brain (using neurosonography). A significant deviation in measurements should be an immediate reason for a detailed examination using MRI of the brain. However, it must be borne in mind that the fundamental factor is the dynamics of development; minor static deviations from the norm can often be due to the individual development of the child and should not cause panic. At the same time, the range of 33.0-37.5 cm is considered normal for the head circumference of a newborn. The head circumference increases most rapidly in the first 3 months (about 1.5 cm every month). Further, the growth rate decreases, and by the year the circumference is on average 44.9 - 48.9 cm).
Treatment of hydrocephalus
The choice of treatment for hydrocephalus depends on its etiology. Conservative therapy is often carried out for acquired hydrocephalus caused by inflammatory diseases, previous TBI, or hemorrhage into the ventricles. The underlying disease is treated, and diuretics (acetazolamide, furosemide) are prescribed to reduce the degree of hydrocephalus and increased intracranial pressure.
Congenital hydrocephalus usually requires surgery to correct the underlying malformation. If hydrocephalus is caused by the presence of a space-occupying process in the brain, then it can also be treated surgically. According to indications, removal of intracranial hematoma, surgery to remove tumors, opening or total excision of a brain abscess, separation of adhesions in arachnoiditis, etc. are performed.
In cases where it is not possible to eliminate the cause of hydrocephalus, shunt operations are used: cystoperitoneal shunting, endoscopic ventriculocisternostomy of the bottom of the third ventricle, ventriculoperitoneal shunting, lumboperitoneal shunting, external ventricular drainage. They are aimed at creating additional pathways for the outflow of cerebrospinal fluid from the cranial cavity. Shunt operations can be performed as an addition to surgical treatment of the underlying disease if the operation fails to restore normal circulation of the cerebrospinal fluid.
LiveJournal
Treatment
Regardless of the type of pathology, complex therapy is used. The main component is drug treatment. Folk remedies, physiotherapy and diet - auxiliary methods - 40-50% of the importance of the full course of treatment.
Medicines
The main goal of drug therapy is to eliminate the destructive processes caused by pathology. The drugs do not cure the pathology. Their combined use helps the body normalize the functionality of the brain and normalize metabolism. If conservative treatment is ineffective, surgical intervention is recommended.
Drugs to eliminate destructive processes that provoke dropsy in adults.
- Normalization of blood pressure: papalfen, clonidine, aminophylline, vincamine.
- Thinning of blood, cerebrospinal fluid: Acenocoumarol, Refludan, Fraxiparine.
- Painkillers: Ketorol, Ketorolac, Codeine; for unbearable pain - morphine, tramadol.
- Preventing liquid thickening: Dipyrylamol, Persantine, Plavix.
- Acceleration of blood circulation and enrichment of blood and brain with oxygen: Vitamins E, Pp, P1, Actovegin, Vinpocetine.
- Diuretics: Furosemide, Amiloride, Uregit.
- Anti-inflammatory: Nemisulide, Nemisil, other drugs with folic acid.
Carefully! Drugs that contain diclofenac sodium retain fluid in the body.
Surgery
Surgery is performed in 90% of cases. They operate not only if conservative methods are ineffective, but also to avoid progression of the pathology.
Indications: constant nausea, vomiting; deterioration of vision and hearing.
Contraindication – serious condition of the patient, if the possible harm exceeds the benefit.
The duration of the operation is 5-8 hours. A valve is connected to the ventricle, which opens when the internal pressure is exceeded. A tube sewn under the skin is removed. The fluid is discharged into the right region of the heart or into the abdominal cavity.
Traditional treatment
Folk remedies are used as additional treatment in combination with medications; as prevention and rehabilitation therapy.
| Product name | Properties | Description | Contraindications |
| Dill seeds | Diuretic | Removes fat and water from the body |
|
| Disinfectant | |||
| Parsley root | Strong diuretic |
|
|
| Mild anti-inflammatory | |||
| Increases immunity and potency | |||
| Bearberry | Light angioprotector | Increases the elasticity and strength of blood vessels, stimulates the secretion of digestive secretions (gastric juice, bile, pancreatin) |
|
| Moderate diuretic | |||
| Stimulation of the gastrointestinal tract and kidneys | |||
| Nettle leaves and seeds | Strong antiseptic | Stimulates wound healing, low effectiveness in tumors. | Internal suppuration if there is a risk of breakthrough into the blood; severe dropsy. |
| Removal of fluid, including pus. |
For 0.5 l. Boiling water 10 bean pods without fruit. 1 tbsp. l. Chopped nettle, 1 tsp. Nettle seeds. Boil over low heat for 10 minutes. Switch off. Let cool. Strain. Drink in 3 doses every 2 hours. Helps if dropsy is caused by infection. Not allowed at temperatures above 37.8.
For 1 liter of cold water 2 tbsp. l. Plantain, 1 tbsp. l. Dill seeds, 1 tsp. Bear ears, 0.5 tsp. Valerian root. During the boiling process, add herbs every 3 minutes in the specified sequence. After valerian – boil for 1 minute. Helps with nausea and nervous excitability.
Reference! Parsley root is brewed separately. In addition to being a diuretic, the plant effectively cleanses blood vessels. The decoction should be weak. For 200 ml of water, no more than 1 teaspoon of root.
Prices for diagnosing moderate mixed hydrocephalus
Conservative therapy for moderate mixed hydrocephalus of the brain is aimed at reducing intracranial pressure.
Neurologists at the Yusupov Hospital prescribe diuretics to patients that reduce the production of cerebrospinal fluid (diacarb, mannitol, mannitol and diacarb in combination with lasix or furosemide), drugs that improve brain trophism (cavinton, pantogam, actovegin, cerebrolysin), vitamin and mineral complexes. With the progression of hydrocephalus symptoms, the only treatment method to improve the quality of life of patients is surgery. If there is a formation that impedes the outflow of cerebrospinal fluid (tumor, intracranial hematoma), it is removed, and the adhesions are separated during surgery.
To create additional outflow pathways for mixed non-occlusive hydrocephalus, neurosurgeons perform shunt operations:
- cystoperitoneal shunting;
- ventriculoperitoneal shunt;
- lumboperitoneal shunt;
- external ventricular drainage.
Shunts are replaced as needed, as they can become clogged, rejected, and become small. An alternative treatment for obstructive hydrocephalus in selected patients is endoscopic ventriculostomy of the third ventricle. The operation is performed using a neuroendoscope equipped with a miniature television camera.
To restore neurological functions, rehabilitation specialists at the Yusupov Hospital use innovative techniques of massage and physical therapy. Selective acupressure massage of the arms and legs, torso, scalp and face, paravertebral points, back and pelvis increases muscle tone. Therapeutic physical culture is aimed at regulating muscle tone, developing normal reflex motor activity, improving blood circulation and metabolism, and increasing the body's reactivity.
Patients undergo a course of acupuncture and manual therapy. They help reduce muscle spasms, improve blood flow, and temporarily relieve pain. Psychologists work with patients who have developed cognitive impairment. Psychotherapists help them restore self-care skills and carry out social adaptation.
Make an appointment with a neurologist by calling the Yusupov Hospital. Timely treatment of moderate mixed hydrocephalus of the brain can stop the progression of the disease. After surgery, patients can return to their normal lifestyle.
Head of the Department of Rehabilitation Medicine – physical therapy doctor, neurologist, reflexologist
Atrophic hydrocephalus develops against the background of the following diseases:
- tumors of the ventricles and brain matter;
- toxic and alcoholic encephalopathies;
- infectious brain lesions (ventriculitis, encephalitis, meningitis);
- vascular cerebral pathology, including rupture of an aneurysm and intraventricular and subarachnoid cerebral hemorrhages resulting from defects in arteriovenous connections;
- pathologies of the development of the nervous system (Dandy-Walker syndrome, stenosis of the Sylvian aqueduct);
- post-traumatic conditions and brain injuries.
In atrophic encephalopathy, cerebrospinal fluid fills the space formed inside the skull as a result of a decrease in brain volume. Atrophic hydrocephalus of the brain in elderly and senile people can develop against the background of impaired blood supply to the brain due to arterial hypertension, atherosclerosis of cerebral vessels, and diabetic angiopathy.
For a long time, patients may not notice signs of replacement hydrocephalus. Computed tomography or magnetic resonance imaging allows you to establish the correct diagnosis. These research methods at the Yusupov Hospital are used by all patients immediately after hospitalization at the neurology clinic.
In the presence of subacute and acute occlusive hydrocephalus of the brain, patients feel a bursting headache, which is accompanied by nausea and vomiting, which brings relief. There is a feeling of pressure on the eyeballs, a feeling of “sand” in the eyes, a burning sensation in the eyeballs.
Patients experience a feeling of “fog” before the eyes, and vision deteriorates. In the fundus, ophthalmologists identify congested optic discs. If the patient does not promptly seek qualified medical help, then an increase in the amount of cerebrospinal fluid leads to the appearance of dislocation syndrome, which threatens the patient’s life.
Depression of consciousness rapidly increases, paresis of upward gaze develops, depression of reflexes, divergent strabismus develops, and coma develops. These symptoms appear when the midbrain is compressed. In the case of compression of the medulla oblongata, the voice changes, swallowing is impaired, respiratory and cardiac activity are depressed, which can lead to death.
With chronic internal hydrocephalus of the brain in adults, intracranial pressure may be normal or slightly increased. Initially, the sleep cycle is disrupted, drowsiness or insomnia appears. Patients complain of fatigue, lethargy, and memory impairment. As the disease progresses, cognitive impairment, including dementia, develops. Patients behave inappropriately and lose the ability to self-care.
Walking is impaired, the gait becomes unstable and slow. Over time, difficulty arises when starting to move, and uncertainty in a standing position. The patient can imitate cycling or walking in a sitting or lying state, but in an upright state he loses this ability.
The gait becomes “magnetic”: the person seems to be glued to the floor, and, leaving his place, takes short shuffling steps on widely spaced legs. Neurologists determine an increase in muscle tone; in severe stages of the disease, paresis of the lower extremities appears and muscle strength decreases. Balance disorders may progress and the patient may become unable to sit or stand independently over time.
Subsequently, urination becomes more frequent, especially at night. There is an urge to urinate, requiring immediate emptying of the bladder. Over time, urinary incontinence develops. Neurologists at the Yusupov Hospital use the following methods for diagnosing atrophic hydrocephalus:
- magnetic resonance or computed tomography, which allows you to determine the size and shape of the cisterns of the brain, ventricles and subarachnoid space;
- radiography of the tanks, with the help of which the type of hydrocephalus is clarified and the direction of the cerebrospinal fluid flow is determined;
- diagnostic test spinal puncture with collection of 40-55 ml of cerebrospinal fluid, accompanied by a short-term improvement in the patient’s condition;
- ultrasound examination of cerebral vessels to determine the state of arterial and venous blood flow.
After analyzing the results of a comprehensive study, individual treatment is prescribed. The tactics for managing patients with severe hydrocephalus are developed at a meeting of the expert council with the participation of professors and doctors of the highest category. Neurosurgeons determine indications for surgical intervention.
For increased intracranial pressure, neurologists at the Yusupov Hospital prescribe diuretics. Mannitol, mannitol and diacarb in combination with furosemide or lasix have a diuretic effect. To prevent hypokalemia, they are used simultaneously with asparkam or panangin.
To improve the nutrition of brain tissue, Actovegin, Cavinton choline, gliatilin, Cerebrolysin, Cortexin, Memoplant, Semax are prescribed. These drugs have a nootropic effect. In case of severe atrophic hydrocephalus, neurosurgeons at partner clinics perform surgical interventions.
If the patient's condition is life-threatening, craniotomy is performed and external drains are installed to allow excess fluid to escape. Medicines are administered through the drainage system. Such an operation for hydrocephalus of the brain is traumatic.
Endoscopic ventriculocisternostomy of the ventricular fundus is a minimally invasive surgical procedure. Neurosurgeons insert a microscopic surgical instrument with a camera at the end into the ventricles of the brain, which makes it possible to monitor all procedures. An additional hole is made at the bottom of the ventricle, which is connected to the cisterns of the brain. The operation allows you to eliminate the cause of the disease and normalize the physiological flow of cerebrospinal fluid between the cisterns and ventricles.
Atrophic hydrocephalus of the brain in adults is a dangerous disease that leads to irreversible changes in the substance of the brain. At the slightest suspicion of hydrocephalus, call the Yusupov Hospital. After the examination, neurologists will prescribe treatment to slow the progression of hydrocephalus symptoms.
Psychotherapist, doctor of the highest category
In addition to the fact that each type of disease is characterized by unique causes of formation, there are common development factors:
- any infectious damage affecting the brain, including: encephalitis, tuberculosis, meningitis;
- subarachnoid hemorrhage;
- head and cervical injuries;
- —strokes—various types, the most dangerous is hemorrhagic;
- brain stem tumors;
- long-term alcohol intoxication, especially when drinking low-quality drinks;
- spinal injuries and compression of the cerebrospinal canals as a result of edema;
- purulent infectious processes in the brain.
Separately, we can note the causes of moderate external hydrocephalus of the replacement type: metabolic problems, senile or vascular encephalopathy, diabetes, atherosclerosis or multiple sclerosis.
Three pathological mechanisms lead to the accumulation of an excess amount of cerebrospinal fluid in the cerebrospinal fluid system of the brain: the production of an excess amount of cerebrospinal fluid, a violation of its absorption, or a disorder of the cerebrospinal fluid circulation. Hydrocephalus may be based on one of these mechanisms or a combination of them. The causes that cause disturbances in the functioning of the cerebrospinal fluid system can act during fetal development and cause congenital hydrocephalus or affect the brain after birth and cause the appearance of so-called acquired hydrocephalus. Causes of hydrocephalus include:
1. Congenital hydrocephalus:
2. Acquired hydrocephalus:
Separately, there is an atrophic (replacement) form of hydrocephalus, which occurs as a result of post-traumatic death or age-related atrophy of brain tissue. In this case, cerebrospinal fluid fills the space that is formed inside the skull as a result of a decrease in the volume of the brain. Atrophic hydrocephalus in old age can develop against the background of impaired blood supply to the brain due to atherosclerosis of cerebral vessels, hypertension, and diabetic macroangiopathy.
Hydrocephalus in adults
The accumulation of excess cerebrospinal fluid in a limited space of the cranium leads to increased intracranial pressure, which causes the most typical symptoms of hydrocephalus.
In adults and older children, these include: intense headache that cannot be relieved by analgesics, nausea, vomiting, and a feeling of pressure on the eyeballs. These symptoms may occur acutely or increase gradually, being transient at the onset of the disease. Atrophic hydrocephalus often occurs without signs of increased intracranial pressure and is detected only with additional examination of the patient. In most cases, hydrocephalus is accompanied by neurological symptoms, which are caused both by compression of brain structures by expanded cerebrospinal fluid spaces and by the underlying disease that causes the development of hydrocephalus. The most common symptoms of hydrocephalus are vestibular and visual disturbances. The first includes vestibular ataxia, manifested by dizziness, unsteady gait, noise in the ears and head, and nystagmus. On the visual side, there may be a significant decrease in visual acuity, loss of certain areas of the visual fields, congestive optic discs; with prolonged hydrocephalus, atrophy of the optic nerves may develop.
Hydrocephalus can occur with disturbances in the motor and sensory sphere: paresis and paralysis, increased tendon reflexes and muscle tone, decreased or complete loss of all types of sensitivity, and the formation of spastic contractures of the limbs. Occlusive hydrocephalus, caused by impaired circulation of cerebrospinal fluid in the posterior cranial fossa, is characterized by symptoms of cerebellar ataxia: impaired coordination and gait, large-scale disproportionate movements, changes in handwriting, etc.
In some cases, hydrocephalus is accompanied by mental disorders, which in adults are more often manifested by disorders of the emotional-volitional sphere: emotional instability, neurasthenia, causeless euphoria with a rapid transition to a state of indifference and apathy. With a sharp increase in intracranial pressure, aggressive behavior is possible.
Hydrocephalus in children
In children, due to the great flexibility of the skull bones, there is no increase in intracranial pressure; hydrocephalus in them is accompanied by an increase in the size of the skull. In newborns and young children, hydrocephalus is characterized by an overly large head size, bulging scalp veins, tension and lack of pulsation of the large fontanel, and swelling of the optic discs.
The symptom of “setting sun” is often noted - restriction of upward movements of the eyeballs. There may be dehiscence of the sutures of the skull. Tapping on the skull is accompanied by a characteristic sound (the “cracked pot” symptom). In children in the first year of life, hydrocephalus leads to developmental delays. They later begin to hold their head up, roll over, sit up and walk.
Children who have severe hydrocephalus are distinguished by a spherical shape of the head, its too large size, deep-set eyes, protruding ears, and thinning of the scalp. There may be decreased vision, increased muscle tone in the lower extremities, and disorders of the cranial nerves. Unlike adults, in childhood hydrocephalus is often accompanied not by emotional-volitional disorders, but by intellectual deficiency.
Children with hydrocephalus are usually sedentary and obese. They are apathetic, lack initiative, and do not have the attachment to relatives characteristic of their peers. A decrease in the degree of hydrocephalus often leads to an increase in the child’s intellectual abilities and activity.
In adolescence, hydrocephalus often occurs acutely against the background of an infectious disease, mental or physical trauma. At the same time, it is accompanied by intense headache, repeated vomiting, and bradycardia. There may be attacks of loss of consciousness, sometimes convulsive attacks. In some cases, episodic psychoses with hallucinatory or delusional syndrome are observed.
The clinical symptoms of hydrocephalus are usually so characteristic that they allow the neurologist to suspect its presence during the first examination of the patient. To determine the degree and form of hydrocephalus, as well as to identify the underlying disease, additional examinations are carried out:
- X-ray. X-rays of the skull reveal thinning of the skull bones and divergence of the sutures between them; On the inner surface of the cranial vault, a symptom of “finger impressions” is observed. Hydrocephalus, caused by stenosis of the cerebral aqueduct, is accompanied by a decrease in the volume of the posterior cranial fossa on radiographs of the skull. Hydrocephalus with Dandy-Walker syndrome, on the contrary, is characterized by an increase in the volume of the posterior cranial fossa on craniograms. Hydrocephalus when one of the interventricular communications is closed is manifested by the asymmetry of the skull visible on the craniogram.
- Computed tomography or MRI. Tomographic diagnostic methods make it possible to determine the nature of hydrocephalus, identify the location of cerebrospinal fluid tract occlusion or an existing congenital anomaly, and diagnose the causative disease (tumor, cyst, hematoma, etc.). In case of hydrocephalus, the most informative use of MRI of the brain. If vascular disorders are suspected, MRA of cerebral vessels is indicated.
- Echography. Among the ultrasound diagnostic methods for hydrocephalus, echoencephalography is used, which allows one to determine the degree of increase in intracranial pressure. In children of the first year of life, ultrasound scanning of the brain through an open fontanelle using ultrasonography is possible.
- Consultation with an ophthalmologist. An ophthalmologist assesses visual disturbances and the condition of the optic discs. As a rule, the list of ophthalmological examinations for hydrocephalus includes ophthalmoscopy, determination of visual acuity and perimetry.
- Lumbar puncture. In the absence of contraindications, to identify the causative disease, it is possible to perform a lumbar puncture followed by examination of the cerebrospinal fluid. Congenital hydrocephalus of infectious etiology requires PCR diagnostics to determine the type of infection that caused it.
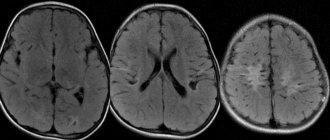
MRI of the brain. Pronounced expansion of the lateral ventricles of an occlusive nature.
The choice of treatment for hydrocephalus depends on its etiology. Conservative therapy is often carried out for acquired hydrocephalus caused by inflammatory diseases, previous TBI, or hemorrhage into the ventricles. The underlying disease is treated, and diuretics (acetazolamide, furosemide) are prescribed to reduce the degree of hydrocephalus and increased intracranial pressure.
Congenital hydrocephalus usually requires surgery to correct the underlying malformation. If hydrocephalus is caused by the presence of a space-occupying process in the brain, then it can also be treated surgically. According to indications, removal of intracranial hematoma, surgery to remove tumors, opening or total excision of a brain abscess, separation of adhesions in arachnoiditis, etc. are performed.
In cases where it is not possible to eliminate the cause of hydrocephalus, shunt operations are used:
They are aimed at creating additional pathways for the outflow of cerebrospinal fluid from the cranial cavity. Shunt operations can be performed as an addition to surgical treatment of the underlying disease if the operation fails to restore normal circulation of the cerebrospinal fluid.
Hydrocephalus: diagnosis and treatment methods
Diagnosis of hydrocephalus is usually not difficult. The congenital form of this disease can be detected using ultrasound even at the stage of intrauterine development. Other diagnostic methods include:
- diaphanoscopy;
- neurosonography;
- craniography;
- CT scan;
- Magnetic resonance imaging.
This is not a complete list of methods used to diagnose hydrocephalus. It can be supplemented by echoencephalography, electroencephalography, lumbar puncture, and so on.
The primary treatment method is dehydration therapy. It is aimed at reducing the production of cerebrospinal fluid and reducing ICP. If hydrocephalus continues to progress, the issue of surgical intervention is decided.
In 2020, scientists from Kazan State Medical University published the results of a study aimed at analyzing the effectiveness of treating hydrocephalus in children using valve shunt systems. As a result, it was found that every second patient required shunt revision, and in half of them, dysfunction occurred within 1 year after shunt implantation. It is worth noting that these figures include data on the results of bypass surgery at the end of the last century: the study was conducted retrospectively with an analysis of experience over the past 20 years. Also, when interpreting the information, you need to know that some patients needed to replace the catheter due to the growth of the child, and in 1.6%, during the audit, shunt independence was identified, allowing the device to be removed.
Photos used from Shutterstock
Used sources
Experience of implantation of cerebrospinal fluid shunt systems in children with hydrocephalus / Danilov V.I., Ivanov V.S., Filatov V.S. et al. // Practical Medicine. — 2020. — No. 7
Hydrocephalus in children / Bogadelnikov I.V., Zdyrko E.V., Kruger E.A. // Child’s health. — 2011. — No. 5
Hydrocephalus (Pathogenesis, diagnosis, surgical treatment) / Khachatryan V.A. // St. Petersburg: Publishing house PHXI named after. prof. A.L. Polenova. — 1998