Multiple sclerosis
This is the most common pathology among demyelinating diseases of the central nervous system;
Around the world, approximately 2.1 million people have multiple sclerosis. The incidence of multiple sclerosis ranges from 2 to 150 patients per 10,000 people, depending on the region. Etiopathogenesis
It is believed that MS is an autoimmune disease that affects people with a genetic predisposition under the influence of external factors. The damage occurs when the body's immune system attacks the structures of its own nervous system. Typically, lesions are localized in the white matter of the brain, periventricularly, in the brainstem, basal ganglia and spinal cord, and often affect the optic nerves.
In MS, oligodendrocytes, the cells that form myelin, are affected. Parallel to the demyelinating process, an inflammatory reaction occurs, in which T lymphocytes participate, crossing the blood-brain barrier. T lymphocytes attack myelin - this is a trigger that starts an inflammatory reaction, which includes many cytokines and antibodies. It has been proven that, in parallel with T lymphocytes, B lymphocytes participate in the pathological reaction.
Diagnostics
Diagnosis of the disease is relatively difficult due to the fact that the symptoms are similar to other diseases. Diagnostic criteria (McDonald criteria) were developed and revised in 2010. The criteria are based on clinical presentation, laboratory and radiological data.
Radiological criteria for the disease are based on the spread of the process in space and dynamics, therefore, it is not always possible to establish a diagnosis at one point, sometimes it is even necessary to perform repeated MRIs. In the cerebrospinal fluid punctate, oligoclonal antibodies (IgG) can be detected, which indicate a chronic inflammatory process. Oligoclonal antibodies are found in the blood of 85% of patients with MS.
Clinical picture
Symptoms in MS depend on the location of lesions in the central nervous system. Classic symptoms include internuclear ophthalmoplegia, Lhermitte's symptom, conduction-type sensory disturbances, pyramidal symptoms, neurogenic bladder, optic neuritis. The onset of symptoms is unpredictable and generally ranges from 24 hours or more. Typically, symptoms reduce slowly, and remissions may not be complete. Any infection can provoke pseudo-relapse.
There is a clinical classification of the course of multiple sclerosis. Based on it, treatment is prescribed.
RS is divided into:
- relapsing-remitting course - exacerbations with complete/partial remission, between exacerbations a stable course (50% within 10 years turn into a secondary progressive form);
- Secondarily progressive course - initially a relapsing remitting course, followed by a steadily progressive worsening of symptoms, with or without exacerbations;
- Primary progressive course – up to 15% of patients, without remissions, starting from the first symptom;
Treatment
MS is not a curable disease.
A distinction is made between treatment of acute episodes, immunomodulatory therapy, symptomatic treatment and rehabilitation.
Treatment is aimed at reducing inflammatory and demyelinating processes, delaying the next relapse and slowing the progression of disability.
To treat exacerbations, use methylprednisolone 1000 mg / 3-5 day course, depending on the severity of the exacerbation. In some cases, when methylprednisolone does not provide a therapeutic effect, plasmapheresis is used.
For the purpose of immunomodulatory therapy, medications are used that reduce the frequency of relapses in the case of relapsing-remitting disease. This group of medications includes: Interferon beta 1a (Avonex, Rebif); Interferon beta 1b (Betaferon, Extavia); glatiramer acetate (Copaxone);
There are certain criteria, according to which, by decision of the council, the patient can receive drug treatment paid for by the state.
Like all other medications, these medications have their own side effects, which may cause the patient to refuse to take them.
Treatment of MS is a team effort, in which a neurologist, neuroradiologist, neuro-ophthalmologist and rehabilitation specialist should participate.
Sclerosis multiplex cerebrospinalis (multiple cerebrospinal sclerosis, multiple sclerosis) is a chronic demyelinating disease in which the human immune system attacks the central nervous system. In our geographical conditions it is a fairly common disease. MS affects about 60-100/100,000 (and even more) people, especially young and middle-aged people.
Sometimes it can develop in contrast - in a child (MRI shows manifestations of incomplete myelination) or, conversely, in old age. The disease most often manifests itself between 20 and 40 years of age and affects more women (the ratio of women to men is 2:1). The exact cause of demyelinating disease is still unclear, but MS is currently considered a chronic inflammatory autoimmune disorder with origins in a disorder of cellular immunity. The development of demyelinating disease is influenced by several factors - genetic, environmental.
Symptoms
Multiple sclerosis is unpredictable and manifests itself individually in each person. In milder forms, symptoms may disappear over time. In other cases, demyelinating disease attacks quickly, leaving permanent effects. The predominant clinical signs depend on the location of the foci of demyelination in the brain. At the onset of the disease, the following clinical picture appears:
- Optic retrobulbar neuritis is a unilateral visual disorder that usually corrects quickly and completely. Sometimes a central scotoma (a place on the retina that is physiologically unresponsive to incident light, also known as a blind spot) remains.
- Sensitive symptoms are mainly paraesthesia (an unpleasant sensation of tingling, itching, burning of the skin without lasting effects) in the upper and lower extremities, mostly asymmetrical. Weakness or numbness in one or more limbs is the first sign of this disease in about half of patients. In younger patients, trigeminal neuralgia may be a secondary symptom.
- Vestibular syndrome (imbalance of the vestibular apparatus) - mainly central, sometimes with severe dizziness. Nystagmus (oscillatory movement of the eye bulbs) is common even without subjective vestibular symptoms. Frequent symptoms are diplopia (double vision) and internuclear ophthalmoplegia (damage to the cervical - occipital nerves). Sometimes MS can begin with a picture of acute disseminated encephalitis (acute inflammation of the brain).
- Spastic motor symptoms - at the onset of the disease there is no pronounced paralysis or spasticity (increased tension in muscle fibers with more or less frequent muscle twitching). Symptoms are accompanied by increased fatigue, uncertainty in walking, weakness, and clumsiness. During the examination, hyperreflexia (increased reflexes) with spasmodic pyramidal phenomena is detected, often - muted abdominal reflexes.
- Cerebellar disorders are a common brain symptom, ranging in intensity from mild ataxia (impaired motor coordination) of one limb to severe gait ataxia, balance problems that may also be associated with spinal ataxia (balance problems worse in the dark and with eyes closed).
- Disorders of the sphincters, especially the urethra, frequent urge to urinate, which must be done immediately (bladder has low capacity, often contracts when contents accumulate). Later, urinary retention or incontinence is added. Sexual dysfunction (impotence) may also occur.
- Mental symptoms – affectivity, depressive syndromes, euphoria. Intelligence is not damaged. Fatigue is common.
Other manifestations are very varied. There are different variants of a dangerous malignant form, in which the patient is bedridden for several years. Death may occur. In benign forms, the patient is mobile for many years and has only minor symptoms. However, in most cases, the dynamics progressively decrease over several years, and spastic and cerebellar symptoms with severe ataxia, deliberate tremor, and combined spastic-ataxic manifestations may predominate.
What is the demyelinating process?
Some nerve endings (in particular, axons of the peripheral and central nervous systems) are covered with a specific myelin sheath.
This structure performs a number of important functions. In particular, myelin is responsible for the speed of transmission of electrical impulses along nerve fibers. In addition, the membrane performs barrier and support functions, and is also responsible for nourishing nerve endings. Demyelinating brain disease is accompanied by some damage to the myelin sheath, which naturally affects the functioning of nerve cells. By the way, demyelinating diseases are a whole group of certain lesions of the nervous system, each of which has its own characteristics and is accompanied by a unique set of symptoms.
In fact, there are many diseases that are in one way or another associated with the process of damage to myelin fibers. For example, Devic's disease is considered to be quite specific, which is accompanied by inflammation and demyelination of the optic nerves and some segments of the spinal cord.
Chronic diseases also include atrophic lateral sclerosis, which most often manifests itself in adulthood. The list of diseases can be supplemented with such pathologies as acute encephalomyelitis, Krabbe disease, periaxial encephalitis, also Balo’s concentric sclerosis (more common in young people), Marburg’s sclerosis and many others.
In fact, there are many diseases that are in one way or another associated with the process of damage to myelin fibers. For example, Devic's disease is considered to be quite specific, which is accompanied by inflammation and demyelination of the optic nerves and some segments of the spinal cord.
The classification of this disease is based on identifying the root cause of the disease:
- If myelin in the body is destroyed for hereditary reasons, they speak of myelinoclasty.
- If the membrane is produced and functions correctly, but then disappears due to the action of external factors, they speak of myelinopathy.
In addition, there are main diseases that are included in the concept of “demyelinating disease of the central nervous system”:
- The most common pathology of this kind, multiple sclerosis, affects all parts of the central nervous system. The characteristic symptoms are very varied.
- Progressive multifocal leukoencephalopathy.
- Marburg's disease.
- Acute disseminated encephalomyelitis.
- Devic's disease.
Demyelinating process of the brain is a disease in which the sheath of the nerve fiber atrophies. In this case, neural connections are destroyed and the conductive functions of the brain are disrupted.
It is customary to refer to pathological processes of this type as multiple sclerosis, Alexander disease, encephalitis, polyradiculoneuritis, panencephalitis and other diseases.
The causes of demyelination are still not fully understood. Modern medicine makes it possible to identify three main catalysts that increase the risk of developing disorders.
It is believed that demyelination occurs as a consequence of:
Genetic factor - the disease develops against the background of inherited diseases. Pathological disorders occur against the background of aminoaciduria, leukodystrophy, etc.
- Acquired factor - the myelin sheaths are damaged due to inflammatory diseases caused by an infection that has entered the blood. May be a consequence of vaccination. Less commonly, pathological changes cause injury; demyelination is also observed after tumor removal.
- Against the background of diseases, disruption of the structure of nerve fibers, especially the myelin sheath, occurs as a consequence of acute transverse myelitis, diffuse and multiple sclerosis. Metabolic problems, deficiency of certain vitamins, myelinosis and other conditions are catalysts for damage.
The following symptoms are typical for violations:
- Increased and chronic fatigue.
Fine motor skills disorders – tremor, loss of sensation in the limbs of the hands.
- Problems in the functioning of internal organs – the pelvic organs often suffer. The patient experiences fecal incontinence and voluntary urination.
- Psycho-emotional disorders are multifocal brain damage of a demyelinating nature, often accompanied by problems in the patient’s mental state: forgetfulness, hallucinations, and decreased intellectual abilities. Until precise instrumental methods began to be used for diagnosis, there were cases when patients began to be treated for dementia and other psychological pathologies.
- Neurological disorders - focal changes in the substance of the brain of a demyelinating nature are manifested in disturbances in the motor functions of the body and motility, paresis, and epileptic seizures. Symptoms depend on which part of the brain is damaged.
Foci of demyelination in the cerebral cortex, white and gray matter lead to the loss of important body functions. Depending on the location of the lesions, specific manifestations and disorders are observed.
The prognosis of the disease is unfavorable. Often, demyelination, which appears as a result of secondary factors: surgery and or inflammation, develops into a chronic form. As the disease develops, gradually progressive atrophy of muscle tissue, paralysis of the limbs and loss of essential body functions are observed.
Single foci of demyelination in the white matter of the brain are prone to proliferation. As a result of a gradually progressing disease, a condition may occur in which the patient will not be able to swallow, speak, or breathe independently. The most severe manifestation of damage to the nerve fiber sheath is death.
What is demyelination? The process develops as a result of the negative impact of antibody proteins on nervous tissue. This is accompanied by the development of an inflammatory reaction, damage to neurons, destruction of the myelin sheath and disruption of the transmission of nerve impulses.
The sheaths of nerve fibers are damaged under the influence of:
- Hereditary predisposition.
- Infectious viral diseases.
- Chronic foci of bacterial infection.
- Poisoning with heavy metals, gasoline, solvent.
- Severe and prolonged stress.
- Excessive consumption of animal proteins and fats.
- Unfavorable environmental situation.
All these unfavorable conditions lead to the development of an autoimmune process, but genetic predisposition plays the greatest role. Certain genes and their mutation lead to the production of abnormal antibodies that penetrate the barrier between the blood and nerve tissue that protects the brain from damage. As a result, the myelin protein is destroyed under the influence of the inflammatory process.
The second provoking factor is infectious diseases. The destruction of normal myelin occurs in a slightly different way. Normally, the immune system, after an infection enters the body, begins to produce antibodies to fight it. But sometimes the proteins of the pathogen are so similar to the proteins in the tissues of the human body that the antibodies confuse them and, together with the bacteria, destroy their own cells.
At the initial stages of damage to nerve fibers, when the inflammatory autoimmune process has just begun to develop, pathological changes can still be reversed. There is a chance for partial restoration of myelin, which will allow neurons to perform a certain part of their functions. But as the disease progresses, the nerve sheaths are destroyed more and more, nerve fibers are exposed, and they lose the ability to transmit signals. It is impossible to get rid of the nervous deficit and restore lost functions to the brain at this stage.
It is difficult to determine the type of demyelination based on symptoms alone. Therefore, additional examinations are necessary. Manifestations depend on the form of pathological changes.
Multiple sclerosis
Foci of demyelination of the brain are most often found in multiple sclerosis. The disease is accompanied by autoimmunization, damage to nerve fibers, breakdown of myelin sheaths and replacement of damaged areas with connective tissue.
It has not yet been possible to fully determine the causes of the violations. It is believed that the brain is most affected by poor heredity, external conditions, infection with viruses and bacteria. The brain and spinal cord are usually affected.
Pathology can manifest itself:
- paresis and paralysis, increased tendon reflexes, muscle cramps;
- impaired balance and fine motor skills;
- weakening of the facial muscles, swallowing reflex, speech function;
- change in sensitivity;
- impotence, constipation, incontinence or urinary retention;
- decreased vision, narrowing of its fields, impaired brightness and color perception.
Marburg disease
This is the most dangerous form of brain damage. The pathology occurs abruptly and is accompanied by a rapid increase in symptoms. This affects the patient's condition in the most negative way. A person can die in a matter of months.
The disease initially resembles an infection and is accompanied by fever and convulsions. With the destruction of myelin, motor functions, sensitivity and consciousness are impaired. Characterized by the appearance of severe pain in the head and vomiting, increased intracranial pressure. In a malignant course, the brain stem, in which the nuclei of the cranial nerves are collected, is affected.
Devic's disease
This causes damage to the optic nerves and spinal cord. Acute development of the pathological process leads to complete blindness. Due to the fact that the disease affects the spinal cord, a person suffers from paresis, paralysis, dysfunction of the pelvic organs, and sensitivity disorders.
The essence of pathology
Most people don't know what it is, what brain demyelination is. However, demyelinating diseases of the nervous system occur in both children and adults. Interestingly, the frequency of their occurrence is related to geographic location and race: the largest number of patients with this diagnosis are Caucasians and are observed in Europe and America.
Neurons have a specific shape that distinguishes them from all other types of cells. They have very long processes, some of which are covered with a myelin sheath, which allows the transmission of nerve impulses and makes this process faster. If the myelin is destroyed, the process will either not be able to communicate with other neurons through electrophysiological impulses at all, or this process will be extremely difficult.
Subsequently, the structure of the human body whose innervation is connected with the damaged nerve will suffer. This means that the disappearance of the myelin sheath can have a wide variety of symptoms and consequences. Patients with similar diagnoses, but different localization of the pathological focus can live for different amounts of time; the prognosis depends on the importance of the affected structure.
The immune system plays a very important role in the destruction of the membrane, suddenly attacking the living structures of the body.
In many cases, this is explained by the fact that the immune system reacts very violently to infectious pathogens located in the medulla, and at the same time to the structural components of the central nervous system; a so-called autoimmune reaction develops. But there are other, non-infectious reasons for such failures.
Causes and mechanisms of demyelination
In the human body, the nervous system is formed of two sections - central (brain and spinal cord) and peripheral (numerous nerve branches and nodes).
A well-functioning regulatory mechanism works in this way: the impulse generated in the receptors of the peripheral system under the influence of external factors is transmitted to the nerve centers of the spinal cord, from where they are sent to the nerve centers of the brain. The normal functioning of the entire body largely depends on the speed and quality of transmission of electrical signals along nerve fibers, both in the ascending and descending directions. To provide electrical insulation, the axons of most neurons are covered with a lipid-protein myelin sheath. It is formed by glial cells, and in the peripheral part - from Schwann cells, and in the central nervous system - from oligodendrocytes.
In addition to its electrical insulating functions, the myelin sheath provides an increased speed of impulse transmission due to the presence of nodes of Ranvier in it for the circulation of ionic current. Ultimately, the speed of signal transmission in myelinated fibers increases 7-9 times.
Diagnostics
Based on clinical symptoms alone, a doctor will not be able to determine an accurate diagnosis, much less choose the right treatment. Therefore, diagnostic studies are needed that allow us to identify pathological processes occurring in the brain.
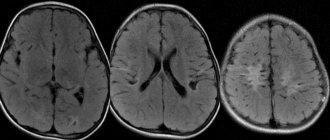
- Magnetic resonance imaging is very informative. It makes it possible to see whether there are single or multiple lesions and their location. Very often, MRI images show changes in the frontal lobes, localized periventricularly or subcortically.
- Electroneuromyography allows not only to determine the localization of lesions, but also the degree of decay of the nerve structure.
- Recently, a method of evoked potentials has been developed that allows one to evaluate the process of conducting nerve impulses by recording the electrical activity of brain structures.
The demyelinating process of the brain requires a careful diagnosis:
- MRI - magnetic tomography shows hypersignal lesions in the white matter of the brain and spinal cord on T2 images and hyposignal lesions on T1 (the number correlates with the severity of the disease);
- examination of cerebrospinal fluid - intrathecal synthesis of IgG, the presence of at least 2 oligoclonal bands in the alkaline part of the spectrum not present in serum, pleocytosis of mononuclear cells (up to 100/3), prevalence of lymphocytes;
- study of evoked potentials (visual and somatosensory) – increase in wave latency;
- ophthalmological examination (in the case of retrobulbar neuritis) - in the acute stage there is swelling of the papilla, later - its temporary fading (manifestation of atrophy);
- histology - indicates the presence of inflammatory changes in the head, dystrophic processes, neuronal degeneration (gliosis).
On the way to diagnosis
The symptoms of demyelination are extremely varied and depend on the location of the lesion, the characteristics of the course of a particular disease, and the rate of progression of symptoms. Typically, the patient experiences neurological impairment, which is often transient. The first symptoms may be visual disturbances.
When the patient feels that something wrong is happening, but it is no longer possible to justify the changes with fatigue or stress, he goes to the doctor. It is extremely problematic to suspect a specific type of demyelinating process only based on the clinic, and the presence of demyelination itself is not always clear to a specialist, so additional research is indispensable.
This is interesting: How to prepare anti-wrinkle cream at home - basic rules
example of demyelination foci in multiple sclerosis
MRI is traditionally considered the main and very informative way to diagnose the demyelinating process. This method is harmless, can be used for patients of different ages, pregnant women, and contraindications include excessive weight, fear of closed spaces, the presence of metal structures that react to a strong magnetic field, and mental illness.
Round or oval hyperintense foci of demyelination on MRI are found predominantly in the white matter under the cortex, around the ventricles of the brain (periventricular), diffusely scattered, and have different sizes - from a few millimeters to 2-3 cm. To clarify the time of formation of foci, contrast enhancement is used, with In this case, “younger” fields of demyelination accumulate contrast agent better than those that have existed for a long time.
The main task of a neurologist when detecting demyelination is to determine the specific form of pathology and choose the appropriate treatment. The prognosis is ambiguous. For example, with multiple sclerosis, you can live a dozen or more years, while with other types, life expectancy can be a year or less.
Causes
Some causes of this central nervous system disease do not depend on lifestyle (for example, heredity), others are associated with a person’s neglectful attitude towards his own health.
Most likely, the demyelinating process of the brain occurs under the influence of several factors simultaneously.
The development of this disease may be associated with the following factors:
- Defects in hereditary information associated with the formation of the myelin sheath.
- Adverse habits that cause poisoning of neurons with smoke, narcotic compounds, and alcohol.
- Long-term exposure to stress.
- Viruses (rubella, herpes, measles)
- Neuroinfections that affect nerve cells.
- Hepatitis vaccination.
- An autoimmune disease that causes destruction of the myelin sheath.
- Metabolism failures.
- A paraneoplastic process that develops due to the growth of neoplasms.
- Intoxication with any potent harmful substances (including those used in everyday life - paints, acetone, drying oil), as well as toxic metabolic products.
- Some congenital anomalies, such as “empty sella turcica” (more details here).
Main causes of demyelinating disease
Any demyelinating disease of the central nervous system can manifest itself for various reasons. The most famous among them:
- Metabolism problems. This is typical for diseases such as diabetes and thyroid diseases.
- Paraneoplastic processes, which are the first manifestation of a malignant tumor.
- Intoxication with chemical components: narcotic, psychotropic, alcohol, paints and others.
- The immune response to proteins found in myelin.
Numerous studies in recent years confirm that demyelinating diseases of the brain can develop due to negative environmental influences, poor heredity, poor nutrition, prolonged stress or bacterial infection. Infectious diseases play an important role in the spread of pathology: herpes, measles, rubella, Epstein-Barr virus.
It is not always possible to find out the reason for the occurrence of such a process. However, in modern medicine it is customary to identify several main risk factors. For example, quite often such a disease develops against the background of hereditary diseases, including aminoaciduria, leukodystrophy, Alexander disease, etc.
Demyelization may be acquired. In some cases, damage to the myelin sheaths occurs against the background of infectious inflammatory diseases, less often after the administration of vaccines. Diseases such as diffuse and multiple sclerosis, acute transverse myelitis can also cause demyelination of nerve fibers.
On the other hand, such diseases can be caused by certain metabolic disorders. In particular, the cause is often acute deficiency of vitamin B12, central pontine myelinosis and some other conditions.
Among the main reasons as a result of which demyelination of the brain begins to develop in the body are:
- The reaction of the human immune system to the protein that makes up myelin. As a result of irreversible processes that occur in the body, such a protein begins to be perceived by the immune system as foreign. The cells begin to attack it and gradually destroy it. This reason is the most dangerous. This mechanism can be triggered by the entry into the body of an infection or features of the human immune system that are hereditary in nature. These include multiple sclerosis, multiple encephalomyelitis, etc.
- The demyelinating process can begin in response to the presence of a neuroinfection that specifically affects myelin.
- Disturbance of metabolic processes in the body. As a result, myelin begins to suffer from a deficiency of the substances it needs and gradually collapses. This is possible in patients who have a history of diabetes and problems associated with the thyroid gland.
- The effect on the body of toxins and chemicals, including: alcohol, psychotropic drugs, acetone, waste products of the body.
- Paraneoplastic processes that occur as a complication of cancer.
As a result of scientific research, it was possible to establish that heredity and unfavorable environmental conditions play a special role in the damage to myelin (the sheath of nerve fibers). There is also information about the connection between the likelihood of the occurrence of this disease and the geographic location of a person, where foci of demyelination are noted.
An important role in the development of demyelinating brain disease is played by stress, poor nutrition, viruses (among which the most common are herpes, measles, rubella, etc.), bacteria and poor ecology.
There are two types of brain demyelination:
- Myelinoclasty - characterized by a hereditary predisposition to the rapid destruction of the myelin sheath.
- Myelinopathy is a process of destruction of the myelin sheath that has other causes.
Treatment methods
Treatment of such complex ailments involves two main approaches: containing pathological phenomena in the central nervous system and combating autoimmune processes (pathogenetic therapy) and mitigating the manifestation of symptoms.
Interferon
The first direction of treatment involves the prescription of drugs containing interferon. The effect on immunity involves the elimination of those immune complexes and antibodies that are in the patient’s blood.
The drugs can be administered intravenously, subcutaneously, and if taken for a long time, the risk of sudden progression is actually reduced.
Plasmapheresis
Another way to eliminate antibodies that are harmful to myelin is to filter the cerebrospinal fluid. During each of eight consecutive procedures, about 150 mg of cerebrospinal fluid is passed through special filters. Plasmapheresis is also used for the same purpose - to remove antibodies circulating in the patient’s vessels and heading to the brain.
Hormones
Treatment with hormones also helps remove aggressive biochemical compounds from the blood that destroy the membrane of neurons. If autoimmunization is pronounced, it is advisable to use cytostatics.
Nootropics
Symptomatic treatment involves the use of nootropic medications that protect the nervous system from the pathological effects of the disease. These drugs are taken for a long time, but they do not have any adverse effects on the body.
Nootropics not only stimulate thinking and optimize basic mental processes, but also prevent the death of neurons and accompanying cells from lack of oxygen. Under their influence, venous circulation and timely outflow of blood from the brain improve, and the sensitivity of brain structures to toxic substances decreases.
Despite many positive effects, nootropics still have contraindications: they cannot be taken for sickle cell anemia, drug addiction, neuroses, cerebrovascular insufficiency and some other conditions.
Muscle relaxants
With these pathologies, a situation may arise when neurons with a destroyed membrane stop sending signals to relax the muscles, and they are in constant tension. To eliminate this problem, muscle relaxants are prescribed.
To reduce the intensity of inflammation and slow down the body's violent reaction to its own inflamed tissues, anti-inflammatory drugs are needed. Under their influence, the vascular network in the central nervous system ceases to be so permeable to autoantibodies and immune complexes.
Traditional methods
Treatment using folk, non-traditional methods can only be auxiliary. Such diseases cannot be overcome with the help of medicinal herbs and home treatments. But some ways to strengthen the immune system may be advisable. In this case, any prescriptions used should be discussed with your doctor.
Therapy focuses on influencing the immunoreactive process. Unfortunately, the cause of multiple sclerosis cannot be eliminated. Therefore, treatment is aimed at improving the patient’s health and mitigating his condition. The methods used can be divided into 3 groups:
- Corticoids are the dominant drugs during an exacerbation. They are administered mainly during an attack, mainly intravenously in infusions. Methylprednisolone is used. If the therapeutic effect is insufficient, Cyclophosphamide can be used once.
- During the period of relapse prevention, maintenance doses of Prednisone or other immunosuppressants (Azathioprine, Cyclophosphamide) are used to slow down further attacks and stabilize the process. This type of treatment is mainly used in the early stages of the paroxysmal form. Long-term use of corticosteroids is fraught with a number of possible side effects, so they are always administered in a single daily dose every other day (alternating method).
- Symptomatic treatment is guided by clinical manifestations. For spasticity, muscle relaxants (Baclofen, Tizanidine, Tetrazepam) are used. Cerebral symptoms are improved by Physostigmine, tremor by Clonazepam, sometimes in combination with Trimepranol. Paresthesia may be relieved by carbamazepine, amitriptyline, or hydantoins. Melipramine or Ditropan can be used against urinary problems. Part of the treatment is well-chosen rehabilitation. Regular targeted treatment is important in the presence of certain provoking factors and improvement of prognosis.
Is there an effective treatment?
The effectiveness of treatment of demyelinated diseases depends on the type of pathology, the location and extent of the lesion, and the advanced stage of the disease. With timely consultation with a doctor, positive results can be achieved. In some cases, treatment is aimed at slowing down the process and prolonging life.
Drug therapy is based on the following methods:
- Preventing myelin destruction by blocking the formation of antibodies and cytokines using interferons. The main drugs are Betaferon, Relief.
- Impact on receptors to slow down the production of antibodies using immunoglobulins (Bioven, Venoglobulin). This technique is used in the treatment of acute stage diseases.
- Instrumental methods – purification of blood plasma and liquid using immune filtration.
- Symptomatic therapy – drugs from the group of nootropics, neuroprotectors, antioxidants, and muscle relaxants are prescribed.
Traditional medicine offers the following remedies for the treatment of pathology: a mixture of onions and honey in a wound proportion; blackcurrant juice; alcohol tincture of propolis; garlic oil; Echinops seeds; medicinal collection of flowers and leaves of hawthorn, valerian root, rue. Of course, folk remedies themselves are not capable of seriously affecting the pathological process, but together with medications, they help increase the effectiveness of complex therapy.
Types of disease
The classification of this disease is based on identifying the root cause of the disease:
- If myelin in the body is destroyed for hereditary reasons, they speak of myelinoclasty.
- If the membrane is produced and functions correctly, but then disappears due to the action of external factors, they speak of myelinopathy.
In addition, there are main diseases that are included in the concept of “demyelinating disease of the central nervous system”:
- The most common pathology of this kind, multiple sclerosis, affects all parts of the central nervous system. The characteristic symptoms are very varied.
- Progressive multifocal leukoencephalopathy.
- Marburg's disease.
- Acute disseminated encephalomyelitis.
- Devic's disease.
Causes of pathologies
Demyelinating diseases are caused by damage to the myelin sheath of nerve axons. The above-mentioned endogenous and exogenous factors that determine the process of demyelination become the main causes of diseases. According to the nature of the provoking factors, the diseases are divided into primary (polyencephalitis, encephalomyelopolyradiculoneuritis, neuromyelitis optica, myelitis, optoencephalomyelitis) and secondary (vaccinal, parainfectious - after influenza, measles, and some other diseases) form.
Schilder's diffuse sclerosis
Demyelinating disease is also known as Schilder's disease. It affects children and young people, is non-hereditary, and has a progressive (rapidly developing) course. Maximum survival time is 10 years.
The basis of demyelinating disease is a significant focus of myelin destruction throughout the entire medulla, usually spreading through the corpus callosum (the caudal body responsible for attaching to the cerebral hemispheres). In addition, there are numerous isolated small demyelinating lesions in the brainstem, spinal cord, and optic nerves.
Symptoms
The development of Schilder's disease leads to the following manifestations:
- hemiplegia (paralysis of the entire left or right side of the body) or quadriplegia (complete or partial paralysis of all 4 limbs and torso);
- homonymous hemianopsia (darkening of half the visual field);
- cortical blindness, deafness;
- pseudobulbar syndrome.
Diagnosis and treatment are the same as for multiple sclerosis.
Symptoms
Symptoms depend on the type of disease and where the areas of demyelination in the brain are located.
In particular, multiple sclerosis is characterized by the following set of symptoms:
- Changes in the intensity ratio of tendon and some skin reflexes, paresis, muscle spasms.
- Changes in vision characteristics (distortion of field, clarity, contrast, appearance of scotomas).
- Changes in the degree of sensitivity of different analyzers.
- Signs of dysfunction of the brain stem and nerves anatomically connected to the brain (bulbar syndrome, dysfunction of facial muscles, nystagmus).
- Pelvic organ dysfunction (impotence, constipation, urinary incontinence).
- Changes of a neuropsychological nature (decreased intelligence, depressive states, euphoria).
Marburg disease (disseminated encephalomyelitis) is a transient, deadly disease that can kill a person in a few months. There is a classification according to which this disease is classified as a form of multiple sclerosis. It resembles an infectious disease in which the following symptoms appear:
- A rapidly developing demyelinating pathology affects the brain stem and the nerves connected to it.
- Intracranial pressure increases.
- Motor function and sensitivity are impaired.
- Headache often occurs, accompanied by vomiting.
- Convulsions appear.
Devic's disease is a process of demyelination that primarily affects the optic nerves, as well as the substance of the spinal cord. The disease is considered more dangerous for adults and less dangerous for children, especially if treatment with hormonal medications is started in time. Manifestations of this pathology are as follows:
- Vision problems leading to complete blindness.
- Paralysis.
- Dysfunction of the pelvic organs.
Another pathology, progressive multifocal leukoencephalopathy, is characterized by a combination of immune changes caused by external factors and the appearance of demyelinated lesions. You can suspect such a disease based on the following signs:
- Decreased visual ability.
- Decrease in intelligence.
- Loss of coordination.
- Cramps.
- Paresis.
As you understand, such problems greatly reduce the quality of life.
Polyneuropathy affecting the PNS
Polyneuropathy is a group of demyelinating diseases of the peripheral nerves that affect both sexes. The occurrence of the disease involves the influence of endogenous and exogenous factors:
- inflammation;
- metabolic disease;
- toxic, immunopathogenic effects;
- deficiency of vitamins and nutrients;
- degenerative, paraneoplastic factors, etc.
The reasons are as follows:
- hereditary: motor and sensory neuropathy;
- metabolic: diabetes mellitus, uremia, liver disorders, porphyria, hypothyroidism;
- nutritional deficiency: lack of vitamins B12, B1, alcohol, malnutrition, malabsorption;
- toxic: alcohol, drugs, organic industrial substances (benzene, toluene, acrylamide, carbon disulfide), metals (mercury, lead);
- inflammatory-autoimmune: Guillain-Barré syndrome, acute and chronic inflammatory demyelinating neuropathies, Lyme disease;
- autoimmune diseases: polyarteritis nodosa, rheumatoid arthritis, systemic lupus erythematosus, sarcoidosis;
- paraneoplastic: cancer, lymphoproliferative disorders, myeloma, gammopathy.
Mainly long nerves are affected, clinical manifestations predominate in the distal limbs (on the opposite side of the lesion). Signs can be symmetrical or asymmetrical. Sensitive, motor, and autonomic symptoms often predominate in relation to the 3 main types of nerve fibers.
Symptoms
The first symptoms include burning, tingling, feeling of tightness, coldness, pain, and decreased sensitivity. These signs usually begin on the soles of the feet and spread to the ankles. Later, when the lesions grow in volume, manifestations reach the area of the tibia and appear on the fingers.
Among the motor manifestations, the most common are convulsions, muscle tremors (twitching), muscle weakness, atrophy, increased fatigue, and unsteady gait.
A disorder of the autonomic nerves causes disturbances in sweating, blood circulation, and heart rhythm. There is a decrease in reflexes, impaired sense of smell, damage to deep sensitivity, etc.
Diagnostics
Polyneuropathy can develop acutely and chronically. Demyelinating disease requires a complete professional examination. It is necessary to examine blood and urine (exclude causes of diabetes, liver, kidney disorders, etc.). A chest x-ray, EMG, cerebrospinal fluid examination (lumbar puncture), examination of family members, and nerve and muscle biopsy are performed.
Treatment
Polyneuropathy can be treated after determining its cause. The basis of therapy is precisely the elimination of the causative factor. A significant part of the treatment process is supportive, aimed at regenerating peripheral nerves, but does not address the underlying causes and does not cure demyelinating disease.
Symptoms
At the earliest stages of pathology development, there is no clinical picture, since compensation mechanisms are activated and healthy cells begin to work for themselves and for the sclerotic tissue.
When half of the structures are affected, the patient begins to complain of various types of visual impairment, decreased sensitivity of the skin on the trunk and limbs, muscle weakness and changes in gait. Further, the state of health gradually worsens, the symptoms are supplemented by pain in the arms and legs due to muscle spasms, the appearance of pathological reflexes revealed during a general examination by a specialist, increased fatigue during normal work activities, and paresis of facial muscles. Mental disturbances, changes in behavior and mood are noted. The patient may speak slurredly or say phrases that are not logically connected. Sometimes defecation and urination are difficult. Epileptic seizures rarely occur.
A person’s well-being can be affected by stuffy rooms, hot showers, and overheating in the sun. It is worth remembering to avoid such nuances in order to prevent attacks.
Sources
- https://vsemugolova.com/bolezni/skleroz/vidy-sk/rasseyannyj/kod-po-mkb.html
- https://diabetik.guru/info/cerebralnyj-ateroskleroz-kod-po-mkb-10.html
- https://yusupovs.com/articles/neurology/demieliniziruyushchee-zabolevanie-tsns/
- https://kiberis.ru/?p=21441
- https://diseases.medelement.com/disease/%D0%B4%D0%B5%D0%BC%D0%B8%D0%B5%D0%BB%D0%B8%D0%BD%D0%B8%D0 %B7%D0%B8%D1%80%D1%83%D1%8E%D1%89%D0%B8%D0%B5-%D0%B1%D0%BE%D0%BB%D0%B5%D0% B7%D0%BD%D0%B8-%D1%86%D0%B5%D0%BD%D1%82%D1%80%D0%B0%D0%BB%D1%8C%D0%BD%D0%BE %D0%B9-%D0%BD%D0%B5%D1%80%D0%B2%D0%BD%D0%BE%D0%B9-%D1%81%D0%B8%D1%81%D1%82 %D0%B5%D0%BC%D1%8B/13509
- https://diseases.medelement.com/disease/12881
- https://NashiNervy.ru/tsentralnaya-nervnaya-sistema/kod-rasseyannogo-skleroza-po-mkb-10.html
[collapse]
Amyotrophic lateral sclerosis (LAS)
LAS begins unnoticed. The patient has difficulty with normal activities (writing, fastening buttons). Later, problems with walking, muscle cramps, and difficulty swallowing develop. At the end, the patient is completely paralyzed and depends on artificial respiration and nutrition. In fatal LAS, the patient gradually loses nerve cells. In 5-10% of cases the disease has a hereditary form.
Demyelinating disease is characterized by selective damage to central and peripheral motor neurons (a motor neuron is a nerve cell that directly innervates skeletal muscles). We are talking about the gradual disappearance of motor neurons of the spinal cord, in the area of the brain stem, degeneration of the corticospinal tract.
Symptoms
Typical manifestations: muscle atrophy, fasciosis, tendinococcal hyperreflexia, spastic phenomena. The disease begins around 40-50 years of age (usually before 60 years of age). Clumsiness of the hands develops, and later difficulties when walking are added. Muscle atrophy soon occurs. Muscle spasms and pain may be present. Sometimes the disease begins with bulbar syndrome, difficulties with speech and swallowing.
Treatment
There is no treatment for demyelinating disease; therapy is only symptomatic, but not very effective and not targeted. Some delay in disease progression has been demonstrated with the drug Riluzole (Rilutek). Progression is very rapid, usually within 5 years from the onset of the disease.
ADEM = acute disseminated encephalomyelitis
Acute disseminated encephalomyelitis (ADEM from Acute disseminated encephalomyelitis) develops after an infection or vaccination. The disease has a monophasic course, but 25% may have relapses. The incidence is 0.4-0.8 patients per 100,000, mortality is up to 5%, complete remission occurs in 50-70%. The disease is characterized by seasonal peaks in incidence in winter and spring.
Pathology
The pathogenetic mechanisms of this demyelinating disease are not fully understood, despite the large number of immunological changes identified during the study of the disease. The study of the disease mainly relies on observations of experimental models of the disease. With ADEM, extensive inflammation of the white and gray matter of the brain is formed, perivenous localization with merging foci of demyelination.
The infiltrate consists of macrophages/monocytes and lymphocytes. Recent studies have found that perivenous demyelination is associated with activation of cortical microglia without loss of myelin. Macroscopically, cerebral edema is observed, and microscopically, hyperemia, endothelial edema, infiltration of the vascular wall and perivascular edema are observed.
Unlike MS, pro- and anti-inflammatory cytokines and hemokines are involved in the pathogenesis of ADEM: IL-1beta, 2, 4, 5, 8, 10; TNF-alpha, IFN-gamma.
Clinical picture
History of infection or episode of fever in recent days or weeks; or vaccination. Neurological symptoms increase quickly, within 2-30 days after infection or vaccination, but the role of infection or vaccination as a trigger of the disease has not been fully proven.
Clinically, general symptoms are observed: high fever, cephalgia, meningism, which appear before the onset of focal CNS symptoms. Classic ADEM symptoms are encephalopathy, seizure syndrome, bilateral optic neuritis and symptoms depending on the location of the lesions in the central nervous system.
Diagnostics
Cerebrospinal fluid classically shows pleocytosis (100/3), oligoclonal antibodies are negative, and myelin basic protein (MBP) is high.
MRI visualizes extensive lesions in the white matter of the brain and spinal cord. Classically, lesions are localized subcortically and in the central white matter. There is evidence that damage is also localized in the gray matter of the cerebral cortex and basal ganglia in ADEM.
Treatment
Steroids: Methylprednisolone 20 mg/kg/day for 3-5 days, sometimes continuing with po Prednisolone, gradually reducing the dose, over 4-6 weeks.
IVIG: alternative treatment, dosage 0.4-2 g/kg 2-3 days.
Plasmapheresis: Used as a last resort to treat ADEM when the patient does not respond to high-dose methylprednisolone. Plasmapheresis improves clinical results, but there is no evidence that the use of this method in the early stages is effective.
A demyelinating disease of the brain and spinal cord that occurs after acute viral infections (measles, rubella, etc.) or certain types of vaccination (for example, against rabies, smallpox, etc.). This is more likely an immunological complication of infection than direct damage to the central nervous system by the virus.
The clinical picture is no different from other encephalomyelitis. CSF findings are either normal or show dissociation of cytological protein.
Modern diagnostic methods
The main diagnostic method for identifying demyelinating diseases is magnetic resonance imaging (MRI). The technique is completely harmless and can be used for patients of any age. MRI is used with caution in obesity and mental disorders. To clarify the activity of the pathology, contrast enhancement is used (recent lesions accumulate contrast agent more quickly).
The presence of a demyelonating process can be detected by conducting immunological studies. To determine the degree of conduction dysfunction, special neuroimaging methods are used.