Perinatal encephalopathy of newborns is an unclassified non-inflammatory disorder of the nervous system observed during pregnancy or immediately after birth.
The disease is called unclassifiable because encephalopathy is not detected by traditional tests. Even high-tech research does not provide a complete objective picture.
The concept of perinatal encephalopathy (PE) is excluded from the International Classification. Today, encephalopathy is defined as the consequences of damage to the fetal brain. If we adhere to the accuracy of terminology, then encephalopathy can be called a consequence of destructive manifestations that destroy the cerebral cortex.
What is encephalopathy?
Encephalopathy is a collective term to denote a brain pathology of a non-inflammatory nature, characterized by the presence of multiple foci of ischemia in the cortex and subcortical structures. There are many reasons leading to hypoxia and subsequent neuronal degeneration. This includes the influence of infectious agents, endogenous or exogenous toxins, and injuries of varying severity. Symptoms of the disease, regardless of etiology, are impaired intellectual functions, motor deficits, and emotional and volitional disorders.
Encephalopathy is unspecified, or idiopathic, and does not have obvious clearly defined development factors. That is, it is impossible to reliably establish what resulted in dystrophic changes in nerve cells. This diagnosis is especially often given to children in the first year of life, when brain damage is “obvious”, and it is no longer possible to identify why this happened and at what period of time.
A newborn child experiences a pronounced phenomenon of neuroplasticity, when intact (healthy) areas of the brain take over the functions of damaged ones.
Therefore, the diagnosis of unspecified encephalopathy in an infant can be removed after a few years, due to the absence of any external or internal signs of the disease.
Causes and classification
The following types of encephalopathy are distinguished:
The congenital form can develop due to:
- genetic abnormalities;
- disturbances in the formation of the brain and internal systems during the intrauterine development of a child.
The danger of encephalopathy is that the pathological condition cannot be cured. Therapy prescribed for such disorders is designed to stop the development of cell necrosis.
The acquired form often occurs against the background of injuries received during childbirth. In adults, other causes may lead to necrosis of brain cells.
Severity
The severity of encephalopathy reflects the characteristics of the increase in symptoms and consequences for the brain and the whole body.
Lightweight
For minor brain damage, a weak degree of PEP is recorded. Symptoms are not expressed; the disease is determined by tests and brain studies. With timely treatment, improvement occurs quickly and does not cause any consequences or complications.
Average
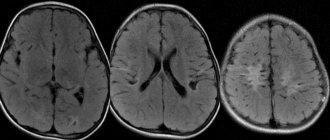
Symptoms of moderate encephalopathy appear as temporary phenomena, not permanently. The child exhibits behavioral disorders and weakened reflexes (sucking, swallowing, etc.). During hardware examinations of the brain, foci of damage and hemorrhage are recorded.
Heavy
In the severe stage of PEP, the newborn is weakened, there is a fading of reflexes, and multiple behavioral deviations. The baby refuses the breast, does not respond to irritation, or is hyperexcitable. Regardless of the quality of treatment, complications remain in the form of developmental delays and behavioral disorders. Children often remain disabled.
Symptoms of the disease
The severity of the symptoms of this pathology and their combination depend on:
- on the age of the child and the degree of maturation of the nervous system;
- on the location and extent of damage to brain tissue and its glial structures;
- on the causative factor and the duration of its effect on brain cells;
- from the presence of concomitant diseases that can aggravate the pathological effect of the main etiological factors (intoxication, metabolic or vascular disorders).
Common signs and symptoms of encephalopathy in children are:
- frequent headaches, anxiety, moodiness, constant screaming (in young children);
- hyperactivity, uncontrollability, disinhibition, obsessive states;
- sleep disorders, which are manifested by drowsiness during the day and insomnia at night;
- neuroses in the form of behavioral disorders or phobias in the form of panic fear of any objects, obvious or imagined, as well as environmental phenomena;
- decreased memory (usually impaired short-term memory for remembering words, numbers or names of objects), cognitive activity and intelligence of the child;
- hearing and vision impairment;
- development of hydrocephalic syndrome (in children of the first year of life).
Parents need to remember that in the absence of diagnosis and timely treatment, there is a progression of diffuse changes in brain cells, the breakdown of connections between neurons and their death lead to significant deviations in the functioning of the central nervous system.
In this case, the symptoms become permanent with worsening signs of encephalopathy in children, the following are noted:
- frequent fainting;
- dizziness;
- asthenia;
- deterioration of attention and memory;
- changes in motor coordination;
- movement disorders (flaccid paralysis, paresis);
- mental and vegetative disorders;
- significant decrease in intelligence;
- behavioral disorders;
- developmental delay.
Discirculatory or toxic
In this form of the disease, organic changes in neurons develop due to the development and progression of vascular diseases, congenital anomalies of cerebral vessels, or toxic effects on neurons of poisons, microbial toxins, drugs or chemicals.
This pathology can be triggered by the influence of the following factors on the child’s brain:
- systemic or infectious vasculitis, embolism, hereditary angiopathy, persistent hypotension, arrhythmias;
- congenital anomalies of cerebral vessels (aneurysms, atriovenous malformations, congenital stenoses);
- blood diseases (leukemia, thrombocytopenic purpura, coagulation disorders);
- viral and infectious diseases with persistent and long-term neurotoxicosis, complicated by septic processes;
- progressive somatic and endocrine pathologies that cause persistent changes in blood vessels, microangiopathy (diabetes mellitus, pathology of the adrenal glands and thyroid gland);
- abuse of alcohol, nicotine, narcotic and toxic drugs (by the mother during pregnancy or adolescence).
Epileptic
Epileptic encephalopathy develops against the background of an increase in convulsive or non-convulsive seizures, leading to the progressive death of nerve cells in the lesion, the formation of new foci of epileptiform activity and disruption of connections between neurons.
Impaired brain function manifests itself in progressive cognitive disorders, decreased memory and intelligence, behavioral disorders, severe asthenia, and sleep disorders.
There are two forms of epileptic encephalopathy:
- epileptic encephalopathy I or destructive epileptic encephalopathy - develops against the background of progressive established epilepsy in a child with frequent, prolonged seizures, recurring status epilepticus;
- Epileptic encephalopathy II is manifested by typical mental disorders, behavioral changes, social maladaptation and cognitive disorders characteristic of destructive epileptic encephalopathy in the complete absence of characteristic epileptic seizures.
Perinatal or residual encephalopathy perinatally caused
This form of the disease comes from the Latin residual, meaning “residual.”
Thus, this type of encephalopathy may be a residual phenomenon of previously suffered pathological processes in the brain.
Quite often this disease is observed after perinatal encephalopathy.
Residual encephalopathy may not manifest itself in any way for a long time, most often up to 3-5 years, and only after this period symptoms begin to appear. The effectiveness of treatment of childhood encephalopathy with early diagnosis, complete and comprehensive treatment, and compliance with all recommendations of specialists in most cases is completely cured within a year and has virtually no consequences in adult life.
Associated syndromes
Brain dysfunctions appear in newborns with PEP in the form of syndromes and behavioral disorders.
Hypertensive-hydrocephalic
This syndrome is recorded with intracranial hypertension, excess fluid in the structures of the brain. The baby's head grows rapidly due to the increase in hydrocephalus, the fontanelle often opens and thickens, reflexes weaken, and Graefe's symptom is recorded.
Cerebrospinal fluid cannot leave the brain due to impaired blood flow.
Movement disorder syndrome
The syndrome is characterized by increased or decreased muscle tone, involuntary muscle contractions (dystonia). The baby takes unnatural positions and remains in them for a long time. Reactions to light, sound, and touch are impaired. The baby often screams, but the crying has no emotional coloring.
Hyperexcitability
The most common PEP syndromes include hyperexcitability. The baby is overly active, the muscles are constantly in increased tone, all reactions are exaggerated. The arms and legs are compressed, convulsions, chin tremor, nystagmus, and insomnia are often recorded. The baby falls asleep for a short time and quickly wakes up crying.
Convulsive
Convulsions can be local in nature (tremor of the eyes, chin) or generalized, when the entire body arches. It is difficult for the baby to hold down food; he constantly burps profusely, sometimes to the point of vomiting. Respiratory disturbances and apnea are observed.
Comatose
Fixed after birth injuries and toxic effects with significant brain damage. The baby completely loses the ability to suck and swallow, all basic body functions are impaired.
Syndrome of vegetative-visceral disorders
With this syndrome, a persistent disruption of the functioning of internal organs and systems in a newborn is recorded, caused by dysfunctions of the central nervous system. Along with external manifestations - discoloration of the skin, respiratory, digestive, genitourinary, and motor dysfunctions are observed.
Attention deficit and hyperactivity disorder
The syndrome is characterized by inappropriate behavior - inability to concentrate, pathological activity, inattention, lack of ability to learn new things.
Course of the disease
Encephalopathy of mixed origin can develop gradually or rapidly. Features of the clinical picture depend on the stage of the pathological process, the causes of its occurrence, and the quality of care provided.
The sooner the problem is identified and specialized therapy is started, the higher the chances of a favorable outcome. At the initial stage of the disease, it is possible to completely restore the functionality of the brain. If no action is taken, the patient will develop dementia and there is a high probability of the patient becoming disabled.
Compensated stage
At this stage, the patient experiences mild cognitive and neurological impairment. Manifestations are minimal and are not constantly present. They can be triggered by a change in weather, physical fatigue or mental stress, or a stressful situation.
The clinical picture is characterized by the following signs:
- headaches of unknown origin, varying degrees of severity and localization;
- sleep problems;
- impaired attention and forgetfulness;
- sudden changes in mood for no reason;
- irritability.
If the causes of brain damage are identified and eliminated, the development of the disease can be stopped. At the same time, there is a high probability of complete restoration of tissue structure and return of their functions without negative consequences for the body.
Subcompensated stage
At the next stage, mixed encephalopathy occurs more aggressively. Symptoms
intensifies and becomes permanent. Problems with attention and intellectual functioning are obvious. Cephalgia practically does not stop, and is supplemented by tinnitus. A person has virtually no control over his behavior. He is characterized by tearfulness, capriciousness, touchiness and even aggressiveness. There are frequent manifestations of depression, which can drag on for several weeks. Blood pressure surges may occur.
As the pathology progresses, memory problems worsen and mental abilities decrease. The patient is absent-minded and may suffer from attacks of amnesia and paranoia. He already needs the help of strangers and is not able to live alone. Starting treatment at this stage can significantly reduce the severity of the clinical picture and improve a person’s quality of life. It will no longer be possible to completely restore lost brain functions.
Decompensated stage
The diagnosis indicates the fact of atrophy of large areas of the brain. Dead tissues cannot be restored; their functions are lost forever. In this case, even those areas that are responsible for the life support of the body suffer. This leads to the development of an extremely aggressive clinical picture.
Symptoms of stage 3 mixed encephalopathy:
- signs of dementia are obvious;
- weight loss occurs;
- symptoms of Parkinson's disease appear;
- uncontrollable behavior - calm periods interspersed with attacks of aggression, moodiness, tearfulness, hysterics and other mental problems;
- headaches are similar to migraine attacks, accompanied by tinnitus and dizziness;
- memory problems up to amnesia;
- the patient cannot control his body, spontaneous bowel movements and bladder emptying occur;
- malfunctions of the musculoskeletal system.
At this stage, encephalopathy of combined origin is subject to symptomatic treatment. It is aimed at facilitating the patient’s condition and the process of caring for him. The processes in the brain are already irreversible; it will not be possible to restore lost or lost functions.
Symptoms and external signs in children under one year of age
The development of PEP in children can be noticed by a number of signs characterizing the disease.
Headache
Encephalopathy is accompanied by paroxysmal or constant headaches, during which the baby screams and cannot calm down and relax.
Insomnia
Sleep disorders are manifested by increased drowsiness, constantly being in a semi-conscious state. Often the child cannot fall asleep, falls asleep for a few minutes and wakes up screaming.
Memory impairment
The ability to learn and remember decreases. A baby with encephalopathy learns new knowledge and skills more slowly, and later begins to become interested in toys and recognize loved ones.
Decreased motor activity of the child
The baby later acquires the ability to hold his head, sit, and crawl. Motor activity is impaired, it is difficult for him to coordinate movements due to insufficient brain function.
Phobias
Children often suffer from obsessive fears - they are afraid of the dark, the absence of parents in the room, noise, bright light.
Hydrocephalus
Children under one year of age often develop hydrocephalus due to the accumulation of fluid in the ventricles of the brain. This is expressed in disproportionate head growth.
Symptoms of the discircular form
The discircular form develops during three stages, each of which is characterized by certain characteristics. At the initial stage, tissue necrosis caused by impaired cerebral circulation is accompanied by frequent dizziness and headaches. The first degree of damage is characterized by a decrease in the patient’s cognitive abilities.
The second stage is characterized by constant headaches and tinnitus. At this stage, depression often develops and sleep problems are noted.
At the last stage, life-threatening changes in brain structures occur. At this stage, coma may develop. With successful treatment of encephalopathy at the last stage, the patient is assigned a disability. It is impossible to completely eliminate the consequences of cell necrosis.
Diagnostic methods
To diagnose PEP, analyzes and hardware studies of the structures of the brain and blood vessels of the head and neck are used.
Neurosonography
The study is carried out on infants from birth through the large fontanel. Accumulations of cerebrospinal fluid, hemorrhages, and changes in brain structures are detected.
Doppler ultrasound
An ultrasound examination is aimed at studying the condition of the vessels of the brain and neck - conductivity, narrowing, changes in structure, the presence of cysts and damage.
Electroencephalography
The hardware procedure reveals brain activity, the speed of impulses, the presence of structural pathologies, and the condition of blood vessels.
Rheoencephalography
Using the procedure, the intensity of blood flow is determined, organic and functional disturbances in the conductivity of the veins and arteries of the brain, and the magnitude of pulse filling are separated.
Blood analysis
A blood test determines the presence of leukocytosis, a form of PEP associated with changes in bilirubin.
Childhood diseases. Evgeny Komarovsky. What is perinatal encephalopathy?
The complex phrase perinatal encephalopathy is found in the vocabulary of pediatricians, and therefore
parents, surprisingly often.
At least half of the readers who look at their child’s outpatient card have a real chance of finding there the famous abbreviation PEP - which, in fact, stands for
perinatal encephalopathy.
Translating this medical term into Russian is not very simple. But we'll try.
“Peri-”— (Greek peri-) a prefix meaning “location around, outside, at something.” “Natal” - from lat. natus - birth. It is easy to conclude that the essence of the concept “perinatal” is associated with childbirth, taking place before, during, after childbirth, there is even such a phrase - “perinatal period” and
science "perinatology".
Apparently, it makes sense to immediately clarify that perinatology calls the perinatal period the interval starting from the 28th week of intrauterine
fetal life until the seventh day after birth.
The word “pathy-”, coming from the Greek pathos-, is translated as “disease”, “suffering”. Also Greek enkefalos - brain. Well, together we get “encephalopathy” -
brain disease.
Brain disease is a non-specific concept; it is not surprising that encephalopathy is not a specific disease, but a term that unites a whole range of very diverse brain diseases. It becomes obvious that it is impossible to diagnose, treat and cure encephalopathy in
principle, because how can you treat a non-specific concept.
disease (damage) of the brain.
For example, bilirubin encephalopathy (brain damage associated with high levels of bilirubin), hypoxic encephalopathy (brain damage associated with oxygen deficiency), ischemic encephalopathy (brain damage associated with cerebrovascular accident). Such phrases as diabetic encephalopathy, traumatic encephalopathy, alcoholic
encephalopathy.
There is no doubt that without a qualifying adjective, the word “encephalopathy” does not make any sense and means something like this: “there is something wrong with the brain.”
And in this aspect, the word “perinatal” looks strange, to say the least, because it in no way specifies the nature of the brain damage.
This term simply indicates the time interval when these changes
happened.
So it turns out that the phrase “perinatal encephalopathy” is simply impossible to intelligibly translate into Russian - well, roughly, “something is wrong with the brain due to damage before childbirth, during
or immediately after childbirth." What's wrong? Who knows...
Taking into account the information provided, readers will perhaps not be surprised by the fact that the diagnosis of “perinatal encephalopathy” is not included in the international classification of diseases and is not used anywhere in the world, except
with the exception, of course, of the CIS countries.
Call the disease by a specific name or, albeit veiled, but say “with
there’s something wrong with the brain”—fundamentally different things.
In the process of development, all sorts of incomprehensibility occasionally arise, reflexes appear, disappear and fade, reactions to the environment rapidly change, sense organs improve, the range of movements undergoes significant changes, etc., etc. Medical science has worked hard and tried
systematize all these changes.
Hence numerous works with information about norms, about what is supposed to happen and what is not, about what can be, what is permissible, and what can never happen. And since there are hundreds of factors analyzed and taken into account, something is necessary
will go beyond the allotted time limits and norms.
And then the question of diagnosis will be on the agenda...
It will not be possible to make a diagnosis based on the international classification of diseases. But there are specific complaints and problems: our chin is trembling, we cried for 30 minutes without stopping, and yesterday we burped four times, and
last week they kicked their legs a lot, etc.
The algorithm for the relationship between a pediatrician and parents within the framework of the national mentality does not at all provide for phrases like “everything is fine, leave the child alone” or “calm down, he will outgrow it.” The standard procedure for any doctor-parent contact begins with the question “on
Why are you complaining? and ends with a specific diagnosis.
A situation in which parents are happy with everything is amazingly rare. A medical examination, during which no deviations from norms, deadlines and standards are found, is a unique phenomenon. A combination of rare and
unique - this is beyond comment.
Source: https://dytyna.info/food/articles/any/3310
How to treat
Early treatment with AEDs can significantly reduce the likelihood of complications in infants and achieve full recovery.
For encephalopathy, complex treatment is used - medications of different classes and physical therapy.
Medicines
Medicines are chosen from several main groups, others are added according to symptoms.
Nootropics
Stimulators of neurometabolic activity improve the conduction of nerve impulses and increase the brain's resistance to hypoxia. For infants use:
- Vinpocetine;
- Pantogam;
- Piracetam;
- Actovegin.
The drugs are prescribed in a course, if necessary, they are replaced and the treatment is repeated.
Vasodilators
To dilate blood vessels, improve conductivity, and relax the smooth muscles of the vascular walls, vasodilators are used - Vinpocetine, Cinnarizine, Papaverine.
Psycholeptics
A group of drugs for suppressing psychomotor agitation and normalizing hyperexcitability - Elenium, Valerianahel.
Anticonvulsants
To relieve muscle cramps and dystonia, anticonvulsants are used - Phenobarbital, Diazepam.
Additional appointments
Other medications are prescribed depending on the leading syndromes and the severity of the condition. These are analgesics for pain relief, antispasmodics, muscle relaxants to reduce muscle tension. In severe cases, corticosteroids are prescribed to improve adrenal function. Infusion therapy compensates for the lack of glucose, sodium, and magnesium.
Physiotherapy
Physiotherapeutic treatment stimulates metabolism in brain tissue and improves the condition of blood vessels.
Electrophoresis
Electrophoresis with drugs is done to improve the trophism of blood vessels and tissues, stimulate local immunity and metabolism.
Amplipulsetherapy
The Amplipulse device operates with alternating currents, improves vascular conductivity and nourishes the brain.
Phototherapy
Phototherapy is indicated for significant increases in bilirubin and jaundice in the newborn. Performed continuously with breaks for feeding.
Massotherapy
Massage and gymnastics normalize muscle tone, have a general strengthening effect, and improve blood supply to tissues.
Important: for infants, regardless of the severity of the condition, breastfeeding is recommended with PEP.
Symptoms
The manifestations of unspecified encephalopathy vary widely depending on the severity, type, age and treatment used. As a rule, in the first stages of the disease, sleep disturbances, lethargy, daytime sleepiness, absent-mindedness, tearfulness, lack of interest, increased fatigue, decreased memory and thinking abilities are observed. Painful sensations, noises and ringing in the head, decreased hearing and visual functions, mood swings, lack of coordination, and irritability may also begin to appear.
Causes of the disease
The causes of the disease in this case formed the basis for the classification. Encephalopathies are divided into congenital and acquired. The first ones are also called perinatal and develop from the 28th week of intrauterine development to the end of the seventh day from birth. The etiological factors for the appearance of pathology diagnosed in infants are:
- Severe pregnancy, accompanied by toxicosis, eclampsia, and the threat of failure.
- Various anomalies and congenital defects of the nervous and cardiovascular systems.
- Fetoplacental insufficiency leading to prolonged fetal hypoxia.
- A condition of prematurity due to premature birth.
- Disturbance of labor (premature placental abruption, prolonged period of pushing).
- Umbilical cord entanglement leading to asphyxia during childbirth.
- Infectious diseases suffered by a woman during pregnancy.
- Intoxication of the fetus with alcohol, nicotine, etc.
- Rh conflict, which results in the breakdown of red blood cells.
- Traumatic brain injuries that occur due to a discrepancy between the size of the woman’s pelvis and the size of the child’s head or rapid labor.
Nervous tissue is considered the most vulnerable to a lack of oxygen, so the slightest deficiency leads to brain damage.
The acquired form of the disease occurs when exposed to the following factors:
- Hypoxia – the cause of which can be a pathology of the respiratory system, respiratory arrest of various origins. This also includes impaired microcirculation in the brain due to atherosclerosis, arterial hypertension, damage to deep arterioles, and stagnation of venous blood.
- Toxins, both external and internal. Harmful substances, and these can be ethanol, salts of heavy metals, pesticides, and waste products of various dangerous microorganisms, have a detrimental effect on neurons.
- Brain injuries - even a concussion can cause a consequence such as post-traumatic encephalopathy.
- Metabolic disorders - decompensated diseases of the liver, kidneys, diabetes mellitus, hypovitaminosis lead to a deterioration in the nutrition of nerve cells and the formation of foci of degeneration.
Encephalopathy, unspecified: causes, diagnosis, treatment
Encephalopathy, unspecified, is a class VI disease (diseases of the nervous system), which is included in block G90-G99 (other disorders of the nervous system) and has disease code G93.4.
Description of the disease
Encephalopathy is a non-localized disease of the brain. It is expressed by the death of nerve cells due to cessation of blood circulation, oxygen starvation and disease.
To diagnose diseases, specialists need to find out the pronounced location of the lesion, the localization of the disease in the gray or white matter of the brain, as well as the degree of impaired blood flow. If the cause of the disease cannot be established, then encephalopathy is called unspecified (idiopathic, i.e., occurring independently). The most common is vascular.
Causes of the disease
Encephalopathy, unspecified (ICD-10 diagnosis code G93.4) is classified into two types: congenital and acquired. Congenital is divided into prenatal (when damage occurs in the womb) and perinatal (in the event that the damaging factor acted in the last weeks before the birth of the baby or immediately after it). This type of pathology is caused by:
- defects consisting in abnormal processes of brain development;
- metabolic disorders in the body caused by genetic factors;
- if during pregnancy the baby was affected by a damaging factor;
- traumatic brain injury that occurs in a baby during childbirth.
Mitochondrial encephalopathy
Mitochondrial unspecified encephalopathy in infants is classified as a separate group of congenital diseases. It is formed as a result of disturbances in the functions and structures of mitochondria.
Acquired encephalopathy is classified into several types due to various damaging factors:
- Post-traumatic is the result of moderate to severe traumatic brain injury (for example, a fall from a height, head injuries in athletes, road accidents, etc.). With this type of disease, various lesions of the nervous tissue of the frontal and temporal lobes, atrophic changes (shrinkage and shrinkage of the brain), and hydrocephalus are observed.
- Toxic encephalopathy unspecified in adults occurs due to poisoning by various toxins: alcohol, high doses of pesticides, heavy metals, gasoline, etc. It is mainly manifested by various kinds of nervous and mental disorders (insomnia, anxiety, irritability, hallucinations, prolonged headaches, etc.).
- Radiation is the result of ionizing radiation to the body during radiation sickness. With this pathology, various neurological disorders are observed.
- Metabolic occurs due to metabolic disorders against the background of diseases of internal organs: liver, kidneys, pancreas. Manifests itself depending on the properties of the underlying pathology.
- Vascular encephalopathy. The cause may be addiction to bad habits, old injuries, atherosclerosis, diabetes, radiation exposure and other factors that cause cerebral hypertension. Signs of this type of disease are: loss of structure and integrity of consciousness, frequent headaches, depressive states, partial loss of one’s own memory.
- Hypoxic is the result of prolonged oxygen starvation. Leads to serious neuralgic complications.
And these are not all varieties.
There is unspecified encephalopathy in children. Thus, as a result of traumatic exposures in the womb, infections or other causes, residual encephalopathy is diagnosed in older children. The venous form is a particular type of vascular, which is manifested by stagnation of venous blood in the brain due to a violation of its outflow.
Metabolic encephalopathy is divided into several other types:
- Bilirubin is found only in newborn babies. It develops against the background of incompatibility between the blood of mother and fetus, as well as due to infectious toxoplasmosis, jaundice, and diabetes mellitus in the mother. It manifests itself as general weakness, decreased muscle tone, poor appetite, belching, and vomiting.
- Gaye-Wernicke encephalopathy occurs due to vitamin B1 deficiency. Side conditions can develop due to alcohol dependence, severe vitamin deficiencies, HIV, and malignant neoplasms. Mainly manifested by hallucinogenic syndrome and anxiety states.
- Leukoencephalopathy manifests itself as a disorder of the white matter of the brain. The disease is progressive. Appears after an infection due to a decrease in the body’s protective functions.
- Atherosclerotic disease develops mainly due to disorders of lipid metabolism in the body. It manifests itself as increased fatigue, weakness, dizziness, headaches, sleep disorders, and isolation.
Scientists say that the cause of any type of unspecified encephalopathy is primarily brain hypoxia (lack of oxygen).
This happens due to the fact that the organ begins to be less well washed with blood, excessive venous accumulations, swelling, and hemorrhages appear. Anoxic encephalopathy can occur due to a low supply of nutrients to neurons and ultimately develop into a separate disease.
Metabolic encephalopathy is a special case of toxic encephalopathy, when toxins are not eliminated and, as a result, penetrate into the blood.
There are several stages of development of this disease. Experts highlight the following:
- In the case of the initial or first stage, the patient’s memory decreases, he is irritable, has trouble falling asleep and sleeps anxiously, and also suffers from headaches.
- In the second case, the nature of the disease is more pronounced, all symptoms worsen. In addition to headaches and sleep disturbances, the patient may complain of apathy and lethargy.
- At the third stage, serious changes in the brain are diagnosed, there are paresis, speech is impaired, and vascular parkinsonism develops.
Symptoms
The manifestations of unspecified encephalopathy vary widely depending on the severity, type, age and treatment used.
As a rule, in the first stages of the disease, sleep disturbances, lethargy, daytime sleepiness, absent-mindedness, tearfulness, lack of interest, increased fatigue, decreased memory and thinking abilities are observed.
Painful sensations, noises and ringing in the head, decreased hearing and visual functions, mood swings, lack of coordination, and irritability may also begin to appear.
What symptoms occur as the disease progresses?
In advanced cases, symptoms can progress, resulting in parkinsonism (slow movements combined with trembling of the limbs) and falsebulbar palsy (manifested by impaired speech, chewing and swallowing functions). Also, do not forget that mental disorders (depression, suicidal thoughts, phobias) may develop. Let's look at how unspecified encephalopathy G 93.4 is diagnosed in infants and adults.
Diagnosis of encephalopathy, unspecified
In order to correctly determine the form of the disease, the doctor must carefully analyze the patient’s medical history for traumatic brain injury, intoxication, atherosclerosis, kidney disease, liver disease, lung disease, pancreas disease, hypertension, exposure to radiation, as well as acquired or genetic metabolic disorders.
To make a diagnosis of “encephalopathy, unspecified G 93.4”, the following procedures are carried out:
- General blood analysis.
- General urine analysis.
- Various metabolic tests (liver enzyme levels, glucose, electrolytes, ammonia, lactic acid, blood oxygen).
- Measuring blood pressure levels.
- CT and MRI (to detect brain tumors, various anatomical anomalies, infections).
- Creatinine.
- Drug and toxin levels (cocaine, alcohol, amphetamines).
- Doppler ultrasound.
- EEG or encephalogram (to detect brain dysfunction).
- Autoantibody test.
These are not all the tests necessary to make a diagnosis. Only the attending physician can order certain tests based on the patient's symptoms and medical history.
Treatment of encephalopathy
Treatment of unspecified encephalopathy is aimed at eliminating the root causes and symptoms that gave rise to the development of this disease. Conservative and medicinal methods are mainly used for treatment.
If the disease is acute, treatment is primarily aimed at reducing intracranial pressure and eliminating seizures. To do this, artificial ventilation of the lungs, extrarenal blood purification are used, and nutrients are administered through a dropper.
Medicines
Subsequently, the patient is prescribed medications that he must take for several months:
- various lipotropic drugs that help normalize cholesterol and fat metabolism (dietary supplements with choline, methionine, carnitine, lecithin, “Lipostabil”);
- drugs that prevent blood clots (Ginkgo Biloba, Aspirin, Cardiomagnyl);
- angioprotectors prescribed for various heart diseases to normalize the walls of blood vessels, the movement and outflow of venous blood (Troxerutin, Detralex, Indovazin);
- neuroprotectors for nourishing nerve tissue (B vitamins, Piracetam;
- tranquilizers and sedatives to reduce rapid nerve impulses in affected neurons (“Sibazon”);
- vitamins and amino acids;
- various performance stimulants.
Also, for a speedy recovery, physiotherapeutic procedures, acupuncture, walks, gymnastics, massage, and a certain rest regimen are prescribed. What is the prognosis for a diagnosis of “encephalopathy, unspecified”?
Disease prognosis
Any type of encephalopathy is characterized by vomiting, nausea, dizziness and headaches. If severe brain damage (or swelling) occurs, the disease develops very acutely, dizziness, very severe headache, anxiety, blurred vision and much more appear.
Typical complications of encephalopathy of unspecified origin are:
If you follow the recommendations of your doctor, you can hope for a favorable prognosis. However, if the disease is started, the following may develop:
- epilepsy;
- paralysis, various types of movement disorders;
- loss of brain function, memory, intelligence;
- emotional instability, depression, mood swings;
- disability.
Source: https://FB.ru/article/351632/entsefalopatiya-neutochnennaya-prichinyi-diagnostika-lechenie
Classification
Based on the method of acquisition, encephalopathies are divided into two groups - congenital and acquired.
Congenital
Congenital or perinatal encephalopathy is a disease that develops in the perinatal period (from 22 weeks of pregnancy to a week after the birth of the baby). It is determined and detected in the first months of life.
Acquired
Acquired encephalopathy affects mainly middle-aged and older people. The causes of this pathology are different, but they are based on post-hypoxic conditions, that is, oxygen deficiency and metabolic disorders of brain cells.
Encephalopathy, unspecified: causes, mechanism and symptoms
Any form of encephalopathy requires difficult treatment and a responsible approach by doctors and patients to their own condition. Encephalopathy, unspecified, is a special type of diagnosis that is made when there is insufficient information to 100% confirm the exact form of the pathology.
Features of the diagnosis
ICD-10 defines unspecified encephalopathy as G93. Synonym: acquired unspecified encephalopathy.
The diagnosis has specific features:
- put when it is not possible to clarify with additional research;
- Pediatricians often find symptoms of unspecified encephalopathy in newborns;
- in 80% of cases the diagnosis is not confirmed after 2-3 years;
- men get sick more often than women by 21%;
- The accuracy of the diagnosis is higher if it is made at 5 or 65 years of age (peak identification of the disease).
The unspecified form of the disease requires additional examinations and is not confirmed in all cases. Most often, true encephalopathy is found in middle-aged and elderly people.
Classification of forms
When making a diagnosis, the signs of the disease are taken into account. At the first stage, unspecified encephalopathy is confirmed less frequently, since pathologies are not detected during examinations, while cerebral changes are already present.
The second degree of severity allows for a faster diagnosis, as patients show mild to moderate signs of the disease. At the third stage, severe neuralgic disorders are noticeable and the diagnosis is confirmed even without additional examinations.
The specificity of unspecified encephalopathy is such that depending on the type of disease (intoxication, infectious), the type of stages also changes. In the acute course of an infectious pathology, the first degree almost immediately passes into the second or third.
Causes of the disease
Any encephalopathy - unspecified or confirmed - can be either congenital or acquired. Congenital pathology is associated with several factors. The first is prenatal, it is characterized by fetal injuries and other negative factors affecting the embryo. The second is perinatal, caused by childbirth, as well as adverse effects after birth.
Most often, these forms of encephalopathy develop as a result of:
- trauma to the skull received during the passage of the fetus through the birth canal;
- metabolic diseases inherited from parents;
- abnormalities in the development of the nervous system and brain;
- alcoholism, drug addiction, infectious diseases of the mother during pregnancy.
Acquired unspecified encephalopathy is divided into several more complex types. There are no average statistics on the frequency of their occurrence, since much depends on a person’s lifestyle and his environment:
- post-traumatic – appears as a result of dystrophy, scars, atrophy of brain tissue after traumatic brain injury;
- vascular – develops when there is poor blood supply to the brain against the background of hypertension, atherosclerosis, vascular pathologies, thrombosis;
- toxic – systemic effect of harmful substances: alcohol, metals, metabolites of bacteria and parasites, chemicals, shock doses of vitamins or minerals;
- radiation – appears as a result of radiation;
- metabolic – develops against the background of diseases of internal organs;
- hypoglycemic – occurs due to a decrease in blood glucose levels.
There is a more precise classification of encephalopathies, the types of which may occur in an unspecified form. This form, known as metabolic, is divided into several subtypes. They may be associated with other disorders, for example, vascular ones: cholesterol plaques narrow the lumen and cause metabolic disorders.
Medical researchers believe that the main cause of any encephalopathy is brain hypoxia.
Diagnosis of a disease is a multi-stage, complex process that requires a lot of time. You cannot rely on the results of one analysis, since any type of encephalopathy may hide other disorders. And pathology can never arise as an independent disease.
Development mechanism
For a more precise understanding of what unspecified encephalopathy is, you need to consider the mechanism of development:
- occurs . It is caused by vascular spasms and other disturbances in the functioning of organs and the circulatory system.
- Metabolic disorder . Cells do not receive enough nutrients, atrophy and degeneration begin.
- Proliferation of lesions . Demyelinated lesions, dying tissue, form in the white matter of the brain.
- They arise . At first they become small and isolated, then they grow.
- Swelling and congestion . The formation of these signs leads to the death of large areas of the brain.
Gradually, a person loses cognitive functions, and the nervous system suffers. Advanced encephalopathy cannot be treated; dead areas of the brain are not restored.
The brain reacts very quickly to any changes, since this organ contains a minimal supply of oxygen. As soon as it is no longer enough, pathological processes immediately develop.
Symptoms of pathology
Encephalopathy occurs slowly, and at least 3-6 months must pass from the onset of the disease to achieve the first symptoms. However, acute types are characterized by an accelerated course . At an early stage, regardless of the type of disease, certain signs are detected:
- difficulties in performing mental activities that previously did not cause problems;
- problems with step-by-step activities;
- memory loss;
- severe sleep disturbances, which lead to daytime drowsiness and nighttime insomnia, the patient experiences nightmares;
- severe fatigue even when doing familiar things that used to be enjoyable;
- extraneous noise in the ears, dizziness, headaches that constantly bother the patient;
- after stress, the patient feels an incredible loss of strength and emptiness;
- the character becomes hot-tempered, the mood often changes, irritability and tearfulness appear;
- the patient suffers from visual and hearing impairments.
In the initial stages of the disease, the patient remains in normal health, and changes begin mainly when weather conditions change. Symptoms are influenced by stress, anxiety and mental overload.
Dysfunctions of the nervous system develop slowly, beginning with a lack of coordination and mild seizures. The mental state is constantly deteriorating: apathy develops, the range of interests narrows, memory, speech, and attention suffer. Dementia is the final stage of encephalopathy.
Each type of encephalopathy, which may initially have been unspecified, develops its own symptoms.
Vascular form
Develops in older people due to problems with blood vessels, less common in adults 30-50 years old. The vessels of the neck, head, and upper half of the body suffer. At stage 2, it manifests itself with pronounced neurological symptoms: shuffling, instability, tremors, urination problems, disorientation.
Post-traumatic encephalopathy
Appears at different ages due to injuries, accompanied by severe nausea and headaches, as well as severe fatigue. Medicines only provide temporary relief. Attacks of falling, convulsions, asthenia, as well as problems with mental activity are possible.
Hypertensive form
Appears during a hypertensive crisis or from constant exposure to high blood pressure. Characterized by unclear speech, muscle weakness, and marked slowness in movement. Patients may experience headaches and deteriorating swallowing functions.
Venous form
The predominant symptoms are those affecting memory and intelligence, as well as thought processes. In the hot season, chills may occur with venous encephalopathy. The patient is bothered by a cough and heaviness in the head. Facial puffiness and pallor may appear.
Toxic form
Unspecified toxic encephalopathy is characterized by convulsions, a feeling of stupor, problems with breathing and circulation. Nausea, weakness and pressure changes, combined with difficulty controlling urination or bowel movements, can be chronic.
Severe poisoning in almost all cases is accompanied by loss of consciousness, hallucinations, and delirium. In advanced forms of the disease, death often occurs.
Alcohol form
Included in the group of intoxication encephalopathy, accompanied by delirium tremens (delusions and hallucinations). If the disease is chronic, then after a few months of constant alcohol consumption, tremors, weakness, anxiety, depression and personality disintegration appear.
Leukoencephalopathy
A form of the disease in which nausea, severe pain in the head occurs, and a person suffers from hallucinations, phobias and obsessive fears. All brain functions are inhibited.
Metabolic encephalopathy
Occurs with attacks of confused consciousness. The person becomes sluggish and has difficulty with processes such as speaking and performing everyday activities. Over time, drowsiness and hallucinations develop, and the patient falls into a coma.
Acute encephalopathy
Rarely occurs in an unspecified form. Severe and extensive brain damage appears, which means its rapid death after a stroke or edema. Symptoms of the acute form overlap with other diseases and do not allow an accurate diagnosis to be made without additional research.
Features of encephalopathy in children
The diagnosis of unspecified encephalopathy is most often made in infants under 6 months of age. However, it can only be confirmed after tests.
In a child, the disease occurs in 3 degrees:
Easy . Crying, excitability and constant anxiety appear. Sleep deteriorates, stress levels increase, appetite decreases, and vomiting attacks become more frequent. Muscle tone changes significantly, and sometimes strabismus develops.
Average . The functioning of the nervous system worsens: blood pressure rises, convulsions and hydrocephalus appear. The child’s skin becomes marbled, the eyes become slightly closed, as in “setting sun” syndrome. The child almost always presses his arms and legs to his body. Constant crying and insomnia develop.
Heavy . There is a complete suppression of brain functions, consciousness is impaired. The baby falls into a coma. In most cases, death occurs.
Childhood encephalopathy often leads to complications. In adults they also develop in 80% of cases.
Mechanism of occurrence
Any type of encephalopathy develops according to a similar scenario. Oxygen starvation and disruption of physiological metabolic processes in nervous tissue lead to degeneration of brain cells, accompanied by their death. This process is diffuse and is observed both in the cortex and subcortical formations. At the site of foci of ischemia and demyelination, connective tissue grows, which does not perform the function of conducting impulses. At the same time, multiple pinpoint hemorrhages occur in the brain parenchyma.
Damaged neurons fail, and accordingly the tasks they perform are lost and motor and mnestic disturbances characteristic of encephalopathy occur.
Provoking factors
Encephalopathy can appear due to infection of the cortical and other layers of the brain. Tissue damage occurs both during fetal development due to infection of the mother (herpes and other viruses), and after birth.
Signs of encephalopathy often appear some time after traumatic brain injury. A pathological condition develops if a person with a TBI does not receive qualified medical care.
Encephalopathy becomes more pronounced when the death of neurons is caused by cerebral hypoxia. Oxygen starvation is caused by the following factors:
- abnormal position of the fetus;
- severe illness in a pregnant woman;
- pulmonary failure;
- overwork;
- damage to the aorta and others.
In elderly patients, encephalopathy occurs as a complication of hemorrhagic stroke or coronary heart disease. Pregnant women experience damage to brain structures due to acute hypertension.
Encephalopathy also occurs as a consequence of clinical death, in which breathing temporarily stops. It is quite difficult to identify common causes of the syndrome. This is explained by the fact that some factors trigger necrotic processes, while others accelerate them.
The risk group includes elderly people, which is explained by a decrease in the elasticity of the walls of blood vessels as a person ages.
Sometimes the causative factor cannot be diagnosed. In this case, we talk about the course of unspecified encephalopathy.
ICD-10 code
Encephalopathy unspecified in children and adults is encrypted in the list of diseases of the nervous system ICD-10 under code G93.4. This diagnosis is valid in the case of an initial examination before identifying the main reasons that provoked the pathology, as a preliminary conclusion. And also, if, as a result of a survey and a thorough examination of the patient, the etiological factor of the disease was not identified. Statistics show that this form of the disease occurs in approximately 4% of the population, and men are affected by it 1.5 times more often than women.
Residual encephalopathy
This type of disease is spoken of if brain damage does not appear immediately. This disease can occur as a consequence of perinatal encephalopathy. The difficulty in detecting pathology is explained by the short-term and insignificant manifestation of symptoms. Residual encephalopathy can develop as a result of a perinatal form not immediately detected or other causes (high blood pressure, traumatic brain injury, infectious and inflammatory diseases). In the second case, it is customary to talk about acquired encephalopathy, which is divided into subtypes: vascular, discirculatory, metabolic, radiation, toxic, post-traumatic. Discirculatory atherosclerotic encephalopathy is considered the most common.
Symptoms of encephalopathy depending on the stage of the disease
Manifestations of encephalopathy depend entirely on the stage of the disease:
- The first degree of pathology is characterized by a predominance of subjective signs over objective ones. Patients complain of increased fatigue, general weakness (even in the morning immediately after waking up), persistent headaches, weather sensitivity, dizziness, staggering while walking. Among the obvious symptoms of the disease, others may observe deterioration in memory and concentration, irritability, unmotivated anxiety, sleep disturbances (drowsiness during the day and insomnia at night). When examining the neurological status, asymmetrical activation of reflexes, postural instability, slowness of step, and mild pseudobulbar syndrome (impaired swallowing and speech) are detected.
Often this stage of pathology goes unnoticed in infants, since children are not able to describe their sensations, and external examination during this period is uninformative.
- The second degree of encephalopathy is characterized by the manifestation of clear cognitive and motor deficits. Patients cannot plan the sequence of their actions, so it is difficult to perform targeted movements. Memory impairment worsens, and its long-term component begins to suffer. Speech, coordination, and walking disorders increase. In 30-35% of patients, an apathetic or depressed mood is observed, and criticality of what is happening decreases. Neurogenic pathology of urination also appears, expressed in its frequency at night.
- During the third stage of the disease, a person completely loses his ability to work and the ability to adapt socially. Patients at this stage become disabled people of the first group and require round-the-clock monitoring and care. The patient is not able to objectively assess his condition; there is a sharp change in mood from tearfulness to aggression. Postural deficit reaches its maximum - most attempts to walk end in falls. Severe tremor develops as a result of vascular parkinsonism, and sensitivity and movement in the limbs are also impaired against the background of paresis and paralysis.
If you let the disease take its course and do not seek medical help, the transition from the first stage to the last can take only a few years.
Hepatic encephalopathy. Symptoms
Treatment of encephalopathy depends on the stage and type. Acquired forms of pathology include hepatic encephalopathy, which most often occurs as a result of liver failure. The main reasons that can lead to the development of this complex disease include the following: alcoholic, toxic, viral hepatitis, liver ischemia, poisoning with drugs, poisons, mushrooms, alcohol, severe bacterial infections in pregnant women. In 10 percent of cases, the cause of the disease cannot be determined. Hepatic encephalopathy, symptoms, the treatment of which depends on the period of development, can result in endogenous hepatic coma for the patient.
Hepatic encephalopathy in chronic diseases occurs against the background of portosystemic shunting, intestinal diseases, infectious diseases, alcoholic excesses, surgical interventions, paracentesis, forced diuresis. One of the important roles in the development of hepatic encephalopathy is assigned to parenchymal (hepatocellular) failure.
Staging
Another method of classification is based on an assessment of the severity of the disorder. In this case, three stages are distinguished.
- First. It is characterized by a practically asymptomatic course. Minor deviations in the functioning of the brain are detected. Slight fatigue, pain in the cranial area, other deviations. Elimination is possible in a short time.
- Second. Subcompensated. The body is still coping with the redistribution of functions between healthy cells and tissues of the nervous system. However, not completely, dangerous manifestations of the disorder begin.
For example, severe headaches, decreased memory, intelligence, problems with vision, hearing, behavioral changes. High-quality therapy is still possible, but a much longer course will be required with constant monitoring and revision as necessary.
- Third. Critical, decompensated phase. The patient loses some of his abilities and becomes disabled. Restorative measures do not give a 100% result. But with deep rooting of organic changes there is no effect at all.
Attention:
The classification by stages is not considered generally accepted and has a lot of variations. However, they all roughly boil down to this form.
Symptoms in other forms
Toxic effects on brain structures provoke neurological disorders. Swelling of local tissues and an increase in ventricular volume are also possible.
The clinical picture in the traumatic form is determined by the severity of the damage caused. This type of encephalopathy tends to be asymptomatic. The first signs indicating damage to brain structures appear after a certain time period after the injury and manifest themselves in the form of:
The radiation form is characterized by brain dysfunction, including disorders of consciousness and epileptic seizures (rarely diagnosed).
Causes
There are plenty of specific culprits. If we talk about common provocateurs of the disorder:
- Hypertonic disease. Persistent systematic increase in blood pressure.
- Atherosclerosis. Narrowing of the lumen of blood vessels in cerebral structures as a result of spasm or blockage of cholesterol plaques. It occurs frequently, especially in elderly patients.
- Diabetes. Impaired insulin synthesis or decreased sensitivity of body tissues to it. It is always characterized by vascular problems, in all cases and regardless of the form of the process.
- Pancreatitis. Acute or chronic inflammation of the pancreas, with a corresponding decrease in its functions.
- Liver pathologies. First of all, severe hepatitis or cirrhosis, necrosis of organ tissue.
- Disorders of the endocrine system. By type of decrease in the functional activity of the thyroid gland, adrenal glands, etc.
- Alcohol intoxication. Including chronic, with long-term dependence on alcohol.
- Taking drugs. Some species rapidly destroy the nervous system. Like heroin or other opioids, for example. Others have the same effect, but disrupt the central nervous system a little more slowly (cannabinoids).
- Brain injuries.
The list is far from complete. Often structures can be damaged even after resuscitation measures, unsuccessful anesthesia, and other disorders. There are many options.
Forms
They are divided into congenital (prenatal) and acquired.
Purchased
Discirculatory encephalopathy is the most common form. The condition of the blood vessels does not allow blood to circulate normally and deliver oxygen and nutrients to the brain in a timely manner. Brain cells experience starvation, and some of them die.
The causes of toxicity are acute or chronic poisoning. In this case, chemicals act on brain cells and contribute to their destruction.
The post-traumatic form occurs due to severe brain injuries.
The hypoxic form occurs due to oxygen starvation of brain tissue.
Diagnostics
In the case of unspecified encephalopathy, correct and timely diagnosis becomes of enormous importance, as it makes it possible to identify the cause of the pathology and influence it by prescribing adequate treatment.
Physical examination
During the examination, the specialist will pay special attention to collecting complaints, life history and illness in order to clarify risk factors for the development of one or another form of encephalopathy. No less informative is the study of the neurological status, during which paresis, sensitivity disorders, instability in the Romberg position, nystagmus, etc. may be detected. Consultation with related specialists (infectious disease specialist, ophthalmologist, endocrinologist) may also be necessary.
Laboratory research
Laboratory diagnostics are aimed at identifying metabolic or hormonal imbalances that can lead to diffuse multifocal damage to brain tissue. It includes:
- Clinical analysis of blood and urine.
- Biochemical blood test (coagulogram, lipid profile, sugar, kidney and liver tests).
- Test for thyroid hormones (free T4 and TSH).
Instrumental diagnostics
Instrumental diagnostic methods that allow you to verify the etiology of encephalopathy or confirm its unspecified form are:
- Electrocardiography.
- Ultrasound Dopplerography (Doppler ultrasound) of extracranial vessels.
- Duplex or triplex ultrasound examination of extra- and intracranial arteries and veins.
- Electroencephalography.
- CT or MRI of the brain.
To more clearly see lesions in the brain parenchyma using computed tomography, it is necessary to use intravenous contrast with iodine-containing water-soluble substances.
Nutrition
For encephalopathy, preference should be given to products that reduce toxin levels, cleanse and enrich the blood. When consuming products with this effect, patients feel a surge of energy, improved mood, and a positive attitude toward treatment and recovery.
It is recommended to eat with a break of 3-3.5 hours in small portions up to 250 grams. Limiting the amount of food helps avoid self-poisoning of the body with toxins.
50% of the diet should consist of raw, boiled or stewed plant foods. Fried foods should be avoided. A wide variety of fruits and vegetables, especially those containing vitamin C, will be excellent helpers in the fight against the disease.
On this topic
- Encephalopathy
Everything you need to know about residual encephalopathy of the brain
- Natalia Sergeevna Pershina
- March 26, 2020
These are apples, tomatoes, sweet peppers, different types of cabbage, citrus fruits, etc. Be sure to eat greens of any kind. A variety of vegetable oils improve the elasticity of blood vessels.
It is recommended to reduce the consumption of protein products during encephalopathy as much as possible. They increase ammonia levels in the blood and have a toxic effect on brain cells.
It is also recommended to exclude or minimize the amount of sweet, salty and fatty foods.
After biochemical studies, the doctor can give additional nutritional recommendations based on the available results.
The last meal should be 3-3.5 hours before bedtime.
It is better to drink at least 1.5 - 2 liters of water, depending on the time of year. It helps cleanse the blood and blood vessels, removes cholesterol.
Treatment of pathology
Treatment of encephalopathy should be comprehensive and, in addition to the use of medications, include lifestyle modification, giving up bad habits and eliminating the influence of possible risk factors that lead to the development of pathology.
Conservative therapy for an unspecified form of the disease is aimed at improving brain nutrition and protecting cells from harmful environmental influences. The following groups of drugs are used:
Treatment
The fight against the disease is aimed at eliminating the symptoms and causes that gave impetus to the development of encephalopathy. Medicinal and conservative methods are used for therapy.
In the acute form, doctors reduce cranial pressure, eliminate convulsions, and use methods that support life processes: artificial ventilation, hemodialysis, and the administration of nutrients through a dropper bypassing the stomach.
Then the patient is prescribed medications that he takes for 1-3 months:
- lipotropic drugs - normalize the metabolism of fats and cholesterol (Lipostabil, dietary supplements with carnitine, methionine, choline, lecithin);
- angioprotectors - prescribed for heart disease, normalize the walls of blood vessels, improve the movement and outflow of venous blood (Detralex, Troxerutin, Indovazin, Cavinton);
- medications against blood clots (Aspirin, Ginkgo Biloba, Cardiomagnyl);
- neuroprotectors – nourish nervous tissue (Piracetam, B vitamins);
- sedatives and tranquilizers - reduce rapid nerve impulses in affected neurons (Sibazon);
- amino acids, vitamins;
- performance stimulants.
For speedy rehabilitation, the patient is prescribed physiotherapeutic procedures, gymnastics, acupuncture, massage, walks, and a certain daily and rest regimen.
Epileptic encephalopathy, which occurs in young children with an EEG pattern characteristic of epilepsy, stands apart. This only indicates a predisposition to epilepsy, which does not exclude its development in the future. The cause is a violation of brain formation.
Consequences and prognosis for unspecified encephalopathy in children and adults
The prognosis depends entirely on the timeliness and completeness of diagnosis and treatment of the pathology. With adequate therapy, patients live for decades with a compensated form of encephalopathy without feeling any of its symptoms. If the moment of seeking medical help is delayed, the following develops:
- Persistent paresis and paralysis.
- Severe cognitive impairment.
- Sensitivity disorders.
- Deterioration or complete loss of speech skills with the ability to understand spoken words.
- Walking problems, unsteadiness.
In children, untreated encephalopathy can cause mental retardation as well as seizures.
Symptoms of the vascular form
The vascular form of encephalopathy can manifest itself as:
- inability to remember new information;
- headaches, dizziness;
- attacks of nausea and vomiting;
- hallucinations;
- asthenia;
- mental disorders (phobias and others).
Manifestations of the vascular form are also characteristic of dementia. The prognosis for this encephalopathy is extremely unfavorable: in many patients, cerebrovascular accident causes death.
Forecast
Fundamental in predicting the further condition of patients with encephalopathy is its type, severity and degree of brain damage.
In some cases, with timely treatment of the etiological factor, the phenomena of encephalopathy may disappear. In more complex situations, stabilization of the condition is considered a positive prognosis.
The main thing for assessing the prognosis is effective treatment of the underlying disease that caused the development of encephalopathy.
Favorable only at the initial stage. Full recovery is possible without any consequences. The longer the process continues, the worse the prospects.
At the second stage, the forecasts are vague. A cure is no longer possible.
All this is not a sentence. With competent complex therapy, there is a chance to transfer the disease to a sluggish stage and compensate for basic neurological functions.
It is usually possible to delay the onset of the critical phase by 5-10 years. It is possible to maintain the normal state of affairs indefinitely, including until the end of life. This prognosis is called conditionally favorable.
But the 3rd stage is associated with a negative scenario. The data is approximate, too many factors influence the outcome. It is best to obtain detailed information from your doctor.
Diabetic encephalopathy
Pathology is a lesion of the central nervous system structures that develop against the background of diabetes mellitus as a result of metabolic disorders. The causes of the disease are metabolic disorders and diabetic microangiopathy. Elderly patients and those who have problems with excess weight are at risk. Patients with elevated sugar levels, lipid imbalance, and elevated levels of lipid peroxidation are predisposed to the development of diabetic encephalopathy.
Diabetic encephalopathy, the symptoms of which are associated with diabetes mellitus, threatens to disrupt the structures and permeability of the walls of small vessels that affect the functioning of the brain. As a rule, this type of encephalopathy occurs after many years of diabetes.
Disease prevention
Prevention of the disease consists of following simple rules, namely:
- Quitting smoking and drinking alcohol.
- Complete treatment of infectious diseases.
- Maintaining a daily routine (sleep at least 6 hours a day).
- Proper nutrition and rational physical activity.
- Eliminating the influence of toxins on the body.
Comprehensive prevention in most cases avoids encephalopathy. However, when the first symptoms of brain damage appear, you should consult a doctor as soon as possible and undergo a quality examination. Timely treatment will delay the progression of the pathology and improve the prognosis of the disease.
Recommendations
Dead brain cells cannot be restored. Therefore, a patient with encephalopathy needs to make certain adjustments to his daily life.
To stop the development of pathological processes, you should:
- spend more time in the fresh air;
- adjust your daily diet in favor of proper nutrition;
- reduce body weight;
- drink up to two liters of fluid per day;
- Do not take pills that are not approved by your doctor.
The patient's diet includes avoiding consumption of salt and foods with unsaturated fats. These preventative measures are not a substitute for traditional treatment. However, following these rules reduces the risk of complications, such as:
- psychological and neurological disorders;
- hypertensive-hydrocephalic syndrome;
- disturbance of nervous regulation.
Encephalopathy develops under the influence of many factors. This condition is characterized by a variety of symptoms. Treatment is selected taking into account the causative factor and is designed to stop the development of brain cell necrosis.
The most serious diseases for humans are pathologies associated with the brain. Such diseases include encephalopathy, the symptoms of which appear from the first minute of birth. This disease is extremely serious and cannot be treated slowly. It can be fatal if you do not fight it in time. Encephalopathy refers to pathological processes in the brain. This does not include inflammatory lesions and changes.
Prevention
Doctors say the main way to prevent the development of encephalopathy in a baby is a woman’s thoughtful and responsible attitude towards pregnancy. In the presence of chronic diseases, it is necessary to compensate for all conditions and prevent the development of exacerbations. During pregnancy, women should follow a routine, rest, walk, and breathe fresh air. When visiting an obstetrician-gynecologist, problems should be reported in order to exclude fetal hypoxia, prepare for childbirth, and avoid intrapartum trauma.
Perinatal encephalopathy is a disease of the newborn that can be avoided if the woman is careful and maintains a healthy lifestyle. If a diagnosis is made, you should follow the doctor’s recommendations, carry out full treatment, give the baby massage, and exercises to prevent complications.
Encephalopathy in infants
This is not an inflammatory disease of the brain; it is associated with impaired blood supply, reduction and destruction of brain cells.
It can be an acquired disease, as a result of birth trauma, hypoxia, which leads to serious brain disorders, but most often it is a congenital pathology.
This disease is diagnosed in approximately 50% of infants. More severe forms of PPCNS occur in only 10% of newborns.
Premature babies are more vulnerable. Congenital is encephalopathy in an infant, complicated during childbirth (birth trauma, placental abruption, abnormal position of the fetus, a large head in a child, a narrow pelvis in a woman). It can be suspected for the first time immediately after the birth of a child.
At birth, the internal organs, including the central nervous system, are not fully developed; the development of all systems requires a period of time. There are several forms of encephalopathy.
Perinatal encephalopathy in newborns.
It is considered from the 28th week of pregnancy to the 8th day of the child’s life. It can occur if (causes of encephalopathy):
- The child's mother is too young or old.
- Abortion.
- Miscarriages.
- Infertility treatment.
- Mom's diabetes.
- Mother's heart defects.
- Mom's flu.
- Smoking, alcohol.
- Toxicosis.
- Risk of miscarriage.
- Work in hazardous production.
- Taking medications.
- Fast (less than 6 hours, slow more than 24 hours) labor.
- C-section.
- Premature placental abruption.
- Umbilical cord entanglement, umbilical cord prolapse.
- Multiple birth.
Periods of perinatal encephalopathy in newborns.
- The acute period is 7-10 days to a month.
- Early recovery period up to 4 – 6 months.
- Late recovery period up to 1 – 2 years.
In the acute period, the following are observed: lethargy, muscle hypotonia, decreased reflexes (sluggish sucking) or, conversely, hyperexcitability of the nervous system (shallow sleep, trembling of the chin and limbs), throwing the head back.
The early period of perinatal encephalopathy in newborns, when general cerebral symptoms decrease and focal brain lesions appear. Muscle hypotonicity or hypertonicity appears.
Paresis and paralysis, hyperkinesis are possible (enlargement of the head, expansion of the venous network on the forehead, temples, enlargement and bulging of the fontanelle.
Marbling and pallor of the skin, cold hands and feet, changes in the gastrointestinal tract (constipation, diarrhea, increased gas production), disturbances in the rhythm of the heart and breathing.
Late period of perinatal encephalopathy in newborns, muscle tone and other functions gradually normalize. Dynamic development occurs in the central nervous system and psyche of the child. Pre-speech and speech development is being formed.
At this age, you can already notice that the child is lagging behind, those reflexes and skills that should be there are either not there, or they are very weak, motor skills are sharply delayed, speech disorders, delayed mental development.
There may be persistent spastic syndrome or, conversely, muscle hypotension.
Hypoxic-ischemic damage to the nervous system.
One of the forms of encephalopathy caused by fetal hypoxia (oxygen starvation of brain cells). With chronic intrauterine hypoxia they suffer, the capillaries of the brain grow slowly and become more penetrating.
During childbirth, this leads to asphyxia (severe respiratory and circulatory disorders). Therefore, asphyxia of a newborn at birth is a consequence of fetal hypoxia.
Several degrees of hypoxic-ischemic form of infant encephalopathy :
- Depression and excitation of the central nervous system, which lasts up to 7 days after birth.
- After 7 days, convulsions, increased intracranial pressure, and disturbances in heart and respiratory rhythm are added.
- Severe convulsive condition, high intracranial pressure.
Mixed lesion disease.
In addition to hypoxic-ischemic damage to the central nervous system, intracranial hemorrhages (not traumatic) are added; the severity depends on where the hemorrhage occurred.
Traumatic damage to the central nervous system.
Damage to the spinal cord during childbirth, this can happen if the fetus is large or incorrectly positioned. When it is easier to remove the head and shoulders, when the head is diligently turned when it is removed, or when it is pulled behind the head, the obstetrician performs these manipulations to reduce the child’s hypoxia.
It all depends on the experience of the doctor. Damage can also occur during a caesarean section with a “cosmetic incision” that is not sufficient to remove the child’s head. Artificial ventilation of the lungs in the first 2 days can lead to damage, especially in premature and low-weight children.
Metabolic disorders.
Alcohol syndrome, nicotine, drug disorders occur as a result of the cessation of the intake of alcohol, nicotine, and drugs.
Intrauterine infection.
Depends on the type and severity of the disease. Such children are often born in a state of asphyxia, with low weight, an enlarged liver, developmental defects, and there may be a convulsive syndrome.
In the maternity hospital, neonatologists examine newborns and identify perinatal damage to the central nervous system and prescribe treatment. But this treatment must be continued at home.
What should alert the mother: frequent restlessness of the child, regurgitation, trembling of the chin, arms and legs, freezing of the child in one position, unusual eye movements, rapid head growth of more than 1 cm per week, enlargement of the edges of the fontanel and its bulging.
If your baby has something, you need to consult a neurologist, the sooner the better, and begin treatment to fully restore your baby’s health.
Treatment of encephalopathy in infants.
Treatment is usually complex, it begins after a complete examination of the baby, for this you need to pass tests:
- Complete blood count
- Blood chemistry
- Complete urine analysis
Take examinations:
- NSG (neurosonography)
- EEG (encephaloelectrography)
- MRI (magnetic resonance imaging)
- Cerebrospinal fluid
- Neurologist
- Oculist
With proper treatment and a timely diagnosis encephalopathy in infants is well treated, treatment is carried out both at home and in the hospital, it all depends on the severity of the disease, but treatment is carried out over a long period of time and in courses.
Drugs are prescribed to restore the structure of the brain, improve blood supply to the brain, B vitamins (Magne B6, Magnelis), sedatives, drugs that treat symptoms: for seizures, anticonvulsants (Konvulex, Finlepsin, Depakine), drugs that relieve muscle hypertonicity, as well as drugs that treat movement disorders.
Other drugs can be prescribed intramuscularly and intravenously. Electrophoresis is well used for the treatment of encephalopathy (if there is no history of seizures), neurologists like to prescribe physical therapy, massage, and herbal medicine.
One of the important principles of treatment is: a daily routine with alternating sleep and wakefulness, mandatory walks in the fresh air, and proper balanced nutrition. If you follow all the principles of treatment and regularly visit a neurologist, pediatrician, or physiotherapist, most children have a chance of a full recovery, without consequences in adulthood.
With a diagnosis of encephalopathy, children are registered at a dispensary for further observation at least twice a year.
Consequences of encephalopathy in a newborn.
With severe damage to brain cells, poor or untimely treatment, complications arise:
- Neuroses.
- Epilepsy.
- Cerebral palsy.
- Dementia.
- Possible depression.
- Strabismus.
- Migraine.
- Hydrocephalus.
- Schizophrenia in adolescence.
- Fainting.
- Dizziness.
- Motor impairment.
Therefore, it is very important to begin treatment of encephalopathy as quickly as possible and follow all recommendations of specialists.
Prevention of encephalopathy.
During pregnancy, the mother should monitor her health, receive adequate nutrition, not have bad habits or avoid them, regularly attend antenatal clinics, and take vitamins.
To prevent the child from receiving a birth injury, you must listen to the obstetrician’s recommendations and follow them.
Source: https://vseprodetok.ru/zdorove-rebenka/encefalopatiya-u-grudnichka/
Treatment methods and drugs
The therapeutic course for encephalopathy is prescribed on an individual basis. When choosing the necessary drugs and procedures, the age of the child, the general clinical picture of his health, the causes of damage to brain neurons and the degree of progression of the pathology are taken into account.
Self-medication for encephalopathy should be excluded. Otherwise, it will be impossible to get rid of its complications.
When treating encephalopathy, the following drugs and procedures may be prescribed:
- Nootropic drugs (Piracetam, Actovegin).
- Means for relieving motor dysfunctions (Dibazol, Galantamine).
- Amino acids (Methionine, Cerebrolysin).
- Painkillers (Bellaspon).
- Drugs for the treatment of hypertensive-hydrocephalic syndrome (Furosemide).
- Medicines against hypertension (Baclofen).
- Preparations of the lipotropic category (Essentiale).
- Drugs in the category of neuroprotectors (Thiocetam).
- Tranquilizers and sedatives (Sibazon).
- Vasodilators (Papaverine, Drotaverine).
- Sedatives (Elenium, Glycine).
- Infusion therapy (glucose, calcium, ascorbic acid).
- Exercise therapy and therapeutic massage.
- Breathing exercises.
- Physiotherapy.
- Artificial ventilation (for complications on the respiratory system).
- Surgical intervention (endovascular surgery).
Prognosis and complications
Any encephalopathy is characterized by headache, nausea, vomiting, and dizziness.
In the case of severe damage or swelling of the brain, a serious violation of microcirculation, encephalopathy develops acutely, severe headache appears, especially in the back of the head, dizziness, restlessness, anxiety, blurred vision, staggering, and possible numbness of the ends of the fingers, nose, lips, tongue. Subsequently, anxiety replaces lethargy and clouding of consciousness.
In acute forms of hepatic, pancreatic and renal encephalopathy, disturbances of consciousness and convulsive seizures are common.
In encephalopathy caused by pneumonia (including exacerbation of the chronic form), heart attack, pulmonary embolism, eye movements not controlled by consciousness, decreased muscle strength, and mental disorders are observed.
Among the typical complications of all encephalopathies are:
- convulsions;
- paralysis;
- to whom.
If you follow the doctor's recommendations, the prognosis is favorable.
Advanced cases of the disease threaten:
- epilepsy;
- paralysis, movement disorders;
- loss of brain functions, intelligence, memory;
- emotional instability, mood swings, depression;
- disability.
Toxic encephalopathy is the most severe and has the worst consequences.
Due to the fact that one type of disease contains many special cases that are classified as a separate type, the symptoms of different encephalopathies are similar and it is often impossible to establish the cause of the disease. The insidious enemy is fraught with life-threatening complications and requires constant monitoring by a specialist and long rehabilitation.
How to detect the development of encephalopathy: main symptoms
In infants, as well as older children, the occurrence and development of brain diseases not associated with inflammatory processes can be identified by the following symptoms:
- an increase in the size of the brain and, accordingly, the head, called hydrocephalus. It is detected in children under 1 month and is a consequence of insufficient outflow of cerebrospinal fluid and venous blood;
- sleep problems. If the baby does not want to sleep or confuses day with night (sleep inversion), then parents should take care of conducting a brain examination. The thing is that similar symptoms very often occur with encephalopathy caused by poisoning with toxic substances;
- the baby’s lack of any interest in the world around him, as well as in games and traditional fun. Doctors call this phenomenon a decrease in cognitive activity and consider it one of the most striking symptoms of brain disorders in newborns;
- problems with short-term memory. When they occur, the child quickly forgets objects, colors, letters and numbers. This symptom can be detected at an older age;
- a newborn baby refuses to breastfeed, cries constantly, shows anxiety, sleeps very poorly;
- frequent headaches in a child after one year;
- the appearance of unreasonable fears in children. The most common of these are claustrophobia and arachnophobia (fear of closed spaces and spiders, respectively).
All of the above symptoms can be more or less pronounced, depending on the severity of brain disorders. Therefore, it is very important to carefully monitor the child’s behavior and consult a doctor after identifying any pathologies.
The main methods for detecting encephalopathy today are magnetic resonance imaging (MRI) or computed tomography, as well as studies such as neurosonography and electroencephalography.
Epidemiology
The disease is more often diagnosed in middle-aged and elderly people. It occurs at any time of the year; certain types of encephalopathies (toxic, infectious) are observed during the cold season.
Infectious encephalopathy occurs under the influence of various pathogens (rubella, tetanus, HIV, mad cow disease). In the latter case, the disease is most severe and is called spongiform encephalopathy.
With constantly elevated pressure, brain neurons die. The result is hypertensive encephalopathy, a serious illness that often ends in death.
Read more about the treatment of cerebral encephalopathy in the elderly.
Discirculatory encephalopathy is a slowly progressive disease of the brain. Read about an integrated approach to treating the disease on this page.