Cortical atrophy of the brain is a devastating, irreversible change that most often affects people between 50 and 55 years of age, although there are cases of cortical atrophy in newborn infants. Pathological disorders, as a rule, manifest themselves in the frontal lobes of the brain, which are responsible for the thinking process, human behavior, and control. The disease progresses slowly with a gradual increase in the main symptoms, which ultimately leads to the emergence and development of senile dementia.
Causes of leukomalacia
The brain of premature newborns is very sensitive to a lack of oxygen, since compensatory mechanisms have not yet developed, and the microvasculature cannot provide blood delivery in a timely manner. In full-term babies with a more or less mature nervous system and blood flow, hypoxia stimulates blood circulation, so the damage will not be as pronounced.
Option for the development of intrauterine hypoxia (oxygen starvation) due to insufficiency of placental blood flow
The problem is aggravated by the fact that premature babies do not have a good connecting network between the arteries of the brain, and the subcortical region around the ventricles, at a distance of up to 1 cm from their walls, is especially affected, more so in the parietal zones. This explains the periventricular (near the ventricles) location of the foci of necrosis.
Hypoxia causes the formation of free radicals, acidic metabolic products, which not only have a direct damaging effect on neurons, but also contribute to disruption of microcirculation in the form of thrombosis, stagnation of blood in small arteries and veins. Thus, hypoxia, which itself causes necrosis, provokes metabolic disorders and thrombosis, which further aggravate the situation.
It has been noted that periventricular encephalopathy develops more often in children who were on artificial pulmonary ventilation (ALV). It would seem that the device provides breathing and oxygen delivery, so the brain should not suffer. However, excess oxygen supplied through the device provokes spasm of the arterioles, which leads to ischemia.
The frequency of LP among newborns depends on the time of year. Typically, a greater number of such patients occur in the winter-spring period. A possible reason is considered to be a lack of vitamins and the influence of unfavorable weather conditions on the body of a pregnant woman in late gestation.
Risk factors for leukomalacia are:
- Severe gestosis;
- Chronic infections in pregnant women;
- Intrauterine hypoxia due to disturbances in the placenta or blood flow to the fetus;
- Anomalies of childbirth - premature birth, premature rupture of water, weakness of labor forces;
- Pathology of newborns – respiratory distress syndrome, pneumonia requiring mechanical ventilation.
Brain damage. Periventricular hemorrhagic infarction (PVI)
Brain damage. Periventricular hemorrhagic infarction
Periventricular hemorrhagic infarction (PVI), also called widespread red softening, venous infarction, cerebral hemorrhagic encephalopathy, periventricular hemorrhagic lesion, and hemorrhagic periventricular leukomalacia, occurs predominantly in very preterm infants (20–35 weeks of gestation). ) and occurs as a result of a violation of the outflow of blood (stasis-thrombosis) in the system of internal cerebral veins. With thrombosis of the vein of Galen, massive bilateral hemorrhagic softening of the semioval centers occurs. However, less significant lesions are more common. PGI is often observed in children with infections, which play an important role in their pathogenesis.
The term PHI has not yet entered into widespread practice among clinicians, who more often use the concept of “periventricular hemorrhage” (PVH). Thus, during an NSG study in children with perinatal lesions of the central nervous system, PVCs are detected in 11% of cases. Probably, part of the ICH is PHI, while the other part may be represented by periventricular ICH and OHL.
Macroscopic examination: in the periventricular areas of the lateral ventricles, usually in symmetrical sections, large areas of flabby dark red tissue are found. PHI is not a simple hemorrhage, it is “soaking” of the periventricular white matter of the brain with blood in combination with its edema and incomplete necrosis.
Along the periphery of the lesions, hypertrophied astrocytes, fat Nissl astrocytes, and sometimes foci of PL are detected. In the early phase of the process, dying gliocytes (most likely oligodendrocytes) are found around the hemorrhages, the nuclei of which take on the shape of hooks and commas.
Thrombi are often found in subependymal and cortical veins, as well as in infarct areas. Single leukocytes may be detected around hemorrhages. PGI, unlike ICH, is bilateral, symmetrical and, to a greater or lesser extent, involves all lobes of the brain. Occasionally the process spreads to the entire semi-oval center.
PGI can cause death. PHI is usually combined with SEC, ischemic lesions of neurons in the cortex and brain stem.
Microscopically, numerous crowns and stitches are detected, often around blood clots of small vessels, alternating with areas of edema and foci of necrobiosis of brain tissue. PHI can be complicated by intracerebral hemorrhage (hematoma) and IVH. In surviving children, numerous cysts with hemosiderosis and gliosis of the white matter of the brain form at the site of PGI.
Issues of etiology, pathogenesis and clinical picture of PGI are still in the early stages of study. Therefore, we should dwell on the research of A. Tovbin, who devoted the largest number of works to PGI. The author distinguishes “periventricular venous infarctions” in premature infants and “cortical infarctions” in full-term newborns.
He believes that as a result of ante- and intranatal hypoxia or respiratory disorders in newborns (hyaline membranes, pneumonia), circulatory disorders occur in the brain with venous stagnation and stasis-thrombosis in the veins, which lead to hemorrhagic necrosis of the brain and intraventricular hemorrhages. Periventricular leukomalacia A.
Tovbin considers it as one of the forms of heart attacks or as micro-infarctions. The author believes that when hypoxia and cerebral circulatory disorders are less pronounced, small damage occurs in the periventricular areas of the brain in the form of two forms: foci of hemorrhages in the subependymal matrix and foci of periventricular leukomalacia.
Their pathogenesis is the same as that of large hemorrhagic venous infarctions. Since foci of PL were often found around hemorrhagic infarctions, A. Tovbin calls them “companions” of the latter. Thus, although A. Tovbin considers LP within the framework of venous infarctions, he still differentiates these two types of necrosis.
Venous hemorrhagic infarctions differ sharply from LPs macroscopically: they represent large fields of flabby brain tissue soaked in blood. At the same time, they should be differentiated from such a complication as massive hemorrhages into the foci of LP.
In surviving children, gliosis and cysts form in the areas of PGI, and the lateral ventricles of the brain expand. Cerebral palsy develops with hemiplegia, quadriplegia and mental retardation.
Terminology problems. It should be noted that when describing the lesion in question, other authors use different terms. Thus, S.V. Courville calls such a pathological process “widespread red softening” and “cerebral hemorrhagic encephalopathy,” considering it a fatal lesion that quickly leads to death. R.L.
Friede notes that with thrombosis of the vein of Galen, massive bilateral hemorrhagic softening occurs in the semiovale center. J. K. Larroche describes periventricular hemorrhagic infarctions in the section of cerebral hemorrhages, linking them with leukomalacia or with ischemia of the deep parts of the white matter of the cerebral hemispheres. J. W. Wigglesworth, K. E.
Rarely believe that periventricular venous infarctions in most cases are secondary to massive subependymal hemorrhages. J. Volpe refers to such lesions as “periventricular-intraventricular hemorrhage.”
Lesions that look like periventricular hemorrhagic infarctions are also called “hemorrhagic periventricular leukomalacia,” which includes cases of a combination of LP with hemorrhages of various sizes. Thus, there is not only terminological confusion, but also insufficient understanding of the essence of the pathological process under consideration.
I believe that PHI should be differentiated from periventricular ICH, as well as from cases of hemorrhage into the foci of periventricular leukomalacia.
Source: https://oborudka.ru/handbook/87.html
What happens in the brain during leukomalacia?
With leukomalacia of the brain, foci of necrosis appear in the subcortical structures, usually coagulative, nerve cells die, and the defects are replaced by multiplying microglial cells, similar to how scars form in other organs. Neurons cannot reproduce, and the brain has nothing to fill the dead fields with, so the result is cysts (cavities) - cystic leukomalacia.
More than half of cases of LP are accompanied by secondary hemorrhages in the area of ischemia and necrosis; hemorrhages into the ventricles of the brain are possible. It is important that the cerebral cortex in such children is affected extremely rarely due to good blood supply.
Leukomalacia begins in the first days and lasts about a week from the moment of birth. Its later occurrence is also possible, usually associated with infection or breathing problems in a newborn child. In these cases, against the background of existing necrosis, new ones may appear, and the child’s condition will progressively worsen.
Foci of multifocal leukomalacia with a diameter of 2-3 mm are found in the parietal and frontal lobes, symmetrically, around the walls of the lateral ventricles. Less commonly, the temporal and occipital lobes of the brain are affected. The outcome of necrosis is the formation of many cysts of different sizes, scattered throughout the subcortical layer of the brain (cystic degeneration), the number of which increases over time. In severe PL they occupy the entire periventricular part of the hemispheres.
We are trying to understand the results of MRI of the brain
We are trying to understand the results of MRI of the brain
- Doc
- 11-09-2015
- VSDshnik's Directory
About how many wonderful discoveries... MRI is preparing for us. Conclusion: lesions in the white matter.
What kind of bullshit is this and what does it threaten?
So, to begin with, let me remind you that I was prompted to do an MRI of the brain by bad symptoms that did not stop for three months.
I'll try to describe the symptoms:
Systemic, almost never-ending mild dizziness, almost imperceptible, but very unpleasant. Constant “fogginess” of perception of the surroundings, “stuckness” and lethargy in the head - I can’t describe it better. Sometimes “skidded” on turns, could “not fit” into the door frame , touch the corner of the table, etc.
Not often, but, as they say, I noticed. My ability to work has deteriorated quite noticeably - let me remind you that my main tool is a computer. It has become hard to work, that’s not the right word... Chronic fatigue - by the end of the day you can’t do anything at all, just drive away bad thoughts about your worthless health.
Problems with sleep – I began to wake up periodically early and could no longer fall asleep. In my case, early is 5 am, I usually slept until 6.30 – 7 am. I go to bed quite early, at 23:00, and someone will say that this is quite enough, but I know how much I need... I have become very sensitive to “lack of sleep”.
By the way, chronic early awakening is one of the main complaints to this day, but it has only gotten worse. But this will be a separate story... Periodic, but not frequent and not severe headaches.
Quite long-lasting (2-5 hours), mainly in the hemispheres and frontal region, there were no occipital pains.
With this “set” I decided to go for an MRI of the brain. Why go straight to an MRI without any referrals from a neurologist? Most likely, the fact that just before I developed these symptoms played a role was the fact that my ex-wife died of cancer. The story is a little different and quite long, I won’t tell it all, I’ll just say what concerns the topic of MRI.
So, as far as I know, her complaints were very similar to mine: no “wild” headaches, dizziness, unsteady gait, etc. As a result, based on the results of an MRI of the brain, she was diagnosed with a tumor (or metastasis to the brain, I can’t say for sure). So I decided that before seeing a neurologist, I had to “dot the I’s,” which is what I did.
It was scary - beyond words!
Now the results. The MRI conclusion (2007) states: MRI picture of a single lesion in the white matter of the brain - probably of vascular origin. Signs of moderate external hydrocephalus. For the general picture, here is a scan of the full text of the research result:
The doctor who wrote the conclusion did not find anything “military” in the study, did not see any tumors or neoplasms. Regarding the “Single lesion in the white matter,” he didn’t turn a blind eye, he said that most likely it was the result of a hypertensive crisis or even congenital, it couldn’t pose any particular threat and could hardly be the cause of my dizziness.
Later, while looking at the MRI results saved on DVD at home, I found this “black hole” in my head:
At the appointment with the neurologist, it was generally not possible to clarify the picture. I did not receive any specific comments about the single lesion, or about hydrocephalus, or even about the “black hole”. Everything is in general terms, like “nothing fatal.” General recommendations, etc. and so on.
Moreover, I visited two neurologists. They prescribed Cerebrolysin, vitamins and sedatives. They told me to periodically monitor him and do an MRI about once every two years to monitor his dynamics. They seem to have calmed down, but on the other hand, there are no concrete measures.
Doctors, of course, know better, but it’s alarming.
There were no changes, much less improvements in my condition. I took the prescribed courses - in vain. Over the years, I performed 4 more MRI studies of the brain. The picture remained almost unchanged. Here are excerpts from the MRI report (2012):
The wording “single” was somewhat annoying, i.e. in plural. The next visit to the neurologist calmed me down a little - I saw practically no reaction to the wording of the conclusion.
Here is the latest study, I present its results in full, because... I noticed (in my opinion) very bad dynamics. MRI GM 2013:
I highlighted with a yellow marker the point that made me worry. On the first MRIs, single lesions were 0.3 cm, but here the figure was already 0.4 cm.
Of course, I understand that I am getting older and my health is not getting better, but the picture was still depressing. Another appointment with a neurologist - again nothing.
The doctor explained the increase in lesions “most likely due to an error or different resolution capabilities of the devices.” Well, what to do is to believe... Moreover, it is more profitable than thinking about the bad.
Plus, a lipoma of the interhemispheric fissure appeared. Just some kind of kick-ass...
The last visit to the neurologist ended with another course of Cerebrolysin (now intravenously) and Mexidol intramuscularly. Plus 20 days of taking Tagista. Plus, the conversation again turned to antidepressants. But more on that later...
On my last visit, I asked the doctor a question about multiple sclerosis. The neurologist categorically denied the diagnosis of MS, but I will still tell you why I once again had an MRI and why I again saw a neurologist.
I think that many VSD sufferers have gone through similar torment and doubts, so in the next post we’ll talk a little about the symptoms of multiple sclerosis.
Source: //xn--80acgb4aire.xn--p1ai/lib/25-head-mrt.html
Manifestations of leukomalacia
Signs of leukomalacia are varied and often nonspecific, but severe hypoxic damage to brain tissue cannot be asymptomatic. There are several degrees of PL:
- Mild degree - signs of damage to the nervous system persist up to a week from the moment of birth;
- Moderate severity – from 7 to 10 days, convulsions, intracranial hypertension, autonomic disorders are possible;
- Severe PL – deep damage with brain depression, often coma.
Symptoms of cerebral leukomalacia include:
- Excessive neuro-reflex excitability or, conversely, its inhibition;
- Convulsive syndrome;
- Muscle hypotonia;
- Stem symptoms;
- Paresis and paralysis;
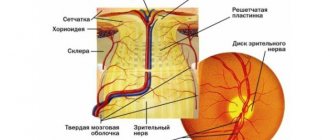
- Visual disturbances in the form of strabismus;
- Delayed psychomotor development, intellectual impairment, hyperactivity, attention deficit.
Experts especially note that neurological symptoms in the acute period and up to 3-5 months of life may not be expressed. In approximately 90% of children, after the acute period, imaginary well-being occurs, lasting up to 5 and even 8-9 months of life. And only after such a long time do signs of a deficit of nervous activity appear against the background of atrophy of brain tissue.
The nerve pathways responsible for the motor function of the limbs are concentrated around the ventricles of the brain, so the main symptom of cerebral leukomalacia in children is cerebral palsy, but its severity depends on the severity of necrosis.
Due to the involvement of the brain stem and cranial nerves, more than half of children suffer from strabismus, more often convergent, swallowing disorders and respiratory disorders are possible. By the age of six months, convulsive syndrome appears. The larger the size of the necrosis fields and, accordingly, the cysts, the more pronounced the brain failure. The nature of the symptoms is determined by the localization of the lesions (motor, visual disturbances, convulsions, mental retardation).
Severe damage to the parietal and frontal lobes leads to cerebral palsy with simultaneous impairment of mental development. If only the pathways responsible for the innervation of the limbs are involved, then paralysis may not be accompanied by impairments in the child’s intelligence and development.
Often, in children who have suffered perinatal hypoxia, symptoms include attention deficit and hyperactivity with intact motor development. This is a relatively favorable variant of the pathology, which can be corrected with special therapeutic measures.
Due to such unpredictability and variety of symptoms, it can be difficult for a mother to figure out what to expect when the baby is born prematurely and under hypoxic conditions. If the damage is moderate or severe, then the child will not develop according to his age - he will not learn to roll over, sit, and, especially, walk in time. Speech development will slow down, the baby will not be able to walk, will not follow toys and will not show such curiosity as is typical for his age.
Particular attention is drawn to hypertension, which can be painful, so the child will be restless, whiny, and sleep will be disturbed. Breastfeeding can be problematic due to a poor sucking reflex, excessive neuromuscular excitability, or atonia.
Poor weight gain, slow growth that is not appropriate for age, and a lack of skills that a growing child needs to master are the main symptoms that parents of a baby with moderate or mild damage to the subcortical structures have to deal with.
By about a year, neurological deficits become noticeable, cerebral palsy develops, and psychomotor development is delayed. After a year, when the recovery period comes to an end, the clinical picture is dominated by such consequences as delayed psycho-speech development, emotional lability, problems with sleep and attention, which can occur along with more severe motor disorders (cerebral palsy).
PL in adults can cause cerebral palsy, hypertonicity, intellectual impairment, and severe mental retardation . With a favorable course of the pathology, adults are not much different from others.
MRI diagnosis of multifocal brain lesions
[▼]:
multiple sclerosis
hypoxic encephalopathies migraine traumatic brain injury progressive multifocal leukoencephalopathy acute disseminated encephalomyelitis note Relevance
. In recent years, the widespread introduction of the latest neuroimaging methods has expanded the possibilities of studying neurological processes that are manifested by multifocal changes in the brain. Differential diagnosis of such changes presents significant difficulties. High tissue contrast, the possibility of multi-planar imaging, lack of radiation exposure, and non-invasiveness make magnetic resonance imaging (MRI) the method of choice. However, a number of vascular, inflammatory, infectious and hereditary diseases may have a similar MRI picture. The term “demyelinating diseases” (DD) of the central nervous system usually refers to primary, usually idiopathic, pathological processes that cause destruction of normally developed myelin. Processes such as vascular (dyscirculatory, hypertensive) encephalopathy, vasculitis, a number of infectious diseases, neurotrauma, degenerative diseases of the nervous system and many others also cause loss of myelin in pathways, which is accompanied by corresponding changes in signal characteristics on MRI. But these processes have a different etiology and pathogenesis, which does not allow them to be included in the group of DD.
► Multiple sclerosis
(MS) is a chronic, progressive disease of the central nervous system, manifested by diffuse neurological symptoms and, in typical cases, having a remitting course in the initial stages (Adams R., 1993).
MRI is highly sensitive in detecting lesions of MS, significantly exceeding the capabilities of both clinical examination and other neuroimaging methods.
However, the specificity of MRI in diagnosing MS is no more than 80%, which is due to the fact that lesions in the white matter, similar to lesions in MS, can be observed both in healthy individuals and in patients suffering from vascular encephalopathy, migraine, vasculitis, bacterial and viral infection and a number of other diseases.
Currently, an international group of experts in the field of MS has adopted the following ► diagnostic criteria
relapsing-remitting MS:
- 1
– one lesion accumulating contrast, or 9 lesions hyperintense on T2 WI;
2
– at least one infratentorial lesion;
3
– at least one subcortical supratentorial lesion;
4
– at least three periventricular lesions.
Diagnosis requires the presence of at least three of the listed criteria. These criteria allow some patients to be diagnosed with multiple sclerosis earlier than standard methods for diagnosing clinically significant multiple sclerosis. In many patients, already in the early stages of the disease, MRI of the brain reveals multiple foci confirming “in situ” dissemination. These may be areas of increased intensity on T2-weighted images (especially when using the FLAIR program) in the white matter and black “holes” on T1-weighted images associated with nerve fiber atrophy. When contrast enhancement is used, active lesions can be identified on T1-weighted images, since paramagnetic contrast accumulates in areas of increased BBB permeability and active inflammation. Typical localization of lesions, usually 0.2–1.0 cm in size, are:
- ♦ corpus callosum, ♦ periventricular white matter, ♦ there may be infratentorial lesions (typically ventral to the fourth ventricle).
Sometimes it is possible for the process to spread to the gray matter - to the subcortical nuclei. The lesion is often asymmetrical and bilateral. Periventricularly located RS plaques are oval in shape and located perpendicular to the lateral ventricles (“Dawson’s fingers”). The perifocal reaction in the form of edema can be weak, only in the “active” phase. MS lesions may accumulate contrast agent, reflecting impaired permeability of the blood-brain barrier. There are 3 types of contrasting plaques in MS (Pronin I.N. et al., 2003):
- ♦ diffuse, ♦ ring-shaped ♦ partial [].
► Hypoxic encephalopathies
. In patients over 40 years of age, small focal brain lesions occur due to hypoxic encephalopathies (dyscirculatory encephalopathy, Binswanger's disease). This is due to atrophy of the myelin sheaths caused by atherosclerotic damage to the arterioles and the resulting chronic hypoxia. This process occurs asymmetrically bilaterally with localization in both deep and subcortical white matter. There is no perifocal reaction. With contrast enhancement, the intensity of the MR signal on T1 VI does not change (there is no accumulation of contrast agent). With dyscirculatory encephalopathy, hydrocephalus often develops, both external (manifested by expansion of the subarachnoid spaces) and internal (enlargement of the ventricular system), due to atrophy of the brain substance.
In contrast to demyelinating processes, in hypoxic encephalopathies there are similar changes in the basal ganglia, zones of glial-atrophic changes after ischemic cerebrovascular accidents or lacunar infarctions, and dilated perivascular Robin-Virchow spaces are visualized. Leukoaraiosis is often detected periventricularly (areas of diffuse increased MR signal on T2 VI in FLAIR mode around the lateral ventricles, often bordering the horns of the ventricles) [].
► Migraine
. Migraine is typical for young patients.
An MRI examination reveals multiple, small (up to 0.5 cm) rounded lesions localized in the white matter of the hemispheres, sometimes in the subcortical nuclei, and are not found subtentorially.
There is no perifocal reaction, no accumulation of contrast agent. The occurrence of such glial changes is associated with the development of vasculopathy of small arterioles [].
► Traumatic brain injury
. With traumatic brain injury, multiple focal changes in the brain substance can be observed. More often, such foci are identified in mild trauma such as a concussion, but sometimes in severe neurotrauma such as DAP (diffuse axonal damage).
The lesions can have different sizes and are most often localized in the splenium of the corpus callosum, pons, and midbrain. In the acute period of injury, they are characterized by the presence of a hemorrhagic component.
In the long-term period, there is no swelling of the brain substance around post-traumatic lesions, no accumulation of contrast agent [].
► Progressive multifocal leukoencephalopathy
. Progressive multifocal leukoencephalopathy develops in individuals with congenital or (more often) acquired immunodeficiency (AIDS, against the background of immunosuppressive therapy). The etiological factor is the reactivation of a latent viral infection.
During an MRI examination, multiple foci are visualized subcortically in the white matter, from small to confluent, of irregular shape, with unclear boundaries on T2 VI (weak edema). Their typical location is the parieto-occipital lobes, but they can be in any part of the brain. The lesion is bilateral, asymmetrical. There is no contrast enhancement of the lesions, but according to ScottW.
, 2002, in 5–15% of patients, peripheral contrast is possible [].
► Acute disseminated encephalomyelitis
.
According to MRI data, a characteristic sign of acute disseminated encephalomyelitis (ADEM) is the presence of foci of demyelination, the number of which decreases during subsequent MRI studies due to partial or even complete restoration of the tissue structure, while in MS the number of foci and their sizes, as well as activity CV accumulations change at each stage of the disease. The ICD values in normal brain tissue of patients with ADEM differ slightly from those in healthy people. On diffusion-weighted images, foci of demyelination are characterized by an increase in MR signal intensity with increasing ADC values in the white matter of the brain [].
► note
. The most informative and promising method for diagnosing multifocal brain lesions is MRI.
It is this that makes it possible to visualize intravitally the multifocal nature of CNS lesions in various diseases and in dynamics allows us to judge the stage of the process in a particular patient.
However, MRI results taken in isolation (without taking into account the clinical picture of the disease) are not an absolute criterion in making a diagnosis. Despite the fact that MRI is recognized as the “gold standard” of neuroimaging, MRI research protocols are constantly being improved and supplemented with modern techniques [].
?
|
laesus_de_liro
Relevance
.
According to A.A. Sotnikova and O.L. Minaeva (GOU VPO Siberian State Medical University of Roszdrav, Tomsk, 2008) about 70% of women, after performing oncological surgical interventions on the mammary gland, subsequently need reconstructive plastic surgery. The mammary gland lost during surgery is restored using free or non-free TRAM flaps or a latissimus dorsi flap followed by endoprosthetics. In addition to reconstructive plastic surgeries, the number of plastic surgeries on the mammary gland for aesthetic correction has now sharply increased. Among these operations, reduction mammoplasty is performed in 39% of cases, augmentation mammoplasty is performed in 44% of cases, and correction of the shape of the nipple or areola is performed in 17% of cases. The final stage of reconstructive plastic and aesthetic operations on the mammary gland is the preservation or restoration of the nipple-areolar complex (NAC) lost during the operation. However, in 8-55% of cases, the reconstructed SAH becomes insensitive in the late postoperative period and is subject to necrotic complications. Therefore, it is so important to know the anatomical and topographical characteristics of SAH. Innervation
of the mammary gland (Christian J. Gabka, Heinz Bohmert, 2010) is carried out
segmentally
, by the lateral branches of the 3rd – 6th intercostal nerves (T3 – T6). The central parts of the mammary gland, including the area of the nipple and areola, receive sensory innervation from the anteromedial and anterolateral fibers of the T3–T5 intercostal nerves; The innervation of most of the mammary gland is carried out by the T4 nerve (fourth intercostal cutaneous nerve - anterior, cutaneus lateralis, IV intercostalis). When performing reconstructive plastic and aesthetic operations on the mammary gland, it is strongly recommended to preserve at least one of these nerves to ensure sensory innervation of the mammary gland. The inferior branches of the cervical nerve plexus also provide sensory innervation to the upper parts of the mammary gland. The medial as well as the lower parts of the mammary gland are innervated by the lateral branches of the 2nd – 6th intercostal nerves (T2 – T6). The lateral cutaneous branch of the 2nd intercostal nerve (intercostobrachial nerve, n. intercostobrachialis) passes laterally through the axilla and forms a nerve plexus with the cutaneous branch of the median nerve (n. medianus), as well as with the 3rd intercostal nerve (T3). These nerves together provide innervation to the superomedial portions of the shoulder.
Practical recommendations
. Preserving these nerves during axillary lymph node dissection for breast cancer can be quite challenging in some cases because the nerves directly pass through the central group of lymph nodes. Before performing any surgical intervention on the mammary gland, it is advisable to assess the sensitivity of the nipple area in order to identify innervation disorders as early as possible in the postoperative period. Intraoperative injuries to the anteromedial and anterolateral segmental branches of the intercostal nerves can cause hypoesthesia up to complete loss of sensitivity in the postoperative period. In some cases, innervation can be partially restored by massaging the damaged area (contraindicated in breast cancer).
© Laesus De Liro
Dear authors of scientific materials that I use in my messages!
If you see this as a violation of the “Russian Copyright Law” or would like to see your material presented in a different form (or in a different context), then in this case write to me (by mail) and I will immediately eliminate all violations and inaccuracies.
But since my blog does not have any commercial purpose (or basis) [for me personally], but has a purely educational purpose (and, as a rule, always has an active link to the author and his scientific work), so I would be grateful to you for the chance make some exceptions for my messages (contrary to existing legal norms). Best regards, Laesus De Liro.
Source: https://laesus-de-liro.livejournal.com/205374.html
Treatment
Leukomalacia is accompanied by irreversible changes in the nervous tissue, and no clear treatment regimen for this condition has been developed. Typically, doctors take a symptomatic approach, depending on the specific manifestations of the pathology.
The main component of treatment is nootropic drugs that help improve blood flow and metabolism in the brain (piracetam, nicergoline, stugeron). Additional therapy is aimed at correcting movement disorders and psychomotor development disorders.
As a preventive measure, obstetricians and gynecologists make every possible attempt to prolong pregnancy until the time when childbirth becomes safe for the baby. If a child is still born prematurely, then it is necessary to immediately establish control over breathing and homeostasis indicators - the level of oxygen and carbon dioxide in the blood, blood pressure, acid-base balance.
Diagnostics
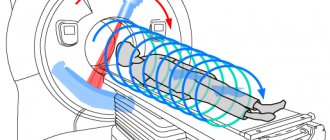
The most revealing research method that can identify foci of demyelination of the brain is magnetic resonance imaging.
A characteristic picture for this disease is the identification of oval or round foci measuring from 3 mm to 3 cm in any part of the brain. Typical localization for this pathology is the area of the subcortical and periventricular zones. If the disease lasts for a long time, these lesions may merge. MRI also shows changes in the subarachnoid spaces and an enlargement of the ventricular system due to brain atrophy. Relatively recently, the evoked potential method began to be used to diagnose dimyelinating diseases. Three indicators are assessed: somatosensory, visual and auditory. This makes it possible to evaluate disturbances in the conduction of impulses in the brain stem, visual organs and spinal cord.
Electroneuromyography shows the presence of axonal degeneration and allows you to determine myelin destruction. Also, using this method, a quantitative assessment of the degree of autonomic disorders is made.
Oligoclonal immunoglobulins contained in the cerebrospinal fluid are subjected to immunological studies. If their concentration is high, this indicates the activity of the pathological process.
Measures for the treatment of demyelinating diseases can be specific and symptomatic. New research in medicine has made good progress in specific treatment methods. Beta interferons are considered one of the most effective drugs: these include Rebif, Betaferon, Avanex. Clinical studies of betaferon have shown that its use reduces the rate of disease progression by 30%, prevents the development of disability and reduces the frequency of exacerbations.
Experts increasingly prefer the method of intravenous administration of immunoglobulins (bioven, sandoglobulin, venoglobulin). In this way, exacerbations of this disease are treated. More than 20 years ago, a new, quite effective method for treating demyelinating diseases was developed - immunofiltration of cerebrospinal fluid. Research is currently underway on drugs whose action is aimed at stopping the demyelination process.
Corticosteroids, plasmapheresis, and cytostatics are used as specific treatments. Nootropics, neuroprotectors, amino acids, and muscle relaxants are also widely used.
Causes and risk factors
Most expectant mothers know about the importance of the first 2–3 months of a child’s intrauterine development. However, the last trimester of pregnancy also poses many dangers for the full growth and formation of the human brain.
A decrease in the supply of oxygen to brain cells is due to meteorological conditions that provoke vascular spasms.
Other factors of neurological disease:
- endocrine disorders in the expectant mother - for example, diabetes;
- anemia of pregnant women;
- vitamin deficiencies;
- intrauterine infection of the fetus;
- heavy bleeding during labor;
- sharp fluctuations in the baby’s blood pressure;
- early acute respiratory failure in a newborn.
However, the main cause of leukomalacia of the brain remains extreme prematurity. Therefore, obstetricians-gynecologists place the main emphasis on timely prevention of premature birth and intrauterine oxygen deficiency.
Kidneys and adrenal glands
MRI of the kidneys allows you to diagnose the following diseases:
- developmental anomalies,
- kidney abscesses,
- polycystic disease (kidney cysts)
- hydronephrosis,
- stones in the kidneys,
- inflammatory diseases (pyelonephritis, glomerulonephritis, tuberculosis),
- tumor assessment (for example, carcinoma or transitional cell carcinoma),
- assessment for xanthogranulomatous pyelonephritis,
- assessment of benign tumors (for example, oncocytoma and angiomyolipoma);
However, MR examination is of greatest value in the differential diagnosis of tumors and cystic formations of the kidneys.
MRI can detect tumors less than 2 cm in diameter, detect metastases in the lymph nodes and tumor thrombi in the vessels of the kidney.
Pathology of the adrenal glands is often detected incidentally when performing an MRI of the retroperitoneum. Most often it is possible to diagnose:
- benign;
- malignant tumors, metastases;
- assess the causes of hormonal imbalance.
Signs of a benign adrenal tumor:
- round shape,
- smooth, clear contour,
- the structure is homogeneous.
Signs of a malignant adrenal tumor:
- wrong shape,
- the contour is uneven, blurred,
- heterogeneous structure (areas with different signal intensities are noted)
The process of pathology formation
In order to understand what PVL is and how to deal with it, it is necessary to understand the mechanism of its formation. Against the background of provoking factors, a pathological focus appears in the nerve cells - due to oxygen starvation, the white matter of the organ dies. Full-fledged neurocytes are replaced by other elements that are not able to perform the same functions.
Later - after 7-14 days, periventricular cysts appear in this area - hollow or filled with a special liquid. At the final stage, scars may appear on the nervous tissue. Less commonly, secondary hemorrhagic infarctions can be observed in the lateral ventricles of the organ. Subsequently, the affected areas completely atrophy.
As a rule, periventricular leukomalacia develops in the first hours of the baby's birth. However, there are cases when the periventricular variant of the pathology occurs later - up to 5-7 days from the moment of birth.
Damage to the lateral ventricles of the brain can also occur in utero - during pregnancy, accompanied by exacerbation of pyelonephritis and hepatitis. In order to avoid this, a woman needs to contact a doctor monitoring the course of her pregnancy at the first signs of deterioration in her health.
Diagnostics
The main method for detecting foci of brain demyelination is magnetic resonance imaging. It allows you to get an accurate picture of the disease. The introduction of a contrast agent delineates them more clearly, making it possible to highlight new lesions in the white matter of the brain.
Other testing methods include blood samples and cerebrospinal fluid testing.
Symptoms and signs of the disease
It is difficult to suspect that leukomalacia of the brain has appeared in newborns - the signs of periventricular pathology are varied and extremely nonspecific. However, the lack of oxygen supply to nerve cells is not completely asymptomatic. The main clinical signs of periventricular leukomalacia:
- excessive excitability of the newborn - loudness, excessive randomness of movements;
- tendency to convulsive states;
- sluggish muscle reflexes.
In extremely premature babies, the symptoms are much more severe:
- fluctuations in body temperature;
- lethargy;
- increased drowsiness;
- decreased appetite;
- sleep disturbance;
- paresis/paralysis of limbs;
- respiratory disorders;
- visual disturbances – strabismus.
Experts emphasize that manifestations of the periventricular form of the disease may subside after the acute period. This period of imaginary well-being lasts up to 8-9 months. And only by the age of one year does leukomalacia of the brain make itself felt by a deficit of nervous activity. The course of the pathological process is indicated by:
- insufficient weight gain;
- slow growth;
- skills lag;
- discrepancy between intelligence and age;
- delayed psycho-speech development;
- pronounced emotional lability.
Gallbladder
Normally, the gallbladder is pear-shaped with clear contours and homogeneous contents.
Horizontal size – less than 5cm. Wall thickness 1-3 mm. The width of the common bile duct is less than 8 mm. The most complete picture of the condition of the gallbladder is provided by non-contrast magnetic resonance cholangiopancreatography. MR cholangiography allows you to identify stones in the gallbladder and bile ducts, diagnose strictures (narrowing) of the bile ducts, and anomalies of their development.
On MR images, free bile has a hyperintense appearance and stones appear as dark spots (filling defect).
Prognosis and severity of PVL
If a woman fails to carry her baby to term, the children are born premature. Parents should prepare in advance to properly care for their newborn.
The prognosis will be relatively favorable for mild leukomalacia of the brain . In the periventricular clinic, attention deficit prevails, as well as hyperactivity - chaotic movements of the limbs. While motor development - the timeliness of crawling, walking, and turning over - is preserved.
Special corrective measures can achieve compensation for the disorder and improve physical and intellectual development.
With moderate and severe periventricular leukomalacia, the baby will not meet average age standards - parents should be prepared for this. He will later begin to roll over, sit down, and walk.
Speech development is also hampered - syllables will appear later, and sentences will be practically inaccessible. Other manifestations of periventricular pathology:
- lack of natural childhood curiosity;
- soreness and tension in the muscles of the limbs;
- restlessness, excessive tearfulness;
- sleep disturbance – intermittency, frequent confusion between day and night;
- breastfeeding is difficult - the sucking and swallowing reflex is poorly expressed;
- deviations in the dative system – the need to use an artificial respiration apparatus.
Treatment tactics
Since foci of leukomalacia imply irreversible death of nerve cells, no clear schemes for eliminating such periventricular conditions have been developed. Experts adhere to a symptomatic approach - treatment is aimed at reducing the severity of negative manifestations.
Periventricular leukomalacia in premature infants requires immediate measures to improve oxygen supply to cells. To do this, full blood flow must be restored. Effective groups of medications:
- nootropics – increase blood flow to nerve cells: Piracetam;
- anticonvulsants – Carbamazepine;
- vitamin complexes;
- for high intracranial pressure - Diacarb;
- for increased tearfulness and sleep disturbances, use herbal-based sedatives, for example, Valerian, Melissa.
In addition to drug therapy, doctors recommend courses of therapeutic massage and physiotherapy. Correctional classes with a psychologist and teachers are required to stimulate memory, thinking, attention, and speech.
In case of severe periventricular disease, treatment measures will be carried out in a hospital setting - restoration of respiratory, cardiovascular activity, compensation of intracranial hypertension. In this case, there will be no talk of a favorable prognosis.
Indications
If other research methods have given questionable results (CT, ultrasound, X-ray, etc.) or their implementation is impossible, then tomography allows you to differentiate various conditions and diseases:
- Diagnosis of liver and biliary tract diseases;
- Jaundice of any etiology;
- Internal bleeding;
- Unexplained abdominal pain;
- Enlarged liver and spleen of unknown origin;
- Ischemic changes in tissues;
- Polyps in the gall bladder;
- Gallstone disease and its complications (gallbladder stones);
- Kidney stones, sand in the kidneys;
- Diseases of the pancreas (acute and chronic pancreatitis);
- Congenital anomalies of organs or blood vessels;
- Suspicion of liver tumors, cancer of the pancreas, kidneys, adrenal glands, extraorgan formations;
- Differential diagnosis of space-occupying formations in internal organs identified by other research methods;
- Assessment of the condition of the spleen in blood diseases;
- Abdominal injuries;
- Detection of damage to the lymph nodes of the retroperitoneal space;
- Benign formations - cysts, adenomas, polyps;
- Preoperative preparation;
- Postoperative monitoring or detection of complications;
- Monitoring the effectiveness of treatment.
A survey MRI of the abdominal cavity evaluates the structure, size, location, shape, and blood supply of the organs located in it.
Prevention
The good health of children is the result of the efforts of their mothers from the first days when they learned about their pregnancy. To prevent periventricular leukomalacia from occurring, it is recommended to take preventive measures in advance:
- observe the principles of a healthy life even at the stage of pregnancy planning;
- adhere to a balanced diet, with the presence of various vegetables and fruits in the diet;
- give up all bad habits, especially the use of tobacco and alcohol products;
- consult a doctor in advance and get tested for the presence of hidden infections in the body;
- avoid heavy physical and psycho-emotional stress;
- strengthen protective barriers - take vitamin complexes;
- get a good night's sleep;
- minimize contact with people suffering from infectious diseases.
A woman who finds out about her pregnancy should immediately register with a doctor who will observe her at all stages of the baby’s intrauterine development. Health care specialists pay great attention to the prevention of various pathologies, including perivericular leukomalacia in newborns - standards for preventive research in pregnant women have been developed.
results
What does an MRI of the abdominal cavity and retroperitoneal space show? During a survey tomography, all internal organs located in the abdominal cavity and retroperitoneum are scanned. Tomography allows you to determine:
- structure of organs, their size and location;
- developmental anomalies;
- various pathological changes (inflammation, dystrophy, cystic transformation);
- benign neoplasms
- primary malignant tumors and metastatic lesions;
- circulatory disorders;
- damage to large vessels (aorta, inferior vena cava);
- gallstones and kidney stones.
It is most rational to use MRI as a clarifying research method.
What does an MRI with contrast show?
Cysts, hemangiomas, and malignant tumors are very similar to each other on regular MRI images. Contrast is used to distinguish these space-occupying lesions. By the peculiarities of filling them with contrast, their nature can be accurately determined.