Extramedullary tumors
Extramedullary tumors can be
Intradural: located inside the dura mater, but on the surface of the spinal cord, and not inside its parenchyma
Extradural: located outside the dura mater
Most intradural tumors are benign and usually include meningiomas and neurofibromas, the two most common primary spinal cord tumors.
Most extradural tumors are metastatic. They usually arise as carcinomas of the lung, breast, prostate, kidney, thyroid, or lymphomas, most commonly as non-Hodgkin's lymphoma, but also as Hodgkin's lymphoma, lymphosarcoma, and reticulocellular sarcoma.
Intradural and extradural tumors often exert their effect by compressing the spinal cord and its roots, rather than by growing into the parenchyma. Most extradural tumors penetrate and destroy bone before they compress the spinal cord.
Clinical manifestations
Pain is an early symptom, especially with extradural tumors. It is progressive, independent of physical activity, and worsens when lying down. The pain may be localized in the back and/or spread to the dermatome (radicular pain).
Neurological disorders indicate damage to a certain part of the spinal cord that has developed over time. Typical examples include spastic weakness, urinary incontinence, and dysfunction of some or all sensory pathways at some level of the spinal cord and below. The abnormalities usually appear bilaterally.
Intradural extramedullary tumors may cause pain when they compress the nerve roots, but may also be painless if the spinal cord is directly compressed without involving the roots.
Home » Types of diseases » Spinal cord tumors
Spinal cord tumors
Tumors of the central nervous system account for 12% of all neoplasms, spinal cord tumors account for 3% of diseases of the nervous system and are found mainly in middle-aged people. In children and elderly people, these tumors are rarely observed. Spinal cord tumors are found predominantly in women. Most often, they develop not from the brain matter, but from the surrounding tissue, and when they increase in size, they compress the spinal cord.
Lipomas, dermoid cysts, sarcomas, epidural ependymomas and angiomas are more common in children. Middle-aged people are more likely to have neuromas, and less often - meningiomas. In older people, meningiomas are in first place in frequency, less often - neuromas; other tumors (except for cancer metastases) are almost never found.
Classification of spinal cord tumors
Spinal cord tumors, depending on their location, are divided into extracerebral (extramedullary), found in 80% of cases, developing from the meninges, its roots and tissues surrounding the spinal cord, and intracerebral (intramedullary), found in 20% of cases, arising from cellular brain elements (true spinal cord tumors). With respect to the spinal canal and dura mater, spinal cord tumors are divided into subdural, epidural and extra-intravertebral (hourglass-type). In relation to the length of the spinal cord, in more than half of the cases, tumors occur in the cervical and lumbar regions. Tumors of the cauda equina occur in approximately 1/5 of patients. In the cervical spine, tumors of the spinal cord in children are twice as common as in the elderly, and in the thoracic spine in older people - three times more common than in children. Tumors in the cauda equina region are 25 times more common in children than in older people. There are also craniospinal tumors: tumors spread from the cranial cavity to the spinal canal or vice versa.
Histological classification of spinal cord tumors.
Meningiomas - tumors of the spinal cord membranes - are benign tumors covered with a pinkish-gray-brown membrane, often of a hard consistency. Occurs in 1/3 of patients.
Neuromas are observed in 1/3 of patients. These are benign tumors, oval in shape, whitish-gray in color, and have a hard consistency. They are often hourglass shaped. They usually arise from the dorsal roots of the spinal cord. Such tumors are also called schwanoma. Multiple neuromas characteristic of Recklinghausen's disease are rare.
Sarcomas make up 15% of all spinal cord tumors. More often characteristic of children, manifesting itself in the form of a nodular conglomerate of a reddish-brown color with a dense consistency.
Astrocytomas are a benign form of intramedullary tumors, most often characteristic of children 2-5 years old and localized in the cervicothoracic spinal cord.
Glioblastoma multiforme and medulloblastomas are malignant intramedullary tumors with infiltrative growth.
Ependymomas occur predominantly in patients 30-40 years old and in school-age children. They are localized mainly in the cervical region and in the cauda equina region. These tumors are pink in color and can spread into two, three or more segments.
Lipomas make up about 1% of all tumors, occurring mainly in childhood. These are tumors of mesenchymal origin, soft consistency, yellow in color. They grow infiltratively in several places, affecting the brain.
Vascular tumors (hemangioendothelioma, hemangioblastoma, hemangiopericytoma, angiolipomas, angiosarcoma) account for 5-6% of the tumors and are found mainly in middle-aged people.
Sympathoblastomas originate from the sympathetic ganglia, growing through the intervertebral foramina, irritating them, covering the roots of the spinal cord, and subsequently causing compression of the spinal cord. The development of these tumors is accompanied by severe radicular pain and the relatively rapid onset of paraplegia.
Chondromas, chordomas. Chondrosarcomas are neoplasms that are rare and localized primarily in the sacral region.
Tumors of a heterotopic nature (dermoid cysts, epidermoids and teratomas) occur mainly in children in the first years of life.
Metastatic tumors occur in 1% of cases and, as a rule, penetrate through the spinal venous system. Such metastases spread to tumors of the bones, kidneys, breast and prostate. These tumors grow quickly, destroying vertebral bone, ligaments and soft tissue, causing compression of the spinal cord. As a rule, they do not grow into the dura mater.
Spinal cord tumor clinic
All spinal cord tumors, regardless of their location, origin and histological structure, are characterized by a progressive wave-like course with an increase in symptoms due to gradual compression of the spinal cord and damage to its roots. The clinical picture of spinal cord tumors is characterized by the following syndromes:
1. Radicular syndrome. Depending on which of the roots is affected, anterior or posterior, it manifests itself mainly as pain, impaired sensitivity and peripheral movements. Radicular syndrome is characterized by an irritation phase and a loss of function phase. Pain is the earliest, constant symptom that can be observed in all phases of the tumor process. More often, pain occurs when the dorsal roots of the spinal cord are irritated, but often the pain can be a consequence of the effect of the tumor on the sensitive conductors and membranes of the spinal cord. Such pain is characteristic of neuromas and meningiomas. Therefore, in adults, pain is more common and more intense than in children. The duration of pain varies - from several minutes to several hours; with extramedullary tumors, pain intensifies in a lying position and decreases in a standing and half-sitting position when the process is localized in the lower spine. This is of great diagnostic importance, since with tuberculous spondylitis and meningitis, the pain is relieved in the horizontal position of the patient. Pain with intramedullary tumors is less pronounced, but has a longer duration compared to extramedullary tumors. The symptom of the spinous process is of great importance: pain upon percussion of the spinous processes and paravertebral points at the level of the pathological process.
The “bow” symptom is characterized by increased pain when bending the head forward. Intramedullary neuromas are characterized by a symptom of the so-called cerebrospinal fluid push - the occurrence or intensification of radicular pain with compression of the jugular veins. In this case, the outflow of blood from the brain becomes difficult, intracranial pressure quickly increases and a wave of cerebrospinal fluid spreads through the subarachnoid spaces of the spinal cord, acting as a push on the tumor with tension on the root, as a result of which pain appears or intensifies.
Depending on the degree of damage to the spinal cord root, sensory disturbances appear behind the radicular type in the form of numbness, “pins and needles”, a feeling of cold or warmth.
At first, paresthesias are temporary (irritation phase), and later they become permanent and turn into a decrease in sensitivity (loss phase), if several roots are affected - to the degree of anesthesia.
Sometimes, with spinal cord tumors in children, a fixed position of the head may occur as a result of tension in the muscles of the back and neck. This symptom is the result of a protective effect, caused by irritation of the root and dura mater of the spinal cord by the tumor. Reflexes, the arcs of which of the spinal cord pass through the affected root or close at the level of the affected segment, decrease or disappear. The level of tumor location can sometimes be determined based on the loss of the reflex arc - certain tendon reflexes (peripheral paresis or paralysis).
2. Syndrome of damage to the diameter of the spinal cord. The appearance and development of this syndrome is caused by increasing compression of the spinal cord by a growing tumor. In this case, the following symptoms are noted: - Sensitivity disorders are wire-based in nature. With extramedullary tumors, an ascending type of sensitivity disorder is observed, with intramedullary tumors, a descending type of sensitivity disorder is observed, which is explained by the law of eccentric arrangement of conductors. — Motor disturbances can be unilateral or bilateral, depending on the medial or lateral location of the tumor and the degree of compression of the spinal cord. They manifest themselves in the form of paresis or paralysis.
Disturbances in muscle tone , namely its increase, are characteristic of impaired conduction of the motor pathways of the spinal cord and correspond to the depth of paresis depending on the degree and duration of compression. A decrease in muscle tone can be observed with the acute development of the disease, rapidly occurring compression of the spinal cord with severe hemodynamic impairment, which indicates an extremely depleted function and a poor prognosis of the disease. A decrease in muscle tone is also typical when the tumor is localized in the cauda equina region and when a peripheral neuron is affected.
Changes in reflexes. Over time, when the inhibitory effect of the cerebral cortex is disrupted, the reflex activity of the segmental apparatus of the spinal cord increases, which leads to revitalization, increased tendon and periosteal reflexes and the appearance of pathological pyramidal reflexes. Skin reflexes, abdominal, cremasteric and others, on the contrary, disappear depending on the location of the tumor, which has a topical significance. With tumors of the spinal cord, Brown-Séquard syndrome is observed (a symptom of damage to half the diameter of the spinal cord), but not in the classical version, but only its elements. The classic symptoms of Brown-Séquard syndrome are characteristic of a wound from a transection of half the diameter of the spinal cord and is characterized on the affected side by the presence of central paralysis and loss of deep types of sensitivity (proprioceptive and vibration) and on the opposite side by loss of superficial types of sensitivity - pain and temperature. Tactile sensitivity decreases on both sides; peripheral radicular disorders are also characteristic on the damaged side.
Dysfunction of the pelvic organs depends on the level of tumor localization. Tumors at the level of the lumbosacral segment may cause urinary and fecal incontinence and sexual dysfunction. Tumors located above the sympathetic (LI-LII) and parasympathetic (SIII-SV) regulation centers of the pelvic organs are characterized by central dysfunction of the latter - urinary and fecal retention.
Due to the effect of the tumor on the trophic segmental centers, compression of sensory and motor conductors, patients may have trophoparalytic syndrome in the form of muscle atrophy and trophic ulcers of the extremities.
With auxiliary examination methods, liquorological syndrome (protein-cell dissociation) and liquorodynamic syndrome (complete, partial or valvular liquor blockade of the subarachnoid spaces) is revealed.
Depending on the location of the tumor along the length of the spinal cord, clinical symptoms vary.
Tumors of the cervical spinal cord at the level of the CI-CIV segment are characterized by early and persistent radicular pain in the occipital region of a shooting nature with limitation of movements in the cervical spine. Central tetraparesis slowly increases. When the tumor is localized at the level of segment CIV, breathing disturbances due to damage to the phrenic nerve (diaphragmatic paralysis) are characteristic. Along with this, with craniospinal tumors, symptoms of intracranial hypertension with congestion in the fundus occur, and with damage to the medulla oblongata, bulbar symptoms are added. When the CV-DI segments are affected - the area of cervical thickening - flaccid peripheral paresis or paralysis of the upper extremities is observed in combination with central paraparesis, which over time turns into paraplegia of the lower extremities.
When the tumor compresses the celiac spinal center, which is located in segments CVIII-DI, Claude-Bernard-Horner syndrome (ptosis, miosis, enophthalmos) or its elements develops. Sometimes nystagmus is observed, which is combined with a change in the functional state of the vestibular analyzer. In some cases, there is a partial dysfunction of the V and IX pairs of cranial nerves (decreased corneal and swallowing reflexes).
Tumors of the thoracic region manifest as radicular pain along the intercostal nerves. When the tumor is localized at the level of segments DIV-DVI, various cardiac abnormalities may be observed. When the lower thoracic segments are affected, pain occurs in the abdominal area, which can lead to an erroneous diagnosis: cholecystitis, pancreatitis or appendicitis. The state of the abdominal reflexes is important in the topical diagnosis of tumors of the lower thoracic region. Their complete absence is typical for tumors in the DVII-DVIII region; the middle and lower ones are absent in DIX-DX tumors. the absence of only lower abdominal reflexes is characteristic of damage to segments DXI-DXII.
Tumors of the lumbar enlargement area (LI-SII). When the tumor is localized in the upper parts of the thickening, a mixed lesion can be observed: in the proximal muscle group - of the peripheral “flaccid” type and in the distal muscle group - of the central type. In this case, the knee reflexes are not evoked or are reduced, and the Achilles is increased. With tumors of the lower segment thickening, the knee reflexes are preserved, but the heel reflexes are lost. Muscle paralysis and anesthesia of the distal extremities extends to the level of the knees and above.
Epiconus lesions (LIV-SII) are characterized by flaccid paralysis of the peroneal and gluteal muscles, with preservation of the knee muscles and loss of Achilles reflexes. When tumors of the spinal cord are localized from the cervical spine to the level of the conus medullaris, dysfunction of the pelvic organs of the central type is observed - retention of urination and defecation.
Tumors in the area of the conus medullaris are accompanied by pain on the posterior surface of the gluteal region and in the anogenital area. Due to the damage to the parasympathetic centers by the tumor process, dysfunction of the pelvic organs of the peripheral type occurs (urinary and fecal incontinence, sexual weakness, the anal reflex disappears early in children). Tumors in the cauda equina area are manifested by severe, sharp and persistent pain in the sacral region, anus and lower extremities, aggravated in a horizontal position. Motor and sensory disorders of the radicular type increase, dysfunction of the pelvic organs of the peripheral type joins, partial urinary and fecal incontinence is replaced by complete.
Depending on the type of spinal cord tumor, the development of motor and sensory disorders in extracerebral and intracerebral tumors is not the same. Extramedullary tumors are characterized by an ascending type of disorders - from the distal parts (foot, perineum) with their gradual spread upward to the level of the lesion, which is explained by the gradual compression of the spinal cord conductors externally, where the longest fibers are located, from which the innervation of the distal parts of the body is located. The clinical picture of the disease often begins with radicular syndrome, followed by the addition of symptoms of spinal cord compression.
For intracerebral tumors , in which internal, shorter fibers that end in segments at the level of the tumor are compressed earlier, a descending type of dysfunction of the spinal cord is characteristic. In this case, radicular syndrome appears against the background of symptoms of damage to the diameter of the spinal cord. Clarification of the level of tumor localization in a particular part of the spinal cord is based on symptoms of segmental and conduction origin. In this case, the most informative are sensory disorders that accurately indicate the level of tumor location.
Diagnostics.
Among the auxiliary examination methods in the diagnosis of spinal cord tumors, lumbar puncture with CSF tests is of great importance. In biochemical and microscopic studies of the cerebrospinal fluid, a significant increase in the amount of protein is observed (2-10 times) against the background of an almost unchanged amount of formed elements (protein-cell dissociation), which is more typical for extramedullary tumors. An increase in protein levels is determined by stagnation in the subarachnoid and epidural veins and transduction of plasma into the cerebrospinal fluid. The lower the tumor is located, the more protein passes from the veins of the tumor into the cerebrospinal fluid.
With vascular tumors, xanthochromia may be observed, and with tissue breakdown, cytological examination can reveal tumor cells. Carrying out liquor-dynamic tests (Queckenstedt and Stukey) reveals disturbances in the patency of the liquor spaces in the form of a complete, partial or valve block. With extramedullary tumors, especially neuromas, after lumbar puncture and removal of cerebrospinal fluid, herniation syndrome is observed, which is manifested by an increase in dysfunction of the spinal cord, especially its conductive tracts. In this case, the paresis deepens or turns into paralysis, and sensory disturbances intensify. This is explained by the fact that the emission of cerebrospinal fluid leads to displacement of the tumor with impaired spinal circulation (A. P. Romodanov et al., 1990).
Spondylography , which is performed in two projections, for tumors of the spinal cord, especially in children, can detect radiological symptoms in the form of narrowing, flattening of the internal contour and shortening of the base of the roots of the arches - Elsberg-Dyck syndrome. In children with spinal cord tumors, changes in the spinal axis are often detected in the form of scoliosis, kyphosis, straightening of the cervical and lumbar lordosis, and deepening of the posterior surface of the vertebral bodies at the level of the tumor.
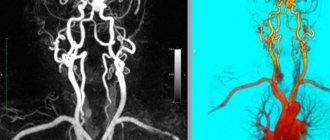
Ascending and descending myelography is used to determine the upper and lower borders of the tumor. In ascending myelography, contrast is used, the specific gravity of which is less than that of the cerebrospinal fluid, usually air. When descending, the contrast is heavier than the cerebrospinal fluid. During radioisotope examination of the spine and spinal cord, xenon and an air-radon mixture are used for contrast.
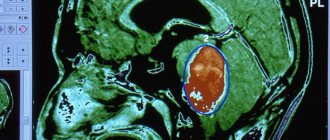
For spinal cord tumors, using radiometry, the maximum radiation level is determined at the level of the lower border of the tumor. Descending myelography begins with a suboccipital puncture, during which a water-soluble contrast agent (omnipaque) is injected into the occipital cistern magna, which, due to its greater weight, is lowered down the subarachnoid spaces of the spinal cord. Extra-medullary tumors are characterized by stoppage of the contrast agent in the form of a “cap”, “cap” or “cylinder”. In intramedullary tumors due to fusiform thickening of the spinal cord, the contrast agent may stop in the form of two bands that gradually narrow, located on the lateral surfaces of the spinal cord. With venospondylography, spinal cord tumors are characterized by changes in the venous vessels of the spinal cord.
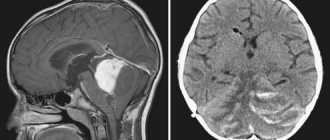
Computed tomography and magnetic resonance imaging make it possible to finally clarify the nature and location of spinal cord tumors.
Treatment of spinal cord tumors is only surgical. The earlier and more radically the tumor is removed, the more favorable the postoperative result. The tumor is accessed by laminectomy. For purely extradural tumors, the dura mater is not cut. The tumor is removed in parts. If the tumor spreads over a long distance along the length of the brain, then every 3-4 vertebrae one arch is left unremoved, removing the tumor from underneath it from above and below. If the tumor is located subdural, then it is removed after incision of the dura mater. Removal of a tumor located intradurally on the anterior surface of the spinal cord is carried out after opening the dentate ligament. Removal of intracerebral tumors is carried out using microsurgical techniques.
In the early postoperative period, patients undergo rehabilitation therapy: therapeutic exercises, massage of the limbs, prescription of vasodilators, B vitamins, etc. In the long-term postoperative period, clinical observation and repeated courses of rehabilitation therapy in a neurological or rehabilitation department are indicated.
The results of treatment of spinal cord tumors depend on the location of the tumor, its morphological structure, and the radicality of tumor removal during surgery: in 90% of cases of extramedullary benign tumors, postoperative results are positive. The prognosis for restoration of function depends on the disorders and the time elapsed before surgery. The more severe the clinical manifestations and the longer the period before surgery, the worse the results of restoration of lost functions after surgical treatment.
Diagnostics
Urgent diagnosis and treatment are required for patients with segmental neurological deficits or suspected spinal cord compression.
The following symptoms may suggest a spinal cord tumor:
Increasing pain, radicular pain or back pain at night, which has no other objective causes
Segmental neurological disorders
Neurological deficit indicating damage to the spinal cord or nerve roots and having no objective cause
Unexplained back pain in patients with a history of cancer, especially tumors of the lung, breast, prostate, kidney, thyroid, or lymphoma.
The diagnosis of a spinal cord tumor is made using an MRI of the affected area of the spinal cord. An alternative is CT with myelography; This method can help determine the location of the tumor, but provides less information than MRI.
Other spinal masses (eg, abscesses, arteriovenous malformations) and paravertebral tumors may present similarly to spinal tumors but can usually be differentiated by MRI.
Bone destruction, widening of the vertebral pedicles, or displacement of paravertebral tissues, especially if the tumor is metastatic, may be an incidental finding on a radiograph of the spine.
Treatment
Tumor resection and/or radiation therapy
In patients with neurological lesions, immediate administration of corticosteroids (eg, dexamethasone 100 mg intravenously, then 10 mg orally 4 times a day) is necessary to reduce spinal cord compression and preserve its function. For tumors that compress the spinal cord, treatment must begin as soon as possible, since the damage can very quickly become irreversible.
Some well-localized primary spinal cord tumors can be excised surgically. Approximately half of patients with this pathology experience improvement. For tumors that cannot be excised, radiation therapy is used with or without surgical decompression. Extradural metastases that cause compression of the spinal cord are usually excised from the vertebral body, followed by radiation therapy. Noncompressive metastatic extradural tumors can be treated with radiation therapy alone, but if radiation therapy is ineffective, surgery is indicated.
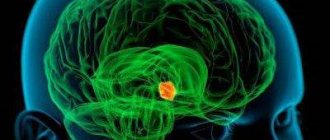
What is a spinal cord tumor
This neoplasm is a proliferation of pathological tissue, which is located in the spinal region. Pathologies can be completely different, but they definitely require treatment and monitoring from a specialist. The disease may not manifest itself for a long time, and symptoms will appear only when the tumor reaches a large size and it becomes much more difficult to treat. Statistics say that such neoplasms occur in only a tenth of patients with tumors in the central nervous system.
Key points
Spinal cord tumors are divided into intramedullary (in the spinal cord parenchyma) and extramedullary (outside the parenchyma).
Extramedullary tumors can be intradural or extradural.
Most intradural tumors are benign and are represented by meningiomas and neurofibromas, the most common primary tumors of the spinal cord. Most extradural tumors are metastatic.
Patients with neurological damage due to spinal cord compression require corticosteroids.
Surgical extraction of the spinal cord tumor and/or radiation therapy is required.
Read also
Spinal tumors
Spinal tumors are divided into benign and malignant, and the insidiousness of benign forms is that they may not produce any symptoms for many years.
Let's look at how... Read more
Hydrocephalus
Hydrocephalus is an accumulation of fluid in the brain. On MRI it looks like ventricular dilatation. Accompanied by increased intracranial pressure. There are two types of hydrocephalus. Obstructive (non-communicating)…
More details
Brain cysts
A brain cyst is an intracranial formation of significant volume, which is a cavity containing fluid. In many cases, the course of this disease is...
More details
Noise in ears
Tinnitus cannot be called an independent disease. It would be more accurate to designate it as a hearing disorder, which manifests itself as a hum, ringing or buzzing in the ears, then, as a real source of sound...
More details
Vertebral artery syndrome
The main vascular highways carrying blood to the brain pass in the neck - these are two carotid and two vertebral arteries. A decrease in blood flow through the vertebral arteries will lead to the development of acute...
More details