Hemangioblastoma is a benign brain tumor originating in blood vessels with a predominant localization in the cerebellum. Clinical symptoms of hemangioblastoma depend on its location and may include headaches, dizziness, nausea, asthenia, congestive optic discs, cerebellar syndrome (ataxia, nystagmus, muscle hypotonia, intention tremor), motor and sensory disorders, dysfunction of cranial nerves and pelvic organs. The basis for diagnosing hemangioblastoma is MRI of the brain and histological examination of a tumor sample. The most effective treatment for hemangioblastoma is its complete removal.
Hemangioblastoma
Hemangioblastoma accounts for about 2% of all tumors located in the skull. Hemangioblastoma is most often observed in patients aged 40 to 60 years. In 10% of cases, hemangioblastoma is a manifestation of the inherited Hippel-Lindau disease - phakomatosis, characterized by multiple neoplasms of internal organs occurring throughout life (pancreatic cysts, pheochromocytoma, renal cell carcinoma, retinal angioma, etc.). In such cases, hemangioblastoma is usually diagnosed at the age of 20-30 years.
Signs of pathology
The first manifestations of the tumor process in 90% of patients are general cerebral symptoms characteristic of intracranial hypertension, these are:
- severe headaches (usually in the back of the head);
- nausea, vomiting;
- forced head position (a person intuitively tilts his head to the side to facilitate the conditions for liquor outflow);
- blurred vision.
A feature of clinical signs, as a rule, is increasing or wave-like dynamics with long light intervals. Then, after a few months, focal signs join the symptoms of ICH, these are:
- movement coordination disorder;
- instability, unsteadiness of gait;
- pyramidal insufficiency;
- speech motor disorders;
- involuntary pendulum-like eye movements;
- mental disorders (neurasthenia, depressive neurosis, dysphoria, personality disorientation, etc.).
The listed clinical picture, based on the symptoms of ICH and cerebellar disorders, is characteristic of many cerebral pathologies. Therefore, they cannot be called pathognomonic, that is, specifically for angioreticularis. This fact does not apply only to patients with Hippel-Lindau disease, in whom this symptomatic complex is always combined with retinal angiopathy. In any case, the final diagnosis can be established only after a comprehensive diagnosis, including examination by a neurologist and ophthalmologist, MRI/CT, and selective angiography.
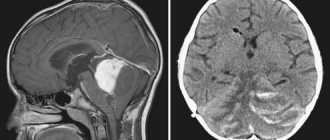
Education on MRI images.
Causes of hemangioblastoma
Like other neoplasms of the nervous system (craniopharyngioma, cerebral astrocytoma, ganglioneuroma, ganglioneuroblastoma, meningioma, etc.), hemangioblastoma can develop as a result of exposure to various carcinogenic factors on the body. The latter include ionizing radiation, increased insolation, contact with industrial carcinogenic substances (asbestos, benzene, vinyl chloride, petroleum and coal tars, phenol-formaldehyde, etc.), oncogenic viruses (for example, retroviruses, adenoviruses, herpes virus). Hemangioblastoma, which is part of Hippel-Lindau disease, has a hereditary etiology and is associated with a genetic mutation in the third chromosome, leading to a disruption in the synthesis of a tumor suppressor. Inherited in an autosomal dominant manner.
Radiosurgery
Stereotactic radiosurgery is recommended for a separate group of patients for whom classical surgery is contraindicated due to health conditions or the dangerous location of the tumor. Radiosurgery is also prescribed after incomplete surgical excision of hemangioblastoma in order to eliminate its remaining elements. In the arsenal of neurosurgery, there are 2 methods of stereotactic exposure (without incisions, trepanation and without pain) - Gamma Knife and Cyber Knife.
- Gamma Knife is a radiological procedure specifically designed to specifically destroy abnormal structures within the brain using Cobalt-60 ionizing radiation. Before the operation, a helmet system is put on the patient’s head, which makes it possible to accurately determine and neutralize the focal area. The radiation “works” strictly within the tumor and does not cause harm to nearby healthy brain structures. To install a stereotactic structure on the head, local anesthesia with a long-acting local anesthetic is performed locally (in the places where it is fixed). The course of Gamma Knife therapy consists of 1-3 procedures. Time of 1 session – 30-180 minutes.
- Cyberknife is a procedure for targeted irradiation of pathological tissues using a robotic installation that generates 6 MeV photon radiation. The principle of therapeutic action and effectiveness are approximately identical to the Gamma Knife. But the CyberKnife radiosurgical device, unlike the Gamma installation, is universal. It can be used to treat oncology in different parts of the human body. During this procedure, you do not need to place your head in a frame, and no anesthesia is required.
Contraindications to Gamma Knife and CyberKnife surgeries are tumors that have reached a size of 3.5 cm or more.
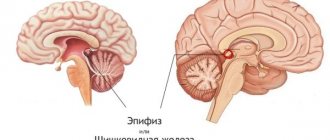
Classification of hemangioblastoma
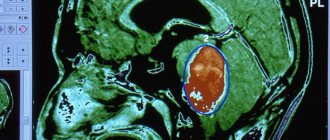
Based on their macroscopic structure, neurology distinguishes 3 groups of hemangioblastomas: solid, cystic and mixed. Solid (soft tissue) hemangioblastoma consists of tumor cells collected in a single node surrounded by a capsule, which has a soft consistency and dark cherry color. It accounts for about 65% of all hemangioblastomas. Cystic hemangioblastoma is a smooth-walled cyst. In most cases, there is a small solid nodule on the wall of the cyst. In approximately 4-5% of cases, mixed type hemangioblastomas occur, characterized by the presence of a solid node within which numerous cysts are located.
Based on the microscopic (histological) structure, the following types of hemangioblastoma are distinguished: juvenile, transitional and pure cell. Juvenile hemangioblastoma consists mainly of thin-walled capillaries that are closely adjacent to each other. Transitional hemangioblastoma contains capillaries and stromal cells in approximately equal proportions. Pure cell hemangioblastoma is characterized by numerous yellowish cells located on pathologically altered vessels.
Classification and causes of neoplasms
Brain hemangioma most often occurs in the following cases.
In an adult:
- Brain injuries or contusions.
- Nervous tension, stress.
- Hereditary factor.
In children:
- Infections suffered by a pregnant woman at a certain stage.
- Taking certain medications during pregnancy.
- Alcohol and cigarette abuse while pregnant.
- Difficult birth.
- Bad heredity.
Doctors are still arguing about the exact cause of malformations. There are several theories in medicine that have not yet been confirmed by scientific facts. Statistics show that men are more likely to suffer from this disease than the fair sex.
Experts classify several types of tumors; the main division is based on the types of vessels that make up the tumor. Hemangiomas are divided as follows:
- arterial neoplasm,
- venous tumor,
- arteriovenous malformation (the most common type).
Vascular tumors are divided into the following subtypes:
- cavernous tumor, the difference is an abundant blood supply, often leading to hemorrhages;
- branched tumor, difference - consists of tortuous strands of arterial vessels;
- bone tumor, the difference is its location on the bone tissue of the skull.
Hemangiomas can also be divided into the following types:
- A venous neoplasm is a locally dilated vein or a tangle of dilated vessels.
- A capillary neoplasm is a tangle of capillaries in which blood flow is impaired.
- A cavernous neoplasm is a tumor with vascular cavities, delimited by septa. This type of tumor is considered the most dangerous. When this type of malformation develops, the tumor is characterized by thin septa and impaired blood supply, which can lead to its rupture at any time. The following factors can provoke this situation:
- Emotional overstrain, severe stress.
- High physical activity.
- Pressure surge.
- Flick.
- Even light blows to the head.
The risk of rupture of this type of tumor is especially high in patients who have suffered a stroke or micro-stroke, in patients with problems of the vascular system. Most often, the rupture occurs in a hemangioma located deep in the brain tissue.
According to specific manifestations, hemangiomas can be divided into the following types:
- sluggish (torpid) form of the disease,
- prone to bleeding (hemorrhagic) form of the disease.
Cerebral hemangioma is a great danger because it practically does not cause any symptoms for a very long time. A neoplasm can be detected mainly by chance, by performing a brain tomography or other specific examinations. But there are still a number of signs that may indicate the presence of malformation in the brain.
When a torpid-type malformation occurs, a large vascular tangle filled with arterial blood, the following symptoms may occur: periodic headaches (pain in a certain place of the head), disturbed sleep, nervous breakdowns, disorders, convulsions. Convulsive manifestations also have certain symptoms.
A cramp may appear in a specific place or be general in nature, but a convulsive syndrome is always accompanied by severe headaches localized in one part, the pain can be so severe that a person may lose consciousness.
A hemorrhagic tumor (a small tangle of blood vessels that is prone to bleeding) mainly causes high blood pressure (hypertension).
Symptoms of hemangioblastoma
Clinical manifestations of hemangioblastoma depend on its location. Hemangioblastoma acts as an intracerebral tumor of the cerebral hemispheres extremely rarely. In 80-85% of cases it affects the hemispheres of the cerebellum, much less often - its vermis. According to various sources, hemangioblastoma of the spinal cord occurs in 3-13% of cases, hemangioblastoma of the medulla oblongata in 2-3% of cases.
Hemorrhoids kill the patient in 79% of cases
The clinical picture of cerebellar hemangioblastoma consists of cerebral, cerebellar and distant symptoms. The general cerebral symptoms of hemangioblastoma are caused by impaired outflow of cerebrospinal fluid and increasing hydrocephalus. A headache is typical, which practically does not disappear while taking analgesics and vasodilators. It can affect any area, but is most often localized in the back of the head. Ophthalmoscopy in the early stages of gamgioblastoma reveals congested optic discs. The so-called “stagnant” labyrinthitis is often observed, accompanied by intense systemic dizziness, nausea and vomiting. Labyrinthitis of congestive origin and associated vestibular ataxia require differentiation of hemangioblastoma from inflammatory lesions of the inner ear with otitis media, functional disorders with aerootitis, toxic damage to the labyrinth with cholesteatoma of the ear, Meniere's disease and vascular disorders (chronic cerebral ischemia).
It should be noted that general cerebral symptoms can be so pronounced that it is difficult to detect the cerebellar syndrome itself, which significantly complicates the diagnosis of hemangioblastoma. Mixed in with this are a variety of long-term symptoms of hemangioblastoma, which may include cranial nerve palsies, convulsive syndrome, pyramidal disorders (paresis or paralysis); Sensitivity disorders are less common.
The symptom of cerebellar damage in hemangioblastoma primarily includes cerebellar ataxia. Hemangioblastoma of the cerebellar vermis is manifested by static ataxia, i.e. a disorder of posture and walking. Unsteadiness or falling in the Romberg position, a forced tilted position of the head, a “drunk” gait, lateropulsion (deflection of the body to the side) when walking, and impaired synchronization of movements (assynergia) are typical. When hemangioblastoma is localized in the cerebellar hemisphere, dynamic ataxia (impaired coordination of movements) predominates, which is detected using finger-nose and knee-heel tests. As with other cerebellar tumors, excessive disproportionately wide movements (dysmetria), excessively large handwriting (megalography), rapid movement disorder (adiadochokinesis), and slow scanned speech (articulatory ataxia) are typical. Other signs of cerebellar damage include nystagmus, muscle hypotonia, and intention tremor.
At the beginning of the development of cerebellar hemangioblastoma, disturbances are observed only on the side of the tumor localization. However, as the hemangioblastoma grows, it begins to compress the opposite hemisphere of the cerebellum and the process becomes bilateral. The addition of symptoms of damage to the cerebellar vermis, resulting from its compression, leads to the development of total cerebellar syndrome. In the later stages, hemangioblastoma is often accompanied by mental disorders, often in the form of asthenia, depressive neurosis or neurasthenia, and impaired consciousness in the form of stupor.
Hemangioblastoma of the spinal cord and cerebral hemispheres is manifested by sensory and motor disturbances corresponding to its localization, as well as dysfunction of the intestines and bladder.
History of the study
The study of hemangioblastomas is largely related to research into the hereditary disease Hippel-Lindau disease. German ophthalmologist Eugene von Hippel (English) Russian. in 1904 described changes in the retina characteristic of the disease [6]. In 1926, Swedish pathologist Arvid Lindau (English) Russian. described characteristic changes in the central nervous system—hemangioblastoma of the cerebellum and spinal cord[2]. A. Lindau, at an autopsy of 50 patients with changes in the retina characteristic of the disease described by Hippel, discovered characteristic changes in the cerebellum in 10 of them. In two patients, they were the direct cause of death[2].
In 1927, Lindau made a literature review of 15 observations of “angiomatosis of the nervous system.” In this work, he described the changes in internal organs characteristic of the disease. After the classic works of the Swedish scientist, after whom pathology began to be named, other publications began to appear, which, citing Lindau, described similar clinical observations [2].
Image of cerebellar hemangioblastoma from an article by the founder of world neurosurgery H. Cushing in 1928.
In particular, in 1928, the founder of American and world neurosurgery H. Cushing described 11 patients operated on for cerebellar hemangioblastomas[2]. Of these, five died either immediately after the operation or a short time later - high mortality after neurosurgical operations was typical for the described time [7]). Having become familiar with Lindau's work, Cushing conducted further examinations of 6 patients. In one of them, the changes described by Hippel and Lindau were found on the retina. In addition, Cushing showed the hereditary nature of the process. Having also analyzed his observation and the cases described by Lindau, he noted that the first clinical manifestations of the disease occur in adulthood and are absent in childhood [2].
In his work, Cushing concluded that when characteristic changes are detected in the retina, attention should be paid to the presence or absence of symptoms of cerebellar damage, since the results will be better if treated in the early stages of the disease [2].
Diagnosis of hemangioblastoma
Difficulties in diagnosing hemangioblastoma are associated with the nonspecificity of its clinical manifestations, masking of neurological deficits and cerebellar syndrome under severe cerebral symptoms. A thorough neurological examination and additional consultation with an ophthalmologist, during which congestive optic discs are identified, allow one to suspect the presence of an intracranial space-occupying lesion. In this case, in addition to the usual initial examination in the form of EEG, REG and Echo-EG, the patient must undergo an MRI of the brain.
In most cases, the study of layer-by-layer horizontal and sagittal sections obtained during MRI allows us to establish the localization of the tumor process and differentiate it from a brain abscess, intracerebral hematoma, a focus of demyelination in multiple sclerosis, the consequences of severe traumatic brain injury, and a brain cyst. Definitive diagnosis of hemangioblastoma and determination of its microscopic type is possible only after a histological examination of the tumor sample. The tumor tissue needed for research can be obtained as a result of a stereotactic brain biopsy or during surgery to remove the tumor.
Main symptoms of malformations by location
A vascular anomaly can develop in any part of the brain, and accordingly, the symptoms will be directly related to the part of the head where the neoplasm appeared. A developing tumor not only puts pressure on brain tissue, but also affects the surrounding space, which contributes to disruptions in the functioning of this particular part of the brain.
When a malformation forms in the frontal lobe of the brain, the patient often experiences decreased vision, because the tumor affects the optic nerves. If the location of the tumor is the cerebellum, then the patient most often experiences disturbances associated with coordination of movements: unsteady gait, problems with fine motor skills.
Hemangiomas that develop deep in the brain tissue are characterized by a ringing in the ears or a sudden, aching headache.
Interesting fact: it has been scientifically proven that symptoms indicating the presence of a neoplasm most often appear in patients under the age of forty; in older people, hemangioma is usually detected during examinations, since it is practically asymptomatic.
Treatment of hemangioblastoma
The only radical treatment for hemangioblastoma is its complete removal. As a surgical approach, craniotomy is used with removal of a section of the occipital bone in the area of the foramen magnum and resection of the arch of the first cervical vertebra. Then the solid tumor node is completely removed. If the hemangioblastoma is cystic, removal of the node is combined with aspiration of the contents of the cyst, the walls of which often do not require removal.
Removal of a cerebellar tumor can be performed on an emergency basis if the cerebellum is herniated into the foramen magnum and there is compression of the brain stem. In such cases, to reduce intracranial pressure, a puncture of the lateral ventricle is first performed. If during the operation only partial removal of the hemangioblastoma is possible, which does not ensure normal cerebrospinal fluid outflow from the cranial cavity, then an additional shunt operation is performed: ventriculostomy, external ventricular drainage or ventriculoperitoneal shunting.
Radiation therapy can be used if there are contraindications to surgical treatment, in the case of multiple hemangioblastoma, or as an anti-relapse treatment when it is not completely removed.
What influences treatment results?
Unsatisfactory outcomes after surgical interventions, as clinical observations show, are not uncommon. Negative results are observed in approximately 11% of cases. This is a large number, despite the fact that hemangioblastomas in medicine are classified as benign and non-aggressive neoplasms. The most common complications that characterize an unsatisfactory outcome are hemorrhages in the remnants of the tumor and surrounding brain tissue, cerebral edema and hematomas, severe circulatory and liquor circulation disorders, and, as a consequence, early death.
Experts have identified a number of factors that have a direct relationship with unfavorable prognostic information after surgical treatment of hemangioblastomas:
- ventricular and brainstem localization of newly formed tissue;
- young age of the patient, male gender (consequences are more common);
- presence of Hippel-Lindau disease;
- dominance of the solid component in the tumor;
- solid element – more than 2.5 cm;
- Karnofsky index less than 50 points;
- degree of hydrocephalus (Evans index) above 45 points;
- unclear delineation of the tumor.
The scar after the operation will become less noticeable over time.
And one last thing. Now we will not reveal a secret to anyone, saying that a lot depends on the experience and qualifications of the surgeon. There are 2 main surgical-dependent factors that determine the outcome of surgical treatment - the adequacy of the choice of surgical tactics and the radicality of hemangioblastoma removal. Therefore, one of the main tasks for the patient is to get to a specialist with a capital “S”.
Central Military Hospital of Prague.
Today, Czech neurosurgeons are in great demand all over the world. Czech neurosurgery occupies one of the leading positions in the ranking of European countries in terms of the degree of development, quality and quantity of successful interventions, and is among the ten best countries in the world. In this country, operations for all oncological and other diseases of the brain are performed at an advanced level. With comparable quality of care provided, Czech central nervous system surgery services cost half as much as in Israel and Germany.
Forecast
Sporadic (single) hemangioblastoma is a disease with a favorable prognosis. In most cases (about 85%), patients are completely cured.
However, an important condition for cure is complete removal of the tumor. If it is not done, then the chances of a relapse of the disease in the near future are high. The prognosis looks less optimistic if we are talking about a tumor due to heredity (Hippel-Landau syndrome). In this case, the disease is expressed in multiple ways. Even with complete removal of the tumor, there is no guarantee that a similar tumor will not appear in another part of the brain.
In any case, if a patient is diagnosed with cancer, it should not be taken as a death sentence. If a tumor is detected in a timely manner, modern medicine in many cases allows for high-quality and effective treatment.