Main symptoms:
- Pain in the eyes
- Pain when turning head
- Protrusion of eyes
- Hallucinations
- Headache
- Dizziness
- Motor dysfunction
- Fine motor impairment
- Mental disorder
- Speech Impairment
- Inability to move independently
- Vocal cord paralysis
- Paralysis of limbs
- Increased intracranial pressure
- Loss of orientation in space
- Vomit
- Decreased vision
- Nausea
- Unsteady gait
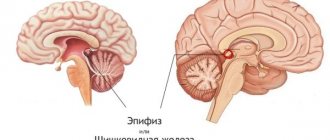
Brain glioma is a neoplasm formed from a variety of glial cells, which in turn is the tissue that covers neurons and ensures their adequate functioning. The development mechanism and predisposing factors leading to the formation of such a neoplasm remain completely unknown, despite the development of neurosurgery technologies.
Online consultation on the disease “Cerebral glioma”.
Ask a question to the specialists for free: Neurologist.
- Etiology
- Classification
- Symptoms
- Diagnostics
- Treatment
- Prevention and prognosis
Clinical manifestations will vary somewhat depending on the location of the glioma and its size. The most common symptoms include severe headaches and dizziness, nausea, paresis and paralysis, decreased visual acuity and seizures.
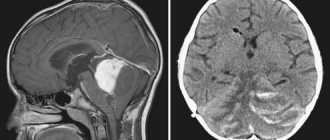
Diagnosing brain glioma in an adult or child can only be done using instrumental procedures based on MRI. It is noteworthy that laboratory tests are practically not used.
Treatment is aimed at excision of the formation, which can be done by several techniques, including chemotherapy, radiation or radiotherapy.
Classification of the disease
Glioma can be benign (grade 1) or malignant. Develops in 4 stages.
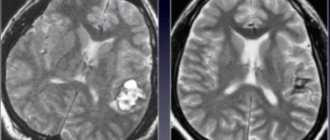
At the initial stage of formation, brain glioma is a benign tumor, or rather, it has a low grade of malignancy (low grade glioma). Easily amenable to chemotherapy. Benign formations are most often located in the cerebellum and cerebral hemispheres. They also occur in young people.
At subsequent stages, a malignant type of brain glioma is diagnosed. The last degree is characterized by the appearance of necrosis - glioblastoma multiforme.
The tumor begins with damage to the optic nerve - its glial elements become the point of development. The gradual growth of the tumor destroys the nerve, vision decreases greatly, and the eyeball protrudes.
Types of glioma localization:
- A diffuse type of brainstem glioma is formed in the area where the brain connects to the spinal cord. This part contains many nerve endings that are responsible for vital functions. This arrangement is life-threatening. The patient may experience impaired breathing, coordination, speech, and hearing. Diffuse glioma is more often diagnosed in children under 10 years of age. Glioma in the spinal cord spreads very quickly.
- Chiasmal glioma – such a tumor is located at the optic chiasm. Patients develop hydrocephalus and vision impairment.
Other types of education:
- by localization - above and below the cerebellum (supratentorial and subtentorial);
- by cell type - astrocytoma, oligodendroglioma, ependymoma;
- mixed – neuroepithelial, neoplasms of the choroid plexus.
Symptoms
Brain glioma can begin to manifest itself at an early stage of the disease. In most cases, the patient consults a doctor with complaints of neurological problems:
- headache not associated with changes in blood pressure, injuries, etc.;
- sensory disturbances in any part of the body (numbness, feeling of heat or cold, crawling sensation);
- paresis of the facial muscles, which can manifest as asymmetry of features, insensitivity of a limited area on the face, etc.;
- impaired coordination of movements and sense of balance (this is most noticeable when trying to change body position);
- disturbances in spatial perception (for example, the inability to accurately judge the distance to an object that needs to be picked up - this often looks like a person trying to grab air);
- increased sensitivity to bright lights, sounds, smells, or an inability to correctly interpret sensory signals.
Symptoms
Brain glioma produces a variety of symptoms depending on its location. General cerebral symptoms are typical - convulsions, severe pain, heaviness in the eyes, nausea. With optic nerve glioma, symptoms of decreased vision appear. With a tumor of the trunk, neurological abnormalities are observed. Glioma gives symptoms of incoordination, unsteadiness, changes in speech, and decreased sensitivity.
Chiasmal glioma causes narrowing of peripheral vision, dizziness, and tinnitus. When a brain tumor develops, mental abnormalities almost always occur. They manifest themselves in disturbances in thinking, memory, and behavior.
Focal manifestations of the disease:
- sensory disturbance;
- tinnitus, hearing loss;
- speech dysfunction;
- muscle weakness, which becomes a factor in paralysis and paresis;
- vestibular ataxia.
Glioma symptoms
The symptoms of a growing glioma directly depend on which part of the brain the tumor occupies. The neoplasm compresses tissues and membranes, which leads to cerebral symptoms:
- Severe headaches that cannot be relieved by taking analgesics and antispasmodics.
- The appearance of heaviness in the eyeballs.
- Nausea resulting from headaches. Patients also complain of periodic vomiting, which also occurs at the peak of an attack.
- Cramps.
If a glioma compresses the cerebrospinal fluid pathways and ventricles of the brain, hydrocephalus develops and intracranial pressure increases. In addition to general cerebral symptoms, glioma also affects the occurrence of focal manifestations of the disease, these are:
- Dizziness.
- Unsteadiness during normal movement.
- Visual impairment.
- Hearing loss or tinnitus.
- Speech function disorder.
- Decreased sensitivity.
- Decreased muscle strength, which causes paresis and paralysis.
In patients with brain glioma, mental changes are also detected, expressed by disorders of all types of memory and thinking, and certain disturbances in behavioral function.
Stages of development
According to the ICD, the degree of tumor development is assessed according to the danger to the patient’s life.
It develops in 4 stages, each with its own manifestations:
- I – benign tumor with slow development. It has a favorable prognosis with timely treatment. Life expectancy – up to 10 years;
- II – slow but constant development of the tumor process, signs of a malignant neoplasm begin, neurological symptoms increase;
- III – malignant process with a prognosis of 3-5 years of life, metastasis occurs to neighboring and distant organs;
- IV – rapid growth of a malignant tumor, with a prognosis of no more than 1 year of life, inoperable.
Diagnostics
At the initial stages of the disease, glioma of the chiasm and other parts is diagnosed extremely rarely, and this happens by chance. The first degree hardly manifests itself at all. Detected by computed tomography or magnetic resonance imaging.
Patients may contact a neurologist with complaints of hearing loss, constant dizziness and other neurological symptoms. In this case, the doctor prescribes a brain examination, and then diffuse glioma and its other types are detected.
Differential diagnosis is performed with the following pathologies:
- abscess;
- intracerebral hematoma;
- other tumors of the central nervous system;
- consequences of ischemic stroke;
- epilepsy.
To evaluate the disease, the patient is sent for magnetic resonance imaging, which fully shows the location and characteristics of brain damage. The patient may also be prescribed positron emission tomography, echoencephalography and other procedures.
The listed methods help to accurately visualize the process, but determining the type and degree of malignancy cannot be done without conducting a microscopic examination. Tissue analysis is possible when obtained during surgery or by biopsy.
Standard Treatments
The therapeutic management of patients with gliomas requires a large multidisciplinary team of medical specialists and healthcare providers. Patients typically present to the emergency department or are referred by their primary care physician for an MRI scan. The patient's brain MRI will then be interpreted by a radiologist or neuroradiologist. Once the initial diagnosis is made, the patient will be considered for neurosurgery to safely remove as much of the tumor as possible (surgical resection). 5-aminolevulinic acid (5-ALA) is a drug that may be given during surgery to cause tumor cells, especially malignant ones, to fluoresce and improve the extent of resection. After surgery, a neurologist will examine and characterize the tumor under a microscope.
Therapeutic management depends on the type of glioma, its size and location, and the specific characteristics of the patient. Especially in patients whose tumor cannot be completely removed because it is invading the brain in critical areas or is inaccessible, surgery will be followed by chemotherapy and radiation therapy. Therefore, collaboration between radiation oncologists and medical oncologists or neuro-oncologists will be required. Examples of chemotherapy for glioma include temozolomide and lomustine. These two drugs are part of a class of drugs known as alkylating agents. Their therapeutic effect is to damage the DNA of tumor cells, which leads to the death of tumor cells. Well-circumscribed gliomas can only be treated with surgical resection.
In addition to chemotherapy, medications prescribed to people with gliomas may include antiepileptic drugs (if the patient has epilepsy), anticoagulant drugs (if blood clots develop), and corticosteroids to alleviate neurological symptoms caused by fluid accumulation around the tumor (peritumoral edema). Neurologists and possibly other medical specialists may be needed to provide prescriptions and follow-up care for affected individuals.
Patients may need to undergo rehabilitation after surgery to regain functions affected by the tumor and surgery. Rehabilitation teams include many health care professionals, including physical therapists, occupational therapists, and nurses. Unfortunately, because some subtypes of gliomas are very aggressive, patients suffering from them may be forced to undergo palliative care, where they will receive optimal treatment to minimize symptoms and pain, including pain medications, antiepileptics and antiemetics.
Treatment
The main treatment for glioma involves a neurosurgical operation, which has its own difficulties, since any errors and inaccuracies lead to serious consequences, including death.
Removal of the tumor is performed in two ways:
- radiotherapy – used in the initial stages of a benign process to prevent relapse after traditional surgery;
- endoscopy – an instrument and a video camera are brought to the tumor, the tumor is removed. Chemotherapy is then performed. Every second patient requires a second operation.
Surgical intervention is performed for operable tumors in the initial stages. Traditional surgery is performed in an open manner, where the skull is opened and the tumor is removed, leaving healthy tissue intact. This treatment option does not provide a 100% guarantee of recovery; the risk of relapse is high.
Contraindications for surgery:
- severe stage of the malignant process with metastasis;
- unstable condition of the patient;
- the presence of other malignant tumors in the body;
- a special localization that does not make it possible to operate without disturbing important parts.
In addition to traditional radiotherapy, stereotactic radiotherapy is used - it allows you to act directly on the lesion without involving healthy tissue.
Radiation therapy is used both before and after surgery. The goal is to eliminate the remnants of the tumor and stop the growth of malignant cells. The course of treatment lasts several weeks. After radiation therapy, hair falls out, the patient experiences nausea and loss of appetite.
Radiation and chemotherapy cannot fully replace surgery. This is due to the fact that in the central part of the formation there is an area that is not susceptible to radiation. Then the procedures can only do harm without having any effect.
Complete removal of a brain tumor is an almost impossible task. This probability appears only at stage 1 of the process. The tumor actively grows into surrounding tissues, significantly infiltrating.
Possible consequences
Glioma is the most common and most dangerous brain tumor. The location of the tumor in the brain or spinal cord makes many treatment methods contraindicated, which affects the prognosis. This is due to the high risk of damage to important elements during surgery.
Glioma is a serious incurable disease, the life expectancy of which rarely exceeds 2 years. As the tumor grows, irreversible changes occur. The patient's vision is impaired, hearing deteriorates, and unbearable pain appears.
For relatives, the behavior of such a person becomes a problem, given that severe brain damage occurs, affecting mental processes. The patient may begin to behave unusually, displaying character traits that are unusual for him.
Brain Tumor Unit
The World Health Organization, part of the UN, has approved a classification of glial neoplasms, which are divided into 4 degrees according to morphological signs of malignancy - the presence of nuclear atypia (abnormal cell development), mitotic figures, endothelial microproliferation (reproduction of cells separating the lesion from the surrounding tissue) and area necrosis (death of tissue).
- Grade I includes non-cancerous neoplasms (not having a malignant origin). The first group includes pleomorphic xanthoastrocytoma, juvenile, giant cell and pilocytic astrocytoma, developing from slowly dividing astrocyte cells. Pilocytic astrocytoma in rare cases spreads to adjacent tissues and reaches large sizes. It is removed surgically.
- By II Art. tumors with a low level of malignancy are related, i.e., with the only sign of cancer transformation, mainly cellular atypia. This group includes diffuse astrocytoma, located in the brain region of the forehead and temples. People between the ages of 25 and 40 are prone to this type. Diffuse astrocytoma in the field of histology is divided into fibrillar, protoplasmic and gemistocytic - the most aggressive type, progressing to the third degree.
- Grade III includes anaplastic astrocytoma, which has 2 out of 3 signs: nuclear atypia, endothelial microproliferation and mitotic figures. The process of tissue necrosis is excluded.
- By IV Art. include gyoblastoma multiforme, in the development of which all 4 signs are involved, including the area of necrosis.
Brain gliomas are further divided into 2 subtypes depending on the location of the tumor formation:
- subtentorial, located in one of the hemispheres; with large tumor sizes, intracranial pressure occurs as the main symptom of the disease;
- supratentorial are located in the posterior fossa of the skull, where spinal and venous outflows occur, which are compressed by the neoplasm and cause the symptom of hypertension.
Gliomas are single types of tumors located in the area of the white and gray matter of the brain or spinal cord; they occur in 6 out of 10 patients with tumors. Quite often pathological growths are found near the central canal and the walls of the ventricles. Occasionally, gliomas of the peripheral part of the visual analyzer are formed. In isolated cases, they form in nerves located outside the brain or spinal cord.
Gliomatosis is a rare type of diffuse glial neoplasm that widely penetrates the structure and affects both lobes of the brain. There are no exact statistics on the percentage of glioma formation in the human body today, but it is known that the number of oncological pathologies has increased significantly.
Description of glial tumors
Brain glioma varies in size from 2 to 100 mm in diameter, has a round shape, and in rare cases, spindle-shaped. Glial neoplasm develops quite slowly and can grow over the course of a year, two or more years without metastasizing. In exceptional situations, the opposite and uncharacteristic development is possible. Gliomas in cross-section have the appearance of a node with fuzzy contours from gray-white to pink, in rare cases, dark red. Often, even under a microscopic instrument, it is difficult to separate a tumor from healthy tissue, especially with the specifically rapid division of glia - the cells that form the growth of the tumor. In isolated cases, a glial tumor grows through the membranes of the brain, gray and white matter and extends into the skeletal system. These exceptions include gliomatosis.
During diagnosis, you can see the basis of the glioma, which consists of many neuroglioma cells with plasmatic processes with an admixture of fibrous glia. Glial neoplasms are divided into 3 types based on their internal structure:
- dense consist of a small number of cells with small nuclei, less protoplasm and a larger number of fibrous glia;
- soft ones have many cells with large nuclei, mostly irregular in shape and insignificant fiber content, very similar to sarcoma, which is why they are called glioplastic sarcoma;
- giant cells consist of very large glial cells, in some cases containing coarseness and mottling.
A glioma that has a gelatinous edema is called myxoglioma. Its cells are arranged in the form of a bell-shaped fence or in chain-like rows that unite the vessels and processes of the meninges. Depending on the location, size and clinical symptoms, glial cells and nerve processes can independently degenerate or remain intact within the neoplasm itself.
Glioma in children
Diffuse malignant glioma of the brain stem in children has irreversible consequences that lead to death. After surgery, the survival rate is 25%. For benign chiasmal glioma in young children, radiosurgery is performed followed by rehabilitation, which can improve the quality of life.
With timely diagnosis and treatment, the child will live more than 5 years. If the disease is detected at the last stage, attempts to fight the tumor become useless. Then life expectancy will not exceed 2 years.
Benign tumors at the initial stage are successfully operated on. In case of a malignant process, treatment is aimed at improving the quality of life and reducing the severity of symptoms. In most cases, surgery helps improve the patient's condition.