Neurosis-like schizophrenia is one of the variants of schizotypal disorder (formerly called sluggish schizophrenia), in which symptoms of neurosis and a psychopathological process are combined in an unusual way. This is a chronic disease that can be controlled and treated using modern methods.
Only an experienced psychiatrist can distinguish true neurosis from neurosis-like conditions in schizophrenia.
In ICD-10, this disorder is coded as F21.3 and is included in section F21 Schizotypal disorder. In the literature there are synonyms “prepsychotic schizophrenia”, “prodromal schizophrenia” and “borderline schizophrenia”.
The question of the causes of pseudoneurotic schizophrenia remains open. The leading one is the genetic approach, according to which gene defects lead to an imbalance of mediators in the brain system.
Neurosis-like schizophrenia: symptoms and signs
With neurotic schizophrenia, there are no delusions or hallucinations - patients do not hear “voices” and are not afraid of persecution or influence from imaginary ill-wishers, as is the case with classical schizophrenia. Therefore, it is classified as an atypical form - schizotypal disorder. Negative symptoms are present, albeit in a smoothed, slowly developing form: the ability to experience vivid emotional experiences decreases, will and motivation are lost, and fatigue appears.
Neurotic manifestations come to the fore (hence the name of the disease), but a persistent psychopathological background - symptoms decrease only with adequate therapy - allows us to qualify the process as pseudoneurosis. Patients experience obsessive fears (phobias), perform compulsive actions (rituals), and are overly concerned about their appearance or health.
When working with a patient, a psychiatrist pays attention not so much to the content of the patient’s fears—whether he is afraid of surveillance or spiders—but rather to the order of development of symptoms and their connection with stress, head injuries, or taking psychoactive substances (alcohol, drugs).
The first signs of the disease in the form of obsessions (fear of the dark, fear for the health of parents) can appear from childhood. But persistent psychopathological changes are formed only in adolescence (18–20 years). Phobias and obsessions determine the picture of the disease and practically do not change over time. For example, if a person was afraid of closed spaces, then over the years, within the framework of neurosis-like pseudoneurotic schizophrenia, he will not begin to worry much about his appearance or be afraid of insects.
The course of neurosis-like schizophrenia is favorable and is characterized by a high number of remissions. A person does not develop schizophrenic dementia and, with well-chosen therapy, can continue to work, get married, raise children, and live a full life.
How to diagnose and treat neurosis-like schizophrenia?
Diagnosis of sluggish schizophrenia is based on clinical and anamnestic data (identification of symptoms by a psychiatrist). A clinical psychologist is involved in making a diagnosis, the disorder is confirmed by laboratory and instrumental methods (Neurotest, Neurophysiological test system).
The main methods of treatment are psychotherapy and pharmacotherapy.
Psychotherapy is a non-drug treatment method that is necessary for fruitful cooperation between doctor and patient and increases motivation for treatment. With its help, patients cope with obsessions and receive stable remission, getting rid of pathological attitudes.
To avoid exacerbations or transition to schizophrenia, you need to carefully follow your doctor’s recommendations. A psychotherapist helps both the patient and his family cope with the disease.
Types of psychotherapy:
- individual - helps a person realize the groundlessness of worries and worries, effectively deal with obsessions;
- family - allows you to resolve family conflicts and problems that may interfere with the establishment of stable remissions;
- group - teaches the patient to adapt to the social environment, helps to establish emotional contact with others.
The rapid development of the pharmaceutical industry in recent years has given us a huge number of high-quality and effective drugs that a person without a medical education will not be able to understand. In the case of neurosis-like schizophrenia, it is not enough to simply choose a treatment regimen. Depending on the prevailing symptoms, the attending physician prescribes antipsychotics, antidepressants, tranquilizers, and nootropics. It is often necessary to change doses and drugs within the same group to achieve maximum effect.
Neuroses, as well as many other endogenous mental pathologies, which can also include low-grade schizophrenia, are called diametrically opposed diseases by psychiatrists. They have their similarities, but there are also differences. The treatment of neuroses is carried out by a psychotherapist, without the help of a psychiatrist, while the treatment of endogenous mental pathologies is the prerogative of psychiatrists. Determining neurosis or schizophrenia is not always very simple, since patients can deliberately imitate the clinical picture of the disease.
It should be noted that what distinguishes schizophrenia is that this disease does not have a so-called starting point or cause. This is a chronic genetic pathology, which in extremely rare cases can develop against the background of prolonged stress, alcohol abuse, after childbirth, and these are considered only trigger factors.
Neurosis is often caused by some situation that has affected the human psyche. It could be severe stress or fear, fatigue. It is important to understand that such a pathology is unlikely to be chronic and continuous with rare attacks of exacerbation. It is also necessary to understand that the fear of transformation of one disease into another has no basis.
Forecast and prevention of attacks of low-grade schizophrenia
The disease has a favorable prognosis. With an integrated approach to treatment, attacks will be extremely rare. Such patients will remain active members of society and will be able to fully perform work duties.
To reduce the risk of relapse of the disease, you must adhere to the treatment regimen prescribed by the doctor. Often it is the independent withdrawal of drugs that leads to an increase in attacks. In addition, it is important to avoid conflicts in the family and strive to protect the sick person as much as possible from possible stress.
Author of the article:
Sokov Andrey Vladimirovich |
Neurologist Education: In 2005, she completed an internship at the First Moscow State Medical University named after I.M. Sechenov and received a diploma in the specialty “Neurology”. In 2009, she completed her postgraduate studies in the specialty “Nervous Diseases”. Our authors
Fundamental difference
The main difference between neurosis and schizophrenia is that the first condition remains critical of itself. A person may realize that he has problems and fear. As a result, the patient tries to understand what is happening to him, can seek help from specialists, and undergo diagnostics. If there are no signs of somatic pathology, which should correspond to the complaints, the best decision would be to refer you for treatment to a psychotherapist.
Psychoses are characterized by completely different behavioral signs. Patients can hardly name today's date or day of the week, are confused about their location, and can sometimes call themselves another person or identify with them. Healthy mental functions familiar to all people, such as thinking, emotions and will, are significantly split. Even when the period of psychosis ends, it is difficult to say that this patient is normal. This is due to the fact that he has a significantly reduced criticism of the events around him, of himself, he can say ridiculous phrases and sentences, and the manner in which his emotions manifest themselves will only cause bewilderment in a healthy person. It is worth noting that not understanding oneself becomes painful. At the same time, such a patient will not go to a doctor for help, trying to hide the problems he has encountered from others.
Features and causes of latent schizophrenia
It is impossible to give a definite answer to the question of what it is - latent schizophrenia. This disease is detected in patients with a mild course, not accompanied by hallucinations and delusions at the initial stage. Mental disorders arise gradually. Officially, psychotherapists do not make such a diagnosis, since it is not included in the international classification.
The exact reasons for the progression of schizophrenia have not been identified. There are several theories:
- Dopamine. Associated with an increased concentration of the substance of the same name. As a result, nerve endings are stimulated and false impulses are generated. This contributes to disruption of brain function.
- Serotonin. It is believed that excessive release of serotonin, which disrupts the transmission of nerve impulses, can influence the development of schizophrenia.
- Noradrenergic. The theory describes the negative effects of inadequate production of adrenaline, norepinephrine and dopamine on the brain.
- Dysontogenetic. Researchers suggest that the progression of the disorder may be due to abnormalities in brain development. This brings the theory closer to hereditary. The trigger mechanism can be viruses, infections, toxic substances and other factors that can disrupt the functioning of brain centers.
- Psychoanalytic. The disease can develop as a result of split personality, inadequate perception of the surrounding world and oneself. Schizophrenia progresses if one’s own “I” begins to prevail over external circumstances. The course of the pathology is aggravated by a negative perception of the surrounding world.
- Hereditary. Confirmed by statistical data. If a child has one parent who is ill, there is a 12% chance of developing schizophrenia. If both father and mother suffer from the pathology, the risk of the disorder increases to 40%.
- Constitutional. It is believed that certain personality traits may contribute to the development of the disease. For example, an atypical physique or negative character traits.
- Cognitive. Scientists suggest that the progression of pathology may be associated with misunderstanding of others. For example, if a child shares his experiences with his parents and is faced with negative emotions, he may become withdrawn and isolated from the outside world.
- Autoimmunization and autointoxication. It is assumed that the cause of the development of the disease may be poisoning of brain tissue by protein breakdown products. This disrupts the functioning of the nervous system.
Patients often experience the first symptoms during adolescence during a period of hormonal fluctuations, so it is believed that this may influence the development of the disease.
Hallucinations
One of the most reliable signs that distinguish neurosis and schizophrenia is hallucinations. At its core, this is a deception of perception, which can be delusional in nature. They usually occur during the onset of psychosis in people suffering from schizophrenia. They can occur extremely rarely in neuroses, but their distinctive feature is their short duration, simplicity, and also the fact that they have a close connection with sleep, that is, they occur during falling asleep or waking up. In neurotics, they can occur as repeatedly repeated thoughts, images, such as spots, pictures.
In patients with schizophrenia, hallucinations are often of a different nature, which may not even have an image, but be in the form of voices. They argue, swear, criticize the patient, make him afraid, thereby provoking feelings of influence on the person. That is, someone invisible forces him to perform some action. Sometimes schizophrenics say that they are subject to some kind of influence, for example, hardware influence. A distinctive feature of such hallucinations is the fact that voices or devices are visible only to the patient who is 100% sure of it.
Classification
In the International Classification of Diseases, 9th revision (ICD-9), latent schizophrenia was coded 295.54[7], and in the version of ICD-10 adapted for use in the Russian Federation - F21.1[8]. F21.1 also includes prepsychotic and prodromal schizophrenia[8]. In ICD-10, latent schizophrenia is considered a subtype of schizotypal disorder.
The American Diagnostic and Statistical Manual of Mental Disorders, Second Edition (DSM-II) also included “latent type of schizophrenia” (eng. schizophrenia, latent type, code 295.5)[9]. It has been described as a diagnostic category for patients who have overt schizophrenic symptoms but no history of a psychotic schizophrenic episode[9]. This diagnosis was excluded from subsequent publications.
How to diagnose
Schizophrenia differs from neurosis in that neurotics retain their personality. In other words, all the personal qualities that characterized a person before the disease - determination, emotionality - remain with the development of neuroses. It is also important to note that neurosis is reversible. The patient receives a course of treatment from a psychotherapist, after which he simply returns to his normal, familiar life, only he already acquires some new skills of self-control and reaction to various stimuli, which led him to neurosis.
Schizophrenia eventually leads to the development of apatoabulic syndrome. It is a condition in which a personality defect develops over the years. Patients are very lethargic, apathetic, emotions are manifested very weakly due to a decrease in the ability to do so. And the clinical picture is growing, voices and delusional ideas are becoming stronger. You shouldn’t expect any initiative from such a person; he closes himself off in himself, his world, and is less and less interested in reality. This provokes disability; there are cases where patients have lost the ability to independently take care of themselves and care for themselves.
You can distinguish neurosis from schizophrenia without outside help using online tests for neurosis, which are freely available on the Internet. It is important to read the instructions carefully to avoid misinterpretation of the results. If you cannot do this yourself, then you need to consult a doctor who knows exactly how to distinguish between these two diseases.
One form of schizophrenia is pseudoneurotic schizophrenia. It is not considered classical, which can be seen in all classifications of diseases. This is a state that can be quite comfortable for a person’s life, since he can remain in it for a very long period of time - up to 30 years.
At this time, psychopathic-like, neurosis-like and other disorders that occur in schizophrenia may develop. But most of all the patient suffers from fear and neurotic attacks. The difference is that there is no progression of the personality defect, and there are no hallucinations or delusions. Other manifestations of this disease may include:
- Unfounded fears;
- Emotional lability;
- A craving for studying subjects that are boring for an ordinary person - philosophy, mysticism;
- Decreased productivity in daily life;
- A person stops taking care of his appearance.
Such people remain socially active, but they rarely complete their education. Sometimes such patients even work, but this work is very unstable, since they give preference to those places of work where they do not need to be active, experience stress, or strain. They rarely have a family, which is due to constant fear with a tendency towards progress, as well as pathological lability of emotions. For example, if a person is afraid of any public transport, then over time he will simply completely stop using it. Sometimes these fears reach the point of absurdity.
Notes
- ↑ 123V. M. Bleikher, I. V. Kruk. Latent schizophrenia // Explanatory dictionary of psychiatric terms. - MODEK, 1995. - ISBN 5-87224-067-8.
- ↑View V. D. Psychotherapy of schizophrenia. — Publishing house “Peter”. - P. 66. - ISBN 978-5-91180-747-4.
- ↑ 123Garrabé J. Histoire de la schizophrénie. - Paris: Seghers, 1992. - 329 p. — ISBN 2232103897. In Russian: Garrabe J. History of schizophrenia / Trans. from fr. M. M. Kabanova, Yu. V. Popova. - M., St. Petersburg, 2000.
- ↑V. D. View. Psychotherapy of schizophrenia. — 3rd ed. - Publishing house "Peter", 2008. - P. 66. - 512 p. — ISBN 978-5-9118-0747-4.
- ↑ 123 Zhmurov V. A. Psychiatry. Encyclopedia. - T/O "Neformat", 2016. - P. 341.
- ↑Sternberg E. Ya., Molchanova E. K., 1978
- ↑World Health Organization. Section V of the “International Statistical Classification of Diseases, Injuries and Causes of Death, 9th Revision,” adapted for use in the USSR. - M., 1983. - P. 29.
- ↑ 12World Health Organization. Class V: Mental and behavioral disorders (F00-F99) (adapted for use in the Russian Federation). Part 1 // International classification of diseases (10th revision). - Rostov-on-Don: Phoenix, 1999. - P. 125. - ISBN 5-86727-005-8.
- ↑ 12American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Second Edition (DSM-II). - Washington, DC: American Psychiatric Publishing, 1968. - P. 34.
Treatment
Treatment of neurosis-like schizophrenia consists of psychotherapy sessions, sometimes it is possible to prescribe mild tranquilizers or sedatives.
Typical neurosis can also be treated by visiting psychotherapists; the need for psychotropics rarely arises. Usually these are short-term courses.
Schizophrenia requires constant, sometimes even lifelong, use of medications.
Schizophrenia and neurosis are two diseases that can often be very similar in their external signs. An experienced doctor can correctly carry out a differential diagnosis, but primary screening can also be done at home through online testing.
Obsessive-compulsive disorder (OCD) is a neuroses. Always has a starting point (cause) that led to disruption of the central nervous system. It manifests itself as anxiety, obsessive ideas that force a person to perform certain actions repeatedly, not paying attention to the fact that he is going beyond normal behavior.
Neurosis and schizophrenia
OCD and schizophrenia are not the same thing, but two completely different diseases. Neurosis begins with an acute, traumatic process for the psyche:
- physical, emotional exhaustion;
- loss of a loved one or pet;
- childhood fears;
- a serious illness that makes you rethink reality;
- constant stress.
Obsession is combined with phobic disorders and certain actions that are repeated regularly. This type of deviation is divided into 2 types.
- Relatively safe.
- Leading to irrational fear, causing severe anxiety.
The first includes deviations characterized by a relatively calm course that does not cause harm to patients. The desire to talk about your memories to everyone.
The second is characterized by constant self-analysis, which often leads to attempts to withdraw from society and abandon a certain type of activity.
In schizophrenia, it is impossible to determine the cause. This disease is transmitted genetically and has a chronic course.
It can occur continuously or appear in paroxysms, followed by remission. The above-described provoking factors of OCD cannot be the cause of schizophrenia, but only aggravate its course. Accordingly, neurosis cannot develop into schizophrenia, but can be an accompanying symptom.
Main differences
Schizophrenia is very different from OCD. Neurotics retain common sense and are able to critically evaluate their actions and condition. They are aware that such a condition is not the norm, and they try to actively solve the problem on their own or by contacting a specialist.
The main difference between schizophrenia and OCD is the inability of patients to indicate their location, time, and self.
In patients, all mental functions are split. Even after emerging from a state of psychosis, the patient remains uncritical, behaves strangely, and his statements cause bewilderment among others. Schizophrenics are burdened by an incomprehensible condition, but they do not rush to see a doctor, but try to hide their problem, not only from others, but also from themselves.
The difference between OCD and schizophrenia lies in the state of patients at the time of the appearance of hallucinations. They occur in many disorders. Thus, a neurotic sees a short-term phenomenon in which there is a meaning that connects the pathological state with the starting point: dark circles, melodies, visual images. Hallucinations appear more often before sleep, when the brain is practically turned off, and at the moment of awakening, while brain activity is still weak.
In schizophrenics, hallucinations are violent.
They hear voices that often criticize the behavior of those around them or those around them and try to persuade them to take certain actions or rituals. This process instills fear in the patient, he tries to hide. Patients are sure that these voices are messages from above. Delusions occur in schizophrenic disorders. Abnormal ideas transport a schizophrenic to a completely different reality, replacing real concepts. If the patient begins to be dissuaded in his views, he reacts aggressively and refuses to communicate.
In the ICD-10 classification, this condition is reflected as pseudoneurotic schizophrenia (not to be confused with real schizophrenia). This condition can last 10-30 years without causing much discomfort to the patient. A person suffers more from neurosis and unreasonable fear. The personality defect does not progress; there are no hallucinations or delusions.
The main symptoms of OCD in schizophrenia:
- strange behavior;
- emotional instability;
- desire to explore areas of philosophy, teachings related to the occult sciences, theories of abstractionism;
- reluctance to take care of one’s appearance, complete apathy in this regard; decreased productivity, reluctance to work;
- unreasonable fears;
- the emergence of ideas that become extremely important in the individual’s perception. Patients feel that their aspirations are underestimated.
An individual usually maintains connections with society. His work does not satisfy him, he tries to find a place where he can avoid problems and earn money without putting in much effort. Patients of this type very rarely start families, because they have problems communicating with the opposite sex or have too high demands. Existing fears progress, reaching the point of absurdity.
Depersonalization and OCD
Depersonalization is considered a separate disease, but it can accompany some mental disorders. It has been proven that this condition can occur in any person at different points in the life cycle.
Depersonalization in OCD is defensive in nature. The body tries to adapt to certain life difficulties, the brain tries to distance itself from painful memories. The patient is fully aware of the delusional state, but cannot cope with it, perceiving himself completely differently. There is a strong desire to free yourself from obsessive thoughts and feel relief.
Schizophrenics take depersonalization for granted, losing their own “I”, turning into a completely different personality.
Reasons that provoke the appearance of depersonalization syndrome:
- severe shock;
- long-term sluggish clinical depression;
- trauma leading to a change in psychological status;
- schizophrenia, OCD, manic syndrome, autism;
- drug addiction, alcoholism.
In neurotics, depersonalization often becomes a consequence of self-examination, when patients begin to think about what they have achieved in their years, try to recall events that they cannot correct, and reproach themselves for this. In schizophrenia, depersonalization can lead to a state close to coma.
The problem does not require special treatment for neurotics. Usually of a short-term nature. It manifests itself as loss, inability to sensibly assess the situation, and fear of going crazy. Patients do not feel hungry and may refuse to relieve their natural needs. because they feel as if they are in someone else’s body.
Diagnostics
Diagnostics will help determine whether a patient has OCD or schizophrenia.
With compulsive disorder, patients suffer from depression, weakness, and may fall into depersonalization, but personal qualities and individuality are preserved. Neurosis is reversible. A course of psychotherapy returns patients to a normal state. They are able to cope well with conflict situations, without going to extremes, and not paying attention to the difficulties that arise in the process of work or relationships with the opposite sex. OCD cannot turn into schizophrenia. These are two different disorders. The first refers to psychological, the second to psychiatric, is chronic.
A schizophrenic is a ticking time bomb. Apatoabulic syndrome increases over time. A personality defect appears. Emotional aspects of life become inaccessible. Voices appear, indicating what to do, how. One's own personality is lost, the individual becomes uninitiative. Painful fantasies touch the most hidden corners of the soul, upsetting the balance between awareness of reality and fiction. Schizophrenics do not realize that they are sick. Attempts to hint at this cause a wave of aggression, patients pull away. Often the state of apathy progresses into a phase when the individual becomes helpless, unable to take care of himself. A test for neurosis helps to establish an accurate diagnosis.
Therapy
Treatment for OCD comes down to psychotherapy. During classes with patients, prevention of social maladjustment is carried out. The main goal of the sessions is to determine the starting point. By eliminating the cause, patients can return to normal life. Relief of symptoms is carried out only in selected cases. Mild sedatives may be prescribed; for severe psychosis, antidepressants are used. After treatment, patients are advised to avoid severe shocks and visit a doctor at least once a year.
Schizophrenia is treated with medications. The drugs can be prescribed for life.
Psychotherapy is appropriate only for patients who maintain common sense and have a combination of OCD and schizophrenia.
How to distinguish neurosis from sluggish schizophrenia?
The diagnosis of schizophrenia is often questioned by psychiatrists. A carefully collected anamnesis and observation do not always confirm the presence of the disease. Depressive, neurotic and personality disorders in some manifestations are similar to the symptoms of low-progressive schizophrenia, so diagnosis is difficult. The difference between sluggish schizophrenia and neurosis is that the personality of neurotic disorders is preserved. There are other differences:
- Neurosis is based on a specific psychotraumatic situation as a starting point that worsens over time (prolonged stress). Schizophrenia is genetically determined.
- With neurosis, a person retains the state of what happens to him. In schizophrenia there is no criticality.
- Over time, the symptoms of sluggish schizophrenia worsen, the personality defect increases: emotions become scarce, painful fantasies intensify, will disappears. Neurosis is a condition that can be corrected and reversible.
The first signs of the disorder are observed in adolescence. The onset of sluggish schizophrenia can be provoked by the use of psychoactive substances, alcohol, or a severe stressful situation. Making a diagnosis is difficult, since the symptoms become clear only at the peak of the disease. At an early stage, all manifestations are similar to many mental disorders. Sluggish schizophrenia - symptoms:
- decreased activity;
- narrowing your circle of interests and friends;
- strangeness and eccentricity are noted in behavior;
- fears;
- obsessive thoughts, ideas;
- depersonalization (a person hears and sees himself as if from the outside);
- episodic hallucinations;
- emotional impoverishment, coldness.
Symptoms also depend on the predominant type of sluggish schizophrenia:
- Psychopathic-like schizophrenia
. Characterized by the loss of “I”: when looking in the mirror, they perceive themselves as an outsider. Pretentiousness and mannerism predominate in behavior, the person is prone to hysterics. Deceitfulness and tendency to vagrancy are increasing. - Neurosis-like sluggish schizophrenia
. Characterized by the presence of various kinds of phobias, a person over time acquires various kinds of fears:
- agoraphobia;
- mysophobia;
- cancerophobia.
Signs of low-grade schizophrenia in men
The development of the disease, its course and symptoms depend little on the patient's character and individual characteristics, but according to average statistical data, low-grade schizophrenia in men begins at an earlier age, progresses faster, and treatment requires a more comprehensive and lengthy treatment. The peak of the disease occurs between 19 and 28 years of age. Signs of the disorder typical for men:
- rapid impoverishment of the emotional sphere;
- in conversation: incoherent speech with pretentious fragments of phrases;
- severe apathy;
- delusions and hallucinations;
Signs of low-grade schizophrenia in women
Sluggish schizophrenia in women has the same symptoms as in men, but in a less pronounced form. The disease debuts later, does not develop so rapidly, and the personality defect is slightly expressed. Treatment is more successful. Symptoms of low-grade schizophrenia in women:
- Appearance: hairstyle, clothes, makeup undergo changes. The woman becomes sloppy, rarely washes, begins to put on vulgar make-up and dress, or completely neglects herself.
- Household chores cease to interest the woman; she may begin to bring various rubbish home and store it away.
- Mood swings throughout the day: hysterics (laughter, sobs), aggression or sadness, tearfulness.
- Paroxysmal course of the disease.
The neurosis-like form of schizophrenia is one of the most favorable types of the disease with pronounced periods of remission. It belongs to one of the types of sluggish schizophrenia, in 42% of cases it occurs in adolescence. Persistent remissions of the disease are observed in 37% of cases; they last on average from six months to several years. The symptoms of the pathology at the beginning of their development are similar to neurosis, so an important task for treatment is the early diagnosis of schizophrenia.
Signs of a latent form of schizophrenia
Possible symptoms include the following:
- Eccentricity. A person’s movements can be careless and angular. The overall appearance gives the impression of sloppiness. The patient may wear mismatched clothes. Pretentious expressions predominate in speech. When talking, the patient is distracted from the essence and describes the details in detail.
- Pseudopsychopathization. The patient generates many ideas and attracts everyone around them to their implementation, but does not achieve practical benefit.
- Passivity. Patients tend to spend most of their time at home. They don't have enough energy to do anything.
- Zigzag behavior. At first, a person gets down to business with great enthusiasm and works hard, then there comes a period of inactivity.
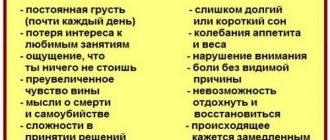
- Tendency to self-isolation and depression. Patients often analyze themselves and their actions. Suicidal ideas may appear.
- Inappropriate reaction to what is happening. Paradoxical emotions arise. Patients may laugh when receiving bad news.
- Lack of interest. Patients become indifferent even to those activities that they previously enjoyed.
- Low motivation. Patients often do not take care of their appearance. For example, they may refuse hygiene procedures because they do not see the point in them due to the need for repetition.
- Conflicting emotions. Patients often experience mood swings. They are capable of experiencing mutually exclusive feelings at the same time.
- Autism. Patients focus on internal sensations and isolate themselves from others. They are reluctant to make contact with people. They prefer monotonous work.
There is no single clinical picture, since there are many variants of the course of the disease. 1 or 2 symptoms are not enough to make a diagnosis; the general characteristics are taken into account. In most cases, latent schizophrenia does not lead to personality degradation. Patients retain the ability to partially adapt to society and often lead a normal lifestyle. Under unfavorable circumstances, another form of schizophrenia develops, but the disease remains sluggish and, in the absence of treatment, takes a long time to progress to the next stage.
Symptoms of latent schizophrenia in men
The signs of latent schizophrenia in men and women are almost the same, but in the former the disease is most often detected earlier. The course in some cases is more severe and can lead to the development of other types of pathology. There are no periods of remission; symptoms persist throughout the progression of the disease. Patients drink alcohol more often and have conflicts with others, which results in injuries.
Symptoms of latent schizophrenia in women
If, due to the characteristics of schizophrenia in men, behavior often becomes aggressive, then in women passivity and depression predominate. In some cases, irritability occurs, which becomes the cause of alienation.
Women may distance themselves from loved ones. Patients either conflict or prefer to remain silent and not express their opinions. Sloppiness predominates in appearance.
Neurosis or schizophrenia?
The onset of the disease most often occurs in adolescence, without analyzing the pathological history; the primary symptoms are similar to neurosis. But the differences between schizophrenia and neurosis are still preserved. People suffering from neurosis are looking for help, they are trying to find out the true cause of their condition, they go to doctors. In the case of schizophrenia, patients do not realize the seriousness of their condition; this problem worries the relatives more than the patient himself.
It is also important to note that neurosis occurs against the background of previous negative events in a person’s life; it does not begin without a reason. The causes of neurosis can be various events, for example:
- severe stress;
- emotional overload;
- suffered a serious illness;
- loss of loved ones, etc.
In cases of schizophrenia, the exact reasons for its development cannot be established, except for a genetic factor that is not inherent in neurosis.
Regarding the course of one and the second pathology, their symptoms also differ. With neurosis, a person’s personal individuality is completely preserved. Despite the depressed state of neurosis, the patient retains his sense of purpose, emotional background and individuality. Schizophrenia, with its long course, leads to varying degrees of severity of the personality defect. The emotional side of a person becomes poorer, he becomes indifferent to the events around him, moves away from society, withdraws into himself and plunges into the world of his own fantasies. There are often cases when a patient cannot care for himself, which leads to his disability.
Unlike schizophrenia, neurosis is a completely reversible pathology; the sooner psychotherapeutic treatment is carried out, the easier it will be to cope with the disorder. Thus, after a while, the person returns to a normal, fulfilling life. And in the case of schizophrenic disorders, the personality defect only grows over the years and, at best, only long-term remission can be achieved.
Characteristics of symptoms
As mentioned above, emotional disorders are one of the main symptoms of a latent form of schizophrenia. These disorders are apathetic in nature and are characterized by slow fading and dimming of emotions. A person suffering from schizophrenia gradually becomes cold, alienated, callous, and incapable of empathy. All his emotions and feelings lose their brightness and natural strength, become amorphous and monotonous. Sometimes paradoxical emotional reactions arise, which subsequently begin to increasingly dominate the patient’s emotional spectrum. Such apathetic disorders are necessarily accompanied by a decrease in will, initiative, inactive indifference, lack of meaning in life and loss of life goals. However, at the same time, certain normal emotional manifestations are preserved, arising, as a rule, in connection with some minor life events.
In addition to emotional disorders, the next main symptom of the latent form of schizophrenia is splitting. This pathological symptom is characterized by the following manifestations. First of all, the patient experiences a lack of unity of mental processes, which leads to a loss of semantic connections of feelings, thoughts and actions. In the patient’s behavior and statements, this manifests itself as the coexistence of the paradoxical, absurd with the real, life-like. In addition, the patient experiences a loss of life goals and a predominance of paradoxical thoughts and ideas in his worldview. Thus, real life seems to be removed, and the main place in the consciousness of a person suffering from a latent form of schizophrenia is occupied by fantastic and absurd conclusions. Combinations of thoughts of completely opposite content are not uncommon. The following phenomena are also observed:
- discrepancy between emotional and facial reactions and statements;
- influxes of thoughts;
- delayed thinking;
- distortion of the experience of self-worth;
- speech interruption;
- distortion of the meaning of words and concepts;
- lack of arbitrariness of motor acts.
In addition to clefting, patients also exhibit manifestations of autism of varying degrees of intensity. As a rule, it is expressed in a lack of desire for activity, for communication with others, for knowledge of the world around us. At the same time, the patient’s life position is limited only to his inner world, and contact with the doctor becomes formal, superficial. The severity of autism depends on the intensity of symptoms such as dissociation and emotional disturbances.
In addition, it must be said that the characteristic features of a latent disease are the absence of productive symptoms and the mild severity of general symptoms.
Clinical picture of neurosis-like schizophrenia
The main symptoms characteristic of the neurosis-like form are dysmorphophobic and dysmorphomanic disorders. Such conditions are characterized by the patient's confidence in his own ugliness. The most common age of onset of these symptoms is between 13 and 20 years of age. Most often, the patient focuses his attention on some part of his body, considering it ugly, for example, a large nose or ears, an unattractive shape or size of the breast, crooked legs, etc. In fact, the defect simply does not exist, or it exists but quite insignificant, but the patient considers it a real deformity.
Another pronounced symptom of the neurosis-like form is metaphysical intoxication. This is a condition in which the patient has thoughts about the so-called “eternal problems”. It is thoughts that come to the fore, not actions; they are unproductive and fixated on one topic. Reflections take on the character of overvalued ideas; it is impossible to convince the patient otherwise. Any criticism is perceived sharply by him and only further assures him of his specialness in front of others. The patient can think about the meaning of life, the existence of other civilizations, the purpose of humanity, etc. Often, philosophical ideas in schizophrenia are especially pretentious and absurd; the patient can sit for hours writing something in a notebook, but, as a rule, nothing related can be read from what is written down .
In addition to these symptoms, patients develop obsessive fears. They may be afraid of some object or thing, as a result of which they come up with a ritual for themselves that should help overcome fear. As a rule, such rituals are pretentious, ridiculous and funny to others. Among the symptoms of a neurosis-like state, hysterical features are also observed. In schizophrenia, they are mannered, theatrical in nature, and there is a kind of “playing for the audience.” Patients can dress ridiculously, combining things that are completely incompatible with each other, for example, wearing socks, shorts and a fur coat of different colors. Such behavior repels others, causes confusion, and sometimes even fear.
Hypochondriacal experiences also occur among the symptoms of the disease. Such experiences manifest themselves in the form of illnesses invented for oneself. For example, a person is sure that he has an incurable disease that no one has suffered from before. Manifestations of hypochondria can be anything, this is a kind of self-hypnosis about the severity of one’s condition. Another example, a patient may imagine that he has an accumulation of pus in his body, in some organ, and he imagines how it spreads throughout the body, poisoning it, as a result of which he will soon die. At the same time, it seems to patients that doctors do not want to help them, that they deliberately do not want to save them from their illness.
Features of the disease
The latent form of schizophrenia has a number of characteristic features, which, in turn, significantly complicate the diagnosis of the disease. This happens, first of all, because this form of the disease, as mentioned above, has erased and mildly expressed signs. In addition, with this disease there is an absence of such characteristic features of the disease as delusions, hallucinations and psychomotor disorders.
As for the features of the course of the latent form of the disease, as a rule, there are three main periods of the disease:
- latent;
- period of active development;
- period of disease stabilization.
At the initial stage, the disease develops latently (hidden). At this time, depressive tendencies of various types (with elements of hysteria, hypochondria) begin to dominate in the patient’s thinking and behavior.
During the active period of the disease, attacks of exacerbation of the disease are usually replaced by stabilization phases. Therefore, in most cases, patients with a latent form of schizophrenia do not have problems in society and successfully undergo social and professional adaptation. Now many psychotherapists say that it is quite difficult to recognize the disease and make the correct diagnosis. Often, manifestations of a latent form of schizophrenia are similar to signs of neuroses and psychopathy.
In the modern medical classification of diseases, there is no diagnosis of a latent form of schizophrenia. Therefore, if any form of schizophrenia with mild symptoms is suspected, careful diagnosis and monitoring of the patient’s condition is necessary.
Source: 1popshiatrii.ru
Prognosis and treatment
Neurosis-like schizophrenia has a relatively good prognosis with correctly prescribed and effective treatment. The personality defect does not reach a pronounced state. But the problem may be different; without proper therapy, schizophrenia can develop into another, more complex form, for example, simple or paranoid.
As a rule, such patients avoid society, despite this, adolescents mostly manage to graduate from high school. Such patients work inconsistently, often in easier conditions and under the supervision of relatives. Over the years, the pathology progresses, the symptoms become thicker, and the patient develops schizoid and hysterical features.
According to statistics, about 14% of patients receive the second disability group. A long-term stationary condition with little changing clinical picture in any direction is diagnosed in approximately 23% of patients. Committing life by suicide within five years after the first period of manifestation occurs in 2% of patients. Long-term remission occurs in about 37% of cases.
Treatment for such conditions depends on which of the clinical manifestations of schizophrenia come to the fore. For example, hypochondriacal syndrome is difficult to treat; it is advisable to use various combinations of psychotropic drugs in combination with ganglion-blocking, thymoleptic or psychotonic medications. Antidepressants and antipsychotic drugs are often prescribed. In addition, group and individual sessions with a psychotherapist, support from loved ones and relatives, rehabilitation in sanatoriums and positive emotions are important. When remission is achieved, the clinical manifestations are mild and the patient can be in society without harm to others.
Reading strengthens neural connections:
doctor website
Etiopathogenesis
- Genetic predisposition;
- Biochemical disorders of brain neurotransmitters (dopamine, serotatin, acetylcholine and glutamate);
- The damaging effect of stress on personality;
- The influence of social factors on the formation of the psyche (upbringing).
According to statistics, the prevalence of schizophrenia among males and females is the same; city residents get sick more often, as do the poor. In men, schizophrenia begins early and has a severe course, in women it is the opposite.
Sluggish schizophrenia is characterized by the absence of a clear boundary between the manifest and initial periods. Most often, neurosis-like states, asthenization, depersonalization and derealization come to the fore in the clinical manifestations of sluggish schizophrenia. Patients are characterized by schizophrenic psychopathization. Most often, they are socially adapted and can work in various fields, serve themselves, have families and friendships, and are sociable. However, even a non-specialist can see that the person has a “damaged” psyche.
Synonyms for sluggish schizophrenia are “mild”, “hidden”, “slow”, “rudimentary”, “sanatorium”, “laureled”, “prephase” and others. You can also often find in the specialized literature such terms as “failed”, “occult”, “outpatient”, “non-regressive”.