Magnetic resonance imaging (MRI) is a highly informative radiation diagnostic method that allows you to detect even minimal changes in the tissues of the hypothalamic-pituitary system and pinpoint exactly where they are located. The study does not require any serious preparation for it and, as a rule, is well tolerated by patients.
From our article you will learn who is recommended for MRI of the pituitary gland, in which cases it is not recommended, and also become familiar with the methodology for performing this diagnostic procedure.
Advantages of the method
The pituitary gland is an appendage of the brain that has a rounded shape and is located in a bone pocket - the sella turcica. This is the central organ of the endocrine system; it produces hormones that regulate the functioning of the entire body. Its dimensions are very individual, but in any case we can say that this gland is small (it reaches 5-13 mm in length, 3-5 mm in width, and 6-8 mm in height).
Neoplasms that can arise in the area of the pituitary gland are often characterized by even smaller sizes. However, diagnosing them is extremely important.
Not any diagnostic manipulation will cope with this task, because in order to assess changes in individual parts of the pituitary gland, it is necessary to obtain its images of the highest possible resolution and the smallest possible thickness. Ideally, the cut thickness should be only 2-3 mm.
Some magnetic resonance imaging scanners can provide a high magnetic field voltage, which provides ideal image quality with minimal slice thickness. Other diagnostic methods (radiography, computed tomography) are not able to compete with MRI in this regard.
In addition, MRI provides an image exclusively of the structures of the pituitary gland and the tissues surrounding it, and when conducting some other studies, bone tissue or others are layered on these structures, making it difficult to diagnose the formation - this reduces the information content of the study.
Separately, we would like to note that MRI of the brain and MRI of the pituitary gland are not the same study. Since the latter requires targeted diagnosis of a specific area of the brain, it is not advisable to conduct it as part of another study; the information obtained will be incomplete. If there is a suspicion that the pathological process is localized specifically in the pituitary-hypothalamus region, the necessary diagnostic method in such a situation is only an MRI of the pituitary gland.
Pituitary gland and its functions
The importance of the pituitary gland for the normal functioning of the human body can hardly be overestimated, since it is this small gland that produces hormones - chemical regulators of the most important functions of the body.
The pituitary gland is located in the cavity of the sella turcica at the base of the brain. It consists of anterior and posterior lobes and weighs, as already noted, no more than 1 gram.
The anterior lobe produces tropic hormones that control the production of other chemical regulators and influence metabolism.
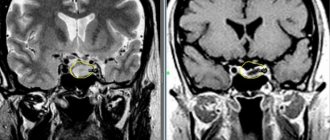
Photo:
The posterior lobe produces hormones that regulate fluid balance in the body and muscle tone.
The pituitary gland influences the growth of the skeleton and soft tissues, human reproductive function, the formation of lactation after childbirth and the breakdown of fats, as well as the synthesis of pigments - skin color, eyes, hair.
Iron has a huge impact on the female and male genital organs, adrenal glands, and thyroid gland, so in the event of the slightest malfunction of the gland located at the base of the brain, a person can develop a number of dangerous diseases.
Timely diagnosis of changes in the pituitary gland allows you to begin the necessary treatment on time, saving a person’s health and even his life.
The most modern and most informative method in diagnosing pituitary diseases, which receives mostly good reviews, is magnetic resonance imaging.
Magnetic resonance imaging of the pituitary gland is often confused with MRI of the brain, but it is worth knowing that these are separate procedures.
READ Diagnostic accuracy of pancreatic MRI
The examination of the gland is carried out separately due to its small size, especially since changes often occur not in the entire gland, but only in one of its parts, and observing these changes during MRI of the brain can be problematic.
Video:
To identify pathologies, the resulting images must have the highest possible resolution, and the slice thickness should not exceed 3 millimeters.
In this regard, the magnetic field voltage in tomographs during magnetic resonance imaging of the pituitary gland is twice as high as the magnetic field voltage during conventional brain tomography. It is 3 Tesla.
Indications
This research technique is indicated for patients who have signs of an endocrine disease, probably associated with a pathological process of a tumor or non-tumor nature in the hypothalamic-pituitary system. It allows you to detect a neoplasm, determine its size (4-5 mm and above), shape, structure, as well as relationships with tissues and anatomical formations located nearby.
So, the indications for MRI of the pituitary gland are:
- headaches of unknown origin;
- disorders of visual function, oculomotor disorders of unknown nature;
- metabolic disorders in the body (including fluctuations in body weight for no apparent reason);
- in women - menstrual dysfunction;
- in men – erectile dysfunction;
- signs of Cushing's syndrome, acromegaly or other hormonal disorders;
- laboratory detection of changes in the concentration of pituitary hormones in the blood (thyrotropin, prolactin, somatotropin and others).
Brain MRI with contrast
A magnetic resonance imaging (MRI) examination of the brain with contrast is a way to learn about anomalies and malformations of the brain, inflammatory processes, oncological tumors, and traumatic injuries.
Indications for MRI of the brain with contrast:
- probable presence of a tumor;
- frequent and incomprehensible fainting;
- trembling, numbness and/or weakness of the arms and legs;
- significant speech impairment;
- dizziness with frequent intensity;
- unpleasant noise in the ears;
- obvious signs of a stroke;
- rapid memory deterioration;
- organic visual impairment;
- decreased intelligence;
- various injuries;
- vascular pathologies;
- epilepsy, etc.
MRI is the best way to diagnose the brain and its brain structures, in particular the pituitary gland. Using MRI of the pituitary gland with contrast, many targeted images, so-called slices, are obtained. The study is carried out using a modern device with high accuracy - this ensures high-quality images of the pituitary gland.
Contraindications
They are usually divided into absolute (if they are present, MRI is categorically contraindicated) and relative (MRI in such conditions is associated with the development of difficulties and complications; the doctor, using an individual approach, determines whether such a patient should undergo the study or not).
Absolute contraindications 2:
- the patient has a pacemaker (artificial pacemaker) - the magnetic field during the study can cause malfunctions of this device, which is life-threatening;
- metal implants, fragments and any other metal objects in the patient’s body (cochlear implants, certain types of clips and stents on blood vessels, artificial heart valves, joint replacements, surgical staples, plates, screws or pins, and so on).
Metal teeth are not always a contraindication for examination.
Relative contraindications are as follows:
- the first 2 trimesters of pregnancy (there is no data indicating a negative effect of MRI on the fetus - this study has been used for more than 30 years, including in pregnant women, no side effects have been detected during this time; however, it is not reliably known how the magnetic field may affect the fetus, therefore, in this category of patients, MRI is performed only for strict indications, when the absence of a mother’s diagnosis may be more dangerous than the negative impact of the magnetic field on the growing fetus);
- claustrophobia (fear of closed spaces); patients suffering from this pathology are recommended to take sedatives before the study or, if possible, undergo diagnostics using an open-type device;
- epilepsy;
- extremely serious condition of the patient;
- the patient’s inability to remain still during the examination (in order to achieve immobility, he may be given anesthesia);
- allergy to contrast agent (if MRI with contrast is necessary);
- severe renal failure - again, this applies to MRI with contrast.
With or without contrast?
The patient may be prescribed a simple MRI of the pituitary gland or a study using contrast. Paramagnetic contrast agents are used. They are administered intravenously immediately before the study. The dose is calculated individually depending on the patient’s body weight.
Iodine-containing contrast agents are not used for MRI. If the patient suffers from chronic kidney disease, he will need to undergo a series of tests before the study (to determine how quickly the kidneys remove the contrast from the body).
What type of MRI – with or without contrast – is needed for a particular patient is determined by the doctor himself. More often, MRI with contrast enhancement is used, since this study allows one to reliably determine the contours of a large formation, its structure, and the nature of its relationship with tissues located nearby. By contrast, it will be possible to more clearly verify the presence of microadenoma.
Indications for MRI
A magnetic resonance imaging method for examining the sella turcica using a contrast agent is prescribed by an endocrinologist if there is a suspicion of a pituitary gland adenoma or a hormonal imbalance; it allows one to determine the size of tumors and its boundaries.
The main reasons for contrast MRI:
- a detailed examination of the structure of the tumor to determine the nature of the formation - a malignant or benign tumor;
- differential study of changes in neoplasms;
- identification of affected areas of the pituitary gland;
- checking for the presence of metastases after tumor removal;
- increased synthesis of individual hormones and glands (corticoids, thyrotropin, somatotropin, prolactin, etc.);
- regular causeless headaches;
- seizures;
- brain pathologies;
- post-infarction and post-stroke conditions;
- impairment of vision, memory and orientation;
- violation of sexual functions - the menstrual cycle in women and deterioration of erectile functions in men;
- rapid weight change;
- growth anomalies - dwarfism or gigantism.
At the same time, the doctor receives complete information about the structure of organs and their changes, which is especially important in cases where there is a threat to the patient’s life. The main reason for prescribing contrast MRI of the hypothalamus is a malignant tumor of the gland.
Research methodology
MRI provides the doctor with information about the condition of the pituitary gland and surrounding tissues.
No special preparation is required for an MRI of the pituitary gland. The only thing is that in the case of a planned contrast study, the patient is recommended not to eat 5-6 hours before it, that is, the procedure should be carried out on an empty stomach, and ideally on an empty stomach. This is necessary in order to minimize side effects in the form of nausea and vomiting, and if complications suddenly arise, the doctor will not need to flush the patient’s stomach before other emergency procedures.
Also, before the procedure begins, the required dose of contrast agent or drugs with a sedative effect are injected into the vein of the subject.
Before entering the office, the patient must remove all metal objects (jewelry, including piercings, clothing with buttons, etc.). Since the object of study (pituitary gland) is located in the skull area, it is not necessary to remove clothing without metal elements.
During the scan, the patient is in a supine position. To ensure maximum immobility, his head is fixed with a special mount - this will allow you to get a clear, high-quality image of the sections. Next, the table with the patient slides into the tomograph until its frame is at the level of the study area.
While the tomograph is operating, the subject is alone in the room. The operator controls the process from the next room, sitting at the monitor, and can communicate with the patient via speakerphone. If a child undergoes an MRI, as a rule, one of his relatives is with him in the room (they, like the patient, leave all metal objects in front of the entrance to the room with the tomograph).
The study lasts on average from 30 to 60 minutes. This depends on the number of slices required, the model of the machine, and whether contrast enhancement is used or not.
What's next?
The computer, using a previously installed special program, processes the signals received from the tomograph and generates a certain number of images from them (according to the number of slices). They can have different thicknesses and be obtained from different angles (the nature of the sections is controlled by the radiologist during the MRI). When the images are generated, the doctor evaluates the pathological changes in them directly from the monitor, and also prints the photos and/or writes them to disk, and then transfers them to the patient or his attending physician.
A rest period after an MRI is not required - the person can immediately engage in daily activities, drive a car and eat what they consider necessary.
Lactating women are not recommended to breastfeed for 24-48 hours after administration of a contrast agent.
The patient's feelings during the examination
Magnetic resonance imaging of the pituitary gland without contrast, as a rule, is not accompanied by any unpleasant sensations for the patient. We have already talked separately about people with claustrophobia - for them, a procedure in a closed apparatus can provoke a panic attack.
MRI with contrast enhancement in some patients causes a feeling of discomfort in the body and the appearance of a metallic taste in the mouth after intravenous injection. Also, in some cases, they react to the contrast with nausea, vomiting or an allergic reaction in the form of itching of the skin, rashes on it (hives), and so on. As a rule, such conditions either go away on their own or are eliminated by administering special medications.
MRI of the pituitary gland: norm and pathology
Normally, on a section made in the frontal plane (as if the device was “looking” straight into the patient’s face), the shape of the pituitary gland resembles a rectangle. Its lower contour has the shape of a sella turcica, and the upper contour is concave, horizontal or convex. The anterior-posterior and right-left dimensions of the organ correspond to those of the sella turcica itself, and the vertical dimension varies within 4-8 cm and changes with diseases. In adolescents, the vertical size can exceed the above values - increase to 9-10 mm, and in women at the end of pregnancy and in the postpartum period - increase to 10-12 mm.
In the frontal section, the pituitary gland is mostly symmetrical (mild asymmetry is more of a normal variant than a sign of pathology). The funnel of the organ is located in the midline, however, experts also regard a slight deviation from it in the absence of structural changes in the pituitary gland and other pathological changes in the area of the gland as normal.
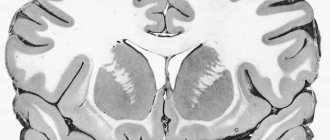
Empty sella syndrome on MRI
With this pathology, MRI images show a thinned pituitary gland spread across the bottom of the sella turcica. At the same time, the optic chiasm cistern sags (scientifically, prolapses) into the cavity of this bone formation. On tomograms performed in the anteroposterior direction, the gland resembles a sickle shape, the thickness of which does not exceed 2-3 mm.
Tumors of the sella turcica and optic chiasm on MRI images
In the area of the pituitary gland, neoplasms varying in size are detected:
- up to 10 mm in diameter – microadenoma;
- 10-30 mm in diameter – macroadenoma; a tumor less than 10 cm can also bear this name, but only if it spreads beyond the sella;
- mesoadenoma is a type of macroadenoma measuring 10-22 mm, located in the area of the sella turcica, without extending beyond it;
- over 30 mm – giant adenoma.
In addition to adenoma, meningioma, craniopharyngioma, germinoma and some other types of tumors, characterized by a number of signs on the tomogram, can be diagnosed in the chiasmal-sellar region.
A neoplasm of the pituitary gland can be localized in the sella turcica, grow into the cavernous sinuses, ventricles of the brain, sinus of the sphenoid bone, pons cistern, and nasal passages. All this will, of course, be noticeable on MRI images.
Indirect signs of a pituitary tumor are:
- heterogeneity of the structure of the gland in any one place (that is, not diffuse, but focal);
- its asymmetry;
- displacement of the funnel from the midline;
- deformation of the bottom of the sella turcica.
It is impossible to make a diagnosis based on these data alone; they must be considered in conjunction with the clinical picture and the results of the examination carried out over time.
MRI in a patient with diabetes insipidus
As is known, the cause of this pathology is a deficiency of the hormone vasopressin, which is normally produced by the cells of the hypothalamus, from there it enters the pituitary gland, and from there into the blood. Hormone deficiency can be caused by an inflammatory process in the hypothalamic-pituitary system or its tumor. Signs of both pathologies will be visible on the tomogram.
In idiopathic diabetes insipidus (the nature of which is unclear), MRI will reveal that there is no hyperintense signal from the neurohypophysis (the posterior lobe of this gland) on T1-weighted images.
GH deficiency on MRI
In case of growth hormone deficiency, 1 or more of the following signs will be detected on the tomogram:
- a characteristic triad - ectopia (location of cells in an atypical location) of the neurohypophysis, hypoplasia (underdevelopment) of the adenohypophysis (that is, its anterior lobe), hypoplasia or aplasia (congenital absence) of the pituitary stalk (the sign occurs in 40% of cases of pathology);
- hypoplasia of the pituitary gland (diagnosed in almost a third of patients);
- signs of empty sella syndrome (described above; found in every fifth patient).
In 10% of patients, there are no pathological changes in the pituitary gland area at all.
What does an MRI of the pituitary gland show?
As a result of the study, the doctor can diagnose changes in the structure and size of the pituitary gland and determine the cause of the following diseases:
- infertility;
- diabetes insipidus;
- acromegaly or gigantism;
- tumor process;
- thyrotoxicosis;
- metabolic disorders, etc.;
MRI also reveals the type of tumor, if present. An adenoma is often diagnosed - a benign tumor, which, although small in size, responds well to drug treatment. A large adenoma must be surgically removed. A malignant tumor of the pituitary gland is very rarely diagnosed.