| Pituitary adenoma | |
| The arrow points to the normal area of the pituitary gland “neurohypophysis” - it is a mistake to mistake this area for pathology | |
| ICD-10 | 35.235.2 |
| ICD-10-CM | D35.2 |
| ICD-9 | 237.0237.0 |
| ICD-O | 8140/0 |
| OMIM | MTHU016150 |
| MedlinePlus | 000704 |
| eMedicine | neuro/312 |
| MeSH | D010911 |
| Media files on Wikimedia Commons | |
Pituitary adenomas
are tumors of the glandular tissue of the pituitary gland (develop from the anterior lobe - adenohypophysis)[1].
Etiology[ | ]
In most cases, the cause remains unknown. Certain importance is given to the consequences of traumatic brain injury, neuroinfection, intoxication, pathology of pregnancy and childbirth, and the use of oral contraceptives [1].
Pituitary adenoma occupies a leading position among all tumor diseases of the gland. Pituitary adenoma most often appears in adults, but sometimes occurs in children, although much less frequently. The peak incidence occurs in people between 30 and 50 years of age. Men and women get sick with the same frequency. Pituitary adenomas account for one sixth of all brain tumors. Very often the tumor is asymptomatic, so the detection rate per 100 thousand people is only 2 people. This is why surgery to remove adenoma
, since medications are no longer effective.[2]
Prognosis for patients
After removal of the cyst, it is possible to achieve normalization of prolactin levels in almost all patients. More than half experience gradual disappearance of headaches and restoration of vision. The formation of pituitary hormones returns to normal in only a third of patients; the rest require replacement therapy.
The risk of relapse remains for six months to 20 years. Most often, re-formation of the cyst occurs within 5 years from the date of removal. Therefore, all this time the patient should be observed by an endocrinologist, neurosurgeon and ophthalmologist.
And here is more information about headaches with an affected pituitary gland.
A pituitary cyst appears during fetal development or under the influence of injuries, infections, or vascular pathologies. Depending on the size, small and large formations are distinguished. By origin they are arachnoid, colloid and embryonic (Rathke's pouch).
Symptoms of hormonal disorders, decreased vision and increased intracranial pressure are characteristic of large cysts, so they need to be removed. Transsphenoidal endoscopic operations or open access are prescribed.
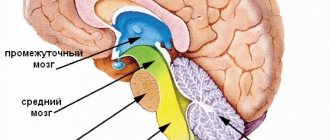
Pathogenesis[ | ]
The process of neoplasm development goes through several stages. At each stage, certain pathogenetic mechanisms are sequentially activated. For example, genetic, autocrine, hormonal, paracrine. Hypothalamic hormones and growth factors play a major role in pathogenesis.
There is an interesting theory of the secondary occurrence of adenoma. First, the hypothalamus is affected, and then the pituitary gland becomes dysfunctional. When exposed to releasing hormones of the hypothalamus, increased stimulation of the pituitary gland occurs, which leads to excessive growth of glandular cells, which must produce an increased amount of hormones. There is also primary damage to the pituitary gland with the formation of an adenoma.[2]
Adenomas develop from a previous focus of hyperplasia[1].
| This section of the article has not been written. According to the plan of one or more Wikipedia contributors, a special section should be located in this place. You can help by writing this section. This mark was set on December 31, 2020 . |
Operation
Surgery is recommended only when the cyst grows and needs to be removed. This method is the best among the others, since after the operation, patients immediately recover. The following improvements are noted:
- Headaches are reduced and disappear completely over time.
- Vision is restored.
- Immune mechanisms become more stable.
- The function of the reproductive and genitourinary systems is normalized.
Classification[ | ]
The international classification of tumors of the central nervous system (WHO, 1979) maintains the division of pituitary adenomas based on their histological features [1]:
- chromophobic
- acidophilic (eosinophilic),
- basophilic,
- mixed acidobasophilic and
- adenocarcinoma.
As data accumulated on the inconsistency of clinical and morphological parallels (acidophilic - acromegaly, basophilic - hypercortisolism, chromophobic - without hormonal activity), new classifications arose. For example, according to the classification of S. Yu. Kasumova et al. (1982), there are hormonally active, hormonally inactive and malignant pituitary adenomas [1]:
Hormonally active tumors include:
- GH-secreting (somatotropinoma),
- prolactin-secreting (prolactinoma),
- ACTH-secreting (corticotropinoma),
- TSH-secreting (thyrotropinoma),
- FSH/-secreting (gonadotropinoma).
If a tumor secretes two or more hormones, it is called a mixed adenoma.
Hormonally inactive include:
- chromophobe pituitary adenoma and
- oncocytoma.
Malignant adenomas are extremely rare and are characterized by rapidly increasing symptoms of hypopituitarism, visual and neurological disorders[1].
The division of adenomas proceeded in this way. There were acidophilic ones, which were accompanied by increased production of somatotropic hormone (GH). There were also basophilic, producing ACTH, chromophobic, not disrupting hormone synthesis, and mixed. However, this classification did not meet modern requirements and had many blind spots. Therefore, in 1995, E.? Horvath and K.? Kovacs proposed a classification taking into account the frequency of occurrence of pituitary adenomas of various types. Thus, adenomas began to be divided into somatotrophic, corticotrophic, thyrotrophic, mammosomatotrophic, silent, plurihormonal, etc.
Therefore, a pituitary adenoma is a benign tumor of the pituitary gland, which grows from the cells of the anterior and middle lobes of the gland. This neoplasm is localized in the area of the sella turcica, which is in the sphenoid bone at the base of the skull.
Pituitary adenoma is not one disease. This term includes a large number of pathologies that differ in location and clinical manifestations. Like other tumors, adenomas differ in their growth method, size, histological characteristics, activity, and secreted hormones. The classification of pituitary adenomas in its modern version is based on the relationship between the concentration of hormones in the blood and the clinical picture. According to another classification, pituitary adenomas are divided into hormonally active and hormonally inactive. Those adenomas that do not manifest themselves clinically are called hormonally inactive.
Adenomas are also classified according to the direction of growth. Height is determined in relation to the sella turcica. In the early stages, endosellar ones arise, that is, those that grow in the cavity of the sella. As the tumor grows, it spreads lower, reaching the sphenoid sinus, which transforms the tumor into an infrasellar neoplasm. As it grows upward, a suprasellar tumor is formed, posteriorly – retrosellar, to the sides – lateral, anteriorly – antesellar. If a tumor grows in several directions, its name is formed from the names of those directions in which its growth is observed. Microadenomas and macroadenomas are distinguished by size.
| This section of the article has not been written. According to the plan of one or more Wikipedia contributors, a special section should be located in this place. You can help by writing this section. This mark was set on December 31, 2020 . |
Causes
Why a cyst appears in the pituitary gland is currently unknown. Nevertheless, there are factors that increase the likelihood of the occurrence and growth of a neoplasm. Among them:
- Hereditary conditioning;
- Diseases of an infectious nature, for example, meningitis;
- Injuries causing damage to the bones of the skull and brain;
- Diseases of the mother that have a negative impact on the development of the fetus during pregnancy, including infectious, sexually transmitted diseases;
- Maternal virus carriage;
- Injuries during childbirth;
- Increased radiation.
However, in some situations even these factors remain undisclosed, and what led to the development of the disease is unknown.
Diagnostics[ | ]
Magnetic resonance imaging[ | ]
MRI is the mainstay of imaging of pituitary adenomas. MRI with CT has a sensitivity of up to 90%. Post-contrast images and especially images after dynamic coronary angiography are an integral part of the MR examination protocol for the pituitary gland and significantly increase diagnostic accuracy. However, sometimes morphological changes can be visible in non-contrast images. These include changes in the gland from the side of the adenoma, thinning and remodeling of the lower wall of the sella turcica, as well as deviation of the pituitary infundibulum from the adenoma [3].
- on T1, adenomas are usually isointense to the pituitary gland;
- T1-KU: on dynamic sequences - a rounded area of reduced enhancement compared to the rest of the gland;
- On delayed images, the pattern ranges from hypoenhancement (the most common pattern) to isointensity compared with the rest of the gland to hyperintensity.
- T2 – the picture is different, but in general – slight hyperintensity.
It is very important to remember the following fact when performing an MR examination of the pituitary gland: small incidentalomas of the pituitary gland are quite common, and in approximately 2-30% of cases, small asymptomatic microadenomas are detected at autopsy.
Diagnostics
Magnetic resonance imaging
Quite often, a pituitary cyst is discovered by chance during an examination of brain structures. This is due to the fact that at the initial stage of its formation there are no symptoms.
If signs characteristic of the growth of a pituitary cyst appear, the patient is prescribed the following tests:
- X-ray – allows you to visualize the location and size of large cysts. At the initial stages of tumor formation, the study is ineffective.
- MRI and CT - helps to determine the size, shape, etiology and location of cysts of any size. For maximum reliability, the procedure is carried out with contrast.
If a pituitary cyst is detected, the patient is referred to an endocrinologist for consultation and further examination. The degree of damage to pituitary tissue and disturbances in its functioning is determined by hormonal levels. To do this, the patient's blood is taken for the following indicators:
- cortisol;
- testosterone;
- TSH (thyroid stimulating hormone);
- T3 – T4 (thyroid hormones);
- estrogen;
- STH (somatotropic hormone);
- prolactin;
- FSH (follicle stimulating hormone);
- ACTH (adrenocorticotropic hormone);
- thyroglobulin.
To assess the functioning of the endocrine system, an ultrasound scan of the thyroid gland may also be prescribed. After receiving all the examination results, the doctor makes a conclusion about the etiology of the pituitary cyst and the disorders in the body’s vital systems that it provokes.
Treatment of pituitary adenoma[ | ]
To treat adenoma, various techniques are used, the choice of which depends on the size of the tumor and the nature of hormonal activity. Today the following approaches are used:
- Observation. For pituitary tumors that are small and hormonally inactive, doctors choose a wait-and-see approach. If the formation increases, then appropriate treatment is prescribed. If the adenoma does not affect the patient’s condition, then observation continues.
- Drug therapy. Indicated for persons with prolactinoma or somatropinoma. Drugs are prescribed that block the excess production of hormones, as a result of which hormonal levels are normalized and the patient’s physical and psychological condition is restored.
- Radiosurgical treatment. This is a modern and highly effective method of radiation therapy, based on the destruction of the tumor by radiation, without surgical manipulation.
- Operation. Surgical removal of a pituitary adenoma is the most effective, but at the same time traumatic method of therapy. Specialists have two access options: through the nasal passages and by opening the cranial cavity. The first approach is more preferable, but is used only for small adenomas.
Often, for the treatment of pituitary adenoma, it is necessary to combine several of these techniques to achieve the desired result.
Symptoms of a pituitary cyst
The first symptoms of pathology:
- frequent headaches, which can be permanent and do not change during the process of changing the position of the body in space (standing, lying down);
- limited mobility of the eyeballs, pain and double vision;
- diabetes insipidus;
- sexual dysfunction;
- problems with the urinary system;
- frequent mood changes;
- lowering blood pressure;
- disruptions of menstrual cycles. Uterine bleeding is observed that is not related to the woman’s cycles;
- a pituitary cyst can affect the hormonal balance in the body, which can cause fibrocystic mastopathy in girls;
- general malaise;
- neurotic disorders;
- dizziness;
- periodic seizures;
- persistent runny nose;
- periodic convulsions.
Notes[ | ]
- ↑ 123456
Handbook of Clinical Endocrinology / Ed. Kholodova E. A. - 1st ed. - Minsk: “Belarus”, 1998. - P. 42-48. — 510 s. — 10,000 copies. — ISBN 985-01-0031-1. - ↑ 12
Pituitary adenoma: its prevention and treatment | Doctor's advice (Russian) (October 5, 2013). Retrieved July 28, 2020. - Neuroimaging.
Pituitary microadenoma
(undefined)
.
Radiography
(2018).
Prevention of consequences
The vast majority of complications that occur in the brain area are caused by an increase in tumor size, as well as compression of neighboring lobes and glands. Similar consequences for pituitary cysts include:
- hydrocephalus;
- increase or surges in pressure inside the skull;
- loss of vision;
- effusions of blood into tumor tissues;
- cystic type changes (so-called cystic adenoma).
Considering the severity of the possible consequences, competent prevention is necessary. This will help keep all brain functions in excellent condition. So, in order to avoid complications with a pituitary cyst, as well as the disease described itself, it is necessary to monitor hormonal levels and avoid mechanical and accidental injuries to the skull.
Those who are at risk should undergo brain examinations once a year. Moderate physical activity, a low-carbohydrate diet, and giving up bad habits are also recommended. Thus, a cyst formed in the pituitary gland is a serious pathology, which, if it does not reach a large size, does not cause concern. With an increase in size, very serious consequences are possible, requiring qualified and long-term treatment.