Disorders of work, functional activity, anatomical changes in cerebral structures are represented by a wide list of deviations that can be deadly.
This is often how it turns out: without proper medical care, the patient risks dying or suffering irreversible changes in the nervous tissues and becoming deeply disabled. This cannot be allowed, we need to act faster.
Brain edema is an acute condition in which the amount of intra- and intercellular fluid in the structures of nerve fibers increases. It occurs against the background of many diseases and conditions of a neurological, traumatic nature, and damage to the cardiovascular system.
The clinical picture is specific, therefore it is quite difficult to confuse the pathological process. Time is running out. Treatment takes place in a neurological hospital, intensive care unit. Depends on the patient’s condition, the current state of affairs.
The forecasts are vague. If you can help in the first few hours, there is a high chance of total recovery without critical complications and consequences.
Development mechanism
There are several pathogenetic pathways for the formation of the disorder. As a rule, they do not intersect with each other; they exist and arise in isolation.
What exactly are we talking about:
- Acute inflammatory processes. May be infectious, such as meningitis or encephalitis. Autoimmune variants of the disorder are slightly less common. They give about the same complications.
We are talking about an increase in fluid concentration as a result of stagnation of cerebrospinal fluid, which also leads to a rapid increase in intracranial pressure.
Attention:
If the inflammatory process is not eliminated in a short time, the likelihood of developing a complication, cerebral edema (CED), increases every hour.
- Oncology. Malignant tumors most often. Mainly glial astrocytomas. Oddly enough, this also includes benign neoplasms. Provided that they are large enough to compress the drainage pathways of cerebral structures.
The likelihood is debatable. It is impossible to predict in advance what the risk of developing this pathological process is. But it’s better to play it safe and start treatment quickly.
- Hydrocephalus. Increased amount of fluid in the skull. It develops as an independent pathological process or as a result of the influence of an external factor. For example, inflammation, trauma or tumor development.
Congenital forms of the disorder cannot be eliminated radically. It is necessary to combat the symptoms and normalize the functioning of the drainage system. For these purposes, diuretics are used.
- Suffered damage. The traumatic mechanism is considered one of the main ones. A very common factor in the development of the pathological process.
Post-traumatic cerebral edema can occur suddenly, some time after a skull injury. Therefore, it is strongly recommended to treat TBI in a neurological hospital. There you can get sufficient supervision and the necessary care.
- Stroke. Acute disturbance of cerebral blood flow. Especially when it comes to the hemorrhagic form. When a blood clot forms, it shrinks, thickens and compresses the tissue. Including a drainage system that distributes cerebrospinal fluid. Dangerous and unpredictable consequences are possible in the form of necrosis of most of the cerebral structures, wedging of the trunk into the foramen magnum and the death of the patient.
These are the main mechanisms for the development of the pathological process.
Children are worth mentioning separately. Newborns experience cerebral edema during severe pregnancy in the mother. It is necessary to observe for some time after birth. At least a week.
Traumatic cerebral edema
Traumatic cerebral edema (TCE) is an increased water content in the brain tissue after TBI. Experimental studies have established the presence of two forms of traumatic cerebral edema:
- vasogenic (VO)
- cytotoxic.
There is also a relatively rare form of traumatic cerebral edema - ischemic, characterized by a two-phase manifestation (first cytotoxic, then vasogenic traumatic cerebral edema).
In case of brain injury, ischemic OMT (similar to the model of ischemic edema with clipping of the main artery in the experiment) can occur with thromboembolism of the trunks of the main arteries, with dislocation entrapment of the posterior cerebral artery in the foramen of the cerebellar tentorium, and in some other cases noted below. Vasogenic and cytotoxic OMT often accompany each other with dominance of one of them.
OMT occurs as a result of increased vascular permeability of the BBB and is accompanied by the release of plasma and its components into the intercellular space.
VO, according to CT data, is formed within the first day. after TBI as a reaction to the impact of mechanical energy on the brain matter, especially during its destruction.
It represents a zone of reduced density on CT (18-25 N), often perifocal, and a corresponding signal of increased activity in the T-2 mode (SE - 2000-2500/150 m/sec) on MRI in the acute period. Foci of type 1 contusion according to their CT characteristics correspond to local VO; pathomorphologically small pinpoint hemorrhages caused by damage to the BBB are also detected.
With the spread of perifocal VO, especially in cases of multiple contusional lesions, zones of reduced density can dynamically merge, turning into a lobar or hemispheric OMT.
Bihemispheric generalization of VO is rarely observed. A diffuse decrease in brain density that is quickly detected, according to CT data, in patients with episodes of hypoxia is referred to as ischemic (anoxic) OMT.
This issue remains poorly understood and needs further development.
With a sufficiently pronounced mass effect, the VO communicates with the ventricles of the brain in the form of a hypodense track on CT, similar in density to perifocal edema on CT or a signal of increased activity on MRI.
It indicates the drainage (clearance) of edematous fluid and breakdown products of the traumatic substrate in the early stages of TBI into the ventricular system. A few weeks later.
o and the disappearance of the sanogenic track on CT-MRI, which indicates the final cessation of the first phase of VO, when the pressure gradient of the resulting edematous fluid is directed from the vessel into the brain tissue and further into the liquor system, and the “switching on” of its second phase, where the pressure gradient changes diametrically and is directed from the site of brain damage to the capillaries (reabsorption). However, it should be remembered that detection after several months. after TBI on CT-MRI, signs of communication between the location of the former intracerebral substrate and the ventricular system and/or convexital surface should be considered as a cystic-atrophic process, including porencephaly. The latter often occurs due to long-term resolution of VO in the area of a large traumatic substrate and craniotomy. In some cases, this happens without surgical intervention. The peak of disruption of the BBB permeability (according to the permeability coefficient for albumin) occurs on the 1st-2nd day. after injury, and according to CT - on the 5-8th day. The addition of meningoencephalitis causes a significant increase in this coefficient and, consequently, the degree of damage to the BBB. With small foci of contusion or intracerebral hematomas of a cortical-subcortical location, resolution of VO occurs through the subarachnoid space and through reabsorption.
There is no clinical picture pathognomonic for traumatic vasogenic edema. This applies primarily to patients who have been in a coma since the injury.
However, with minor disturbances of consciousness (stunning of varying degrees), the symptoms of progressive VO can consist of an increase in disturbance of consciousness, increased headache, the appearance of vomiting, psychomotor agitation, bradycardia, and the development of congestive optic nerves.
At the same time, in response to dehydration therapy, a wave-like changing level of consciousness is often noted in the first day. after injury.
With epidural and subdural hematomas, the density of the brain tissue of the underlying hemisphere on CT decreases slightly. Before evacuation of the hematoma, ischemic disorders predominate in the adjacent hemisphere due to mechanical compression of the brain.
The role of VO, if there are no concomitant foci of contusion and/or intracerebral hematomas, is insignificant. At the same time, after removal of extracerebral hematomas, on the evacuation side, according to radionuclide studies, a significant increase in volumetric cerebral blood flow can be detected, leading to its interhemispheric asymmetry.
At the same time, the relationship between VO and swelling (hyperemia) of the brain remains unclear.
Cytotoxic cerebral edema is characterized by edema (swelling) of the cellular elements of the brain parenchyma, caused by the effects of hypoxia and certain chemicals.
The main mechanism of this type of edema is a violation of osmoregulation of brain cells, depending on the functioning of the sodium-potassium “pump”. All data presented were obtained experimentally.
There are no reliable methods for diagnosing cytotoxic OMT in the clinic.
Treatment of VO cannot be considered without regard to the size and number of foci of brain contusion and/or intracerebral hematomas, treatment tactics (surgical removal of the substrate or conservative management), age of patients, initial level of consciousness and other components of the clinical picture.
In recent years, glucocorticoid therapy has been shown to be of little effectiveness in severe TBI, so it can be recommended only when life-threatening complications occur - traumatic, hemorrhagic shock combined with TBI, or arterial hypotension and hypoxemia in isolated TBI requiring emergency resuscitation. Considering the dependence of the body when a different hormonal balance is imposed on it, it is advisable, after achieving the necessary clinical effect, to continue glucocorticoid therapy with a tendency to reduce it and stop it within 4-6 days.
Due to the circulation in the blood and especially in the CSF of a large number of toxic breakdown products of brain tissue and their metabolites, the use of detoxification therapy (hemodesis, native plasma) is mandatory, based on the specific treatment situation. The most justified dehydration therapy is the use of saluretics (Lasix, furosemide).
Their use is indicated in the acute period of TBI to achieve the required clinical effect—elimination of CT signs of mass effect and neurological dislocation symptoms, reduction of ICP, as well as for the purpose of relieving concomitant renal failure and pulmonary edema.
Doses of saluretics depend on the immediate objectives of treating the patient and usually vary from 20 to 60 mg for a single dose (intravenously or intramuscularly). If saluretics are ineffective and in cases where a rapid reduction in ICP is required, the use of osmotic diuretics is indicated.
Mannitol is used at a rate of 0.5-1.0 g per kg of patient body weight in the form of a jet infusion. The upper limit of blood pressure should not be lower than 100 mm Hg. Art. Having a powerful dehydration effect, osmotic diuretics allow you to gain time, in particular with dislocation syndrome.
However, one should remember about their short-term effect in reducing ICP, dehydration along with edematous intact tissues and the possible phenomenon of “recoil” after 4-6 hours. after administration, the need to correct water-electrolyte balance. In patients in terminal coma, when there is a complete loss of autoregulation of cerebral blood flow, the use of osmotic diuretics is contraindicated.
A necessary condition for treatment is the use, starting from the first days of injury, of nootropic drugs that also indirectly act as activators of the body's antioxidant system, as well as improving metabolic processes in the brain (Cerebrolysin, etc.).
The use of drugs that improve microcirculation in the vascular bed (reopolyglucin, trental) is indicated. The latter is used if there is no risk of bleeding.
Starting from the first hours and during the first day after severe TBI, anti-enzyme drugs are included in the treatment complex.
Taking into account the indications and contraindications in each observation, the resolution of VO can be facilitated by the application of external ventricular drainage, because
a decrease in ICP, even for a short period of time, increases the clearance of edematous fluid and decay products of brain tissue through the ventricular system.
Source: https://dreamsmedic.com/spravochniki/nejrotravmatologiya/terminyi-na-o/otyok-mozga-travmaticheskij.html
Classification
Cerebral edema is divided into vasogenic, interstitial and cytotoxic. They have slightly different formation mechanisms and require a separate approach to therapy.
Vasogenic
The essence of the disorder is the penetration of positively charged ions into the brain tissue. Normally, they cannot enter the cerebral structures. The blood-brain barrier interferes.
As a result of inflammatory processes, tumors and other conditions, the degree of protection decreases. Charged particles lead to an increase in osmotic pressure. Accordingly, the fluid leaves the cells into the intercellular space.
The next noticeable step is compression of the tissues of cerebral structures and the development of cerebral tissue edema itself. The clock is counting. In some cases - for days. If you are lucky, you will be able to react and help the patient.
Cytotoxic
Simply put, the concentration of fluid in this case increases inside the nerve cells themselves. They are mostly composed of water. Immediately the volumes grow even more.
Cytological units lose the ability to respond normally to stimuli and work as usual. Swelling develops relatively slowly over several days. There is time to help the patient.
Interstitial
Develops against the background of hydrocephalus. Stagnation of intracranial fluid, cerebrospinal fluid, leads to compression of the brain and spinal cord itself, and then to focal disorders that are dangerous to health and life.
Each option requires its own, special approach to therapy.
Intracranial trauma
Intracranial injury is a fairly broad spectrum of brain injury with different causes and injuries. Let's look at the most common diagnoses.
Brain concussion
Functionally reversible brain damage with short-term loss of consciousness caused by TBI. Pathomorphological changes can be detected only at the cellular and subcellular levels.
Clinical picture
- Brief loss of consciousness following injury
- After regaining consciousness: headache, dizziness, nausea, often vomiting, tinnitus, sweating
- Vital functions are not impaired
- There are no focal neurological symptoms
- Retrograde amnesia
- The general condition usually improves during the first, less often the second week after the injury.
Diagnostics
- There are no injuries to the skull bones
- CSF pressure and its composition unchanged
- CT and MRI without pathological signs.
It should be differentiated from the period of light interval with the development of brain compression.
Treatment
- Hospitalization is required; continuous monitoring for at least 24 hours after injury in order to timely diagnose cerebral compression
- Symptomatic therapy (non-narcotic analgesics for pain, antibacterial agents for soft tissue wounds).
Traumatic cerebral edema
Brain edema - manifests itself as increased accumulation of fluid (water, lymph) in the tissues of the brain and its blood vessels.
Cerebral edema is a serious condition because as a result of an increase in brain volume, an increase in intracranial pressure occurs, which can cause various complications in the body.
The term “increased intracranial pressure” is also used to describe this condition, as well as “cerebral edema”. Its essence lies in the fact that pressure increases inside the skull, in response to this, cerebral circulation is disrupted, and this, in turn, leads to the death of brain cells
In some cases, this condition can lead to coma and even death. For example, cerebral edema is one of the immediate causes of death with systematic alcohol abuse.
Causes of cerebral edema
Trauma, illness, infection, and even changes in altitude - any of these reasons can lead to brain swelling. Ischemic stroke is the most common type of cerebrovascular accident resulting from the formation of a blood clot. In this case, brain cells, not receiving the proper amount of oxygen, begin to die, and edema develops.
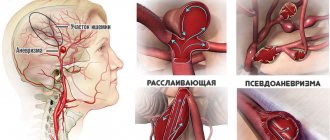
Hemorrhagic stroke is the result of damage to the blood vessels of the brain. The resulting intracerebral hemorrhage leads to increased intracranial pressure. Most often, hemorrhagic stroke develops due to high blood pressure, other causes include head trauma, certain medications, and congenital malformations.
Infectious diseases: meningitis, encephalitis, toxoplasmosis, subdural abscess, tumor, drop.
Symptoms of cerebral edema
Symptoms of cerebral edema vary depending on the cause and severity of the condition. Typically, signs of the disease develop suddenly: headache, pain or numbness in the neck, nausea, vomiting, dizziness, uneven breathing, visual disturbances, amnesia, impaired balance and gait (ataxia), difficulty speaking, decreased level of consciousness (stupor), convulsions, loss of consciousness.
Treatment of cerebral edema
Surgical and drug treatments are aimed at supplying the brain with oxygen. As a result, the swelling goes away. As a rule, timely therapy contributes to an earlier and complete recovery and consists of the following: oxygen therapy, intravenous infusion, lowering body temperature.
In some cases, medications are prescribed for cerebral edema. Their choice is determined depending on the cause and symptoms accompanying the development of edema.
Ventriculostomy is the drainage of cerebrospinal fluid from the ventricles of the brain through a catheter. This operation is performed to reduce increased intracranial pressure.
The purpose of surgical intervention for cerebral edema may be:
- Removal of a piece of skull bone to relieve intracranial pressure. This operation is called decompressive craniectomy.
- Eliminating the cause of swelling, for example, repairing a damaged blood vessel or removing a tumor.
Diffuse brain injury
Diffuse brain injury is an injury in which either deceleration or acceleration of the head results in subsequent stretching and tearing of axons (nerve fibers connecting nerve cells).
When fibers rupture, diffuse brain injury occurs, which can be caused by a large number of factors: road accidents, blows to the head, fights, beatings, falls from a height, loss of consciousness, and much more.
Symptoms of diffuse injury.
Diffuse brain damage is accompanied by microscopic hemorrhages, which are detected in the centrum semiovale, corpus callosum and upper parts of the brain stem.
Trauma usually manifests itself in the form of a prolonged coma, in most cases turning into a vegetative state, which can last for several months or years.
Treatment of diffuse injuries . Diffuse brain injury cannot be cured by surgery. As a rule, victims receive a number of other comprehensive measures. For example:
- long-term mechanical ventilation in hyperventilation mode;
- therapeutic measures to improve metabolic processes:
- correction of water-electrolyte and acid-base balance;
- normalization of blood composition.
In order to avoid complications in the form of inflammation or infections, the patient, taking into account the characteristics of his intestinal microflora, is prescribed antibacterial drugs.
Diffuse brain injury may have indications for surgery, but only if concomitant focal injuries that cause pressure are detected. Conservative treatment, as a rule, is almost always carried out in the intensive care unit.
Epidural hemorrhage
Epidural hemorrhage (synonyms: extradural hematoma, intracranial suprathecal hematoma) is an accumulation of blood between the dura mater and the bones of the skull.
According to the “classical” concept, the occurrence of an epidural hematoma is caused by a fracture of the temporal bone with damage to the middle meningeal artery at the site of its passage in the bone groove in the pterion region.
The resulting bleeding leads to detachment of the dura mater from the bone with the formation of a hematoma.
An alternative point of view is that the detachment of the dura mater occurs primarily, and bleeding occurs secondary.
Causes of Epidural Hemorrhage
The source of hemorrhage into the epidural space is the branches of the middle meningeal artery, large veins and venous sinuses. Often, epidural hemorrhage is combined with cephalohematoma, especially with linear fractures of the skull bones.
Symptoms of Epidural Hemorrhage
In the absence of surgical treatment, the situation progresses, decerebration, atonic coma and death of the patient occur successively. Other symptoms that occur in a patient with an epidural hematoma are nonspecific and reflect increased intracranial pressure (hypertension, convulsions, headache, vomiting).
It should be remembered that in some patients with epidural hematoma, hemiparesis may be ipsilateral.
Treatment of Epidural Hemorrhage
In most cases, the presence of an epidural hematoma is an indication for urgent surgical intervention.
With timely diagnosis and treatment (in the “light period”), the mortality rate is 5-10%. If the epidural hematoma occurs without a “lucid interval,” the mortality rate increases to 20-25%.
In approximately 20% of patients with an epidural hematoma, a concomitant subdural hematoma is also detected; in such cases, the prognosis is much worse, mortality can reach 90% (as with delayed surgical intervention).
Traumatic subdural hemorrhage
Subdural hemorrhage will develop when the venous sinuses and large veins rupture.
The brain is surrounded by three membranes. The outer, tough meninges are usually the densest. Often, injuries to the head and brain will result in bleeding into the area between the brain and the dura mater. In acute injuries that result in the formation of a subdural hematoma, brain tissue is usually damaged.
The hematoma may grow rapidly. These patients often experience severe neurological differences as well as death. Chronic subdural hemorrhage occurs when the previous hemorrhage does not resolve.
Chronic subdural hemorrhage with its small growth can reach cyclopean sizes, which causes various symptoms.
Traditionally, acute subdural hemorrhage occurs due to trauma, although sometimes there is no head trauma. Hematoma also occurs when the patient takes blood thinning medications.
Traditionally, chronic subdural hemorrhage develops at the site of an unresolved blood clot, limited to its membrane. The vascularized lining may re-bleed into the hematoma, expanding it.
An arteriovenous malformation, brain tumor, or aneurysm can sometimes bleed into the subdural space and form a subdural hemorrhage.
Among the sources of subdural hemorrhages, one can distinguish damaged cortical and vascular vessels, often in the area of the contusion focus. Subdural hematomas are also caused by ruptures of the vein of Galen, as well as damage to the middle meningeal artery, including the accompanying veins.
The main factor of occurrence is trauma due to a discrepancy between the birth canal and the size of the fetus.
This also happens when the neck of the uterus is rigid, when the duration of labor is too short, as well as its long duration with long compression of the fetal head, with excessive softness and pliability of the skull bones, when using vacuum extraction, as well as rotation of the fetus during childbirth, with abnormal presentation of the fetus.
In case of large subdural hematomas, urgent neurosurgical intervention is necessary. In the case of small hematomas, their resorption is used. If the falx or tentorium ruptures, the prognosis is unfavorable.
Sometimes secondary hydrocephalus may develop.
Causes
The main factors in the formation of the process will be as follows:
Traumatic brain injuries
Bruises, concussions and many other pathological conditions. They can provoke stagnation of cerebrospinal fluid and cerebrospinal fluid. Which will ultimately become a factor in the development of the disorder.
Recovery is carried out under the supervision of a neurologist. Minor damage can be corrected at home.
More serious ones, in order to avoid unnecessary risk, are best dealt with in a hospital, in the neurological department of the hospital. We will consider treatment issues further.
Inflammatory processes
Mostly infectious. These are well known to many encephalitis and meningitis. Of course, they do not always lead to the named pathological process. But this is possible, the risks increase as the condition worsens, the temperature rises, and the number of pathogenic organisms increases.
Autoimmune lesions of cerebral structures are slightly less common. They lead to the same consequences.
Treatment of these disorders takes place strictly in an infectious diseases or neurological hospital, under the supervision of a group of doctors. Otherwise there will be complications.
Intoxication, some forms of poisoning
For example, damage to the body by salts of heavy metals. Lead, mercury and others. Toxic vapors of volatile substances: hydrogen sulfide, phosphine and many others.
Everything that has the potential to slow down metabolic processes in cerebral structures and disrupt cellular respiration.
This may also include some medications. As a rule, cerebral edema as a side effect is prescribed directly in the annotation itself, the instructions for a specific drug. All that remains is to look and estimate the risks.
In any case, you cannot prescribe medications on your own. Leave this job to the doctor.
Malignant tumors
Less commonly, benign oncology. In the first case, a couple of factors influence the brain.
- On the one hand, neoplasia grows through healthy tissue, destroying and killing cells. Causes the release of cerebrospinal fluid into internal structures.
- On the other hand, if the size is sufficient, it compresses the fibers. As for benign forms, we are talking only about the mass effect, compression of cerebral structures.
The only way to help the patient is to remove all or most of the tumor. And then, no one guarantees that a relapse will not occur.
Stroke
Acute weakening of the nutrition of nerve tissues. The cause of cerebral edema is the disruption of local blood circulation, the release of fluid from cells into the external space and the increasing phenomena of tissue compression.
The process is closed; the vicious circle can only be broken through medical intervention. A stroke can be ischemic or hemorrhagic, when the vessel cannot withstand it, bursts, and a large hematoma forms.
The result is the same. In the second form, an additional pathogenetic factor appears, extensive hemorrhage. The chances of recovery and even survival are much lower.
Severe allergies
It’s interesting, but even banal immune reactions, false responses of the defense forces can cause brain edema.
Most often, the culprit of the pathological process is anaphylactic shock. The same result occurs with Quincke's edema.
Edema-swelling of the brain is a consequence of stagnation of cerebrospinal fluid, accumulation of cerebrospinal fluid in the intercellular space against the background of damage to cells of cerebral structures by one’s own antibodies.
Fortunately, this is an infrequent problem, and there is every chance you won’t encounter it.
Alcoholism
Long-term alcohol consumption increases the permeability of small and large vessels. The liquid fraction seeps into the intercellular space and literally bursts apart the cerebral structures.
This is very dangerous because it can cause the brain to move and cause death. Such pathological complications develop not only in binge alcoholics and experienced drinkers.
Anyone can encounter a problem by simply exceeding the dosage. If you give up alcohol, the likelihood of a pathological condition will gradually decrease. You need to be observed by a neurologist for at least six months. Just in case.
These are only some of the possible reasons. In fact, the number of pathogenetic factors goes into dozens.
Thus, during the experiments, information was obtained about the swelling of cerebral tissues after intense exposure to cold. The causes of cerebral edema can be liver disorders, cirrhosis and subsequent dysfunctional phenomena.
But these are the main ones. The issue should be considered in its entirety and the pathogenesis clearly delineated. This will help in developing a treatment strategy. You won't be able to figure it out on your own. The participation of a specialist is required.
A look from the inside: what happens under the skull?
If we move away from medical terminology and talk about the problem in ordinary words, then cerebral edema is a pathology in which a failure occurs in the circulation of cerebrospinal fluid. Its volume increases sharply. The situation is aggravated by the fact that the brain is enclosed in a closed cavity. The cerebrospinal fluid begins to put pressure on the tissues, impedes blood circulation, and causes necrotic phenomena (death of parts of the brain). Symptoms of edema appear very quickly, the patient becomes worse and worse. The vessels cannot withstand such loads, the respiratory center stops working, and cardiac arrest occurs.
Causes in children
Factors for the development of edema in younger patients may be those described above. With some exceptions for obvious reasons. But there are also provocateurs that are found only in children in the early period of life.
This may include:
Congenital traumatic brain injuries
The bone structures of a newborn are too soft and pliable. Therefore, it is very easy to get damaged. As a rule, it can be avoided.
This is due to insufficient qualifications or outright negligent attitude of medical personnel, obstetric nurses, obstetricians, and doctors.
The most common occurrence is a concussion. There are also fractures of the skull bones and severe deformities.
Recovery is not always possible. The prospects for correction are considered individually, based on the situation.
Hydrocephalus
This condition has already been discussed. The concentration of cerebrospinal fluid increases, in different volumes.
Recovery is carried out in a neurological hospital, after undergoing primary therapeutic measures. Emergency assistance.
In fact, the child is transferred from the maternity hospital to the hospital. Further, systematic measures of drug correction will be required. And this will continue indefinitely.
Eclampsia in mother
The so-called late toxicosis. The exact reasons for the development of this dangerous pathological process are not fully understood. It is impossible to say anything concrete, there are only assumptions.
Among them are disorders of the liver and kidneys of the expectant mother, unhealthy diet, physical overload, stress, bad habits.
The disorder is characterized in a rather specific way. Blood pressure increases, and significantly: tonometer readings of 200 to 120 are not the limit. If nothing is done, both mother and child will die. There is a risk.
After birth, dangerous complications begin. Almost all children born in such a difficult way end up in intensive care and fight for their lives.
Fortunately, with sufficiently qualified doctors, the chances of recovery are high. Over 70%.
Newborns are monitored for a week or more when there are risks.
In case of cerebral edema, if the child has recovered from the pathological condition, he is registered with a neurologist. It is necessary to examine a young patient at least once every six months.
Diagnosis
The diagnosis of general edema and swelling of the brain is based on clinical data and the results of additional research methods. The cardinal symptom of this process is an increase in intracranial pressure, which is diagnosed by measuring the pressure of the cerebrospinal fluid using tensiometric sensors, as well as on the basis of radiological signs of hypertensive changes in the bones of the skull, EEG data (the appearance of slow waves), and a slowdown in general cerebral circulation; reduction in the volume of the brain ventricles and subarachnoid spaces, detected by encephalo- or ventriculography (see Encephalography).
Local edema and swelling of the brain are diagnosed using echoencephalography (see), when the cut is determined by the displacement of the affected area of the brain; pneumoencephalo- or ventriculography, in which a displacement of the ventricular system in the opposite direction and possible deformations of the ventricle in the focal area are detected; angiography, in which a slowdown in local blood flow, displacement of the vessels of the affected area, and the appearance of a seemingly avascular area are observed in the cut; radioisotope scanning (see), based on the fact that certain isotopes (labeled albumin, 32P, etc.) accumulate in increased quantities in the area of edema and swelling of the brain. A particularly highly informative and largely differentiated understanding of edema and swelling of the brain, their relationship and dynamics of development is provided by the determination of the electrical impedance of brain tissue (see Impedance), carried out using deep electrodes and currents of a certain frequency.
Symptoms, clinical picture of cerebral edema
The manifestations of the pathological process are obvious and typical enough to immediately understand the essence of the disorder.
Among the signs:
- Disorders of consciousness. Symptoms of cerebral edema in adults in the acute phase, with rapid development, include stupor and coma. They differ from simple fainting in depth and duration. If nothing is done in the first few hours, the patient will most likely never regain consciousness.
- Cramps. Attacks of muscle contractions. Like an epileptic seizure. The manifestation is typical for both acute and gradually increasing edema of brain tissue.
- Unbearable headache. In some cases, a person does not lose consciousness immediately. Then this debut is preceded by pronounced evidence of central nervous system dysfunction.
Associated signs of cerebral edema include dizziness, weakness, a feeling of unreality of what is happening and a weak body. This is the result of sharply weakened blood circulation in the nerve tissues.
- Nausea. Not always.
- Vomit. Similar.
- Visual impairment. Double vision due to compression of nerve tissue. They grow gradually.
- Hallucinations. Visual or auditory deceptions of perception.
- Movement coordination disorders.
- Symptoms of cerebral edema include problems with breathing and heart function. Especially in the later stages.
Brain edema in children is accompanied by a drop in blood pressure, apathy, and lack of reactions to stimuli, which should not be normal.
Diagnosis is complicated because it is impossible to know how a person is feeling. It is not immediately clear what is happening.
What are the symptoms of swelling of the brain tissue?
The signs of the pathology are so specific that doctors usually immediately diagnose cerebral edema. Symptoms of this disorder:
- clouding of consciousness is definitely present. Some patients experience stupor, others develop coma;
- headache, which is felt with equal intensity in all parts of the head;
- paralysis of a body part;
- speech and visual disturbances, hallucinations, loss of coordination of movements (if the patient is conscious);
- short-term cramps, muscle weakness;
- drop in blood pressure, unstable pulse. If the patient has such symptoms, this indicates that the swelling has spread to the brain stem, where the vital nerve centers are located;
- sometimes - dizziness, vomiting (not bringing relief), nausea;
- difficulty breathing;
- exotropia;
- floating eyeballs.
The condition deteriorates very rapidly, the person does not realize what is happening to him and loses motor activity.
First aid
We can do little on our own. You need to call an ambulance. While the brigade is driving, it’s worth following a simple algorithm:
- Lay down or make the patient sit. Under no circumstances should blood rush to the head. Therefore, find the optimal position for the victim.
- Provide fresh air. Open a window or window.
- Create conditions of complete peace. No noise, no intense light irritation. Nothing that could lead to the release of excess hormones.
- Carefully monitor your breathing, the condition of your pupils, and your heart activity. If this is possible, then also blood pressure.
What do doctors do after they arrive on site? First, conditions are provided to transport the patient to the hospital.
Several types of drugs are used:
- Osmotic diuretics. The favorite of this type is Mannitol. The concentration is selected individually.
- Electrolytic solutions to restore basic functions of the central nervous system and heart.
- Hormones, corticosteroids. Prednisolone, Dexamethasone, Hydrocortisone in individual quantities. These medications reduce the permeability of the blood-brain barrier.
- Psychomotor agitation is almost always present. It is eliminated with tranquilizers. For example, Diazepam.
- Cerebrovascular drugs. Another option is Piracetam.
Also other means at the discretion of the paramedic or doctor. Next, you need to transport the patient to a hospital. It is important to restore all body functions. This cannot be achieved in an outpatient setting.
Diagnostics
Neurologists and specialized surgeons examine patients. Other related doctors as needed.
Among the events:
- Oral interview with a person. To identify symptoms of the disorder. Provided that the victim is conscious and able to speak. As briefly as possible.
- Anamnesis collection. Study of the origin of the pathological process. The same. The specialist evaluates the overall picture in a nutshell.
- Auscultation. Listening to breathing and heart rate.
- Blood pressure measurement.
- Basic, routine neurological examination. Analysis of reflexes and their preservation.
- ECG, ECHO.
In fact, there is not much time. An experienced specialist understands everything just by looking at a person and studying reflexes. You can’t delay or delay. We need to act.
After emergency care, you can return to a more detailed assessment of the situation. The anamnesis is studied again, an EEG, Dopplerography of the vessels of the head and neck, and carotid arteries is prescribed. An MRI is performed.
It is important to find the cause and eliminate it. This will prevent relapses.
What examination is used to clarify the diagnosis?
Traditionally, in such cases, MRI is used to determine how badly the soft tissue is damaged, where the lesion is located, and to predict complications. A CT scan is done to determine the size of the swelling and the cause that caused it. The patient will also be prescribed clinical tests. A blood test will detect intoxication. Cerebrospinal fluid is often collected. This is necessary to identify infectious diseases and tumors. Diagnostics may include brain scanning with radioactive isotopes, pneumoencephalography, and X-ray of the brain.
Treatment
Therapy depends on the specific provoking factor. Here is a sample list of options:
- TBI. They use diuretics (diuretics), cerebrovascular drugs (Piracetam), nootropics to speed up metabolic processes in the brain (Glycine, Phenibut). Next - depending on the situation. Surgery is needed if there are structural changes in the skull or nerve tissues.
- Inflammation. Antibiotics, anti-inflammatory drugs, antiviral agents, stimulators of interferon production, immunomodulators. If the process is autoimmune - glucocorticoids (Prednisolone as a starting point).
- Poisoning. Detoxification solutions, antidotes. It all depends on the toxic component.
- Oncology. Removal of the tumor. If it is malignant - radiotherapy, chemotherapy.
- Stroke. Nootropics, loop diuretics (Furosemide), also Mannitol, cerebrovascular after partial recovery. If a hematoma forms, surgery is required to remove it.
- Allergy. Glucocorticoids, antihistamines (Pipolfen, Suprastin, Tavegil, Cetrin) are usually enough to relieve cerebral edema.
- Alcoholism. Detoxification, coding and rehabilitation. In different variations.
- Eclampsia. Antihypertensive drugs. In the later stages, labor is provoked. The risks are too high.
- Hydrocephalus. Loop diuretics. Then thiazide and potassium-sparing diuretics to support the body. In severe cases, a catheter is installed to drain excess volumes of cerebrospinal fluid.
The strategy is determined by the doctor after a thorough diagnosis.
Possible consequences
Even if the treatment is competent, in 20% of cases some echoes of the past pathology remain. Among the complications:
- Headache.
- Disorders of higher nervous activity.
- Weakness.
- Regular attacks of nausea.
In addition, the consequences of cerebral edema include weakening of thinking abilities, memory, concentration, and a tendency to weather sensitivity.
In the acute phase, movement of the brain in the skull and death are possible. Also potentially fatal respiratory and cardiac disorders, deep coma. Death or severe disability.
The condition is very dangerous. With proper treatment, the probability of survival and complete preservation of central nervous system functions is more than 90%. It is important not to delay.