You can often find a cerebral hematoma among a variety of brain injuries resulting from head injuries. These are not just bruises, these injuries can be mild, moderate or severe, with possible death. It occurs through the accumulation of clots of coagulated blood in the damaged part of the human brain. The consequences of this injury can be very serious, including death.
Blood vessels that are located both inside the brain itself and pass near the walls of the skull are also susceptible to injury. Such damage can lead to rupture of a brain hematoma.
Mechanism of occurrence
In the skull, the brain is surrounded by cerebrospinal fluid, which has a protective function. However, in the event of a strong impact, it shakes sharply. In this case, the fluid may not cope with its function, and the brain hits the skull. In this case, vascular damage occurs and a hematoma occurs. It can occur immediately after the impact or after some time.
Causes
The following factors can lead to the appearance of a hematoma:
- The presence of a tumor or other neoplasm in the brain.
- Trauma (bruise, consequence of an accident, etc.).
- Disturbances in the development of blood vessels.
- Hypertension.
- Infectious diseases of the brain.
- Neurological diseases.
What can a brain injury lead to? Read the detailed article.
- Liver pathologies.
- Autoimmune processes.
- Blood diseases associated with blood clotting disorders.
- Blood poisoning.
- Use for the treatment of anticoagulants, which inhibit the blood clotting process.
In newborns, a cerebral hematoma can appear as a result of:
- Complicated childbirth.
- Hypoxia suffered during intrauterine development.
- Injuries that a baby can receive while passing through the birth canal.
- Disorders of the blood clotting process.
Symptoms
The first signs of the development of a hematoma in the brain may appear immediately after the injury or after some time. Over time, pressure on the meninges increases, and the victim may experience the following symptoms:
- Headache.
- Dizziness.
- Nausea or even vomiting.
- Increased sleepiness.
Neurologist Mikhail Moiseevich Shperling will talk about the symptoms and treatment of the disease:
- Weakness in the limbs (usually on one side of the body).
- Confusion.
- Different pupil sizes.
- Speech impairment.
If a large amount of blood is released as a result of hemorrhage, then other manifestations of hematoma are possible:
- Coma.
- Lethargic state.
- Cramps.
A hematoma in the brain can be single, or several may appear at once. If this was the result of an impact, then it can occur both directly at the site of damage, and on the opposite side.
First aid
Correctly providing first aid in case of injury means eliminating or at least reducing the likelihood of complications. Do not forget that first aid must be provided correctly so as not to cause further harm. If you get a head injury from a fall, you should do the following to provide first aid:
- Place a tight bandage on your head. This will help prevent hematoma formation.
- Apply something cold for a short time - up to 15-20 minutes. This will help if the victim is in pain. After this, you can apply ice every half hour.
- Lay the victim down. If you have such an injury, you should never stand or sit.
During the first day, apply cold compresses; after two days, you can use alcohol compresses made from vodka and alcohol in a 1:1 ratio. You can use anti-inflammatory drugs to make the hematoma resolve faster - iodine, bodyagu. But remember: consult your doctor before using any product. If the injury is not too serious, treatment can be carried out at home, otherwise the victim must be taken to a traumatology department.
Has the patient lost consciousness or fainted? Contact your doctor immediately. You should also consult a doctor if the patient experiences nausea, vomiting, bleeding from the nose or ears, or convulsions. These symptoms of a brain contusion indicate serious damage to the brain, so delaying help can be life-threatening. In such a situation, it is better to even call an ambulance rather than risk trying to take the victim to the hospital yourself.
Epidural hematoma
An epidural hematoma of the brain can occur as a result of mechanical trauma (fall or blow). They usually appear in the parietal or temporal areas, although they can also be in the occipital or frontal part of the head.
A hematoma occurs between the membrane of the brain and the bones of the skull. Its distribution turns out to be limited by the bone sutures and cannot go beyond their boundaries. Therefore, such hematomas cannot appear at the base of the skull, since here the meninges are in close contact with the cranial bones. Outwardly, it resembles a lens convex on both sides.
The manifestations of an epidural hematoma will depend on the speed and volume of hemorrhage. If an artery has been damaged, it forms very quickly and, as a rule, is large in size, as a result of which the symptoms will be pronounced. When a vein is damaged, the speed of its appearance is insignificant, and the symptoms develop relatively slowly.
Typically, epidural hematoma is characterized by an acute development. Subacute and chronic are most often diagnosed in elderly patients. The cause of its occurrence in most cases is atrophic change.
Manifestations that are characteristic of this type of pathology:
- The presence of a light gap. A certain amount of time passes from the moment of injury to the appearance of its symptoms. As a rule, when injured, a person loses consciousness, which is later restored in full. The patient experiences slight dizziness, minor headaches, muscle weakness and nausea. Over time, the condition begins to deteriorate noticeably.
Definition from Wikipedia: A lucid interval is a temporary improvement in a patient's condition after a traumatic brain injury, followed by a sharp deterioration. The light gap is most typical for epidural hematoma, in which it is observed in 20-50% of patients.
- On the side where the hematoma occurred, the pupil becomes wider and the eyelid droops.
- On the opposite side, manifestations of pyramidal insufficiency are noted (muscle weakness, increased tendon reflexes, etc.).
Symptoms of epidural hematoma
Symptoms are associated with compression of adjacent brain tissue by blood. Neighboring areas begin to shift. Intracranial pressure increases. As a result, the patient experiences psychomotor agitation, which is replaced by depression of consciousness. A coma state gradually develops. At the moment when the victim is conscious, he complains of a severe headache, and vomiting often occurs. Due to the fact that certain brain structures are displaced, a person’s breathing quickens, blood pressure increases, and the pulse becomes disrupted. As compression of the brain stem increases, circulatory and respiratory function may be impaired, which can cause death.
From the moment the first manifestations of a hematoma occur until falling into a coma, different times may pass, depending on where it appeared and how much blood entered the cranial cavity. Usually it takes from a couple of hours to several days.
Development process
A brain hematoma can have several stages of development. According to the time of their formation, acute, subacute and chronic formations are distinguished. In the first case, a cavity with blood is formed in the first three days after the rupture of the vessels. At the same time, the symptoms of this condition are determined (before the formation of the capsule).
Subacute hematomas appear during the formation of a dense shell of the formation. Symptoms are more pronounced in the period from the 4th to the 15th day from the moment of the provoking factor.
Chronic hematomas make themselves felt 15 days after a head injury. Treatment depends on the volume and process of development of this formation.
However, the most important thing in diagnosis is to determine the area where the hemorrhage occurred. This will be confirmed by symptoms and subsequent examination of the intracranial space.
Subdural hematoma
This form of pathology is considered the most diagnosed. It is not limited in its distribution in the brain region. Because of this, the subdural hematoma of the brain has a significant volume. In most cases, lamellar or mantle-shaped hematomas are diagnosed. Often two hematomas occur simultaneously (one at the site of injury, the other on the reverse side).
Acute subdural hematomas do not have a clear space. The victim's condition worsens gradually (consciousness is impaired, signs of autonomic disorders appear, indicating that the brain stem is being compressed). At the initial stage, the patient experiences a severe headache with nausea and uncontrollable vomiting. Gradually, they are added to: speech impairment, pupils become different sizes, sensitivity is lost. Due to irritation of the cerebral cortex, the victim experiences convulsions, breathing and pulse are disrupted, and blood pressure first rises and then drops sharply.
Subacute subdural hematomas are especially dangerous. Immediately after a blood vessel is damaged, the person loses consciousness for several minutes. Then a light period begins, lasting up to 2 weeks. In this case, there are no neurological manifestations of pathology. General weakness, minor headache and fatigue are possible.
At the end of the light period, the victim experiences psychomotor agitation, convulsions and possible loss of consciousness. This happens:
- Speech impairment.
- Weakness in the limbs, on the side opposite to the source of injury.
- Enlargement of the pupil on the side where the hematoma occurred, which stops responding to external stimuli.
- Uncontrollable vomiting.
- Slowing heart rate.
- A jump in blood pressure.
Coma gradually develops. If the damage affects the brain stem, a person may experience changes in the functioning of the body that are incompatible with life.
Dear readers, we have prepared a lecture on TBI for you. Watch the video below:
Chronic subdural hematoma begins to manifest itself after a long time (sometimes even months) after a traumatic brain injury. This diagnosis is more often made in older people. During the light period, patients feel a slight headache and fatigue. At the same time, their way of life is not disrupted.
At the end of the light interval, a sharp manifestation of focal brain damage occurs. Outwardly, this is very similar to the symptoms of a stroke. However, patients rarely associate this condition with a TBI. The person’s condition gradually worsens, a change in pulse occurs, breathing and consciousness are impaired. To make a diagnosis, the doctor prescribes a CT or MRI.
Classification
A hematoma on the head after a blow or other incident can be one of three types:
- Epidural. This is the most common and easiest injury, during which the vessels are damaged only above the surface of the skull. The victim, having received such a bruise, does not lose consciousness, but may still experience some symptoms.
- Subdural. It is a more dangerous injury because when it occurs, damage occurs to the vessels that are located between the inside of the skull and the brain.
- Intracerebral. The most dangerous type of damage, during which blood accumulates in the brain tissue, which leads to the death of nerve cells - neurons.
A hematoma of any of these types can cause very serious consequences, sometimes even death, so treatment should begin as soon as possible after injury.
An intracranial hematoma occurs when blood accumulates in the soft tissues of the head or in the limited space between the bones of the skull and the meninges. The location of the damaged vessel determines the type of hematoma.
- Subdural hematoma. It develops when the vessels (usually venous) are damaged, located in the cavity between the brain and the dura mater.
- Epidural hematoma. The most common and relatively mild type of hemorrhage due to head injuries. Occurs when blood vessels (mainly arteries) are injured in the area between the dura mater and the bones of the skull. Epidural (extradural) hematoma is typical for head injuries and skull fractures.
- Intracerebral hematoma. Hemorrhagic stroke occurs when blood vessels are destroyed and hemorrhage in the brain tissue. As a result, the white matter is affected, which can cause the destruction of nerve cells. With severe injuries, several intracerebral (intraparenchymal) hematomas or a combination of different types may appear.
Depending on the length of the period between the injury and the appearance of symptoms, several options for the course of the disease are possible:
- Spicy. The first symptoms appear immediately after injury and progress during the first three days.
- Subacute. Signs of hematoma appear 4-14 days after injury.
- Chronic. The clinical picture is observed for 15 or more days.
Any type of head hematoma requires a mandatory consultation with a neurologist!
When a bruise occurs, few people attach serious importance to it. However, in order to prevent serious health problems, it is necessary to know which degree of the disease does not require special treatment, and which requires qualified therapy.
Degrees of hematoma:
- First degree. It is a minor damage to the skin that goes away on its own within a few days;
- Second degree. In the second degree of hematoma, more serious damage is observed, such as muscle rupture with the formation of hematoma and swelling of soft tissues. In this case, the site of injury hurts, and general health worsens;
- Third degree. Muscles and tendons are damaged, and dislocation may occur. The third degree is especially dangerous for injuries to the head, joints and tailbone;
- Fourth degree. The most dangerous degree, as a result of which the functioning of the damaged part of the body may be partially or completely disrupted.
READ MORE: Laser treatment of nail fungus in St. Petersburg reviews
According to the type of hemorrhage, hematomas can be arterial, venous or mixed. And according to localization they are divided into intermuscular, subcutaneous and subfascial.
Main symptoms:
- pain;
- swelling;
- dysfunction of the damaged muscle;
- swelling;
- change in fabric color;
- pulsation, which occurs when large arteries are incompletely ruptured;
- local and general increase in temperature.
A head hematoma is the formation of a clot of dried blood between soft tissues, meninges, or in the brain after traumatic injury to blood vessels. Occurs after birth injuries, accidents, falls from a height, blows. Impaired blood cell functions in diseases such as hemophilia, leukemia, and liver disease increase the risk of the formation of blood tumors after bruises.
There is a classification based on the location of hemorrhage and other characteristics. There are several types based on location:
- Subcutaneous, intramuscular, submucosal - an ordinary lump.
- Epidural - above the dura mater.
- Subdural - between the dura and arachnoid membranes.
- Intracerebral, incl. in the ventricles of the brain.
- Paraorbital - blood flows into the orbital tissue.
Subcutaneous hemorrhage after a bruise does not pose a strong threat to the patient’s life. It can be combined with a mild concussion, which manifests itself in some stupor of the victim. Typically, such formations, which are a jelly-like substance of clotted blood, are removed in a hospital emergency room. Most often, such hemorrhage resolves on its own.
An epidural can also lead to a coma, as this causes bleeding from large vessels. A subdural blood tumor can compress brain tissue, which also leads to serious consequences - impairment of memory, skills and other functions of the cortex.
Intracerebral - serious damage that can push back the brainstem, thereby jeopardizing vital centers - the vasomotor and respiratory.
There are also types of blood tumors based on their outcome:
- Pulsating occurs, as a rule, when a large vessel is damaged. At the same time, blood continues to flow into the cavity, around which connective tissue has already formed. Pulsation of the vessel is felt when the swelling is palpated. This is one of the most dangerous injuries, which can lead to both large blood loss and blockage of this vessel with thrombotic masses.
- Festering. When a blood tumor forms, it either resolves with the help of tissue enzymes, or an infection develops in it, leading to suppuration.
- Curled up.
According to the flow, acute, subacute and chronic blood tumors are distinguished. In case of acute intracranial hemorrhage after a contusion, surgical decompression of the brain is necessary.
TBIs are injuries associated with a tear or disruption of the integrity of the soft and bone tissues of the skull, cells, lining of the brain, nerve endings, blood vessels, as well as the gray matter located inside.
Head trauma is classified according to the nature of the injuries received:
- open;
- closed;
- penetrating.
A closed skull injury, on the contrary, is characterized by the undisturbed natural integrity of the external soft tissues and is not dangerous due to the entry of pathogenic bacteria inside.
The most common types:
- concussion – brain activity is not impaired. The recovery process lasts about a month. Possible short-term memory loss, nausea, vomiting;
- compression of the brain - an internal hematoma that appears during an injury or air that has penetrated inside puts pressure on the brain. The general condition of the patient depends on the severity of the injury - mild or severe. The mild form is characterized by a short-term loss of consciousness. The consequences of severe traumatic brain injury are a constant increase in the size of the hematoma, which leads to protrusion of some part of the brain located on the opposite side of the pressure point;
- brain contusion (concussion) – has three degrees of severity (mild, severe and moderate);
- a fracture of the base and vault of the skull is usually combined with a brain contusion. Characterized by profuse bleeding from the nose and ears, paralysis of the facial muscles;
- hemorrhage.
Severe injuries to the skull lead to prolonged loss of consciousness, lasting two weeks or more. The patient has weak muscle tone, cramps, and partial paralysis of the limbs. In case of a bruise with such symptoms, a fracture of the base of the skull is most often diagnosed.
Therapy used in the treatment of head injuries involves avoiding secondary trauma.
is based on the division of all gunshot wounds into soft tissue damage, non-penetrating and penetrating open craniocerebral injury proposed in 1917 by N. N. Petrov.
Soft tissue injury occurs in approximately 50% of traumatic brain injuries. Traumatic brain injury with massive damage to the soft tissues of the head (injuries of all layers of soft tissues with damage to the aponeurosis to the periosteum) is classified as open injuries of the skull. At the same time, there is a real possibility of infection spreading through the veins with the further development of infectious and inflammatory intracranial complications (meningitis, encephalitis, etc.).
Open TBI without damage to the dura mater is classified as non-penetrating TBI. It is characterized by damage to the soft tissues and bones of the skull while maintaining the integrity of the dura mater and occurs in 20% of cases. In this case, contusions, areas of crushing of the brain and intracranial hematomas are often formed, requiring urgent surgical intervention.
Penetrating wounds are characterized by disruption of the integrity of the dura mater and direct infection of the intrathecal spaces and substance of the brain. The frequency of penetrating wounds reaches 30% of all gunshot injuries (B.V. Gaidar et al., 1997).
Based on the type of projectile that causes injuries, a distinction is made between spherical, fragmentation, and wounds caused by special projectiles (spherical, arrow-shaped elements, etc.). Based on the type of wound channel, blind, through, tangential, and rebound wounds are distinguished. Are you blind?
Intracerebral hematoma
This pathology is associated with the accumulation of blood directly in the brain tissue. It usually occurs in the frontal or temporal parts, and has a rounded shape. If the cause is trauma, then the hematoma forms near the cerebral cortex, and with a vascular nature of development, in the depths of the brain tissue.
Symptoms occur immediately after hemorrhage. This is due to the fact that blood instantly fills the nerve tissue. In this case it is observed:
- Inability to speak or perceive speech.
- Loss of sensation in a specific part of the body.
- Facial distortion.
- Paresis.
- Visual impairment.
- Impaired movement coordination.
- Severe mental disorder.
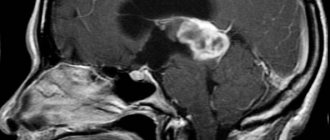
Intracerebral hematoma on an MRI.
Symptoms will depend on where in the brain the nerve tissue was damaged. Along with focal manifestations, the patient also experiences other disorders:
- Spontaneous movement of the eyeballs.
- Strabismus.
- Impaired pulse and breathing.
- Difficulty swallowing.
If the ventricles are damaged, the victim's condition worsens sharply. In this case, the body temperature can rise to 40 degrees, consciousness is impaired, coma develops, which can lead to the death of the patient.
Doctors' opinion
In no case should we forget that head injuries are not to be joked about. Even if the injury does not seem serious, you should definitely consult a traumatologist, since sometimes with head injuries, symptoms do not appear at first. This is where the main danger of head injuries lies. Fortunately, modern medical technologies make it possible to accurately diagnose injuries and thereby facilitate treatment.
Remember that if any serious symptoms appear, it is better to call an ambulance and not try to take the victim to the hospital yourself. If he is not provided with qualified assistance, complications that are dangerous to health and even life may develop. The main thing in a successful recovery is timely assistance.
Subarachnoid hematoma
In this case, hemorrhage occurs between the soft and arachnoid membranes of the brain. There are traumatic, non-traumatic and spontaneous subarachnoid hematomas. The main symptom is sharp pain, which patients compare to a blow. There is pulsation in the occipital region.
Other symptoms include:
- Cramps.
- Vomit.
- Increased pressure.
- Impaired consciousness.
Treatment for this pathology consists of surgery to stop the bleeding and remove the hematoma. About half of people with this diagnosis die.
Diagnostics
To make an accurate diagnosis, the doctor will need:
- Collect anamnesis.
- Analyze existing clinical symptoms.
Epidural hematoma on MRI image
- Perform vascular angiography.
- Do an echoencephalography.
- Conduct a CT or MRI (read which is better here).
Treatment
The doctor will be able to prescribe treatment only after a comprehensive examination and diagnosis. Conservative and surgical methods are used for this. The treatment method is selected based on the nature of the injury, its severity and the patient’s condition.
Conservative treatment
If the identified hematomas are small in size and they do not pose a threat to the life of the victim, he is prescribed conservative treatment, which consists of bed rest and the use of medications:
- To relieve headaches, drugs are used - analgesics (Analgin, Ketanov, etc.).
- To eliminate vomiting, Cerucal is prescribed.
- Treatment of excessive mental arousal is carried out with tranquilizers and antipsychotics.
- If respiratory function is depressed, artificial ventilation of the lungs is necessary.
- Treatment of cerebral edema requires taking Mannitol.
- To prevent spasms of blood vessels, the doctor will prescribe calcium channel blockers.
- To improve blood circulation, treatment with Pentoxifylline or Heparin is used.
- Additionally, nootropics, multivitamins and preparations based on B vitamins are prescribed for treatment.
As a rule, the hematoma resolves within 1 month.
Surgery
If the hematoma is extensive, then the patient needs open brain surgery. The consequences after surgery can be very severe and accompanied by various complications, and the patient will require long-term rehabilitation.
Craniotomy
There is the possibility of endoscopic surgery to remove the hematoma. This treatment method is more gentle and, according to patient reviews, requires a shorter recovery period.
The effectiveness of surgical treatment depends entirely on the stage at which it was carried out.
Consequences
The consequences of a brain hematoma are quite severe:
- Speech disorder. At the same time, it is difficult for the patient not only to speak, but also to perceive speech; he has difficulties with writing, reading, etc.
- Chronic fatigue.
- Impaired mental activity and memory.
- Sleep disorder.
- Depressive state.
- Increased weather sensitivity.
- Swallowing dysfunction.
- High irritability.
Urinary incontinence (incontinence) is an involuntary leakage of urine that cannot be controlled by volition.
- Sudden change of mood.
- Unreasonable aggression.
- Neuroses.
- Weakness in the limbs, even to the point of paralysis.
- Impaired coordination of movement and perception of surrounding reality.
- Urinary incontinence or spontaneous bowel movements.
- Cramps.
- Development of dementia.
The prognosis for babies can be quite favorable. This depends on the shape, degree of development of the hematoma and the timeliness of its treatment. Among the consequences:
- Development of cerebral palsy (CP).
- Developmental delay or delay (physical or mental).
- Various mental disorders.
- Hydrocephalus.
- The occurrence of epileptic seizures.
Diagnostic methods
To determine the presence of a cerebral hematoma, first of all, a visual examination of the patient’s condition is carried out, his ability to speak, follow the movement of objects, determine the size of the pupils and their reaction to light.
If general symptoms occur, it is urgent to determine the type and location of the hematoma; for this, the following methods of studying the brain are used:
- echoencelography;
- Magnetic resonance imaging;
- CT scan;
- angiography of the vessels of the head.
It is important to conduct a comprehensive examination, since often the same injury can cause both a subdural and epidural hematoma.