Source of the image for the article (c) Can Stock Photo / peshkov
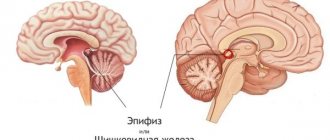
If you are looking for information on the topic “cyst in the brain” or the answer to the question “what is a cyst in the brain?”, then this article is for you. A cyst in the brain, or more precisely, an arachnoid cerebrospinal fluid cyst, is a congenital formation that arises during development as a result of splitting of the arachnoid (arachnoid) membrane of the brain. The cyst is filled with cerebrospinal fluid (CSF), a physiological fluid that washes the brain and spinal cord. True congenital arachnoid cysts should be distinguished from cysts that appear after damage to the brain due to traumatic brain injury, stroke, infection, or surgery.
Arachnoid cyst ICD10 code G93.0 (cerebral cyst), Q04.6 (congenital cerebral cysts).
What causes a cyst in the head?
A benign spherical formation - a cyst in the brain - is filled with cerebrospinal fluid inside. The severity of symptoms depends on the size of the tumor, but it is detected during a random medical examination or when any other disease is diagnosed. Arachnoid cysts of the brain are asymptomatic in most cases. Vivid neurological symptoms are present in only 20% of patients. Factors influencing the appearance and growth of cysts:
- any brain injury;
- increase in fluid pressure inside the cystic formation;
- inflammatory process in the brain (infection, virus).
Treatment methods
The most common treatment for this type of tumor is surgery. But drug treatment is also possible.
First of all, wait-and-see tactics are used for small tumors, especially if growth is not observed. If an underlying disease (inflammation, infection) led to the formation of a cyst, then it is this disease that is treated, and the symptoms are relieved with the help of medications. Surgery is resorted to if conservative treatment is ineffective.
There are several types of surgical interventions performed to treat arachnoid retrocerebellar cyst of the brain.
- Brain shunting (used in case of constant flow of cerebrospinal fluid to the cyst);
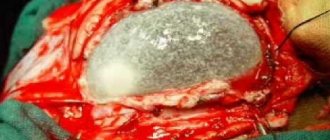
- neurosurgical operation with craniotomy (the tumor and adjacent tissues are completely removed);
- endoscopy (a more gentle method, which is rarely used due to the depth of the tumor);
- laser excision.
Characteristics of the disease
A cerebrospinal fluid cyst is a formation in the brain tissue that is not a tumor, as confirmed by its morphological structure. It is a cavity isolated from other brain structures with liquid contents and dense walls. Clinically significant are large cystic formations that cause mechanical compression, compression, deformation of surrounding tissues - the brain matter, cerebrospinal fluid outflow tracts, elements of the circulatory system supplying the brain.
Arachnoid cysts are formations whose share, according to the results of intravital instrumental diagnostics, is equal to 1% of all volumetric processes occurring in the brain, which is less than that detected during autopsies (5 cases per 1000 patients). Normally, in adults and children, arachnoid cerebrospinal fluid cysts are absent in the brain tissue; if they are present, the degree of impact on health is determined by their size. Depending on the volume of the cystic cavity, the types of formations are distinguished:
- Small (volume does not exceed 30 ml).
- Medium (volume does not exceed 70 ml).
- Large (volume exceeds 70 ml).
Large formations are almost always associated with dislocation (displacement) of brain structures, which leads to neurological deficits. The suprassellar (growing deep into the skull) form is considered the most dangerous because it almost always causes occlusion or hydrocephalus. Treatment of hydrocephalic syndrome alone in this case is not enough due to significant compression of brain structures with the appearance of focal symptoms.
Diagnostic signs
To identify this pathology, it is necessary to undergo a thorough diagnosis. When a patient consults a doctor, it is necessary to collect an anamnesis, which includes data on previous diseases and injuries. It is also worth asking the patient in detail about the complaints. After collecting an anamnesis of life and illnesses, the patient is sent for diagnostic procedures.
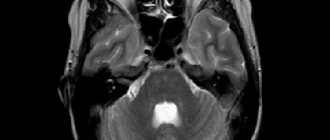
- Magnetic resonance imaging helps to clarify the location and size of the tumor. Normally, no cavities should be found.
- Computed tomography is another modern and highly accurate diagnostic method that provides detailed information about the pathology.
- A biochemical blood test is necessary to detect elevated cholesterol levels and increased blood clotting.
- A blood test to detect infections in the body that may cause the disease.
- Angiography of cerebral vessels. Using this study, it is possible to differentiate malignant neoplasms from brain cysts. In the presence of a cancerous tumor, the contrast agent accumulates in its body, but with a cyst this sign is not observed.
- Monitoring changes in blood pressure levels.
- Ultrasound Dopplerography (Doppler ultrasound) allows you to assess the condition of the vessels and their patency.
- Diagnosis of pathology of the cardiovascular system. This is necessary, since developed heart failure is a pathological factor in the formation of brain cysts.
Why is a retrocerebellar arachnoid cyst dangerous?
Untimely treatment of the disease leads to serious consequences that significantly worsen the quality of human life. First of all, a large cystic tumor begins to put pressure on various parts of the brain, causing a disruption in the functioning of vital systems.
Another serious complication of a cerebrospinal fluid cyst is a violation of the integrity of its membrane. In this case, the fluid accumulated from the inside pours into the brain and provokes the development of infectious pathologies.
Monitor your health and well-being very carefully. Negligent attitude to the manifested symptoms, in the presence of a tumor, is fraught with death.
This type of tumor is located between the soft and hard membranes of the brain. A risk factor is that a retrocerebellar arachnoid cyst may subsequently promote cell death, a condition that leads to the development of a malignant tumor. In children, the neoplasm leads to developmental delay or hypermobility syndrome. In adults, a growing cyst increases pressure on the gray matter and brain tissue.
Prognosis and possible complications
With adequate treatment of a cerebrospinal fluid cyst, the prognosis of the disease is favorable in most cases. The chances of a full recovery are high even after surgery.
Important! The risk of complications appears in the absence of timely measures and in especially severe cases.
Such patients experience: hearing loss, decreased vision, speech disorders, convulsions, seizures, loss of skin sensitivity, paralysis of various parts of the body. When seeking medical help late, patients may develop brain hernias, tissue necrosis, hydrocephalus and other dangerous diseases. Their outcome is often death.
Classification of pathology
Arachnoid cysts are primary and secondary. In the first case, they appear as a congenital developmental anomaly. In the second - as a result of pathological processes affecting brain tissue. The walls of the secondary neoplasm are formed by collagen and scar tissue.
In 88% of cases, single cystic formations are observed, in 12% of cases – multiple ones. The location of multiple in 5% of cases covers both hemispheres. Arachnoid changes are classified depending on the location and nature of the growth of the cystic formation. The following forms are distinguished:
- With localization in the Sylvian (lateral) fissure (34% of cases). Congenital anomaly. Symptoms depend on the diameter of the cavity and the degree of dislocation (displacement) of nearby brain tissue. More often it manifests itself as a feeling of fullness in the head area, which is accompanied by pulsation and the occurrence of tinnitus while maintaining hearing function. Seizures and visual disturbances are common.
- Suprasellar (2% of cases). Congenital form. The cavity is most often localized in the area of the chiasm formed by the optic nerves. Manifested by dizziness, visual dysfunction, and impaired motor coordination.
- Localized in the area of the lateral ventricle (2% of cases). Congenital or acquired form. The clinical picture is represented by motor and visual disturbances, hearing impairment (sensorineural hearing loss), tinnitus, dysphagia (swallowing dysfunction).
Cerebellar (localized in the cerebellum) cyst formed in the brain occurs with a frequency of 32% of cases. It manifests itself as a violation of motor coordination, changes in muscle tone (hypotonia), nystagmus (usually horizontal). The patient experiences a change in gait, which becomes unstable and shaky.
An arachnoid cerebrospinal fluid cyst localized in the posterior cranial fossa is accompanied by oculomotor disorders (strabismus, loss of visual fields, paralysis of the optic nerves). A cystic formation in the area of the right or left frontal lobe is manifested by characteristic symptoms - deterioration of cognitive abilities, changes in gait, speech dysfunction (aphasia).
Arachnoid cyst of the brain: symptoms, causes, treatment and prevention
Based on statistical data, a cystic tumor most often forms during fetal development. However, there are also acquired liquor neoplasms, the development of which is caused by:
- Birth injuries: too large a fetus, prematurity, the use of additional instruments during childbirth, mechanical damage during labor resulting from poor-quality manipulations by the obstetrician;
- Traumatic brain injuries accompanied by concussion;
- Previous infectious diseases affecting the brain: meningitis, encephalitis, neurogenic infections;
- Pathologies of the cardiovascular system, causing the formation of blood clots or deterioration in the outflow of blood fluid;
- Previous operations during which manipulations were performed with the brain.
The clinical picture of liquor cystic changes may not appear for quite a long time, and sometimes for a lifetime. In such situations, the tumor is not life-threatening and does not require elimination. But if the size of the neoplasm is large, and the pathology affects important endings, blood vessels and brain tissue, then the following signs may appear:
- Headaches that cannot be relieved with painkillers;
- Frequent attacks of nausea and vomiting;
- Feeling of pulsation in the area of tissue damage;
- Deterioration of sensitivity;
- Loss of coordination;
- Deviations in the perception of the surrounding world;
- Psychological deviations (increased excitability, irritability or, conversely, a passive attitude towards everything that happens);
- Unreasonable spasms of muscle tissue;
- Partial loss of hearing, vision, voice;
- Movement disorders.
The above symptoms do not appear at the same time. It all depends on which part of the brain the cyst is localized in and how much pressure it puts on the brain.
To establish an accurate diagnosis, determine the size and nature of the progressive cyst, doctors refer the patient to the following examination procedures:
- X-ray of the brain;
- Laboratory examination of blood fluid;
- Computer and magnetic resonance imaging.
After receiving the results, the necessary treatment tactics are selected individually for each patient.
Asymptomatic small AKs are discovered incidentally during examination for another reason. Symptoms become more pronounced with growth and depending on the location of the cyst, compression of tissues and brain matter. The manifestation of focal symptoms occurs against the background of the formation of a hygroma or when the aortic valve ruptures.
As the formations progress, adults lose orientation and sleep. They complain of uncomfortable conditions in which muscle tone is disturbed, limbs twitch involuntarily and go numb, and lameness occurs. I regularly experience tinnitus, migraines, nausea with vomiting, and often feel dizzy and even lose consciousness. Also in patients:
- hearing and vision are impaired;
- hallucinations and convulsions occur;
- the psyche is upset;
- “bursting” inside the head and the pulse is felt;
- Pain under the skull intensifies when moving the head.
A secondary (acquired) cyst complements the clinical picture with manifestations of the underlying disease or injury.
The development of a ramolation formation (cyst) in infants occurs anywhere in the arachnoid membrane due to inflammation, damage or other pathology of the brain. All cysts disrupt the circulation of fluid within the tissues. Until now, there is no universal list of types of neoplasms and their localization.
- pulsating fontanel;
- disoriented look;
- profuse, fountain-like regurgitation after feeding.
This is the basis for a full examination of the baby at the medical center.
Signs of a cyst appear as it grows. Headaches begin, tinnitus and skin sensitivity are disrupted. If an arachnoid cyst of the brain is not treated, paralysis of the limbs may occur, epileptic seizures may appear, deafness may increase, and vision may be lost. Symptoms of the disease are characteristic of a specific affected area.
In adults
Small bubbles with liquid contents in the brain tissue do not pose a threat to humans, and he can easily live with them throughout his life. Large formations of a progressive type have clear signs of pathology. This:
- loss of orientation;
- regular migraine;
- loss of sleep;
- violation of muscle tone;
- lameness;
- nausea, vomiting;
- twitching of limbs (involuntary);
- dizziness.
In children
When a cyst forms in newborns as a result of inflammation, damage or other pathology of the brain, it is a ramification formation that manifests itself anywhere. If the baby has parasites, for example, tapeworm, then a parasitic cyst may develop. Brain tumors are a consequence of impaired circulation of interstitial fluid.
- pulsating fontanel;
- lethargy of the limbs;
- disoriented look;
- spitting up like a fountain after feeding.
Cysts can be divided into several types:
- Cerebellar cyst of the brain
In medical practice, the pathology is called a retrocerebellar cyst and is diagnosed in the area of mass death of gray brain cells. Inside the cyst bubble, spinal fluid and remnants of dead tissue are found. Arachnoid cysts of the presented nature are among the group of the most dangerous accumulations of cells in the brain.
The tumor occurs in the gray matter, and even a slight increase leads to pressure on neighboring tissues. In approximately 90% of cases, a cerebellar cyst of the brain occurs as a result of a complex course of cardiovascular pathologies. Often diagnosed in older people as a result of atherosclerosis.
- CSF cyst of the brain
It develops in another part - in the cavities between the structures of the brain, does not affect the gray matter, but can put pressure on it during growth. Pathology is formed as a result of hemorrhages and surgical interventions. Doctors prescribe symptomatic treatment; surgical intervention is rarely required.
Liqueur arachnoid changes practically do not manifest themselves in any way; in most clinical cases they are not detected throughout life. If the pathology occurs in a child, then the head becomes enlarged as it grows up, and a dimple may appear on the forehead.
- Congenital arachnoid cyst of the brain
Included in the category of primary pathologies, it develops at the stage of embryonic maturation. The cause of the pathology is considered to be a genetic abnormality of the skull, as well as the influence of extraneous chemical or physical factors.
The last two signs mean: medications, radiation, toxic effects. In some cases, a tumor forms due to oxygen starvation as a result of difficult childbirth.
- Subarachnoid leukrocystic change
It is formed during the formation of the embryo for the same reasons as the simple form. As a person grows older, it causes abnormalities in gait and strange pulsations in the skull and muscles.
Unlike an arachnoid cyst, a cerebellar cyst of the brain always forms inside the gray matter, and a simple form - only in the intermediate tissue. Ordinary arachnoid cysts do not require surgical intervention.
A retrocerebellar neoplasm destroys the central nervous system, as it always enlarges and leads to the death of surrounding cells.
Neoplasms affecting the membrane differ from each other in the place of origin: arachnoid cyst of the sella turcica, arachnoid cyst of the posterior cranial fossa, a formation in the lumbar region or the spinal canal.
Reasons for development
Arachnoid changes of a liquorocystic nature are formed even during the period of bearing a child; they are called primary:
- drug abuse, use of several groups of drugs in one period of time;
- radiation exposure during pregnancy (CT, MRI, X-ray);
- intrauterine infections: herpes, toxoplasmosis, rubella;
- bad habits;
- constant overheating of the mother's body;
- genetic mutations (Marfan syndrome);
- poor environmental situation.
A secondary arachnoid cerebrospinal fluid cyst forms in response to inflammatory processes that affect the brain. Most often these include: encephalitis, meningitis, arachnoiditis. May occur in response to hemorrhages, surgical interventions, hematomas and strokes. A concussion often provokes the formation of a cyst.
There is another factor due to which the arachnoid cyst of the brain begins to grow - secondary injuries and severe infections.
Arachnoid cerebrospinal fluid cysts manifest themselves in different ways, and often the symptoms do not make it possible to make a diagnosis. Here are just a few common signs:
- congenital pathologies begin to manifest themselves closer to 15-20 years, but not later;
- the nature of the symptoms is influenced by the size of the tumor formations;
- hemispheric location leads to problems with coordination, vomiting, nausea and constant headaches;
- arachnoid cyst of the posterior cranial fossa, as well as focal lesions lead to symptoms depending on the area on which the tumors press;
- general cerebral symptoms are accompanied by high blood pressure, vision problems, epilepsy and inhibited psychomotor development.
Patients often experience general weakness, severe hand tremors, and an unusual gait. Convulsions and seizures lead to the fact that arachnoid cysts are often confused with other diseases of the nervous system.
Arachnoid changes of a liquorocystic nature are diagnosed in several ways:
- CT scan. Determines the position and parameters of the tumor.
- Magnetic resonance imaging. The MRI picture of arachnoid changes of a liquorocystic nature reflects the type of tumor - malignant or benign.
- ECG, Echo-CG. Prescribed to determine the condition of the heart and its rhythm.
- Ultrasound Doppler. Displays parameters of cerebral circulation and vascular patency.
- UAC. The test provides true information about the causes of the tumor.
- Upper pressure control. Observation is necessary to determine the patient's susceptibility to stroke.
- Contrast x-ray of blood vessels. Carry out to exclude oncological processes.
- Cholesterol measurement. Necessary to determine the risk of vascular pathologies.
Reasons for education
The following types of neoplasms are distinguished depending on location:
- Arachnoid cyst. The formation is located between the membranes of the brain. More often diagnosed in male patients. If the tumor does not grow, treatment is not required. In childhood, it can cause the appearance of hydrocephalus and an increase in the size of the skull.
- Retrocerebellar arachnoid cyst of the brain. The development of a pathological formation in the thickness of the organ is characteristic. Main causes: stroke, encephalitis, circulatory disorders. A retrocerebellar cyst can lead to the destruction of neurons in the brain.
- Subarachnoid cyst of the brain. This is a congenital pathological formation that is discovered by chance. The disease can cause convulsions, unsteadiness of gait, and pulsation inside the head.
- Arachnoid cerebrospinal fluid cyst of the brain. Education develops in patients with atherosclerotic and age-related changes.
Depending on the causes of development, the pathology is:
- primary (congenital). Formed during intrauterine development of the fetus or as a result of suffocation in a child during childbirth. An example of such a formation is a Blake's pouch cyst;
- secondary. Pathological formation develops against the background of previous diseases or exposure to environmental factors.
According to the clinical picture of the disease, the following are distinguished:
- progressive formations. An increase in clinical symptoms is characteristic, which is associated with an increase in the size of the arachnoid formation;
- frozen neoplasms. They have a latent course and do not increase in volume.
Determining the type of brain cyst according to this classification is of paramount importance for choosing effective treatment tactics.
Congenital (brain cysts in newborns) are formed against the background of disturbances in the processes of intrauterine development of the brain. Provoking factors:
- intrauterine infection of the fetus (herpes, toxoplasmosis, cytomegalovirus, rubella);
- intoxication (drinking alcohol, smoking, using drugs with a teratogenic effect, drug addiction);
- irradiation;
- overheating (frequent exposure to the sun, visiting a bathhouse, sauna).
An arachnoid cyst of the sphenoid sinus can develop against the background of Marfan syndrome (mutations of connective tissue), hypogenesis of the corpus callosum (lack of septa in this structure).
Secondary formations develop due to the following conditions:
- traumatic brain injuries;
- brain surgery;
- cerebrovascular accidents: stroke, ischemic disease, multiple sclerosis;
- degenerative processes in the brain;
- infectious diseases (meningitis, meningoencephalitis, arachnoiditis).
An arachnoid cyst in the temporal region often develops as a result of the development of a hematoma.
In 80% of cases, an arachnoid cyst of the brain does not lead to the development of unpleasant symptoms. The pathology is characterized by the presence of nonspecific symptoms, which complicates diagnosis. Manifestations of the disease are determined by the localization of the pathological formation and its size.
- Dizziness. This is the most common symptom that does not depend on the time of day or exposure factors.
- Nausea and vomiting.
- Cramps (involuntary contraction and twitching of muscles).
- Headache. The development of a sharp and intense pain syndrome is characteristic.
- Possible loss of coordination (wobbly gait, loss of balance).
- Throbbing inside the head, feeling of heaviness or squeezing.
- Hallucinations.
- Confusion.
- Fainting.
- Decreased visual and hearing acuity.
- Numbness of the limbs or certain parts of the body.
- Memory impairment.
- Noise in ears.
- Tremor of hands and head.
- Sleep disturbance.
- Speech impairment.
- Development of paralysis and paresis.
As the disease progresses, general cerebral symptoms develop, which are associated with secondary hydrocephalus (impaired outflow of cerebrospinal fluid).
With a frontal lobe cyst, the following symptoms may develop:
- decrease in intellectual level;
- talkativeness;
- gait disturbance;
- speech becomes slurred;
- the lips are drawn out in the shape of a tube.
With an arachnoid cyst of the cerebellum, the following symptoms are noted:
- hypotonia of muscles;
- disorders of the vestibular apparatus;
- unsteadiness of gait;
- involuntary eye movements;
- development of paralysis.
It is worth noting that a cerebellar cyst can be a rather dangerous neoplasm.
An arachnoid neoplasm at the base of the brain can provoke the development of the following symptoms:
- dysfunction of the visual organs;
- strabismus;
- inability to move the eyes.
Congenital arachnoid formation in children can cause the following symptoms:
- pulsation of the fontanel;
- decreased tone of the limbs;
- disoriented look;
- profuse regurgitation after feeding.
An arachnoid cyst of the posterior cranial fossa provokes the development of the following symptoms:
- constant headache;
- paralysis of one half of the body;
- mental disorders;
- frequent and severe cramps.
A temporal lobe cyst is characterized by the development of symptoms of “frontal psyche”: patients are not critical of their own well-being, tearfulness develops, and auditory and visual hallucinations appear.
During a routine examination by a doctor, it is impossible to detect an arachnoid tumor. Symptoms can only indicate the development of pathological formations, and therefore will be a reason for conducting a hardware examination:
- MRI or CT. They allow you to determine the presence of a cyst, evaluate its size and location.
- Angiography with contrast. Helps to exclude the presence of malignant tumors - cancer is capable of accumulating contrast agents.
- Blood test for infections.
- Determination of cholesterol levels in the bloodstream.
- Doppler ultrasound, which allows you to assess the patency of blood vessels.
- ECG and ultrasound of the heart. The development of heart failure can provoke deterioration of cerebral circulation.
Types and symptoms of pituitary adenoma of the brain
Frozen formations: arachnoid cyst of the left temporal lobe, cyst of the hippocampus, posterior cranial fossa, base of the brain, cerebellum do not require treatment and do not cause pain. However, patients need to determine the underlying causes to prevent the development of new formations.
Conservative treatment of an arachnoid cyst of the head is required only for a progressive type of formation. Medicines are prescribed to relieve inflammation, normalize cerebral circulation, and restore damaged neurons. The duration of the course is determined individually.
- Longidaz, Caripatin for resorption of adhesions;
- Actovegin, Gliatilin to restore metabolic processes in tissues;
- Viferon, Thymogen to normalize immunity;
- Pyrogenal, Amiksin - antiviral drugs.
Surgical treatment of arachnoid formation begins only when conservative methods are ineffective. There are the following indications for surgical intervention:
- risk of educational disruption;
- mental state disorder;
- frequent convulsions and epileptic seizures;
- increased intracranial pressure;
- increased focal symptoms.
The following methods of surgical therapy are used for arachnoid cystic formations:
- Drainage. The needle aspiration method allows you to effectively remove fluid from the cerebrospinal fluid tumor of the left and right lobes.
- Shunting. The technique involves draining the formation to ensure the outflow of fluid.
- Fenestration. It involves excision of a pathological formation using a laser.
- Trepanation of the skull. This is a radical and effective procedure. The method is highly traumatic and can therefore lead to dangerous consequences.
- Endoscopy. This is a low-traumatic technique that allows you to remove the contents of the cystic cavity through punctures.
Prevention of primary arachnoid formation involves maintaining a healthy lifestyle by the woman during pregnancy. To prevent the development of secondary formations you need:
- maintain normal cholesterol levels;
- monitor blood pressure levels;
- the development of infectious or autoimmune diseases requires timely treatment;
- Monitor your well-being after a brain injury.
Arachnoid cyst is a dangerous disease that has serious consequences if left untreated. If the patient consults a doctor immediately after identifying the tumor and adheres to all recommendations, then the prognosis is optimistic.
Otherwise, a cerebrospinal fluid cyst of the right temporal lobe, an arachnoid cyst of the pineal gland or another part of the brain will eventually cause unpleasant symptoms, complications (convulsions, epilepsy, loss of sensitivity), and death.
The exact causes have not been identified. A subarachnoid cyst is most often a congenital pathology of the cerebrospinal fluid circulation system. The walls of the voluminous neoplasm are represented by the tissue of the arachnoid membrane, the contents are cerebrospinal fluid or a fluid similar in composition.
A congenital arachnoid cyst formed in the brain is considered true and belongs to the primary form of pathology. According to the results of ultrasound diagnostics during the perinatal period, cystic cavities in the fetal brain are formed during the 20-30 week of development. Secondary liquor cysts appear in the head due to various reasons:
- Past diseases of infectious etiology (meningitis, encephalitis).
- Surgery in the head area.
- Traumatic brain injuries.
- Agenesis (loss of the ability to fully develop) of the corpus callosum.
- Marfan syndrome. A genetically inherited disease characterized by dysplasia (improper formation) of connective tissue.
Arachnoid changes of a liquorocystic nature are a pathological process that is not accompanied by a change in tissue structure at the cellular level, which confirms the non-tumor nature of the neoplasm. Surgical removal of the cystic formation or its contents is indicated in the presence of neurological symptoms and the absence of therapeutic results after conservative treatment.
Diagnostic methods
Due to the fact that arachnoid changes are usually asymptomatic, diagnosis is carried out only when one or more alarming signs appear.
Usually the doctor prescribes several procedures:
- MRI or CT. They allow you to prove the presence of a cyst, determine its size and location.
- Angiography using a contrast agent. Proves or disproves the presence of cancer cells.
- Blood test for infectious diseases.
- Cholesterol level analysis.
- Dopplerography. This is the study of the patency of blood vessels. Shows whether there are any disturbances in the blood circulation process.
- Electrocardiogram and ultrasound of the heart. Irregularities in the functioning of the heart can provoke deterioration of blood circulation in the brain.
To diagnose an arachnoid cyst in young children, an examination is carried out by a neurologist, ophthalmologist, pediatrician and geneticist. Specialists conduct an external examination of the child, assess his behavior and general condition.
If necessary, infants and infants are prescribed NSG or neurosonography, spiral computed tomography and MRI. The latter procedure makes it possible to determine the presence of concomitant pathologies, in particular, hydromyelia or Arnold-Chiari syndrome.
Based on the results of the examination, a treatment plan is drawn up.