The site provides reference information for informational purposes only. Diagnosis and treatment of diseases must be carried out under the supervision of a specialist. All drugs have contraindications. Consultation with a specialist is required!
Necrosis of brain tumors usually occurs as a result of exposure of the tumor itself to radiation therapy, which is necessary to destroy it.
What to expect from brain tumor necrosis? If radiation therapy treatment is successful, then it is possible that some living brain tissue will still remain. This is not yet a reason for joy, since in such cases patients regularly suffer from very severe headaches. In addition, they also experience very frequent convulsive conditions. You can still live with this. In the worst case, this pathology can cause death of the patient.
Most often, this disease makes itself felt only half a year after radiation therapy. In very rare cases, this pathology develops in a cancer patient after several years. If the patient feels normal, then after a certain period of time it is still possible to get rid of necrosis. This can only be done through surgery, which is why patients with severe cancer cannot undergo such operations. There are also situations when surgical intervention is simply necessary, since without it the patient’s general condition cannot be improved in any way. In general, cases are actually different.
Why does necrosis still occur during radiation therapy? The fact is that this treatment method has a destructive effect on the blood-brain barrier. As a result, a fairly large amount of fluid begins to accumulate in the brain area, which prevents blood from flowing normally into this area. Since there is not enough oxygen, tissue necrosis begins.
Author: Pashkov M.K. Content Project Coordinator.
Brain death
- a condition when the death of the brain occurs, while with the help of resuscitation measures the function of the heart, blood circulation and respiratory activity are artificially maintained, creating the appearance of life. Currently, “brain death” is understood as a pathological condition associated with total necrosis of the brain, as well as the first cervical segments of the spinal cord, while maintaining cardiac activity and gas exchange, ensured by continuous artificial ventilation.
Brain death can be due to many reasons, including brain injury, intoxication, and swelling of the brain due to other causes.
Necrosis of the first cervical segments is caused by cessation of blood circulation through the vertebral artery system.
The actual synonym for brain death is the concept of “exorbitant coma,” the treatment of which is meaningless. A patient who is declared brain dead is actually a “living corpse.” In the practice of pathologists, the term “respiratory brain” is sometimes used. The condition must be distinguished from a chronic vegetative state.
What is atrophy that occurs in the brain
Atrophic changes occurring in the brain look like a compensatory increase in the volume of cerebrospinal fluid against the background of a decrease in the proportion of neurons (brain parenchyma).
The condition resembles hydrocephalus with the difference that it does not reflect a focal loss of tissue volume, but progressive pathological changes in them. Grade 1 atrophy occurring in the brain is characterized by the absence of pronounced symptoms. A person may experience headaches, be depressed, emotionally unstable, become irritable and tearful. Copes with the usual tasks of professional activity and lives a full life.
Neurological symptoms are more pronounced - motor dysfunction, movement coordination disorder. Pathological processes lead to inevitable and irreversible dementia. The third degree is accompanied by death - necrosis of areas of gray and white matter from which the brain is built.
- incoherent, uninformed speech;
- loss of professional skills;
- loss of orientation within space and time period;
- loss of self-service skills.
The number of complaints about poor health decreases as the destructive processes of cortical atrophy increase. This is an alarming signal indicating a deterioration in the adequate perception of one’s own physical and mental state.
Symptoms of radiation necrosis
It is necessary to understand that radiation necrosis is a long-term complication of radiotherapy, the development of which often occurs months, or even years, after completion of treatment with ionizing radiation. It most often appears between 6 months and 2 years after completion of the last course of radiotherapy.
In modern medical literature, there are data on the incidence of radiation necrosis, which are characterized by significant variability - from 5% to 37% of all patients receiving radiotherapy for intracranial tumors.
However, some authors report that up to 10% of all cases of this complication of radiotherapy were asymptomatic and the detection of radiation necrosis in such cases is entirely due to progress in neuroimaging methods. Attending physicians need to take into account the possible absence of symptoms of radiation necrosis in patients, despite the development of the pathological process.
In cases where the development of radiation necrosis is nevertheless accompanied by symptoms, patients most often experience the following symptoms:
- headache;
- nausea;
- cognitive impairment;
- seizures;
- focal neurological symptoms associated with the localization of the necrosis focus;
- personality change;
- apathy;
- hemiparesis.
Cerebral hemorrhages during radiation necrosis are a rare phenomenon, but, nevertheless, encountered in the practice of neuro-oncologists.
Causes of the disease
Understanding the topic of what atrophy that occurs in the brain is, it should be noted that this is always a secondary diagnosis that develops against the background of long-term damaging effects on the central nervous system. Doctors name several reasons why brain cells die:
- Genetic predisposition. The most important factor.
- Intoxication of the body, repeated with high frequency, associated with the use of alcoholic beverages and drugs.
- Injuries to the skull and soft tissues inside the skull.
- Insufficient blood supply to tissues, cerebral ischemia.
- Chronic anemia – insufficient oxygen supply. The condition occurs as a result of low concentrations of hemoglobin protein and red blood cells in the blood, which deliver oxygen to the tissues.
- Infections that affect the nervous system - polio, meningitis, Kuru disease, leptospirosis, brain tissue abscess.
- Diseases of the cardiovascular system - ischemia of the heart muscle, heart failure, atherosclerotic vascular pathologies.
- Decortication due to coma.
- Intracranial pressure. It is often the cause of cerebellar atrophy in newborns.
- Large tumors that compress surrounding tissues and interfere with normal blood supply to parts of the brain.
- Cerebrovascular disease is destructive changes in the vessels located in the brain.
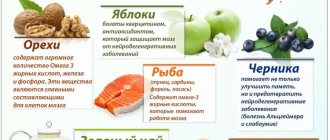
If a person avoids mental activity, the risk of developing atrophic diseases occurring in the brain increases. Among the factors that increase the likelihood of the death of neurons located in the brain are smoking, low mental stress, chronic arterial hypertension, hydrocephalus, and long-term use of drugs that constrict blood vessels.
At this stage, medicine is unable to answer the question of why the destruction of neurons begins, however, it has been found that the predisposition to the disease is inherited, and birth injuries and intrauterine diseases also contribute to its formation. Experts share congenital and acquired causes for the development of this disease.
Congenital causes:
- genetic predisposition;
- intrauterine infectious diseases;
- genetic mutations.
One of the genetic diseases that affects the cerebral cortex is Pick's disease. Most often it develops in middle-aged people and is expressed in the gradual damage of neurons in the frontal and temporal lobes. The disease develops rapidly and leads to death within 5-6 years.
Infection of the fetus during pregnancy also leads to the destruction of various organs, including the brain. For example, infection with toxoplasmosis in the early stages of pregnancy leads to damage to the nervous system of the fetus, which often does not survive or is born with congenital abnormalities and mental retardation.
Acquired causes include:
- drinking large amounts of alcohol and smoking lead to cerebral vascular spasm and, as a result, oxygen starvation, which leads to an insufficient supply of nutrients to the cells of the white matter of the brain, and then their death;
- infectious diseases that affect nerve cells (for example, meningitis, rabies, polio);
- injuries, concussions and mechanical damage;
- a severe form of renal failure leads to general intoxication of the body, as a result of which all metabolic processes are disrupted;
- external hydrocephalus, expressed in an increase in the subarachnoid space and ventricles, leads to atrophic processes;
- chronic ischemia causes vascular damage and leads to insufficient supply of neural connections with nutrients;
- atherosclerosis is expressed in a narrowing of the lumen of veins and arteries, and as a result, an increase in intracranial pressure and the risk of stroke.
Atrophy of the cerebral cortex can be caused by insufficient intellectual and physical activity, lack of a balanced diet and poor lifestyle.
The main factor in the development of the disease is a genetic predisposition to the disease, but various injuries and other provoking factors can accelerate and provoke the death of brain neurons. Atrophic changes affect different areas of the cortex and subcortical substance, however, with all manifestations of the disease, the same clinical picture is observed.
Atrophy of the frontal lobes of the brain can develop during intrauterine maturation or prolonged labor due to prolonged oxygen starvation, which causes necrotic processes in the cerebral cortex. Such children most often die in the womb or are born with obvious abnormalities.
The death of brain cells can also be triggered by mutations at the gene level as a result of exposure to certain harmful substances on the body of a pregnant woman and prolonged intoxication of the fetus, and sometimes it is simply a chromosomal malfunction.
At the initial stage, signs of brain atrophy are barely noticeable; only close people who know the patient well can detect them. Changes manifest themselves in the patient’s apathetic state, the absence of any desires and aspirations, lethargy and indifference appear. Sometimes there is a lack of moral principles and excessive sexual activity.
Progressive death of brain cells symptoms:
- decrease in vocabulary; the patient takes a long time to find words to describe something;
- decrease in intellectual abilities over a short period;
- lack of self-criticism;
- loss of control over actions, body motor skills deteriorate.
Further atrophy of the brain is accompanied by a deterioration in well-being and a decrease in thought processes. The patient stops recognizing familiar things and forgets how to use them. The disappearance of one’s own behavioral characteristics leads to the “mirror” syndrome, in which the patient begins to unwittingly copy other people. Further, senile insanity and complete personality degradation develop.
Changes in behavior that appear do not allow an accurate diagnosis, therefore, to determine the reasons for changes in the patient’s character, it is necessary to carry out a series of studies.
However, under the strict guidance of the attending physician, it is possible to determine with a greater probability which part of the brain has undergone destructuring. So, if destruction occurs in the cortex, the following changes are distinguished:
- decreased thought processes;
- distortion in speech tone and voice timbre;
- change in the ability to remember, up to complete disappearance;
- deterioration of fine motor skills of the fingers.
The symptoms of changes in the subcortical substance depend on the functions that the affected part performs, so limited brain atrophy has characteristic features.
Necrosis of medulla oblongata tissue is characterized by respiratory failure, digestive failure, and human cardiovascular and immune systems are affected.
When the cerebellum is damaged, there is a disorder of muscle tone and incoordination of movements.
When the midbrain is destroyed, a person stops responding to external stimuli.
The death of cells in the intermediate section leads to disruption of body thermoregulation and metabolic failure.
Damage to the anterior part of the brain is characterized by loss of all reflexes.
The death of neurons leads to the loss of the ability to independently support life and often leads to death.
Sometimes necrotic changes are the result of injury or long-term poisoning with toxic substances, resulting in restructuring of neurons and damage to large blood vessels.
Radiation necrosis: symptoms, diagnosis, treatment methods
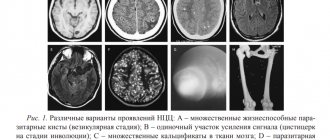
Radiation necrosis , which is a focal structural lesion at the site of the tumor, is a long-term complication of the central nervous system (CNS) after radiotherapy or radiosurgery.
Tissue swelling and the presence of a neoplasm cause changes in the parenchyma of the central nervous system organs located in the tumor bed, which increase the likelihood of developing radiation necrosis. Radiation necrosis can occur when radiotherapy is prescribed for primary central nervous system neoplasms, metastatic brain lesions, or head and neck tumors. Radiation necrosis can occur following any use of ionizing radiation to treat tumors or any protocol for such treatment.
Diagnosis of radiation necrosis and its treatment pose significant difficulties, since the manifestations of this complication of radiotherapy are often overlapped by symptoms of tumor recurrence. An erroneous diagnosis (recurrence of a tumor instead of radiation necrosis) can lead to the prescription of incorrect treatment, which can pose a danger to the patient’s life.
Types of pathology
The generalized form of cerebral atrophy involves multiple areas of nerve cells in the brain tissue. Diffuse brain atrophy is the uniform death of neurons in all areas of the brain structures. It develops as a result of arterial hypertension, which is characterized by damage to small vessels located in each part of the brain.
The initial symptoms of diffuse atrophy resemble dysfunction of the cerebellum. The progressive course leads to a rapid increase in symptoms, which makes it possible to differentiate the pathology at later stages. Unlike the cortical type, with diffuse atrophy the symptoms of damage to the controlling, dominant hemisphere are clearly expressed. With cortical subatrophy occurring in the brain, destruction and tissue destruction are only just beginning.
Subatrophy, which occurs in the brain, is a condition that precedes the stage of neuronal death. The mechanism of the disease has already been launched, destructive processes have begun, but the body independently compensates for the violations that have arisen. Subatrophic changes are accompanied by mild symptoms. Bihemispheric cortical atrophy occurs in the tissues of both hemispheres. Manifested by Alzheimer's syndrome.
Organic damage to the structures of the brain matter, which develops against the background of constant exposure to ethanol, is called toxic encephalopathy. Affects all parts of the brain. The cortical layers and cerebellum are especially sensitive to the negative effects of alcohol. Often leads to cranial nerve palsy. The frontal lobes are responsible for behavior, intelligence, emotions and moral qualities - properties that characterize a conscious personality.
Developing pathology causes atrophic changes in tissues and is one of the main causes of dementia. Dementia, as a consequence of alcoholism, is diagnosed in 10-30% of patients who abuse alcoholic beverages. A person becomes infantile and loses the ability for abstract logical thinking.
Covers multiple areas - the cerebellum, basal ganglia, spinal cord. If we understand in detail the topic of what atrophic degenerative changes are that affect the brain in a multisystem form, it is worth noting the progressive course, cerebellar ataxia (motor dysfunction) and autonomic failure syndrome.
Cortical atrophy is expressed by the death of neurons located in cortical structures in the frontal lobe. The frontal lobes are responsible for speech function, emotional behavior, determine personal characteristics, regulate human motor activity - planning and execution of voluntary movements. Cortical atrophy occurring in the brain negatively affects these abilities.
Atrophy of the cortex and frontal areas of the brain is predominantly associated with age-related destructive changes in tissues. Signs indicating cortical atrophy are behavioral disturbances and loss of intellectual abilities. With cerebral atrophy of the 1st degree cortical type, the patient is characterized by unmotivated actions that do not comply with generally accepted ethical standards.
A person cannot explain the reasons or assess the consequences of his actions. A characteristic sign that indicates atrophy affecting the frontal lobes of the cerebral hemispheres is regressive changes and personality degradation. Cognitive abilities decrease, the ability to think, remember, and concentrate is lost.
The cerebellum is the department responsible for motor coordination. Destructive changes are manifested by malfunctions of the musculoskeletal system, imbalance, disorders of swallowing functions and eye control. The tone of the skeletal muscle corset decreases. It is difficult for a person to keep his head straight. Enuresis is often observed.
Classification
According to the international classification, atrophic lesions are divided according to the severity of the disease and the location of the pathological changes.
Each stage of the disease has special symptoms.
Atrophic diseases of the brain of the 1st degree or subatrophy of the brain are characterized by minor changes in the behavior of the patient and quickly progress to the next stage. At this stage, early diagnosis is extremely important, since the disease can be temporarily stopped and how long the patient lives will depend on the effectiveness of treatment.
Stage 2 of the development of atrophic changes is manifested in a deterioration in the patient’s communication skills, he becomes irritable and unrestrained, and the tone of speech changes.
Patients with degree 3 atrophy become uncontrollable, psychosis appears, and the morality of the patient is lost.
The last, 4th stage of the disease, is characterized by a complete lack of understanding of reality by the patient; he stops responding to external stimuli.
Further development leads to complete destruction; vital systems begin to fail. At this stage, hospitalization of the patient in a psychiatric hospital is highly advisable, as it becomes difficult to control him.
Classification according to the location of the affected cells:
- Cortical atrophy most often develops in older people and lasts as long as a person lives, affecting the frontal lobes;
- Diffuse atrophy of the brain is accompanied by impaired blood supply, atherosclerosis, hypertension and decreased mental abilities. Stage 1 of this form of the disease most often develops in the cerebellum, and then affects other parts of the brain;
- Multiple system atrophy develops as a result of mutations and gene disorders during pregnancy. In this form of the disease, not only the brain is affected, but also other vital systems. Life expectancy directly depends on the degree of mutation of the entire organism and its viability;
- Local brain atrophy of the 1st degree appears as a result of mechanical lesions, strokes, focal infections and parasitic inclusions. Symptoms depend on which part is damaged;
- The subcortical or subcortical form of the disease is an intermediate condition in which the centers responsible for speech and thought processes are damaged.
Brain atrophy in children
Depending on the age at which brain atrophy begins, I distinguish between congenital and acquired forms of the disease. The acquired form of the disease develops in children after 1 year of life.
The death of nerve cells in children can develop for various reasons, for example, as a result of genetic disorders, different Rh factors in mother and child, intrauterine infection with neuroinfections, prolonged fetal hypoxia.
As a result of the death of neurons, cystic tumors and atrophic hydrocephalus appear. Depending on where the cerebrospinal fluid accumulates, cerebral hydrocele can be internal, external or mixed.
A rapidly developing disease most often occurs in newborns, in which case we are talking about serious disorders in the brain tissue due to prolonged hypoxia, since the child’s body at this stage of life is in dire need of intensive blood supply, and a lack of nutrients leads to serious consequences .
When asked whether a child’s brain matter can atrophy, doctors give an affirmative answer. Atrophy that affects the brain in recently born children is often a consequence of birth injuries and abnormalities in the intrauterine development of the nervous system. It is diagnosed in the early stages of life - usually in the first weeks and months. They are treated with medications, physiotherapeutic and sedative procedures. The prognosis is unfavorable.
Symptoms
Initial signs of atrophy affecting the tissues and structures of the brain usually appear in people over 45 years of age. Pathology is more often diagnosed in female patients. Characteristic symptoms:
- Changing personality type. Apathy, indifference, narrowing of interests.
- Psycho-emotional disorder. Mood swings, depression, increased irritability.
- Impaired memory function.
- Reducing vocabulary.
- Motor dysfunction, impaired coordination of movements and fine motor skills.
- Deterioration of mental activity.
- Decreased performance.
- Epileptic seizures.
The body's regenerative reactions weaken. Reflexes are depressed. Symptoms become brighter and more expressive. Atrophic changes are manifested by Parkinson's and Alzheimer's syndrome. The following signs indicate a specific affected area:
- Medulla. Deviations in the functioning of the respiratory, digestive, and cardiovascular systems. Defense reflexes are suppressed.
- Cerebellum. Weakness of skeletal muscles, malfunctions of the musculoskeletal system.
- Midbrain. Inhibited or absent reactions to external stimuli.
- Diencephalon. Pathological deviations in the functioning of the thermoregulation system, disruption of the hemostatic and metabolic systems.
- Frontal lobes. Secrecy, aggression, demonstrative behavior.
Signs such as impulsiveness, previously unusual rudeness, increased sexuality, decreased self-control, and apathy indicate malfunctions in the functioning of the main organ of the central nervous system.
What atrophies does the brain undergo?
Subatrophic changes in the brain precede global neuronal death. At this stage, it is important to diagnose brain disease in a timely manner and prevent the rapid development of atrophic processes.
For example, with hydrocephalus of the brain in adults, the free voids released as a result of destruction begin to be intensively filled with released cerebrospinal fluid. This type of disease is difficult to diagnose, but proper therapy can delay further development of the disease.
Changes in the cortex and subcortical substance can be caused by thrombophilia and atherosclerosis, which, in the absence of proper treatment, first cause hypoxia and insufficient blood supply, and then the death of neurons in the occipital and parietal zone, so treatment will consist of improving blood circulation.
Brain neurons are sensitive to the effects of alcohol, so drinking alcohol-containing drinks initially disrupts metabolic processes and addiction occurs.
Alcohol breakdown products poison neurons and destroy neural connections, then gradual cell death occurs and, as a result, brain atrophy develops.
As a result of the destructive effect, not only the cortical-subcortical cells suffer, but also the fibers of the brain stem, blood vessels are damaged, neurons shrink and their nuclei are displaced.
The consequences of cell death are obvious: over time, alcoholics lose their sense of self-esteem and their memory decreases. Further use entails even greater intoxication of the body, and even if a person comes to his senses, he still later develops Alzheimer's disease and dementia, since the damage done is too great.
Use of medications
Many studies have been conducted on the effectiveness of drugs in parallel with the use of radiotherapy, which provides the opportunity to recover.
- The administration of radioprotectors helps protect healthy tissues during the irradiation procedure; The administration of radiosensitizers increases the sensitivity of educational cells to the effects of radiation;
The use of these drugs makes it possible to deliver the required amount of radiation to the tumor without affecting healthy cells.
Types of diagnostics
Brain atrophy is diagnosed using instrumental analysis methods.
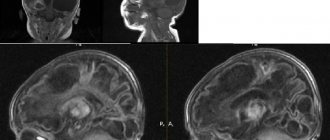
Magnetic resonance imaging (MRI) allows you to examine in detail changes in the cortical and subcortical substance. Using the obtained images, it is possible to accurately make an appropriate diagnosis already in the early stages of the disease.
Computed tomography allows us to examine vascular lesions after a stroke and identify the causes of hemorrhage, determine the location of cystic formations that interfere with normal blood supply to tissues.
The newest research method - multislice tomography allows you to diagnose the disease at an early stage (subatrophy).
To determine after which cases of atrophied areas of brain tissue appear, diagnostic studies are prescribed. The difficulty of diagnosing in the early stages prevents correct, timely treatment and full restoration of functions. During the examination, the doctor determines the level of reflexes and reactivity - the ability to respond to external stimuli. Instrumental and hardware methods:
- MRI, CT. Allows you to identify cystic and tumor formations, hematomas, and local lesions.
- Ultrasound, neurosonography - in newborns.
- Dopplerography. Reveals the condition and patency of elements of the vascular system.
- Angiography is an X-ray examination of blood vessels.
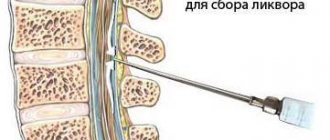
Neurophysiological studies, including electroencephalography (determining the degree of brain activity), rheoencephalography (determining the state of cerebral circulation), diagnostic punctures, are carried out to identify the causes that led to damage to the cells that make up the brain tissue.
Radiation necrosis: treatment
For effective treatment of radiation necrosis, a correct diagnosis is of paramount importance, since an erroneous diagnosis of tumor recurrence and subsequent antitumor treatment can lead to undesirable severe consequences.
For patients without symptoms of radiation necrosis in whom a necrotic mass is detected by MRI during follow-up, a wait-and-see approach may be chosen. If the choice of treatment strategy does not depend on whether the patient has radiation necrosis or recurrent glioma, the patient's condition should be monitored using serial MRI.
However, treatment tactics should be different in the presence of symptoms such as space-occupying syndrome in the cranial cavity, increased intracranial pressure, and neurological disorders. In such cases, it is possible to use the following treatment methods (separately or in combination):
- administration of corticosteroids;
- if steroids are ineffective, the use of bevacizumab (a monoclonal antibody that selectively binds to and neutralizes biologically active vascular endothelial growth factor (VEGF) may be considered);
- hyperbaric oxygen therapy (oxygen supply under pressure of 2-3 atm. Per course of treatment: 20-30 sessions lasting 90-120 minutes each).
Surgical treatment of radiation necrosis has its advantages and disadvantages. Removal of the necrotic mass helps to quickly reduce increased intracranial pressure and restore neurological functions. However, such an operation is associated with a risk of serious complications and is performed mainly on patients in whom conservative treatment has failed.