Reactive meningitis is an extremely dangerous infectious disease that affects the spinal cord and brain. This type of inflammation can affect children born prematurely, as well as people with head injuries and disorders of the nervous system.
The danger of the pathology is explained by the fact that symptoms arise unexpectedly and develop rapidly. It is important to start treatment on the first day after the appearance of characteristic signs, but even in this case there is no guarantee that the person can be saved.
Causes
Why does reactive meningitis occur, and what is it? The causative agents of this infectious disease can be various pathogenic organisms, such as staphylococcus, meningococcus, Pseudomonas aeruginosa and others.
The routes of infection are as follows:
- Hematogenous - from inflammatory foci, the pathogen is carried into the brain with the blood.
- Contact – skull injury with infection.
- Airborne - when a carrier of infection or a sick person coughs and sneezes.
- Perineural – transfer of infection to brain tissue during inflammation of the nerves.
- Transplacental - through the placenta to the fetus from the mother.
- Lymphogenic – transfer of infection to the brain through the lymphatic system.
According to statistics, reactive meningitis most often develops as a secondary infection against the background of an existing meningococcal or streptococcal infection.
Complications and prognosis
Complications of the disease include such severe conditions as disseminated intravascular coagulation syndrome (DIC), sepsis, infectious-toxic shock, and hyponatremia. If treatment is not started promptly, symptoms such as deafness, blurred vision and paralysis may persist after the patient has recovered.
Complications of reactive meningitis cause death in 10% of cases. An unfavorable prognosis is observed with infection in childhood and old age. In these cases, it is rarely possible to stop the rapid development of meningitis. In middle-aged people, complete recovery is possible. If you follow preventive measures, especially vaccination, the likelihood of developing the disease is reduced several times.
Symptoms of reactive meningitis
Reactive meningitis develops at lightning speed (1-2 days). The rapid growth of purulent foci and cerebral edema with delayed help leads to the death of a person.
Characteristic signs of reactive meningitis are as follows:
- High body temperature (above 39 degrees) and severe chills. A characteristic feature of the disease is temperature fluctuations. In the first hours of the spread of infection, the temperature reaches 40 degrees, but is easily reduced by antipyretics. However, after a few hours, no medications have any effect.
- Intense headache, spreading all over the head, aggravated by movement, sudden noise or light stimulus.
- Debilitating vomiting not associated with food intake. It occurs from the first hours of the disease and is extremely painful for the patient.
- Some patients may experience cramps, muscle pain, and severe weakness.
- Signs of shock: tachycardia, arterial hypotension, cold skin at high body temperature, the patient’s feet and hands acquire an ashy hue.
- The patient's hands and feet become gray.
- Excitement and anxiety that appear in the first hours of the illness are replaced by confusion, prostration and coma. Shortness of breath, hypoxemia, oliguria, and other manifestations of respiratory distress syndrome occur.
- Some patients develop a maculopapular rash, which after some time becomes hemorrhagic. Most often it is localized in the area of large joints, on the buttocks, and on the hind limbs. However, it can appear in other places.
- DIC syndrome develops in the absence of adequate treatment and an increase in the manifestations of septic shock. In this case, the rash becomes necrotic, confluent in nature, collaptoid spots appear, gangrene of the toes and hands develops, hemorrhages occur in the sclera, oral mucosa, conjunctiva, the patient’s death occurs from multiple organ failure and refractory septic shock.
In most patients, death with reactive meningitis occurs as a result of refractory septic shock and multiple organ failure.
What kind of disease is this and what is its danger?
Reactive infectious meningitis occurs differently in each patient. There are chronic and acute development of the disease. The fulminant form of pathology is the most dangerous disease, posing a real threat to human life and health.
In the absence of proper treatment, the patient falls into a coma and dies due to numerous purulent formations in the brain. Only timely diagnosis will help provide medical care in the initial stages of development of fulminant meningitis.
Only 90% of patients are able to completely recover from this form of inflammation of the brain and spinal cord, but most suffer from various complications.
Diagnostics
An accurate diagnosis of reactive meningitis can be made using a lumbar puncture. This is the only way to distinguish it from other diseases with a similar clinical picture. Meanwhile, this procedure takes a lot of time, which an infected person often does not have.
In addition to cerebrospinal fluid examination, common methods for diagnosing reactive meningitis are:
- fundus examination;
- electroencephalography;
- radiography of the skull;
- nuclear magnetic resonance and computed tomography.
In general, the diagnosis of meningitis can only be made if the patient has three main signs of the disease.
Consequences
Fleet meningitis is a serious disease that is fatal for many who become infected. Timely recognition and intensive therapy are not in all cases able to avoid the severe consequences of this disease.
The infected person's sodium ion concentration immediately decreases. Poor blood clotting is observed. The patient is developmentally delayed, has poor hearing and poor vision. Septic shock and paralysis may occur.
Even if treatment is started at the first stage of the disease, the result is rarely positive.
What are the dangers of bacterial meningitis?
- Svetlana Aleksandrovna Kiseleva
- March 26, 2020
Children and older people have weak bodies, so the prognosis for them is often unsatisfactory. The disease progresses very quickly. Timely assistance in the form of therapeutic treatment does not always save from a fatal outcome.
Treatment is more successful in middle-aged patients. A correct diagnosis can be the key to a quick recovery.
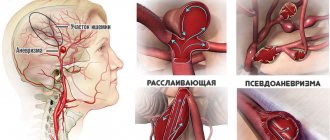
Disseminated intravascular coagulation syndrome is a mortal danger for those infected with reactive meningitis. As a result, blood clots merge in many vessels. Blockage of the blood supply can lead to the death of many organs. When blood vessels rupture, hemorrhages occur in the brain.
How to treat reactive meningitis
A person with meningeal symptoms should be hospitalized immediately.
For reactive meningitis, treatment must be immediate and intensive, otherwise death cannot be avoided. Because there is no time to determine the sensitivity of microflora, antibacterial drugs are prescribed empirically, choosing groups that can affect all possible microbes - penicillins, cephalosporins, macrolides. As the severity of the patient's condition increases, antimicrobial agents are injected directly into the spinal canal.
When convulsions and muscle spasms occur, antispasmodics and muscle relaxants are used. When adrenal function decreases, glucocorticoids are prescribed. To prevent cerebral edema, furosemide is administered. When swelling has already formed, it is necessary to prescribe sorbilact. In addition, the patient will be given intravenous plasma substitutes, saline solutions, and antipyretics.
Reactive meningitis is an extremely dangerous disease, the prognosis for which in most cases is unfavorable. Only timely and intensive treatment can avoid death; in children and the elderly, the progression is so rapid that medicine is often powerless.
Traditional medicine recipes for meningitis
It is impossible to cure this form of pathology at home without medical help. Lack of adequate and correct drug therapy can lead to death. Traditional medicine recipes can only be used as an additional treatment, and after the patient’s condition has normalized, acute inflammation of the brain has been eliminated.
A tincture of peppermint or lavender leaves is the best anticonvulsant. Simple recipes will help you cope with migraine attacks and irritability due to an infectious disease:
- A decoction of herbal tea: rosemary, lavender, primrose root, valerian, peppermint, pour boiling water over the leaves, bring to a boil, leave and filter.
- Infusion of linden flowers.
- A decoction of strong green tea with rose hips.
Before using traditional medicine, you should consult a doctor. Only a specialist can decide on the advisability of using a particular recipe.
Health care
Treatment of reactive meningitis is carried out only in a hospital, most often in the intensive care unit. For small patients and adults, the principle of treatment is almost the same; there may only be prescriptions of different groups of antibiotics, but this depends on the patient’s well-being and his body’s reaction to the drug. Young patients always have complications that occur immediately during illness or later.
The goal of therapy is to prevent sad consequences for the patient, as well as to begin treatment as early as possible.
Treatment with broad-spectrum antibiotics, in the highest possible doses, begins immediately. For this purpose, drugs from the groups of penicillins, cephalosporins and macrolides are used.
In 20% of cases, the cause of the disease is never identified, which is why antibiotics are immediately prescribed that act on all harmful microorganisms.
If the patient's condition worsens, the drug can be injected into the spinal canal. A course of antibiotics is prescribed for a period of at least 10 days, but if there are purulent lesions in the brain area, the course is extended.
If the drugs used: Penicillin, Ceftriaxone and Cefotaxime do not help, and the patient faces fatal complications, then Vancomycin and Carbapenem, which have serious side effects, are used.
In addition, therapy is carried out to relieve symptoms with the following drugs:
- antispasmodics and muscle relaxants - relieving cramps and spasms in muscles;
- glucocorticoids – improving the functioning of the adrenal glands;
- Furosemide – prevention of cerebral edema;
- Sorbilact - if there is already swelling;
- for general therapy, saline solutions, plasma expanders, and antipyretics are administered using droppers.
In the first hours of treatment, all drugs are administered intravenously - this is how the medicine acts most effectively, helping to avoid toxic shock. It is timely treatment that will help to cope with the disease without serious consequences for the patient.
Before the ambulance arrives, the patient must be provided with physical and mental peace and maximum comfort, because all his senses are heightened.
It is necessary to close the windows with curtains, isolate from noise and screaming, to reduce pain, put ice or rags soaked in cold water on the head, arms to the elbows and legs to the knees, changing them as they warm up. The patient can be given a medication for headaches.
Signs of pathology
This life-threatening disease, like other disorders, has its own characteristic symptoms. For the reactive type of disease, the distinctive feature remains the speed of development of symptoms.
The first clinical signs include:
- clouding of consciousness;
- increased body temperature;
- drowsiness;
- fatigue;
- fever;
- muscle weakness;
- urge to vomit and nausea;
- severe headaches radiating to the back and cervical spine;
- increased sensitivity to light;
- heart rhythm disturbance;
- shortness of breath;
- paresis of limbs;
- hearing and visual impairment;
- skin manifestations.
For infants, a symptom of meningitis is also swelling and tension in the area of the large fontanel.
Headaches that occur when the membranes of the brain are damaged do not go away when taking medications. Posture, which is also a kind of sign of meningitis, helps relieve pain. If you feel better with your head thrown back and your knees bent and pressed to your stomach, you can assume that the person has infectious reactive meningitis.
Development mechanism and reasons
The opinion has become firmly established among the population that reactive meningitis is one that is characterized by an extremely rapid development of the clinical picture. In fact, such meningitis is called fulminant, or fulminant.
Reactive meningitis is one that occurs in response to something.
The mechanism of development of reactive meningitis is based on:
- autoimmune processes;
- aseptic inflammation;
- allergic reactions;
- damage to the vessels of the membranes by bacterial waste products.
There are many causes of reactive meningitis. The main ones include:
- medications administered endolumbarally, that is, into the spinal canal;
- toxoplasmosis, syphilis, leptospirosis, tuberculosis and other diseases in which microorganism toxins irritate the meninges;
- vaccination;
- malignant neoplasms of the central nervous system;
- extensive ischemic strokes;
- subarachnoid hemorrhages;
- rupture of echinococcal cysts;
- breakthrough of a purulent abscess into the subarachnoid space.
Methods of transmission
Fulminant meningitis has a number of methods of disease transmission:
- airborne;
- contact;
- hematogenous;
- perineural;
- transplacental;
- lymphogenous.
8 types of brain meningitis
- Svetlana Aleksandrovna Kiseleva
- May 23, 2020
Reactive meningitis occurs as a result of spinal cord or traumatic brain injury. There are cases in which the disease progressed due to a skull fracture.
Infectious pathogens, once inside, provoke the process of inflammation of brain tissue. The resulting edema causes improper microcirculation in the cerebral vessels. Absorption of cerebrospinal fluid slows down. The infected person gradually begins to increase intracranial pressure. Dropsy of the brain is formed. Progressive disease allows the inflammatory process to spread to the roots of the cranial nerves.
How to protect yourself long before illness?
As such, there is no 100% effective prevention of this disease, since even vaccination does not give such a result, however, it significantly reduces the risk of the disease.
Following standard rules of behavior gives good results, in particular:
- personal and public hygiene,
- refraining from visiting crowded places during epidemiological periods,
- follow the recommendations of doctors when visiting meningitis-prone areas,
- If you have any doubts, consult a doctor immediately,
- Avoid contact with infected people.
So, reactive meningitis is an extremely dangerous and insidious disease, and neglecting a visit to the doctor or the desire to self-medicate can be fatal. Don’t risk your health and the health of your loved ones, take care of yourself!
Prevention measures
To protect yourself from reactive meningitis you must:
- get the appropriate vaccination;
- immediately treat any disease of an inflammatory nature;
- avoid contact with infected people;
- isolate infected people;
- carefully observe the rules of personal hygiene;
- be careful when in potentially dangerous areas.
Sources
- https://neuromed.online/reaktivnyy-meningit/
- https://NashiNervy.ru/infektsionnye-zabolevaniya/reaktivnyj-ili-skorotechnyj-meningit.html
- https://nevrology.net/sindromy-i-zabolevaniya/infektsionnye/reaktivnyj-meningit.html
- https://NeuroDoc.ru/bolezni/infekcii/reaktivnyj-meningit.html
- https://lechenie-simptomy.ru/reaktivnyj-meningit
- https://superlor.ru/bolezni/chto-takoe-reaktivnyy-meningit
- https://simptomy-lechenie.net/chto-takoe-reaktivnyj-meningit/
- https://nevralgia.ru/meningit/reaktivniy/
How does infection occur?
Reactive meningitis is a deadly disease in which the meninges become inflamed. The threat to life is especially high for children, the elderly and people with a low immune response. The disease is difficult to diagnose due to the rapid progression of the inflammatory focus, which puts a person into a coma within a few hours.
The main reason for the development of pathology is infection. The causative agents of the disease are staphylococci, meningococci and other pathogenic microorganisms. The infectious agent enters the body as follows:
- by airborne droplets, when a person inhales contaminated air while communicating with a carrier;
- by contact, in which pathogens settle on the skin and then penetrate the body;
- through food products containing pathogenic microorganisms.
If a person becomes infected in one of the described ways, primary meningitis is diagnosed. If the disease develops as a result of a complication of sore throat, pneumonia or other infections, then a secondary form of the disease is detected.
The airborne method of spreading infection often leads to epidemiological outbreaks.
When meningeal pathogens enter the body, inflammatory phenomena develop in the meninges. Then the brain swells, leading to disruption of the functioning of cerebral vessels. Due to decreased absorption of spinal fluid, intracranial pressure increases sharply, and hydrocephalus is diagnosed. As a result, the spinal and cranial nerve endings become inflamed.
The development of meningitis is also facilitated by head and back injuries, inflammatory diseases, and the presence of boils on the body.