Serous meningitis belongs to a number of infectious diseases of the nervous system of polyetiological origin. This means that its occurrence can be due to many reasons. Literally, serous meningitis implies an inflammatory process of the membrane of the brain or spinal cord and is characterized by the appearance of fluid of non-purulent origin.
This variant of the pathology has a more favorable course and prognosis than the purulent one. Since serous meningitis is classified as a polyetiological disease, it can be caused by many pathogens:
- Viruses such as enteroviruses, Echo or Coxsackie;
- Bacteria such as mycobacteria and spirochetes;
- Fungi of the genus Candida or Coccidioides immitis.
By origin, serous meningitis can be:
- Primary, when the pathogen directly affects the meninges;
- Secondary, in which the disease manifests itself as a complication of another infectious process.
Serous meningitis in adults occurs in people with immunodeficiencies, as it mainly affects children. Also, this disease is characterized by a seasonal process - mostly people get sick in the summer. A harmful agent can enter the body in the following ways:
- Airborne, when the pathogen penetrates through the air along with droplets of the patient’s saliva when coughing or sneezing, or when talking;
- Contact, through household items if personal hygiene rules are not observed;
- Water in case of swimming in contaminated places, drinking contaminated drinks with a pathogen.
How to analyze cerebrospinal fluid for meningitis, and what indicators should cerebrospinal fluid have
Meningitis is a dangerous brain disease that leads to disability and, in the absence of medical care, death. Since cerebrospinal fluid changes its properties during meningitis, the doctor, after examining it, can make an accurate diagnosis and immediately prescribe the necessary treatment. Cerebrospinal fluid is taken using a lumbar puncture (puncture). There is no need to be afraid of this procedure, because it helps you choose the most effective treatment method.
What is cerebrospinal fluid
Cerebrospinal fluid controls the functionality of the nervous system. To obtain it, the doctor performs a lumbar puncture on the patient. Functions of cerebrospinal fluid:
- protect the brain from damage and exposure to mechanical factors;
- maintain optimal pressure inside the skull;
- promote metabolic processes between the brain and the fluid environment of the body;
- evacuate metabolic products;
- maintain the functioning of parts of the brain.
The total volume of spinal fluid ranges from 140 to 270 cubic meters. cm . It is formed by secretion by cells located in the vascular connections of the ventricles of the brain. Approximately 700 cubic meters are produced every day. see cerebrospinal fluid.
Liquor in normal and pathological conditions
Liquor is a special cerebrospinal fluid that is produced by certain cells of the ventricular system of the brain and performs a number of important functions to ensure the full functioning of the central nervous system.
The main functions of cerebrospinal fluid include:
- Protective. Liquor can be called a “water shock absorber” in the cranium for the brain.
- Bactericidal. Cerebrospinal fluid contains white blood cells (neutrophils and lymphocytes), which are necessary to fight infectious agents.
- Energy. Transport of nutrients and energy substrates for brain cells occurs.
- Maintaining pH (acid-base balance), as well as osmotic pressure due to the content of electrolytes (Na, Cl, K, etc.) in the cerebrospinal fluid.
- Part of the blood-brain barrier.
- Oncotic pressure is maintained by proteins present in the cerebrospinal fluid.
Per unit time, the spinal cord and brain contain from 100 ml to 150 ml of cerebrospinal fluid, which is completely renewed in 3-4 hours. At a time, the ventricles of the brain contain from 40 ml to 50 ml of cerebrospinal fluid, and the subarachnoid spaces contain the remaining amount (100-150 ml). Continuous fluid exchange allows you to maintain a constant internal environment of the brain.
Normal indicators
Normally, cerebrospinal fluid has the following indicators:
- density - from 1.005 to 1.009;
- the pressure should be within 100-200 millimeters of water;
- there should be no coloring;
- cytosis (per 1 microliter): ventricular fluid - up to 1, cisternal fluid - up to 1, lumbar fluid - within 2-3);
- alkaline index - from 7.31 to 7.33;
- total protein - from 0.16 to 0.33 grams per liter;
- glucose indicator - from 2.8 to 3.9 mmol per liter;
- chlorine (ions) - 120-128 millimoles.
How to do a lumbar puncture
Meningitis is an absolute indication for lumbar puncture. This procedure is prohibited if:
- severe swelling of the brain tissue (the procedure can cause great harm);
- a sharp jump in cerebrospinal fluid pressure;
- the presence of a large formation inside the brain;
- dropsy.
Carrying out a puncture procedure for hydrocephalus and in the event of a pressure surge inside the skull can lead to a condition where a piece of brain tissue extends into the opening of the back of the head. At the same time, the work of the most important human life support centers is disrupted.
During the puncture, the person lies on his side, tilts his head to his chest and brings his legs bent at the knee joint to his stomach. This position ensures optimal accessibility at the puncture site. It is located between the 3rd and 4th vertebrae in the lower back. There is no longer a spinal cord in this place.
Alcohol is applied to the puncture site, and an anesthetic is injected under the skin. The skin is pierced with a special needle with a tip. If it is inserted correctly, cerebrospinal fluid begins to be released through the needle.
MedGlav.com
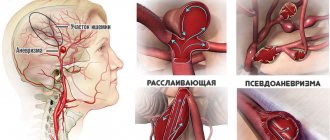
Meningitis (from the Greek meninx - meninges) is an inflammation of the membranes of the brain and spinal cord. They belong to airborne anthroponoses. Carriage of meningococci is widespread. The portal of infection is the mucous membrane of the upper respiratory tract. There are purulent meningitis, characterized by the presence of pus in the membranes, and non-purulent (serous) meningitis, in which the membranes of the brain are saturated with serous effusion. The causative agents of the disease can enter the membranes of the brain: penetrating from the bloodstream into the so-called subarachnoid space; through the lymphatic pathways and cerebral venous sinuses during inflammatory processes of the middle ear; from open cranial wounds; sometimes from distant foci (purulent processes in the lungs, bones, etc.). Some forms of meningitis occur in epidemic outbreaks (eg Cerebrospinal Meningitis ).
Depending on the causes of occurrence, course, pathological and anatomical changes and outcomes of meningitis, there are symptoms characteristic of meningitis, united in the so-called.
- Meningeal syndrome: headache, vomiting, severe limitation of movements, contractures.
Headache is one of the most common and persistent symptoms of meningitis; its intensity varies, it is especially strong in the acute period. The cause of the headache is irritation of the nerves of the pia mater, as well as an increase in intracranial pressure due to the resulting dropsy of the brain. Vomiting is a constant symptom of meningitis and is not associated with food intake; occurs as a result of direct irritation of the vomiting center in the brain or by reflex. contractures are : stiffness of the occipital muscles (impossibility of active and passive adduction of the chin to the chest), inability to extend the leg at the knee joint when bending it at the hip joint (V.M. Kering’s symptom), involuntary flexion of the legs at the knee joint when bringing the head to chest when the patient lies on his back. There is a violation of mental functions , up to complete loss of consciousness. The composition of the cerebrospinal fluid changes, the nature of which depends on the form of meningitis (purulent, serous).
Forms of meningitis.
Caused by a filterable virus. It is observed in the form of epidemic outbreaks and less often in the form of isolated diseases. The inflammatory process can spread to the brain substance. Serous meningitis also occurs as a secondary disease in some common infections (influenza, measles). Symptoms The temperature rises to 38-39C. Meningeal syndrome, which is often accompanied by cerebral symptoms (incomplete paralysis, convulsions, dizziness). It develops acutely, less often gradually, as with other forms of meningitis. Increased intracranial pressure may occur. Limited acute serous meningitis of various localizations are designated as Arachnoiditis (arachnoiditis of the posterior cranial fossa, arachnoiditis of the convex surface of the brain). Treatment. Infusion of 40% methenamine, 1-2% trypaflavin, 40% glucose; symptomatic remedies. For arachnoiditis, sodium iodide (10% solution) can be administered intravenously, 10 ml every other day (8-10 infusions), then 3-5 ml are administered, depending on age. X-ray therapy has been successfully used. For progressive, cystic arachnoiditis, surgical intervention is possible.
Caused by meningococcus. Meningococcus (from the Greek meninx - meninges and cocci) is a microorganism, has the shape of a double ball, is unstable, bends at temperatures above 42C and when exposed to direct sunlight, and is sensitive to drying. A 1% solution of chloramine or carbolic acid, a solution of mercuric chloride 1:1000 kills meningococcus almost instantly. Epidemic outbreaks are observed in the spring. Occurs mainly in children. The process is localized in the membranes of the convex surface of the brain and on its base and is purulent in nature. When moving to the brain substance, purulent encephalitis develops. The disease develops acutely, the temperature rises to 39-40C.
Symptoms Already at the very beginning of the disease, vomiting and severe headaches begin, tension in the neck muscles is sharply expressed. There are photophobia, increased sensitivity of the skin, and often rashes on it. There may be eye movement disorders and suppression of tendon reflexes. Leukocytosis is observed in the blood. The cerebrospinal fluid is cloudy or purulent; in the early period, menigococcus is found in it. The disease can be lightning fast and acute, sometimes it ends suddenly (abortive course), and relapses are possible. If timely treatment is not carried out, the disease often leads to death. Complications can be in the form of dropsy of the brain, deafness, deaf-muteness, blindness, etc. Treatment . Treatment in a hospital. All patients are subject to mandatory hospitalization and are placed in specially designated wards or in isolation wards and boxes. The patient is prescribed semi-liquid, easily digestible high-calorie food. Penicillin is prescribed intramuscularly and into the spinal canal in combination with sulfonamide drugs. Penicillin is administered intramuscularly (1,200,000 units per day for an adult, every 4 hours). In the first 3 days, in addition to intramuscular injections, endolumbar injection of crystalline penicillin sodium salt is used once a day in a dose of 50,000-90,000 units after extracting 10-12 ml of cerebrospinal fluid. Sulfonamides ( norsulfazole 1 g after 6 hours until the main clinical symptoms disappear, then 0.5 g 6 times a day until cerebrospinal fluid parameters normalize. Sulfonamides are less effective than penicillin. The best results are obtained by combination therapy with penicillin and norsulfazole. The effectiveness of treatment is assessed after the disappearance of clinical signs and based on the results of repeated studies of the cerebrospinal fluid. The condition for discharge is the disappearance of clinical signs, normalization of the cerebrospinal fluid and the absence of meningococci in a smear of mucus from the throat of patients with a double bacteriological examination of these smears. In addition, patients must be isolated for the period prescribed by the instructions .
Caused by various forms of pneumococci. More often it develops as a secondary infection from the primary focus (pneumonia, purulent processes in the ears, paranasal cavities). It occurs in children and adults, more often in spring and autumn.
Pneumococcal meningitis is always purulent. Pus is found in the meninges, in the superficial layers of the brain, as well as in its ventricles. It develops mainly acutely, at high temperatures. All meningeal symptoms are usually severe. Atypical cases may be more mild. Some symptoms (paresis and paralysis, convulsions, etc.) depend on the involvement of the brain itself in the process. Dropsy of the brain is a common complication of this form of meningitis. The cerebrospinal fluid is always purulent, with a large number of cellular elements and an increase in protein. There is significant leukocytosis in the blood, ESR is increased. Treatment in a hospital should begin as early as possible. Intensive penicillin therapy is effective. Penicillin is administered intramuscularly, intravenously, and also into the spinal canal. Sulfonamides - orally. Benzylpenicillin is administered at the rate of 200,000 units/kg per day. For adults - 12,000,000 units/day. The intervals between penicillin administrations should not exceed 4 hours. Penicillin is administered intramuscularly; intramuscular and intravenous administration can be alternated. The dose of penicillin cannot be reduced during treatment. The duration of antibiotic therapy is 5-8 days. The antibiotic is discontinued only after positive results of the cerebrospinal fluid analysis. penicillins (ampicillin) are also effective Levomycetin succinate is also prescribed in a dose of 1-1.5 g IV or IM, rifampicin 0.6 g orally every 8 hours. With the development of infectious toxic shock, crystalloid solutions , prednisolone (120 mg), etc. are administered IV.
Occurs in tuberculosis patients in the phase of attenuation or exacerbation of the main tuberculosis process. It occurs 8-10 times more often in children than in adults. There is an effusion at the base of the brain, and millet-like rashes are found on the membranes. Inflammatory changes in the ventricles and at the base of the brain lead to the closure of the cerebrospinal fluid flow and to the development of cerebral hydrocele. In chronic stages, the process spreads along the meninges to the spinal cord and the cerebral hemispheres. Softening in the substance of the brain and limited or diffuse inflammation of the soft and dura maters are often observed. The cerebrospinal fluid is transparent, flows out under high pressure, and the amount of proteins in it is increased. Symptoms The disease develops gradually: fatigue, immobility, sleep disturbances increase, and constipation often occurs. Vomiting and headaches occur periodically. On the 7-10th day, meningeal syndrome increases, the pulse becomes rare, red spots appear on the face or torso, and paresis (incomplete paralysis) of the abducens, oculomotor and other nerves is observed. If treatment begins late or is unsuccessful, then a disturbance of consciousness occurs, paralysis and convulsions appear.
Treatment. With early diagnosis and timely treatment, it is possible to save up to 90% of patients. Streptomycin, as well as PAS, ftivazide and saluzide are used for treatment. Streptomycin is injected intramuscularly or into the spinal canal. PAS and ftivazid are used simultaneously with a restorative regimen, enhanced nutrition and stay in a favorable environment. After treatment, patients need a course of treatment in a sanatorium.
Features of analysis
Cerebrospinal fluid during meningitis is examined according to certain rules. The first drops of it do not fall into the test tube and are carefully removed because they contain an admixture of blood. The liquid must be in a sterile and chemically clean tube. It is collected in two vessels: one is sent for chemical and general clinical analysis, and the other for bacteriological.
All liquor samples are carefully protected from overheating and cooling. To determine bacterial bodies, they are additionally heated.
Liquid analysis is carried out in several stages:
- assessment of color, volume, measurement of relative density;
- counting cells in the sample (calculated per 1 ml);
- microscopic examination of the sample;
- cytological examination of the stained sample;
- biochemical analysis;
- microscopy.
Accents in treatment
Treatment of serous meningitis is carried out in a hospital. Firstly, the condition requires constant medical attention. Secondly, the patient is contagious. The patient remains in the hospital for about two weeks, even if the acute symptoms were managed earlier. The disease is deceptive: it tends to subside and then return.
How the treatment is structured:
- etiotropes. Drugs are prescribed aimed at destroying a specific pathogen;
- general antiviral agents. For example, which contain interferon;
- immunomodulators. Necessary for patients who have reduced immunity;
- antipyretic. If the temperature persists;
- analgesics. In case of cephalalgia;
- nootropics and vitamins. Important for restoring cerebral circulation;
- diuretic. May be needed to relieve swelling;
- antibiotics. Adults are prescribed before receiving test results. And doctors try to prescribe help for children without substances that suppress cell growth.
Patients diagnosed with meningitis are prescribed a special diet. They are entitled to fractional meals. The menu focuses on fruits, fish, poultry, eggs, and dairy products. The amount of salt, fats and sweets in the diet is reduced.
With timely treatment, patients recover completely and live a full life without consequences. Their job is to prevent relapse. To do this, you need to be stricter in matters of personal hygiene, strengthen your immune system, and eat right. The risk of disease is also reduced if you are vaccinated against rubella, tuberculosis, mumps, and polio.
Deviations from normal indicators - video
In the presence of brain diseases, the cerebrospinal fluid changes its characteristics:
- If pathogenic microorganisms are present in it, it turns greenish-gray. A large number of leukocytes are found in the fluid.
- The red color of the cerebrospinal fluid indicates the presence of red blood cells. It happens with intense inflammatory damage or after injury.
- With the development of inflammatory processes in the body, the cerebrospinal fluid becomes yellow and even brown, and hemoglobin decomposition products are found in it. This condition is called xanthochromia.
- False coloration of the cerebrospinal fluid is also possible. It occurs with prolonged use of certain medications.
- The green color of the liquor occurs with purulent inflammation of the lining of the brain.
- A cyst rupture turns it dark.
- When protein elements are cytosed, the cerebrospinal fluid becomes opalescent.
- The disease process in the meninges increases the density of the spinal fluid to 1.015.
- Increased amounts of fibrinogen promote the growth of fibrosis clots and films. Typically, such phenomena occur during the development of the tuberculosis process.
Sometimes enzymes are found in the liquor. Normally, it should contain few enzymes. An increase in the content of these substances may indicate a disruption in brain activity.
With meningitis, counting the number of microbial cells is of particular importance . This number is critical for determining an accurate diagnosis and selecting a treatment method. The following calculation methods are used:
- determination of the number of cells that are stained using the Romanovsky Giemsa or Nokhtu method);
- counting liquor elements using a Fuchs and Rosenthal chamber. In its absence, a Goryaev chamber is used.
The increase in cells in the cerebrospinal fluid during meningitis is called pleocytosis. It is often diagnosed during inflammatory diseases. This phenomenon is most pronounced in the tuberculous form of meningitis.
Staining with Samson's solution makes it possible to accurately differentiate microbial and other cells. With meningitis, the number of lymphocytes, neutrophils, monocytes, eosinophils, and basophils increases. The doctor is interested in the quantity of all these elements.
Slow leakage of cerebrospinal fluid, the impossibility of obtaining it, pronounced coloring, discrepancy between the patient’s serious condition and the composition of the fluid, pronounced coagulation of the cerebrospinal fluid indicates that the patient is developing blocked types of meningitis.
The presence of atypical cells in the fluid while maintaining its transparency and the absence of increased protein content does not confirm the diagnosis of meningitis. The patient is referred for additional studies, since this sign may indicate the progression of a malignant process in the brain.
Liquor in pathology
Pathological processes in the spinal cord and brain lead to changes in the physicochemical properties of the cerebrospinal fluid, as well as to changes in its cellular composition. These changes, as a rule, are characteristic of a number of diseases, which greatly facilitates the diagnosis of the patient and facilitates the choice of treatment tactics.
- Changes in color and transparency.
Cloudiness of the cerebrospinal fluid can occur with an increase in protein in its composition, the appearance of bacteria or fungi, or with an increase in the number of erythrocytes (> 400 * 10 6) and leukocytes (> 200 * 10 6). Red blood cells in the cerebrospinal fluid can appear in large numbers with subarachnoid hemorrhage, brain tumors and traumatic brain injuries. Infectious and inflammatory diseases of the brain occur with an increase in the content of leukocytes in the cerebrospinal fluid. Purulent meningitis causes clouding and a change in color (usually gray). Liqueur in serous meningitis may remain colorless or acquire a xanthochromic (yellowish) tint and flow out under high pressure.
A grayish-pink color of the liquid will appear when the number of erythrocytes is 0.6-1.0*109/l, pinkish-red when the number of erythrocytes is 2-50*109/l, when the number is 51-150*109/l - the color of fresh meat, and at >150*109/l - bloody.
- Cellular composition of cerebrospinal fluid in pathology.
When the total number of cells in the cerebrospinal fluid increases, the term “pleocytosis” is used, the causes of which are organic lesions of the central nervous system.
If the number of cells in the cerebrospinal fluid ranges from 6 * 106 / l to 70 * 106 / l, then in this case they speak of weak pleocytosis. Moderate pleocytosis - from 70 to 250 *106/l, pronounced - from 250 to 1000 *106/l, pronounced - more than 1000 *106/l.
Bacterial meningitis, meningoencephalitis, and multiple sclerosis occur with mild pleocytosis. Severe pleocytosis occurs in malignant brain tumors, as well as in stroke, especially in the first 24 hours. Hematomas and subarachnoid hemorrhages also occur with pronounced pleocytosis.
- Changes in the number of neutrophils and lymphocytes, as well as their ratio.
The reasons for the sharp increase in the number of lymphocytes are viral meningitis, tuberculous meningitis, parasitic diseases of the brain (echinococcosis, etc.), multiple sclerosis, subacute sclerosing panencephalitis, syphilitic meningoencephalitis and other diseases.
Changes in spinal fluid in purulent meningitis
The liquor in this case is heterogeneous. A feature of the disease process is that the number of pathologically altered cells and microorganisms in the cerebrospinal fluid rapidly increases. If the patient is suspected of developing purulent meningitis, then a general examination should be carried out no later than 60 minutes after the lumbar puncture.
If the number of neutrophils in the spinal fluid decreases significantly, this indicates that the outcome of the disease is favorable. Analysis of cerebrospinal fluid during meningitis helps determine the severity of the pathological process.
In the presence of purulent formations, the amount of protein increases, but with timely sanitation it begins to decrease. The combination of pleocytosis and elevated protein indicates an unfavorable prognosis for meningitis.
With the purulent variety of the disease, there is a decrease in glucose in the cerebrospinal fluid . If its quantity increases, then this indicates regression of the disease.
Diagnostics
If you suspect meningitis or any of the above symptoms appear, you should immediately contact a specialist. This disease cannot be delayed; the sooner it is detected, the greater the chance of recovery without serious consequences.
Despite the fact that the first signs of meningitis are pronounced and there are many symptoms typical only for it, diagnosing the disease is a rather labor-intensive task.
Diagnosis of meningitis includes the following set of measures:
- Anamnesis collection, a clear survey of the patient’s complaints, their analysis.
- Examination of the patient for the presence of cerebral symptoms, neurological symptoms (speech assessment, the presence of seizures, the presence of facial asymmetry, etc.), the presence of reflex symptoms characteristic of meningitis, assessment of the mental state (delusions, hallucinations, confusion).
- Analysis of laboratory tests. A blood test showed signs of inflammation.
- Examination of cerebrospinal fluid (CSF). To do this, a lumbar puncture is performed. This diagnostic method helps confirm meningitis; in this case, protein or even pus is detected in the cerebrospinal fluid.
- Magnetic resonance imaging or computed tomography of the head.
- To identify the type of meningitis pathogen, PCR (polymerase chain reaction) is performed and blood or cerebrospinal fluid is examined.
Characteristics of spinal canal fluid in tuberculous meningitis
Laboratory tests for microorganisms for the tuberculous type of meningitis do not show positive results. A more thorough study of the cerebrospinal fluid helps to detect the presence of a pathogen in it.
Precipitation can be noticed no earlier than 12 hours after analysis. The sediment looks like a fibrin network in the form of a web or flakes. A large number of Mycobacterium tuberculosis can be found in it.
During the tuberculous process, the cerebrospinal fluid remains transparent, without noticeable coloring. Cytosis occurs in a fairly wide range and differs depending on the stage of meningitis. In the absence of etiotropic treatment, the number of cells always increases. Repeated cerebrospinal fluid sampling after the start of therapy notes a decrease in the number of cells.
A characteristic feature of the development of pathology is the presence of lymphocytes in the cerebrospinal fluid. If the level of monocytes and macrophages in it increases, this is a bad sign. Neutrophils and giant lymphocytes can be found in large quantities in the cerebrospinal fluid. Protein in this pathology usually increases; its level can reach 3 grams per liter.
The glucose level in the cerebrospinal fluid with tuberculous meningitis sharply decreases to 0.8 mmol. Sometimes the chloride level also decreases. A favorable indicator is an increase in the level of these cerebrospinal fluid indicators.
Treatment
If meningitis is suspected, urgent hospitalization is required; in difficult cases, the patient is placed in the intensive care unit. Complex therapy is carried out, including etiotropic and symptomatic measures.
To eliminate the cause of the disease, the following drugs are used:
- For meningococcal infection and other purulent bacterial lesions, intensive antibiotic therapy is carried out. The drugs are administered intravenously and intramuscularly; Penicillin, Ampicillin, Carbenicillin, Oxacillin, Ceftriaxone, Cefotaxime, Meropenem are used. The combination of medications and dosage is determined by the doctor.
- For the tuberculosis form, Isoniazid, Phtivazid, and Streptomycin are indicated. To enhance the effect of drugs - “Rifampicin”, “Pyrazinamide”.
- For the fungal form, treatment is carried out with Fluconazole, the duration of therapy is 1.5–2.5 months, then prophylactic administration of the drug is required to prevent relapses.
- For protozoal infection, Chloridine is prescribed in combination with Sulfadimezin.
In case of bacterial damage to the brain, there is no specific therapy; general restoratives are administered to influence metabolic processes. Severe cases require the use of glucocorticosteroids and interferon drugs.
Symptomatic treatment
Therapy is aimed at relieving the negative manifestations of the disease that threaten the patient’s life.
- Infusions are carried out to detoxify the body, restore electrolyte balance and metabolic processes - “Hemodez”, “Calcium carbonate”, “Thiamin” (B1), “Pyridoxine” (B6).
- Diuretics are prescribed to activate urine secretion, remove fluid from tissues, and eliminate cerebral edema - Lasix, Mannitol, Uroglyuk.
- “Cytoflavin” is necessary to increase immunity, remove toxins, and restore the characteristics of the cerebrospinal fluid.
For seizures, anticonvulsants are used.
Folk remedies
It is impossible to cure meningitis using traditional medicine; the disease cannot be treated at home. In addition to the main treatment, agents are used to relieve fever, support the immune system and reduce pain.
- For the serous form, lemon balm, mint, and coriander are used. A mixture of dry raw materials in the amount of 60 g is poured with vodka and kept for 2 days in the dark. Compresses are applied to the back of the head and temples.
- For bacterial damage, use lavender inflorescences. Dried flowers are poured with boiling water (400 ml), left to cool. Filter and give the patient a glass of the drink in the morning and evening.
- Linden blossom (1/4 cup) is steamed in a liter of boiling water, after a quarter of an hour the medicine can be consumed. Drink 150 ml infusion three times a day.
- Mash a spoonful of cranberries and put them in a thermos, pour boiling water (200 ml), leave for 5 hours, filter. The volume of liquid is calculated for the day, it is divided into 3 parts.
Spinal canal fluid in meningococcal meningitis
Bacterial examination of the cerebrospinal fluid is mandatory to establish the type of pathogen. If the analysis was carried out on the first day after hospitalization, then in almost all cases pathological microorganisms are detected. On the 3rd day of disease development, the number of microbes decreases significantly.
Changes in cerebrospinal fluid go through several stages:
- increased level of intracranial pressure;
- development of neutrophilic type of cytosis;
- the appearance of changes indicating the development of a purulent type of meningitis.
If meningitis is not treated or is not treated correctly, bacteria are found in the patient’s cerebrospinal fluid. The amount of protein and neutrophils increases. The more protein, the more severe the disease.
Severe meningitis
Pathoanatomically
two forms of otogenic meningitis should be distinguished: serous and purulent. Serous meningitis often accompanies other intracranial complications of ear origin. Typically, serous meningitis is a phase preceding the development of purulent inflammation of the meninges, but as an independent disease it is rarely encountered in the practice of an otolaryngologist. Therefore, describing its flow is not our task. We also do not touch upon the course of concomitant, sympathetic, collateral meningitis, since they do not represent an independent nosological unit, but are a response of the meninges to irritation by various purulent processes in the cranial cavity (brain abscesses, sinus thrombosis, etc.) or the ear.
For practical purposes
Obviously, the most suitable clinical classification is one that takes into account, whenever possible, pathomorphological changes. It comes from the clinical manifestations of the disease in all its diversity.
Based on numerous observations
, as well as the study of literary materials concerning otogenic meningitis, we propose a classification based on the characteristics of the course and manifestation of the inflammatory process. This gives us reason to distinguish between severe and moderate forms, as well as the typical, atypical, wave-like course of otogenic meningitis: a) the typical form of otogenic meningitis is characterized by a clearly outlined picture of the disease; b) atypical - proceeds sluggishly, with scanty symptoms, normal or subfebrile temperature; c) the wave-like course of otogenic meningitis is expressed either in the worsening or in the improvement of the process (this course of the disease is caused either by irrational therapy or by the presence of an abscess that has not been opened in the cranial cavity); d) forms of meningitis accompanied by clearly expressed cerebral phenomena. Focal cerebral signs are caused by encephalitis, cerebral edema, or localized accumulation of pus on the surface of the brain.
Here we will touch
only two clinical forms of otogenic meningitis.
Severe meningitis
Sick
complain of severe headache, nausea, vomiting and dizziness. Clinically, this form of meningitis occurs at high temperatures, reaching 40° and above, sometimes accompanied by chills. The pulse is weak, rapid, breathing is rapid. Consciousness is often obscured or completely absent. There is general hyperesthesia, sometimes delirium. Meningeal signs: stiff neck, Kernig, Gillen and Brudzinsky symptoms are pronounced. The head is often thrown back (opisthotonus). Pathological reflexes of Oppenheim, Gordon, etc. are often noted in the disease picture.
Cerebrospinal fluid
cloudy, cellular elements are found in huge quantities, mainly neutrophils. Their number in 1 mm3 reaches many thousands. The protein content is increased, globulin reactions are sharply positive. The percentage of sugar and chlorides is reduced. On the white blood side, hyperleukocytosis and a shift of the neutrophil formula to the left are noted. The erythrocyte sedimentation reaction is accelerated.
Severe forms of meningitis
proceed this way from the very beginning or acquire such a course subsequently, sometimes as a result of late treatment. They are often combined with other intracranial complications of ear origin (brain abscesses, sinus thrombosis, etc.). From a pathological point of view, we are talking about diffuse purulent inflammation of the soft meninges.
Features of cerebrospinal fluid in serous inflammation
In serous meningitis, the cerebrospinal fluid is usually clear with the presence of a small number of lymphocytes. At the initial stage of the disease, some accumulation of neutrophils is observed. This indicates a complicated course of the disease and usually indicates a poor prognosis for meningitis .
Most often, protein levels fluctuate within normal limits. Among some patients, the amount of this substance in the cerebrospinal fluid decreases slightly, which is caused by an increase in the production of cerebrospinal fluid. Pleocytosis is increased only in the case of meningitis caused by the Coxsackie virus. With herpes, on the contrary, it is almost absent.
During the recovery stage, the patient exhibits lymphocytosis. In mild cases, it is noted already on the third day of illness. With serous meningitis caused by the mumps virus, the cerebrospinal fluid is usually clear and without color. It reveals the presence of lymphocytes, and the level of chloride ions and glucose increases slightly.
source
Symptoms of serous meningitis
Since the disease refers to the process of inflammation, it goes through several periods:
- Incubation period is the time from the moment the pathogen enters the human body until signs of the disease appear. This period for serous meningitis takes about a couple of days;
- A clinical manifestation in which the infected organism expresses a reaction to the toxins of the pathogen. That is, symptoms of serous meningitis appear;
- Convalescence, also known as recovery.
Inflammation of the meninges has clear signs, with rapid development. At the beginning, general symptoms characteristic of any cold appear:
- Fatigue and irritability;
- Increase in temperature to high numbers, up to 40° C;
- Unpleasant sensations in the nasopharynx with the occurrence of nasopharyngitis;
- Intense pain in the head, accompanied by nausea and vomiting.
In addition to general signs of inflammation, specific symptoms of damage to the nervous system appear. Without them, the diagnosis of “serous meningitis” will be invalid. As well as without laboratory confirmation. Specific manifestations include:
- The occurrence of stiffness of the neck muscles. The muscle group becomes unyielding and hard, its resistance increases sharply. So, when trying to straighten the patient’s head in the occipital region, the doctor encounters involuntary resistance;
- Positive Kernig's sign, which is detected with the patient in the supine position. The doctor bends the patient's leg at the hip and knee joints at an angle of 90°. When you try to straighten it, you encounter resistance. This is due to a reflex increase in the tone of the muscles that flex the lower leg;
- Positive Brudzinski's sign, due to irritation of the meninges. There are three types: lower, middle or pubic and upper. The upper one is manifested by involuntary bending of the legs with pulling them towards the stomach, in the case of a passive tilt of the patient’s head. The middle one is associated with pressure on the pubis, which leads to flexion of the hip and knee joints of the lower extremities. The lower symptom appears in one leg when testing the other. At the same time, the unexamined leg involuntarily moves at the knee and hip joints and is pulled towards the stomach. In addition to these three variations of Brudzinski’s symptom, the buccal one is also distinguished. It occurs when pressure is applied to the buccal area, which leads to a reflex raising of the shoulders and bending of the arms at the elbow joints;
- Positive sign of Lessage (suspension). It is used to diagnose meningitis in babies under one year of age. At the same time, the doctor takes the child under the arms and lifts him up. In a sick baby, the legs will involuntarily pull towards the tummy;
- Pathological reflexes of Babinski and Oppenheim;
- Symptoms of damage to the cranial nerves, usually III, IV and VII pairs;
- Clonic and tonic seizures, which can result in status epilepticus.
Everything about cerebrospinal fluid in meningitis: what it is, how the study is carried out and other nuances of the disease
Meningitis is an inflammation of the meninges of an infectious nature with the appearance of meningeal and cerebral manifestations. Cerebrospinal fluid analysis is considered the only reliable way to accurately and quickly diagnose meningitis. Thanks to the method, it is possible to identify the causative agent of the infection, distinguish the purulent form from the serous one, and also monitor the effectiveness of therapy.
Nature of the disease and first risk zone
More often, doctors diagnose serous meningitis. In this form the disease is relatively mild. In 80% of cases, serous meningitis is caused by viruses.
Usually those that initially inhabit the cells of the digestive organs are enteroviruses. The disease is also caused by infectious agents of herpes, influenza, polio, cytomegalovirus and adenoviruses. The bacterial nature of the disease is rarely stated.
The disease mainly affects preschool children - up to 90% of patients. In the remaining 10%, the diagnosis is given to young people - those who are not yet 30 years old.
Since the main causative agents of the disease are enteroviruses, an increased risk of infection occurs in the summer. The virus can be inhaled, eaten or drunk. Encephalitis ticks are also carriers. There is evidence of infection from rodents.
The most common routes of infection:
- air. Serous meningitis is transmitted from person to person. This can happen in transport, at work, on the playground, when communicating face-to-face with an infected person;
- domestic. The disease enters the body through tap water, poorly washed hands, vegetables and fruits “from the garden”;
- water. Beaches, open water and swimming pools are an ideal environment for viruses that cause serous meningitis.
What kind of liquid is this?
Liquor is the fluid that constantly circulates in the elements of the brain and spinal cord. Normally, it looks like a colorless transparent fluid substance that fills the ventricles of the brain, subarachnoid and subdural spaces.
Cerebrospinal fluid is produced in the ventricles of the brain by the choroid covering these cavities. Liquor contains various chemicals:
- vitamins;
- organic and inorganic compounds;
- hormones.
In addition, the liquor contains substances that process incoming blood and decompose it into useful nutrients. At the same time, sufficient levels of hormones are produced that affect the endocrine, reproductive and other systems of the body.
Types of meningitis
Depending on the type of disease, various methods of treating meningitis may be prescribed.
The classification of meningitis includes the following types of this disease:
According to the rate of progression of the disease:
- lightning;
- spicy;
- subacute;
- chronic.
Useful to read: Chronic meningitis: symptoms, causes and treatment methods
Types of meningitis by etiology:
Viral meningitis. It occurs due to the entry of various viruses into the body - enteroviruses, echoviruses, and the Coxsackie virus. This type of meningitis is manifested by fever, severe headache, general weakness, but without disturbances of consciousness.
Bacterial meningitis. The disease manifests itself as a result of the ingestion of bacteria such as pneumococci, group B streptococci, meningococci, diplococci, Haemophilus influenzae, staphylococci and enterococci. Bacterial meningitis has a severe course with signs of intoxication, high fever and other clinical manifestations. Sometimes bacterial meningitis is fatal.
There are some types of meningitis included in the group “bacterial meningitis”: – Fungal meningitis. Diseases appear as a result of the ingress of fungi such as: cryptococci (Cryptococcus neoformans), Coccidioides immitis (Coccidioides immitis) and fungi of the genus Candida (Candida); – Protozoal meningitis. Capable of infecting the spinal cord and brain with simple organisms, for example, amoeba; – Mixed meningitis. The spinal cord and brain become inflamed while the body is simultaneously exposed to an infection, which can have a different etiology; – Nonspecific meningitis. The occurrence of this type of disease has not yet been precisely established.
Types of meningitis by origin:
Primary meningitis. This is an independent disease. Develops without the presence of any foci of infection in other human organs.
Secondary type of meningitis. Capable of developing with other infectious diseases. These include: syphilis, tuberculosis, HIV infections, measles, mumps.
Types of meningitis according to the nature of the inflammatory process:
Purulent meningitis. The disease is a severe course, with a purulent process in the meninges. The cause of purulent meningitis is a bacterial infection.
Serous meningitis. It is a less severe course without any purulent formations. The cause of this type of disease is a viral infection.
Group of serous meningitis: – Tuberculous; – Syphilitic; – Influenza; – Enteroviral; – Mumps and others.
Types of meningitis according to the course:
Fulminant (fulminant) meningitis. The development of this type of meningitis occurs very quickly. The patient can die literally on the first day after the virus enters.
Acute meningitis. After the lesion, several days may pass with an acute clinical picture. After this, the person may die.
Chronic meningitis. Development can occur, increasing in symptoms.
Types of meningitis according to the prevalence of the process:
Basal. Inflammation is concentrated at the base of the brain. Convexital. Inflammation is concentrated on the convex parts of the brain. Total. Inflammation affects all parts of the brain. Spinal. The inflammation is concentrated at the base of the spinal cord.
Types of meningitis by localization:
Meningitis. The inflammatory process covers the soft and arachnoid membranes of the brain and spinal cord. Pachymeningitis. The inflammatory process covers the hard membranes of the brain. Panmeningitis. Damage occurs simultaneously to all membranes of the brain. In medical practice, the term “meningitis” usually means damage to only the soft tissues of the brain.
Mild meningitis; Moderate-severe; Severe.
How is the research conducted?
The procedure performed to collect cerebrospinal fluid is called a lumbar puncture. To carry it out, the patient takes a lying or sitting position. If the subject is sitting, he should be upright, with his back bent so that the vertebrae are located in the same vertical line.
When the patient is lying down, he turns to his side, bending his knees and pulling them to his chest. The injection site is chosen at the level of the spinal column, where there is no risk of damaging the spinal cord.
Lumbar puncture is a procedure that can only be performed by a qualified doctor! The doctor treats the back of the person being examined with alcohol and an iodine-containing solution, after which he feels the puncture site along the intervertebral spaces: in adults at the level of the II and III lumbar vertebrae, and in children - between the IV and V.
The specialist injects an anesthetic there, after which they wait 2-3 minutes to provide tissue anesthesia. Next, the doctor performs a puncture using a Beer needle with a mandrel, moving between the spinous processes and passing the ligaments. A sign of a needle entering the subarachnoid space is a feeling of failure. If you remove the mandrin after this, liquid will be released if the procedure is performed correctly.
A small amount is taken for research.
Treatment of aseptic meningitis
Treatment options include:
- Replacement therapy - your doctor may recommend resting and drinking plenty of fluids. The patient may need to be hospitalized for monitoring and to avoid dehydration;
- Taking medications - if specific causes of meningitis are suspected, the doctor may recommend that the patient take: Antiviral medications;
- Antibiotics;
- Antifungal medications;
- Medicines for pain (eg, acetaminophen, ibuprofen).
Note: Aspirin is not recommended for children and adolescents with current or recent viral infection due to the risk of developing Reye's syndrome.
Table of the relationship between the form of the disease and the color of the liquid
| Serous, viral | Tuberculous | Syphilitic | Purulent | |
| Color | Transparent | Transparent, opalescent | Transparent, rarely cloudy | Turbid |
| Cells in 1 µl | 20-800 | 200-700 | 100-2000 | 1000-5000 |
| Protein (g/l) | Up to 1.5 | 1-5 | Moderately elevated | 0,7-16 |
| Glucose (mmol/l) | Not changed | Sharply reduced | Not changed | Sharply reduced |
| Chlorides (mmol/l) | Not changed | Reduced | Not changed | Reduced or not changed |
| Pressure (mm water column) | Increased | Increased | Slight increase | Increased |
| Fibrin film | In most cases absent | Present in 40% of cases | Absent | Coarse or in the form of sediment |
Composition of the fluid substance
Depending on the causative agent of the infection, cerebrospinal fluid may have a different composition. Let's take a closer look at the cerebrospinal fluid 2 forms of inflammation.
Serous
Characteristics of cerebrospinal fluid:
- Color – colorless, transparent.
- Cytosis: lymphocytic pleocytosis is detected. The level of cellular elements is from 20 to 800 in 1 µl.
- Protein values: increased, up to 1.5 g/l (protein-cell dissociation).
- Glucose and chloride levels were unchanged.
Purulent
Characteristics of cerebrospinal fluid in pathology:
- The color varies depending on the causative agent of meningitis. For example, with meningococcus it will be cloudy, yellow, with pneumococcus it will be whitish and bluish in the case of blue-purulent bacillus.
- Cytosis: a huge number of cells (cell-protein dissociation), reaching 1000-5000 cellular elements per 1 μl. Neutrophilic pleocytosis is characteristic.
- Protein content: increased, in the range of 0.7-16.0 g/l.
- Glucose levels are reduced, about 0.84 mmol/l.
- The amount of chlorides is reduced or unchanged.
- The presence of a fibrin film in the cerebrospinal fluid or sediment.
Signs
The main symptoms of infectious meningitis:
- fever, increased temperature;
- increased breathing with rhythm disturbance;
- a change in heart rate, initially tachycardia is observed, and as the process worsens, a slowdown in heart rate is detected.
In some cases, multiform rashes appear on the body.
Meningeal, or meningeal, syndrome includes:
- Headache. The sensations are usually painful, localized in the back of the head or in the frontal region, and are often accompanied by gushing vomiting.
- Hyperesthesia. Patients are concerned about increased sensitivity to light or sounds.
- Characteristic pose. Due to tonic muscle tension, the patient lies with his back arched and his head thrown back. The legs are bent, the stomach is sunken. Stiffness of the neck extensor muscles prevents the head from being tilted forward, causing pain.
- Tendon reflexes are observed early in the disease.
When inflammation is localized in the brain, early strabismus, drooping eyelids, and sometimes paralysis of the eye and facial muscles are observed.
Depending on the severity of the course, the symptoms of meningitis in adults are accompanied by clouding or loss of consciousness, hallucinations and delirium, convulsive contraction of the muscles of the limbs and body. When the brain substance is involved in inflammation, paresis and paralysis are possible.
Not all meningeal symptoms always appear immediately; in young children and elderly patients, the clinical picture is often blurred. In infants, signs of toxicosis become fundamental: fever, loud crying, regurgitation, convulsions, dehydration, dyspepsia. In infants, due to increased intracranial pressure (ICP) and accumulation of cerebrospinal fluid, bulging of the fontanel is noticeable.
Decoding indicators
Based on the values of the cerebrospinal fluid data, specialists clarify the diagnosis and, in accordance with this, can prescribe adequate therapy.
Number of cells and cytosis
The cells in the cerebrospinal fluid are counted and their predominant type is then determined. An increased content (pleocytosis) indicates the presence of an inflammatory process. Pleocytosis is more pronounced with bacterial meningitis, in particular tuberculous inflammation of the meninges.
In other diseases (epilepsy, hydrocephalus, degenerative changes, arachnoiditis), cytosis is normal. Specialists count cellular elements, which are represented in most cases by lymphocytes or neutrophils.
After studying the cytogram, the doctor can draw a conclusion about the nature of the pathology. Thus, lymphocytic pleocytosis indicates serous meningitis or tuberculous meningitis with a chronic course. Neutrophilic leukocytosis – observed during acute infection (bacterial meningitis).
Protein
Analysis of the protein content in the CSF allows us to clarify the nature of the disease, as well as assess the state of the blood-brain barrier. Normally, its level is in the range of 0.2-0.45. An increase in protein in the cerebrospinal fluid is characteristic of meningitis and cerebral hemorrhages.
Glucose
Glucose values should be 2.8-3.9 mmol/L. However, even healthy people may have slight fluctuations in the content of the substance. To correctly assess glucose in the cerebrospinal fluid, it is advisable to determine it in the blood: in the absence of pathology, it will exceed 2 times the values in the cerebrospinal fluid.
Increased levels are observed in diabetes mellitus, cerebrovascular accidents, and acute encephalitis. Reduced glucose levels occur with meningitis, neoplasms, and subarachnoid hemorrhage.
Enzymes
Liquor is characterized by low activity of the enzymes it contains. Changes in the activity of enzymes in the cerebrospinal fluid in various diseases are mainly nonspecific. With tuberculous and purulent meningitis, the content of ALT and AST increases, LDH increases in bacterial inflammation of the meninges, and an increase in total cholinesterase indicates the acute course of meningitis.
Chlorides
Normally, the content of chlorine salts in the CSF is 120-130 mmol/l. A decrease in their level may indicate meningitis of various etiologies and encephalitis. An increase is observed in diseases of the heart, kidneys, degenerative processes and formations in the brain.
Liquor is normal
Liquor, like human blood, has a number of indicators that can be assessed using laboratory research methods. Cerebrospinal fluid for research is obtained using a lumbar puncture, during which up to 10 ml of fluid can be collected once without complications for the patient.
The following indicators are assessed:
Cerebrospinal fluid is normally colorless, transparent and odorless. 99% of liquor consists of water, the remaining 1% is dry residue.
- The normal relative density is 1.006-1.007.
- Amount of protein 0.2-0.33 hl.
- The amount of glucose is 2.8-3.9 mmol.
- Amount of Cl- (chlorides) 120-130 mmol.
- The acidity of the cerebrospinal fluid (pH) is normally 7.28-7.32. If the permeability of the blood-brain barrier is not changed, then the pH of the cerebrospinal fluid remains within normal limits even when the pH of the blood changes.
- The number of cells in 1 μl of cerebrospinal fluid (cytosis) is up to 4 cells.
Cytology allows you to determine the total number of cells per 1 µl or 1 liter of liquid, as well as differentiate cellular elements (lymphocytes, neutrophils, in some cases, erythrocytes and other cells). In an adult, 1 liter of cerebrospinal fluid contains from 3*106 to 5*106 cells, and in children in the first three months of life their number reaches 20-25*106/l.
- The content of lymphocytes is 80-85%, neutrophils 3-5%.