Neurosurgical assistance in the treatment of stroke, according to the program for assistance to patients with vascular diseases, can be provided on the basis of regional vascular centers. Neurosurgical departments are also available in many primary vascular centers; in this case, the patient is operated on “on the spot”.
Neurosurgical operations can be performed for both ischemic and hemorrhagic strokes and can include both the prevention of the development of strokes, when there are signs of narrowing of the main arteries of the head and neck, and the elimination of the consequences of a stroke.
Before surgery, special studies are usually performed:
- Duplex ultrasound scanning
- Computed tomography of the brain
- Angiography
These studies help determine the level and degree of disturbance of blood flow in the vessels of the neck and head, the speed of blood flow, the presence of plaques and some other parameters of cerebral circulation.
Indications and contraindications for
Craniotomy refers to emergency surgical interventions that are performed for:
- increased intracranial pressure;
- pronounced swelling of brain tissue;
- the presence of large hematomas;
- thrombosis and atherosclerosis of cerebral arteries;
- the presence of malignant tumors;
- the addition of infections and inflammatory processes;
- the need for tissue sampling for histological examination.
In some cases, the operation is dangerous to the health and life of the patient. The list of contraindications to craniotomy includes:
- severe arterial hypertension;
- operations in the intracranial space undergone during the last 6 months;
- decompensated acute and chronic heart failure;
- severe diseases of the central nervous system;
- old age (in this case, surgery is performed only for life-threatening conditions that are not amenable to drug therapy);
- exacerbation of chronic diseases of internal organs;
- late stages of oncological pathologies;
- purulent lesions accompanied by soft tissue necrosis.
Stroke and trepanation - what to expect in the end
Stroke is an acute cerebrovascular accident (CVA), leading to severe consequences. There is even such a thing as a “therapeutic window,” which means that the patient can be helped as fully as possible only in the first 6 hours.
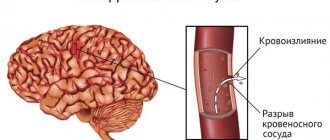
One of the most severe types of stroke is hemorrhagic, the consequences of which are often unpredictable. It is accompanied by a cerebral hemorrhage resulting from a ruptured blood vessel.
The size of the hematoma can vary, and the same differences are observed in symptoms - from moderate to extremely severe.
If the size of the hematoma is above average and conservative treatment is ineffective, surgical treatment is often resorted to.
Sometimes the patient’s condition is so severe that surgery is the only option.
Non-surgical consequences
Once the postoperative period has passed and the danger caused by the stroke has receded, other difficulties come to the fore. The patient first begins to worry about the defect of the skull bones, since part of the bone is sometimes removed. Cranioplasty is a way out of the situation and prevention of trephine syndrome.
There are frequent cases of sudden weight loss by the patient, memory impairment, constant weakness, short-term disturbances of consciousness, episyndrome, and indigestion.
But it is impossible to say unequivocally that it is trepanation that causes such symptoms, since in the postoperative period a lot of potent drugs are prescribed; some of the symptoms can be caused by the stroke itself, especially if help is not provided in a timely manner.
Source: https://GolovaLab.ru/insulto/kak-lechit/trepanaciya-cherepa-pri-insulte.html
Preparation
Preparation for trepanation for hemorrhagic stroke includes:
- Examination. Before the operation, blood and urine tests are taken. The qualitative and quantitative composition and blood clotting are assessed, signs of inflammatory diseases that can become contraindications to intervention are identified. Indications for surgery are determined using CT or MRI of the brain. An ECG is performed to assess the functions of the cardiovascular system.
- Refusal to take medications. 2 weeks before the procedure, the attending physician discontinues medications that can cause postoperative complications. These include anticoagulants and antiplatelet agents that reduce blood clotting. On the day of the procedure, stop taking all medications.
- Refusal to eat the day before the intervention. On the day of surgery, drinking liquids is not allowed.
- Consultation with a neurosurgeon. The doctor tells the patient about the chosen treatment method and possible risks. At this stage, the medical history is studied.
Important information: Early and late complications after stroke in men
Surgical procedures
A cerebral stroke occurs due to the appearance of pathology in the circulatory system that ensures the functioning of the brain. Such problems arise both in large vessels and in small ones. However, the amount of damage will vary. Typically, the most common vascular pathology is the formation of atherosclerotic plaques in various places, which contribute to the thinning of the choroid, increased pressure in a certain area of the vessel, protrusion of its wall and ultimately to the rupture of the blood vessel.
In some cases, the cause of the pathology is dissection of the arterial walls and rupture of the vessel. During a stroke, a blood vessel in the brain may be blocked by a blood clot - a thrombus. In any narrow place where the vessel is dissected or damaged, the clot gets stuck and interferes with the flow of blood. The main goal of surgeons is to remove the blood clot and restore normal blood circulation in the brain.
Aneurysm clipping
Clipping an aneurysm is by no means a safe procedure. After it is performed, patients may experience speech impairment, visual problems, numbness of the limbs, and memory problems. The most dangerous complication is the occurrence of new blood clots, which will provoke another stroke.
Important! Statistics show that a person can suffer two strokes; the third stroke is fatal for most patients. However, clipping is one of the main procedures performed for ischemic cerebral stroke.
At the initial stage, the doctor will determine the patient’s health condition and the advisability of surgery, as well as possible contraindications to the operation. The doctor is provided with all the necessary information after diagnostic procedures (MRI, CT, angiography); if the patient is conscious, the doctor will try to find out what medications the patient is taking. If a pregnant woman suffers from a stroke, she should inform the doctor about this, since in this case clipping is not used.
When starting the operation, the doctor connects the necessary sensors to the patient. Vital signs are displayed on the monitor screen and anesthesia is administered. A catheter is placed to collect urine. During the operation, general anesthesia is given. In the area required for the incision, the hair is shaved off, and the skin is treated with an antiseptic.
The next stage of the operation is one of the most important. The doctor performs a craniotomy - opening the skull to provide access to the problem area. Using a microscope, the doctor determines which area is affected, where there is a rupture of the vessel, or where there is a blood clot. The aneurysm is then separated from healthy tissue, and the vessel is clipped with a special titanium clamp-like device. After this, blood circulation in the vessel is restored.
At the final stage, the part of the skull removed for the operation is returned to its place, the scalp is stitched, and the seam is treated with an antiseptic. Previously installed catheters are removed from the body. The staff monitors the patient’s vital signs, the doctor always monitors the situation, and upon recovery from anesthesia, examines the patient, evaluates the success of the intervention, and identifies complications that will have to be dealt with during the rehabilitation stage. In some cases, patients go into a coma after surgery.
For several days, patients are placed in neurosurgical intensive care, and then transferred to a ward (for at least a week). On average, the operation lasts from three to five hours - the doctor simply does not have more time.
Removal of hematoma
With a hemorrhagic stroke, a hematoma occurs that puts pressure on the brain. It must be removed as soon as possible. This will help not only free areas of the brain from compression, but also eliminate the effect on the brain of toxins released when a hematoma appears. The task of the neurosurgeon in this case is to remove blood clots from the resulting cavity as thoroughly as possible and minimally damage the healthy brain matter, preserving the functioning of vital centers.
The indication for surgery is the presence of a hematoma with a volume of more than 20 cm3 and with a volume of more than 10 cm3, if the hematoma compresses the brain stem and lateral ventricles. The operation is performed using craniotomy or puncture, when the contents are aspirated and the ventricles are drained.
At the moment, doctors prefer to move away from open operations - such intervention is performed only on every fourth patient, and in other cases, sparing operations are performed. Rehabilitation after surgery for a stroke is the same as for clipping.
This will SAVE you from a STROKE! 10 tips from professional doctors Treatment of stroke with pine cones Stroke - symptoms and causes, methods of treatment. First aid for stroke
How is trepanation done?
Depending on the size of the lesion and the general condition of the patient, the operation can take from 5 to 10 hours. The surgical plan includes the following steps:
- Patient preparation. Drugs for general anesthesia are administered intravenously, after which the trachea is intubated. The patient's head is fixed using a special device that holds the skull in an upright position. This allows you to completely immobilize the operated area during surgical procedures. At the same stage, a lumbar drainage is installed, which is necessary to drain the cerebrospinal fluid. Sometimes cerebrospinal fluid pressure is reduced with medication.
- Skin incision. The surgical wound lies along the hairline. They try to minimize the risk of cosmetic defects after the intervention. The skin flap is separated from the cranial bones.
- Opening the skull. A drill makes several small holes. Using a medical saw, a bone flap of the required size is cut out. It is stored throughout the surgical procedure for the purpose of subsequent return to its place.
- Gaining access to the medulla. The surgeon puts on glasses with an operating microscope, and then makes an incision in the dura mater. The organ is tightly compressed by the skull, so it is impossible to move its tissues. To perform manipulations, the neurosurgeon uses thin instruments inserted into the thickness of the brain. The focus of necrosis or hematoma is removed, the intervention is combined with constant monitoring of the condition of the cranial nerves and the cardiovascular system.
- Closure of the skull defect. The cut bone flap is returned to its original position or fixed with metal staples. The surgical wound is sutured, after which a sterile bandage is applied.
Important information: Medicinal recipes for stroke tinctures made from pine cones and are there any contraindications?
Why is surgery needed after a brain injury?
Surgery is indicated in the presence of hemorrhage.
Efficiency does not always occur, and in addition, the localization of the source of the stroke does not allow surgery in all cases. Indications for surgery are the following conditions:
- Cerebellar stroke, the focal lesion of which is above 3 cm. Especially if the neuralgic changes progress, and there are also signs of cerebral edema or compression;
- The presence of hemorrhage on the surface of the cortex;
- Pouring of blood into the cerebral ventricles;
- Brain swelling;
- Coma, from which the patient does not recover for more than 6 hours;
- Vascular pathologies with bleeding.
The following types of operations are carried out:
- Aneurysm clipping. Performed when an aneurysm ruptures. A catheter is inserted through the artery in the thigh, and the aneurysm is fixed with clips;
- Trepanation of the skull. It is rarely indicated for cases of large hemorrhage and hematoma pressure on the brain, leading to severe headaches, high blood pressure and fainting. This method is used when there is a clear threat to the patient’s life and when stroke recurs. During this procedure, the skull is opened, the surgeon removes the accumulated blood, and then the removed part of the bone can be replaced with screws or a plate. If the lesion is large, decompression trepanation is prescribed - part of the skull is removed, which reduces the pressure on the undamaged areas of the brain;
- Carotid endarterectomy. It is carried out for frequent ischemic attacks, as well as for diagnosing vessel narrowing;
- Selective thrombolysis. A catheter is inserted through a large artery, and a special thrombolytic is administered through it - a drug that dilutes the blood clot and removes it from the vessel;
- Stenting. Most often, this operation is performed to prevent recurrent strokes.
Consequences
Craniotomy after a stroke can cause the following complications:
- intracranial bleeding;
- swelling of brain tissue;
- epileptic seizures;
- addition of bacterial infections;
- injury to tissue or blood vessels of the brain;
- complete or partial paralysis of the limbs;
- speech disorder;
- memory impairment;
- disruption of the processes of memorization and perception of new information;
- severe headaches, nausea and vomiting (in the early postoperative period, pain is eliminated with narcotic analgesics);
- the presence of a cosmetic defect associated with the removal of a bone flap (cranioplasty helps solve this problem);
- dysfunction of the digestive and respiratory systems;
- muscle weakness.
Rehabilitation after trepanation includes:
- stay in the intensive care unit (during the first 2 days you need to monitor the performance of the brain and heart);
- care of the surgical wound (the bandage is changed daily, the wound is treated with antiseptic solutions, the sutures are removed after 10-14 days);
- following a special diet (the patient should eat easily digestible foods that do not interfere with intestinal motility);
- exercise therapy (helps avoid stagnation of blood and lymph caused by prolonged immobilization);
- drug therapy (at this stage, nootropics and neuroprotectors are used that normalize brain functions).
Disability after craniotomy is assigned in the presence of severe consequences of a stroke and the operation itself.
How dangerous is surgical treatment for stroke?
Open surgery carries a great risk to the patient's life.
The effectiveness and safety of trepanation depend on the promptness of first aid, the age of the sick person and the severity of the stroke. Surgery is not omnipotent, so in some cases serious complications arise after surgical treatment. The following consequences of craniotomy are noted:
- epilepsy;
- intracranial bleeding;
- extensive swelling;
- violation of the integrity of tissues and blood vessels;
- infection;
- partial or complete paralysis;
- problems with memory and speech;
- weight loss;
- prostration;
- improper digestion;
- temporary clouding of reason;
- nausea and vomiting;
- dizziness and migraines;
- difficulties with the perception of surrounding reality.
In some cases, another stroke may occur after surgery. Relapse is associated with weakness of the walls of blood vessels and arteries. During surgery, healthy tissue is sometimes damaged. In the future, this leads to repeated hemorrhages into the brain cavity. The postoperative period is always difficult to bear. Patients practically learn to walk, talk, write, read, etc. again. They gradually remember the facts of their lives and do not immediately recognize their relatives and friends. However, full recovery is possible. The main thing is proper care for the patient and the efforts of the patient himself.
Stroke surgery
If the consequences of a stroke are difficult for the patient’s health, only surgery can correct the situation. Surgery of this level is very complex and is carried out using special equipment.
In this case, two methods are used:
- trepanation - drilling into the skull;
- Craniotomy - an incision into the skull.
This can help save the patient's life. But no specialist will make predictions in advance for a complete recovery.
Sometimes craniotomy is the patient’s only chance of recovery.
Before establishing the possibility and necessity of surgical intervention, you need to:
- Complete examination of blood vessels. To do this, a special scan is done using ultrasound.
- Be sure to conduct a full examination of the brain using a computer and a magnetic field.
- X-ray examination of blood vessels, which checks their function, blood flow and the development of pathology.