Brainstem stroke is a pathological condition in which certain disturbances in the usefulness of cerebral circulation occur, affecting the immediate parts of our brainstem.
Moreover, the consequences of such violations can be not only moderately unpleasant, but also globally sad. It must be said that, like any other type of stroke pathology of the brain, according to its origin, brainstem stroke can be divided into ischemic and hemorrhagic lesions.
Insufficient blood supply due to blockage of blood vessels in the brain
Namely, ischemic brainstem stroke is a type of pathology that develops as a result of blockage (spasm, thrombosis, embolism, etc.) of the brain vessels supplying blood to parts of its brainstem and resulting from such blockage, insufficient blood supply.
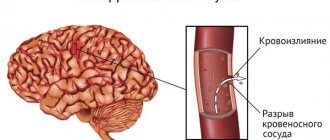
Hemorrhagic brainstem stroke, accordingly, is a pathology, the development of which becomes possible with the rupture (complete or partial) of the vessels supplying blood to certain parts of the brain stem and with the development of hemorrhage in these parts. As a rule, the prognosis for survival and consequences for the human body with hemorrhage are more negative.
Of course, the symptoms of this disease can vary significantly depending on which part of the brain is affected and how extensive the affected area is.
It should be noted that a stroke in general and an ischemic stroke of the brain stem in particular is an emergency pathological condition in which sudden death of our brain cells becomes possible.
However, the symptoms of damage to the brain stem are quite specific for doctors and, therefore, experienced doctors, even at the stage of the initial examination and examination of the patient, can assume the localization of the necrotic focus.
Actually, it is at this stage that it becomes possible for an experienced doctor to make the first preliminary forecast regarding what the further treatment, recovery, and recovery of a particular patient will be. However, let us immediately make a reservation that only timely specialized (instrumental) CT or MRI studies can completely confirm or refute the preliminary prognosis for treatment, survival, consequences and recovery of the patient.
general characteristics
The brain stem connects the brain to the spinal cord. This area consists of the medulla oblongata, midbrain and pons.
The brain stem is extremely important as it houses vital nerve centers. A stroke in this area can lead to disruption of the functionality of various internal organs.
Trunk stroke, depending on the nature of the damage, can be hemorrhagic or ischemic. The first option means a rupture of a blood vessel with subsequent spillage of blood into the brain tissue, the second implies a blockage of blood flow (thrombus, atherosclerotic plaque).
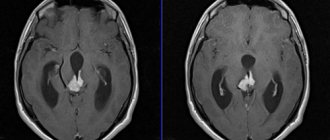
MRI shows stroke
MRI, as noted earlier, always shows a stroke. This statement is confirmed from the standpoint of evidence-based medicine. MRI examination is recommended by both the World Health Organization and the World Association of Neurologists.
Since the development of medical physics does not stand still, such phenomena as diffusion and perfusion are also applicable to MRI. It is with the help of diffusion-weighted imaging (MRI scanning mode) that changes in the brain are detected minutes after the onset of stroke symptoms. MRI stroke.
Extensive infarction in the middle cerebral artery area
Causes
There are many possible causes of a brain stem stroke. Most often, the appearance of pathology is provoked by the following factors:
- Atherosclerosis. This is more often observed in elderly patients. Fatty plaques appear in the arteries, and their rupture leads to thrombosis. The vessel becomes clogged, and the brain matter necrosis.
- Arterial hypertension. The arteries and arterioles of the brain undergo irreversible changes. The walls of the vessels become thinner and brittle, which means they are at risk of rupture and subsequent hemorrhage.
- Aneurysms, vascular malformations. This cause of brainstem stroke is typical for patients at a young age.
The likelihood of a brainstem stroke increases with certain diseases. People with the following pathologies are at risk:
- metabolic disorders (usually diabetes);
- heart valve disease;
- rheumatism;
- bleeding disorders (may occur while taking certain medications).
When treating, it is important to consider not only the causes of the pathology, but also the extent of the lesion. An important condition for a favorable outcome is timely assistance.
What does an MRI show after a stroke?
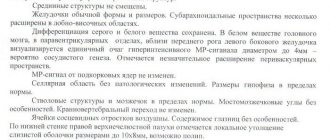
On MRI sequences such as PD/T2WI (proton-weighted imaging) and FLAIR (fluid attenuation inversion recovery) MRI sequences appear to be high intensity signal from a lesion.
MRI sequences such as PD/T2WI (proton-weighted imaging) and FLAIR (fluid-attenuated inversion recovery) detect up to 80% of strokes with first-onset symptoms within 24 hours. In up to 30% of cases, for the first time 2-4 hours after the onset of symptoms, these sequences may not detect a stroke, then DWI (Diffusion weighted imaging) comes to the rescue.
The high signal on these classic MRI sequences is the result of irreversible brain damage—cell death.
A high signal is very bad news, indicating the death of brain tissue
Is a stroke visible on an MRI?
Stroke is always visible on MRI, and according to the recommendations of the World Health Organization (WHO), the World Association of Neurologists (WAN) is the “Gold Standard” in identifying any type of stroke. The radiologist, after receiving the data on his personal computer, evaluates the anatomical changes of the brain. Since the data from the first study is saved to disk and printed on film, the attending neurologist after treatment can evaluate the prescribed therapy and raise the question of correcting drug treatment, which is very important for the patient’s future quality of life.
In a patient, even with sparse neurological symptoms, lesions are detected on classic MRI sequences
Symptoms of brainstem stroke
In most cases, there is a sudden onset of brain stem stroke. Common manifestations of pathology include the following signs:
- dizziness, headache;
- loss of consciousness;
- speech disorder;
- numbness of the limbs, paralysis;
- increased breathing;
- paleness of the skin, a blue or green tint is possible.
With an ischemic stroke, part or all of the face may turn red. Breathing becomes difficult, sometimes wheezing appears. The victim begins to sweat, body temperature rises, pulse decreases, but becomes tense.
With a brainstem stroke, signs appear very quickly, literally in a matter of hours.
The patient may have locked-in syndrome. In this case, impulses do not travel from the brain to the body, so it is completely paralyzed. At the same time, intellectual abilities do not suffer, the person understands everything.
General information
Brainstem stroke is a common neurological disease, accounting for 18–20% of all acute cerebrovascular accidents. In this case, the ratio of ischemic and hemorrhagic types is 3:1. The likelihood of developing pathology increases with age - people over 50–55 years of age suffer 1.8–2 times more often with each subsequent decade, but there is a steady trend towards younger age of the disease. The gender structure of vertebrobasilar strokes is usually dominated by men, although some forms are more common in women. Representatives of the Negroid race get sick more often than Europeans; the lowest risk was recorded in Asians.
Diagnostics
In case of a brainstem stroke, it is important to quickly diagnose the violations that have occurred. The most effective initial measure is computed tomography. It allows you to see hemorrhage in the shortest possible time.
If computed tomography does not bring results or is not informative enough, then magnetic resonance imaging is used. Such research takes more time, but provides a more complete picture.
Additionally, other diagnostic methods can be used:
- Angiography. Such a study is necessary to assess the state of the cardiovascular system and identify atherosclerosis, thrombosis and a number of other pathologies.
- Ultrasound scanning of blood vessels. It allows you to evaluate various indicators of blood flow.
- Cardiography. This diagnosis detects changes in heart rhythm, indicating disturbances in the intensity of blood flow.
Due to the lack of equipment or the impossibility of using it around the clock, it often turns out that proper research has not been carried out. This situation negatively affects the prognosis of the pathology.
Can an MRI fail to show a stroke?
Today, MRI technologies have reached such a level that viewing a stroke even in the most acute period (up to 3 hours after the development of stroke symptoms) is not difficult if a competent radiologist uses technology such as DWI (Diffusion weighted imaging). When using this diffusion-weighted imaging protocol (in brain scanning) on MRI, changes are visualized a maximum of 5 minutes after the development of symptoms.
But MRI may not show a stroke in the acute period if standard classical research protocols are used, although even with classical protocols, MRI in diagnosing a stroke reveals changes much faster compared to CT (computed tomography).
This is a T2 MRI image of a patient who showed neurological symptoms two hours ago. Conclusion is the norm
The same patient who underwent diffusion-weighted and perfusion MRI scans. Lesion in the basin of the right middle cerebral artery. The patient was prescribed intensive therapy.
Conservative treatment of brain stem stroke
Treatment for brainstem stroke should begin immediately, in the first 4-6 hours. For this, a person must be hospitalized in a specialized department.
A patient with a brainstem stroke must stay in the intensive care unit for at least a week. The following measures are important at this time:
- Supports lung function. To do this, aspiration of the upper respiratory tract is performed, that is, pathological contents (sputum, mucus) are removed. The patient may need tracheal intubation or connection to a ventilator. If the oxygen concentration in the blood decreases, then oxygen therapy is performed.
- Maintaining normal blood pressure levels. In this case they are up to 160/90 mm Hg. Art., and for hypertensive patients – up to 180/100 mm Hg. Art. You can adjust your blood pressure with Enalapril, Labetalol, Dibazol. These drugs are first administered intravenously, and when the acute period subsides, they are taken orally. With low blood pressure, infusion therapy with a solution of albumin and sodium chloride is required. It is combined with the use of vasopressor drugs - Mezatone, Dopamine, Norepinephrine.
- Maintaining biochemical blood parameters. Sugar can be low or high. In the first case, the patient needs glucose, in the second, insulin.
- If body temperature is above 37.5°C, then it must be reduced. To do this, use Paracetamol or Ibuprofen. Magnesium sulfate is also prescribed intravenously.
- Reducing cerebral edema. In this case, an integrated approach is required. The patient is given glycerin or Mannitol and an albumin solution is injected. They also resort to sedatives and muscle relaxants: Diazepam, Pancuronium. If drug therapy is ineffective, the patient is put into a barbiturate coma or craniocerebral hypothermia is used (the temperature of the brain is lowered).
- To reduce blood clotting, anticoagulants are prescribed. Often a person needs such therapy for life.
Depending on the characteristics of the patient's condition, symptomatic treatment is required. Severe nausea and vomiting can be treated with Cerucal. For convulsions, they resort to Diazepam. Relanium and magnesia are effective as sedatives.
Damaged brain structures can be restored using neuroprotective therapy. It includes taking Glycine, Piracetam, Cerebrolysin and other drugs of these groups.
Classification
Brainstem stroke is a special case of acute disruption of cerebral blood flow through the vertebrobasilar vessels. It comes in two types - ischemic and hemorrhagic (parenchymal or intraventricular hemorrhage). In its development, the disease goes through several stages: acute, subacute, organization (recovery). Taking into account the etiopathogenetic features, several types of ischemic strokes are distinguished:
- Atherothrombotic. They occur against the background of atherosclerosis of the cerebral arteries and progress gradually. Acute ischemia can be preceded by transient disturbances of cerebral blood flow.
- Cardioembolic. Accompanied by complete or partial occlusion of the lumen of the main artery by an embolus of extracranial (cardiogenic) origin. They begin suddenly, are characterized by a severe course, the presence of a hemorrhagic component, and have a serious prognosis.
- Hemodynamic. The development of strokes is caused by disorders of systemic hemodynamics, combined with pathology of extracranial and intracranial arteries in the absence of significant atherosclerotic occlusion, sources of cardiogenic embolism. They arise acutely or gradually.
- Lacunar. Caused by damage to perforating arteries. Lacunar stroke is characterized by the formation of limited areas of ischemia located in the subcortical nuclei and white matter of the brain.
When making a diagnosis, the localization of pathological foci, the extent of the process, and the side of the lesion are taken into account. Taking into account the location in the brainstem, strokes of the pons, thalamus, medulla oblongata and midbrain occur. In addition to isolated injuries, two or more sections may be involved. Damage to stem structures is rarely mild, usually the condition varies from moderate to extremely severe.
Surgery
Conservative therapy and auxiliary measures are not enough. In this case, surgical intervention is advisable.
If intracranial pressure cannot be stabilized by other methods, then hemicraniectomy . Its effectiveness is higher, the younger the patient's age. After 60 years, such intervention is not performed.
The essence of hemicraniectomy is to provide free space for the swollen brain. This helps prevent it from being squeezed. The patient has part of the bone tissue removed, closing the resulting hole with a flap of skin.
Minimally invasive intervention can be used to resolve the hematoma . In this case, it is enough to make a small hole and inject a thrombolytic into it, which will resolve the hematoma.
How does a stroke manifest in pathology of the midbrain arteries?
The clinical picture of cessation of blood circulation depends on the degree of destruction of the nuclei of the III and IV pairs of cranial nerves. A brainstem stroke is accompanied by the appearance of Claude (Loyer) symptoms. The patient experiences ptosis of the upper eyelid, impaired coordination of movements, and trembling of the limbs. The oculomotor nerve is affected and paralysis is observed on the side of the lesion.
The patient experiences rhythmic contraction of the soft palate. The muscles of the larynx, pharynx, and eyeballs are affected. Many patients experience the following disorders simultaneously with brainstem symptoms:
- false light sensations;
- weakened vision;
- memory loss;
- changes in sensitivity and touch.
If the third pair of cranial nerves is affected, the patient suffers from the inability to move the eyeballs to the side and up. A bilateral stroke in the midbrain region causes insomnia and impaired consciousness. The patient is in a state of deep stupor, sometimes a mental disorder develops, accompanied by hallucinations and delusions. A person perceives reality as if through a veil, sleeps a lot during the day, is silent, and does not come into contact with the people around him.
Rehabilitation activities
Rehabilitation after a brainstem stroke is definitely required, as this will allow you to achieve very good results and normalize your well-being. If there are problems with the swallowing process, but motor activity is not impaired, then classes with a speech therapist are required.
If there are problems with movements, it is important to restore the normal functioning of the limbs in the first 2-3 months, since after this the dynamics decrease significantly. If motor activity has not returned to normal within a year after the onset of the disease, then subsequent rehabilitation will be significantly more difficult.
It is impossible to eliminate respiratory distress during a brainstem stroke on your own. The prognosis for rehabilitation is disappointing, since patients cannot cope without artificial aids. If the breathing center is partially disrupted, victims experience slight shortness of breath during sleep.
Impaired heart function and thermoregulation are practically impossible to correct, as this may indicate atrophy of brain cells.
The recovery process takes quite a long time. Even with minor and localized brain damage, it is almost impossible to completely eliminate all existing changes. During the patient’s rehabilitation process, he is prescribed exercise therapy and additional rehabilitation procedures. The first classes are performed lying down, and they are aimed at completely restoring the required motor functions of the limbs. Over time, exercise therapy is prescribed to restore facial expressions and speech functions. Massage and manual therapy help very well. There is also evidence that magnetic therapy is effective, as it has a positive effect on the restoration of nerve endings.
Treatment of movement disorders
The consequences of ischemic stroke are eliminated using various methods of restoring impaired functions. In the early period of the disease, treatment measures are aimed at saving the patient’s life. Before starting rehabilitation therapy, the general condition of the patient and the presence of associated complications are studied. The doctor prescribes drugs that activate the functioning of nerve cells:
- Gammalon;
- Actovegin;
- Piracetam;
- 0.1% nasal drops Semax.
For decreased muscle tone, medications are used:
- Prozerin;
- Nivalin;
- Oxazyl.
Special gymnastics helps prevent increased muscle tone. Position therapy is prescribed. The patient lies on his back and healthy side for several hours. The paralyzed arm is placed on a pillow, and the affected leg is bent at an angle of 15-20°. Position therapy avoids stress on the same muscle groups and reduces the likelihood of developing pain in the shoulder joint.
The patient is prescribed a course of massage for post-stroke movement disorders. Use acupuncture, gentle rubbing, shallow kneading. Active gymnastics is of great importance for stabilizing a person’s motor function.
Hemorrhage in the area of the pons
The occurrence of ischemic stroke is facilitated by thrombosis of the great vessels or narrowing of the lumen of the vertebral arteries. Symptoms of damage to the pyramidal tract and the gray nucleus of the pons are characterized by complete paralysis of the arm and leg on one side, disruption of the facial and hypoglossal nerves. The patient suffers from a sensitivity disorder. There is a decrease in muscle tone, a lack of protective reflexes, and vegetative-trophic disorders appear.
The patient's strength of the extraocular muscles changes. Consciousness is preserved. If bilateral hemorrhage occurs, the patient is completely immobilized. The swallowing process is disrupted, the patient cannot chew food. The voice becomes hoarse and speech becomes difficult. The face resembles a mask, a large amount of saliva is released from the mouth, and intelligence decreases.
If the circumflex branch of the left atrial artery is damaged, the patient experiences an imbalance of the body when walking, drooping of the upper eyelid, and constriction of the pupils. The patient does not respond to external stimuli, and sometimes convulsions develop. Ischemic stroke (heart attack) is accompanied by a sensitivity disorder of the facial nerve on the affected side. A seriously ill person experiences coma or other blackout syndromes.